Abstract
Purpose
Caring for a child with cancer or hematologic disease places unique stress on a family unit. Families’ subjective experience of this care-related burden mediates the relationship between cost and health-related outcomes. While financial costs are well described for families of pediatric hematology/oncology patients, it is unclear how cost and other factors each contribute to families’ overall experience of care-related burden. This study identifies and groups the challenges that families report and describes their association with overall reported burden.
Methods
This mixed-methods analysis of a cross-sectional single-center study was conducted via structured, self-administered questionnaire provided to inpatient and outpatient caregivers of pediatric hematology/oncology patients. Respondents rated their perception of burden associated with that day’s medical encounter on a 5-point Likert scale. The questionnaire included an open-ended prompt for caregivers about areas they deemed most burdensome. Primary themes were extracted and categorized.
Results
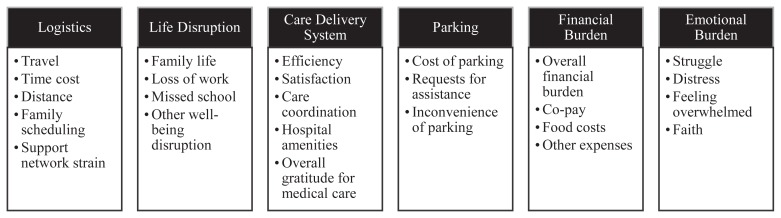
A total of 278 outpatient and 42 inpatient caregivers participated. Six thematic categories emerged: logistics, life disruption, care delivery system, parking, financial burden, and emotional burden. Outpatient caregivers reported more burden than inpatient caregivers for the first three categories, while inpatient caregivers reported more burden for the last three. Salient subthemes associated with higher and lower overall burden were identified in each theme category.
Conclusions
These data establish theme categories for future study of caregiver-perceived burden in pediatric hematologic/oncologic encounters, demonstrate that certain components of cost contribute disproportionately to caregivers’ overall sense of care-related burden, and identify areas within each of the 6 burden categories that can be best targeted to alleviate caregiver burden.
Keywords: cancer, oncology, cost of illness, caregiver, burden of care
Families of children with complex medical needs grapple not only with the emotional burden of their child’s illness but also with the distress of financial and logistical hurdles to care. There is a well-described connection between overall financial toxicity of cancer treatment and health-related quality of life1 and early mortality2 in adults; however, there is a paucity of research describing how families experience the burden of care over individual care encounters in the pediatric population.
Understanding the perceived burden per care encounter is critical in the pediatric hematology/oncology population, as patients primarily access cancer care via repeated or prolonged encounters.3,4 Financial burden increases with increased number of encounters or encounter days5,6 and thus may correspond to an increase in nonfinancial burden on an encounter-by-encounter basis. Our previous research describes that financial costs can be accurately modeled in terms of travel costs, lost wages, direct medical expenses, and food expenses.7 However, the relationship between cost and health outcomes is mediated by a key factor: how patient families actually perceive the burden and value associated with various health care costs.8–11 Cost analysis can describe which components of care produce the most financial burden; understanding how each individual stressor contributes to the overall psychosocial burden of care requires family input on their perception of burden.
Current research indicates that some of the detrimental effects of cost and burden may be mediated by caregivers’ psychological perceptions of those costs and burdens, but a review of pediatric cancer research finds that the psychosocial effects of cancer-related costs have not been comprehensively studied in the pediatric cancer population.12 In the pediatric complex care population, however, one caregiver-crafted testimony noted that measures decreasing the anxiety and isolation of care also lead to improved engagement with care.13 Further, in caregivers of pediatric patients with chronic pain, psychosocial caregiver burden can include parental depression, anxiety, self-blame, and maladaptive behavioral responses.14 In the geriatric population, which shares some analogies in caregiver-patient relationships, the patient caregiver’s perception of burden directly interferes with what information they give health care providers and the health care provider-patient relationship.8 In pediatric patients considering bone marrