Abstract
PURPOSE
Primary care transformation is widely seen as essential to improving patient outcomes and health care costs. The medical home model can achieve these ends, but dissemination and scale-up of practice transformation is challenging. We sought to understand how to move past successful pilot efforts by early adopters to widespread adoption by applying cognitive task analysis using the diffusion of innovations framework.
METHODS
We undertook a qualitative cross-sectional comparison of 3 early adopter practices and 15 early majority practices in Alberta, Canada. Practices completed a total of 42 cognitive task analysis interviews. We conducted a framework-guided qualitative analysis, with allowance for emergent themes, using the macrocognition framework on which cognitive task analysis is based. Independent codings of interview transcripts for key macrocognitive functions were reviewed in group analysis meetings to describe macrocognitive functions and team mental models, and identify emergent themes. Two external focus groups provided support for these findings.
RESULTS
Three prominent findings emerged. The first was a spectrum of mental models from “doctor with helpers,” through degrees of delegation, to fully team based care. The second was differences in how teams distributed macrocognitive functions among members, with early adopters distributing these functions more widely across the team than early majority practices. Finally, we saw emergence of several themes also common in the diffusion of innovations literature, such as the importance of trying new practices in small, reversible steps.
CONCLUSIONS
Our findings provide guidance to practice teams, health systems, and policymakers seeking to move beyond early adopters, to improve team functioning and advance the medical home transformation at scale.
Key words: patient centered medical home; cognitive task analysis; diffusion of innovations theory; chronic disease; practice patterns, physicians’; change, organizational; primary care; practice-based research
INTRODUCTION
Transformation of primary care is widely seen as essential to addressing quality, satisfaction, and cost issues in health care. The patient-centered medical home (PCMH)1 in the United States and the patient’s medical home (PMH)2 in Canada are similar models for doing so; both emphasize a team-based approach and require profound changes in practices. The PMH transformation is an important reason for the Ministry of Health’s funding for the 41 primary care networks (PCNs) in Alberta, Canada.3,4 Although nearly all practices have joined a PCN, giving them access to funding and support for transformation, widespread adoption of the PMH has not occurred. Alberta is not alone: a 2015 national report identified scaling up from demonstration projects to systemic practice as one of the central problems that Canadian health care faces today.5
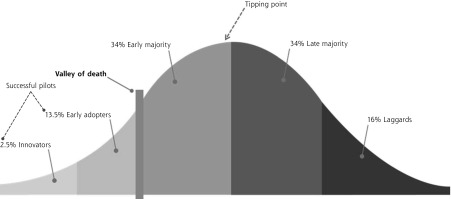
We examined the problem of dissemination and scale-up using the diffusion of innovations framework.6 Diffusion of innovations is a large body of literature addressing the adoption of new practices, products, and technologies that has proven applicable across many fields, including health care. It is best known for its identification of the specific subgroups depicted in Figure 1. We focused particularly on the so-called chasm or valley of death: the gap between the early adopters and the early majority. A main challenge appears to be that the early majority and the innovators and the early adopters who successfully demonstrated the innovation have different mental models of practice and practice change.
Figure 1.
Diffusion of innovations framework.
From Rogers.6
A mental model7 is more than a set of beliefs and values; it is a dynamic structure. Mental models determine what we pay attention to, what options and possibilities we consider, and how we make sense of events and experiences, solve problems, formulate judgments, and ultimately make decisions and act. Mental models are a cognitive-science path to addressing 2 of the 3 key basic clusters of factors in diffusion of innovations: perceptions of the change and characteristics of the potential adopters.8 Changes in mental models have been identified as important in adopting the PCMH.9,10 We suspected that the mental models of early adopter practices and early majority practices differed in crucial ways that would have to be addressed directly in order to move the PMH transformation across the valley of death.
METHODS
Participants
We trained a group of highly skilled and experienced practice facilitators based in the Alberta Medical Association11 as research associates for this project. The 10 research associates (9 women and 1 man, all cisgender) all had graduate or professional degrees in nursing, education, or social sciences.
The Alberta Medical Association facilitators have extensive personal networks of contacts among family physicians and PCNs across Alberta. They compiled a list of candidate physicians fitting the early majority profile: open to change but not necessarily the first to take up a change, interested but cautious. They similarly compiled a list of early adopters. Physicians were chosen from the lists to maximize geographic diversity (rural-urban and north-south) and demographic diversity (sex, years in practice, full vs part time), and asked to also suggest others in an informal chain-referral sampling process.12 Physicians who joined nominated 1 or 2 team members who might be interested in being interviewed. Because we were interested primarily in the mental models of the early majority, we selected most participants from that group, including only 3 early adopters to provide contrast. No participants asked to withdraw after agreeing to participate.
Data Collection
We used cognitive task analysis (CTA) to elicit physicians’ and team members’ mental models of team-based chronic disease management (CDM) and of taking on new ways of working. CTA is a set of highly structured qualitative techniques with a long track record of successfully enabling understanding and improvement of team functioning in high-stakes settings such as aviation, fire fighting, military command, intensive care, and surgical training.13–15 We pioneered the application of CTA to primary care16 and developed a program for training primary care practice facilitators in the method.17 We used CTA because it provides tools that illuminate physicians’ and teams’ knowledge work (macrocognitive) skills and actions (Table 1), is a proven method of eliciting teams’ mental models, and, most importantly, has been demonstrated to translate that understanding into practice change and performance improvement.
Table 1.
Descriptions of Macrocognitive Functions
| Function | Description |
|---|---|
| Sensemaking and learning (SL) | Deliberate attempt to find coherent situational understanding |
| Modifying a mental model or generating a new one | |
| Includes sense giving (presenting an understanding to others to adopt) | |
| Decision making (DM) | Decisions in, or about, patient care and administrative processes |
| Planning and replanning (PL) | Shaping or reshaping patient care or administrative processes |
| Monitoring and problem detection (MD) | Tracking the progress or outcomes of patient care or administrative processes |
| Planned, ad hoc (“noticing”), formal (data collection), or informal | |
| Managing the unknown, unclear, unexpected, and irregular (MU) | Planned or anticipatory (contingencies, fallbacks) |
| Evaluating/estimating risks | |
| Unplanned, “scrambling” | |
| Coordinating (CO) | Any activity that helps synchronize 2 or more individuals in a patient care or administrative process, especially transmitting information or expectations |
| Maintenance of “common ground,” shared expectations/understanding/mental models of processes |
We chose the team knowledge audit method of CTA13 as that best suited to our task. The research associates (K.K.W., J.A., L.T., and others) and the University of Alberta researchers (L.A.G., T.B.) together developed the interview guides (Supplemental Appendix, available at http://www.AnnFamMed.org/content/17/Suppl_1/S50/suppl/DC1/). The research associates conducted 1-hour individual interviews with 1 physician and 1 or 2 team members (nurses, medical office assistants [MOAs], or practice managers) in each clinic. Interviewers worked in pairs consisting of a lead and a note-taker/second, which is standard practice for CTA.13
We conducted a total of 42 CTA interviews across 18 family medicine clinics in Alberta (Table 2). Interviews were audio-recorded and transcribed for coding and analysis. Transcripts were not returned to participants for comment. The interviewers made field notes addressing contextual information such as physical space and workflow patterns, and collected artifacts such as copies or screenshots of forms used to pass information.
Table 2.
Participant, Practice, and Focus Group Characteristics
| Characteristic | Number |
|---|---|
| Participants (n = 42) | |
| Physiciansa | |
| Men | 10 |
| Women | 4 |
| Early adopters | 3 |
| Early majority | 15 |
| Staff | |
| Men | 0 |
| Women | 15 |
| RN or LPN | 7 |
| MOA or manager (clinical) | 5 |
| Practice manager (nonclinical) | 2 |
| Dietician | 1 |
| Practices (n = 18) | |
| Setting | |
| Rural | 8 |
| Urban | 10 |
| Location | |
| North | 9 |
| South | 9 |
| Focus groups (n = 2) | |
| Total participants | |
| Focus group 1 | 6 |
| Focus group 2 | 7 |
| Participant credentials | |
| RN (including chronic disease management nurses) | 12 |
| Other (MOA, LPN) | 1 |
| Participant employment | |
| Directly by clinic | 1 |
| By a primary care network | 12 |
| Participant practice setting | |
| Rural | 3 |
| Urban | 9 |
| Both | 1 |
LPN = licensed practical nurse; MOA = medical office assistant; RN = registered nurse.
Time in practice ranged from ≤1 year to 43 years.
Data Analysis
We conducted a framework-guided qualitative analysis, with allowance for emergent themes, using the macrocognition framework (Table 1) on which CTA is based.18–20 Each transcript was divided into utterances comprising a query and its reply, and every utterance was coded by 2 research team members. The 2 team members were chosen in alternating fashion, so each of the 12 research team members coded at least 1 transcript. We chose not to calculate interrater reliability, to avoid dampening discussion.
Whole-team analysis meetings were then held to review the coded transcripts. The whole-team approach was chosen because (1) it maximized shared learning among the team members, and (2) it allowed interaction of those who had visited a site and those who had not, capturing the rich information of the former but also avoiding unspoken assumptions through the questioning of the latter. Each meeting lasted 3 hours and typically completed a single practice’s transcripts, for example, those for a physician and 1 or multiple team members. Each began with a description of the site presented by the interview team, along with review of artifacts and field notes. The coded transcripts were then reviewed, and discrepancies were reconciled in discussion.
All utterances for each code were grouped, and for each code, the team reviewed, discussed, and built a narrative description of how and how well the practice conducted that macrocognitive function. The team then came to consensus on the degree to which that function was centrally held or distributed across the care team. The team then reviewed the coded transcripts for disconfirming information (inconsistent with the narrative), and the summary was adjusted as needed. Finally, the team reviewed all of the narrative summaries and distributions of functions, plus emergent findings, to build a narrative description of the mental model of the practice.
Two methods were used to address trustworthiness of our findings. First, sites’ own findings were discussed informally with them. Second, for geographic reasons, study findings were discussed in 2 focus groups (Table 2) that were conducted by 2 of the research associates with nonstudy practices in study PCNs, to gather external validation perspectives. These groups included only staff, because of limitations on physician availability.
Ethical Considerations
This project was evaluated by the University of Alberta Health Research Ethics Board and deemed outside of review (Pro00065548 and Pro00066588). All identifiers were removed at the time of transcription.
RESULTS
Spectrum of Mental Models
We found a distinct spectrum of mental models. At one end were teams whose mental model could be described as “the doctor takes care of patients and hires some people to help her/him.” Next were teams that used their PCN’s services, such as diabetes care nurses or registered dieticians, but in a directed and circumscribed role. Their mental model we described as “the doctor takes care of patients and refers them out to get specific things done.” Further along the spectrum were teams that incorporated CDM nurses, registered dieticians, or others into the team and delegated meaningful decision making in those areas to them. Their mental model we described as “the doctor takes care of patients but delegates significant work to team members.” Finally, at the other end of the spectrum was the fully team based model: “we take care of patients.”
For brevity, we designated this 4-level spectrum of mental models as physician-centric, referral, delegating, and team-based. All 3 early adopter practices and 2 of the 15 early majority practices were at the team-based end, with 2 more close to it. Three early majority practices were physician-centric, 3 were referral, and the remaining 5 were delegating or between referral and delegating. The 2 ends of this spectrum—physician centric and team based, respectively—are represented in the following quotes; each is a physician describing his or her working relationship to the CDM nurse:
Well she (CDM nurse) could be introduced at the end of the introducing the disease (to the patient) because quite honestly, an awful lot of people don’t have the right idea, they don’t have the right figures about what’s going to happen. … She’s maybe employed by the PCN, but she works in our clinic.
and
… she (CDM nurse) knows sort of my scope of practice, I know her scope of practice, we don’t really have a hierarchical relationship … we work together as a team and there are times that she will see patients independent of me and let me know what’s happening afterwards as well.
In early adopter practices, the mental model was typically held by all members of the clinic, that is, a fully shared mental model. In most (11) of the early majority practices, however, we observed that the mental models were not shared across the clinic teamlets (physician plus 1 or more staff who normally worked with him/her). Rather, 1 teamlet was often substantially further to the right on the spectrum than the others in the clinic. The other teamlets were sometimes not very aware of what the index teamlet was doing, but frequently were aware and not very interested. One physician described how the MOA role changed in certain teamlets but not the full clinic:
It was really between me and my MOA and between the other doctor and his MOA, and the other doctors expected different things from their MOAs. They didn’t really expect them to look at the screening. So it was very much doctor and MOA, and not a team (clinic) thing.
Distribution of Macrocognitive Functions
Closely tracking the mental model spectrum were marked differences in how the macrocognitive functions were distributed across team members. All 3 early adopters involved all members of the team in sensemaking, coordination, and other functions. One physician described his deliberate effort to distribute the macrocognitive functions:
… the nurses were not really maximized in terms of scope, nor were the MOAs … and so at that time, I identified to them the need from my perspective that we had to achieve a high-level standard of care, so the rationale, the “why” for the team.
Early majority practices tended to hold these functions more centrally, in the physician or at most, the physician and another formal leader (eg, a practice manager). Six practices held them almost entirely centrally and 4 were more centralized than not; 5 had become mostly distributed. Importantly, interviews from those 5 practices indicated that they had achieved that distribution by deliberate effort over time, from a starting point of centrally held functions. The following quotes illustrate the range of distributions, from less to more distributed:
No, like it came down from above, and I know that it was probably discussed with the doctors and then the information flows over to us to …
and
… but every plan that we make, we have to bring first to the doctors group and they approve it and then we can move onto the MOAs …
and
Previous management was basically a 1-doctor show … the big shift has been to a partnership and a team-style management where we ask for input, and we discuss things together …
Themes Related to Diffusion of Innovations
Themes important in the diffusion of innovation literature appeared, unanticipated, in our “emergent” category. Only a few were found in any 1 interview, but each was found in several. Our analysis of these themes was limited, as our interview guide did not probe for them, but we present them as an important serendipitous finding.
Early adopters often spoke in terms of the big picture, with a clear sense of how what they were doing for CDM fit into the PMH as a whole:
We also have a multidisciplinary team out here that we’ve been building, not just for CDM, but to be a better clinic.
Early majority physicians, however, tended to speak in terms of the immediate project, rather than the big picture. This phenomenon is depicted in 1 physician’s description of the benefits of the nurse’s role changing:
… I get to know about all those with the blood pressure a heck of a lot sooner than I did in the past because now the nurse picks up on it, “you know, we need to look at this guy.”
Early majority physicians were open to considering changes that could improve patient care, but only in small, manageable, potentially reversible steps (referred to in the diffusion literature as trialability), and only if there were no disincentives or system barriers. One physician discussed the process of addressing patient wait times via a trial period:
… we talked about how much time to spend with each patient, right, and then we just increased the time, and then we just sort of discussed what does that mean in terms of how the EMR [electronic medical record] functions and those sorts of details, and then we said, we’ll try this out for 3 months, and at the 3-month mark we came back and said, “Yes, this is working much better.”
A practice manager we interviewed also found a 3-month trial the best approach for having practices implement new ways of working:
So another thing that I always say is, let’s trial it for 3 months, let’s just see what happens, let’s see and let’s take a review at the end of our 3 months … So at the end of 3 months, what I did was statistical information showing where we were before and where we went to, and it was overwhelmingly big.
In contrast, early adopters were willing to make larger changes and to swim upstream against local norms and system barriers. A physician explained this process in terms of getting the clinic on board with complex care plans:
Well, we had to motivate our physicians that these (visits) were worthwhile. Then we had to decide who the clinical providers were, to do different step. … We got our different levels of care providers to do those time-consuming tasks that need to be done, so that they’re done and then we can present them to the patient and come up with a plan. Then we had to say to our physicians … if all these other things are done for you, then what are you doing? You’re overseeing it all, but then actually one of the real heart of the matters on this thing is, that the physician is seeing their patient and that they’re making goals.
Finally, early adopters were often willing to try something they read about or saw presented at a conference:
The owner actually … he was at a conference … where they were talking about medical homes and he came back and he said, “… you’ve got to look this up, what is this?” and so I did some research on it and … this embodies everything that we believe in, this matches up with our vision and our mission statement, and this is who we want to be …
Early majority physicians, on the other hand, often engaged once an idea was brought to them by a trusted, local source, such as a physician who reported hearing about their program implementation from trusted PCN members:
… it was just really accessible right in front of us, and it was really ready to use.
Participants in the external focus groups indicated that the findings resonated with them also and did not suggest any missing themes. We did not transcribe or code the discussions; they served only for providing assurance that we had not missed important points.
DISCUSSION
In our data, we found a well-defined spectrum of mental models and distinct differences in the distribution of team macrocognitive functions across that spectrum. We also found emergent themes that are common in the diffusion of innovation literature. The findings on the spectrum of mental models replicate and extend those of PCMH research in the United States.9,10 The findings on distribution of macrocognitive functions are, similarly, consistent with long-standing observations that team roles must change to implement the PCMH,10 adding specificity to those previous findings as well as confirming them through a different methodology. The distribution findings also parallel findings from studies of communication networks in primary care teams.21,22 The spontaneous emergence of diffusion of innovation themes in our data lends credence to the methods we used for data collection and analysis.
A limitation of our study is that we are not certain that we achieved saturation; however, we used CTA as it most often is, and was designed to be, used: to guide action. In this engaged-scholarship23 project, the benchmark of success for our stakeholders is not necessarily a complete understanding of all the facets of the spread and scale problem, but rather timely delivery of an actionable understanding of major aspects that can direct intervention. It is possible, perhaps even likely, that minor aspects remain to be discovered, but it is unlikely that major aspects have been missed.
Taken together, these 3 sets of findings help us understand how early majority and early adopter practices differ, why health systems in Canada and elsewhere have difficulty moving the PMH beyond early adopters, and how that difficulty might be addressed. An early majority practice may successfully transition to a team-based mental model, but it does not become an early adopter in how it processes change. It still needs small, manageable steps and active facilitation, and will not spontaneously swim upstream.
The findings about distribution of macrocognitive functions provide an implementable path forward. Distributing those functions is a skill that can be taught, as demonstrated in the macrocognition literature, and can be undertaken in small steps amenable to the early majority’s inclination. Further, the experience gained will guide practices along the spectrum of mental models. This skill cannot, however, be learned from meetings, seminars, or lists of best practices. It requires coaching for the physician and the team, as well as support for these potentially anxiety-provoking changes. It also requires skill building for the team members, to give them the ability to take up a larger role in those key team functions. These requirements lead us to conclude, as others have also shown, that practice facilitation is essential.24
Acknowledgments
We thank all the participants for engaging in this important research that seeks to transform our primary health care system toward our vision: the Patient’s Medical Home. We also thank the many primary care networks (PCNs) that supported this work. Lastly, we acknowledge the full Alberta Medical Association team for their dedication, insight, and enthusiasm: Sandee Foss, June Cooper, Laurie deBoer, John Lester, Sue Peters, Barbra McCaffrey, Andrea Atkins, Mark Watt, Eileen Patterson, and Arvelle Balon-Lyon.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.AnnFamMed.org/content/17/Suppl_1/S50.
Funding support: Alberta Innovates’ Senior Translational Health Chair award provided funding for this research.
Previous presentations: Portions of this work have been presented at the Family Medicine Forum; November 8-11, 2017; Montreal, Quebec, Canada, and at the North American Primary Care Research Group Annual Meeting; November 17-21, 2017; Montreal, Quebec, Canada. The Office of the Auditor General of Alberta has been briefed on the final analysis.
Supplemental Materials: Available at http://www.AnnFamMed.org/content/17/Suppl_1/S50/suppl/DC1/.
References
- 1.Patient-Centered Primary Care Collaborative. http://www.pcpcc.org/. Published 2014 Accessed Apr 6, 2014.
- 2.College of Family Physicians of Canada A vision for Canada. Family practice: the patient’s medical home. https://www.cfpc.ca/uploadedFiles/Resources/Resource_Items/PMH_A_Vision_for_Canada.pdf. Published Sep 2011 Accessed Apr 5, 2019.
- 3.Government of Alberta Primary Health Care Strategy. https://www.alberta.ca/primary-health-care.aspx?utm_source=redirector#toc-5 Accessed Aug 4, 2015.
- 4.Auditor General of Alberta Primary care networks. https://www.oag.ab.ca/reports/health-primary-care-networks-oct-2017. Published Oct 2017 Accessed Jul 4, 2017.
- 5.Naylor D, Girard F, Fraser N, et al. Unleashing Innovation: Excellent Health Care for Canada. Ottawa, ON: Health Canada; 2015. http://healthycanadians.gc.ca/publications/health-system-systeme-sante/report-healthcare-innovation-rapport-soins/alt/report-healthcare-innovation-rapport-soins-eng.pdf Accessed Apr 5, 2019. [Google Scholar]
- 6.Rogers EM. Diffusion of Innovations. 5th ed. New York, NY: Free Press; 2003. [Google Scholar]
- 7.Johnson-Laird PN. Mental models and deduction. Trends Cogn Sci. 2001; 5(10): 434–442. [DOI] [PubMed] [Google Scholar]
- 8.Berwick DM. Disseminating innovations in health care. JAMA. 2003; 289(15): 1969–1975. [DOI] [PubMed] [Google Scholar]
- 9.Cronholm PF, Shea JA, Werner RM, et al. The patient centered medical home: mental models and practice culture driving the transformation process. J Gen Intern Med. 2013; 28(9): 1195–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010;8(Suppl_1):S45–S56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toward Optimized Practice (TOP). http://topalbertadoctors.org/home/ Accessed Apr 26, 2015.
- 12.Given LM, ed. The Sage Encyclopedia of Qualitative Research Methods. Los Angeles, CA: Sage Publications; 2008. [Google Scholar]
- 13.Crandall B, Klein GA, Hoffman RR. Working Minds: A Practitioner’s Guide to Cognitive Task Analysis. Cambridge, MA: MIT Press; 2006. http://www.books24x7.com/marc.asp?bookid=12926 Accessed Oct 8, 2012. [Google Scholar]
- 14.Wingfield LR, Kulendran M, Chow A, Nehme J, Purkayastha S. Cognitive task analysis: bringing Olympic athlete style training to surgical education. Surg Innov. 2015; 22(4): 406–417. [DOI] [PubMed] [Google Scholar]
- 15.Potworowski G, Green LA. Cognitive task analysis: methods to improve patient-centered medical home models by understanding and leveraging its knowledge work. https://pcmh.ahrq.gov/sites/default/files/attachments/CognitiveTask_032513comp.pdf. Published 2013 Accessed Apr 5, 2019.
- 16.Christensen RE, Fetters MD, Green LA. Opening the black box: cognitive strategies in family practice. Ann Fam Med. 2005; 3(2): 144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Potworowski G, Green LA. Training change agents in CTA to bring health care transformation to scale: the case of primary care practice facilitators. J Cogn Eng Decis Mak. 2016; 10(4): 328–349. [Google Scholar]
- 18.Klein G, Wright C. Macrocognition: from theory to toolbox. Front Psychol. 2016; 7: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patterson ES, Miller JE, eds. Macrocognition Metrics and Scenarios: Design and Evaluation for Real-World Teams. Burlington, VT: Ashgate; 2010. [Google Scholar]
- 20.Klein G, Ross KG, Moon BM, Klein DE, Hoffman RR, Hollnagel E. Macrocognition. IEEE Intell Syst. 2003; 18(3): 81–85. [Google Scholar]
- 21.Mundt MP, Agneessens F, Tuan W-J, Zakletskaia LI, Kamnetz SA, Gilchrist VJ. Primary care team communication networks, team climate, quality of care, and medical costs for patients with diabetes: a cross-sectional study. Int J Nurs Stud. 2016; 58: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mundt MP, Gilchrist VJ, Fleming MF, Zakletskaia LI, Tuan W-J, Beasley JW. Effects of primary care team social networks on quality of care and costs for patients with cardiovascular disease. Ann Fam Med. 2015;13(2):139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rewarding community-engaged scholarship. Transforming university policies and practices. Resources. http://engagedscholarship.ca/resources/ Accessed Feb 15, 2016.
- 24.Wang A, Pollack T, Kadziel LA, et al. Impact of practice facilitation in primary care on chronic disease care processes and outcomes: a systematic review. J Gen Intern Med. 2018; 33(11): 1968–1977. [DOI] [PMC free article] [PubMed] [Google Scholar]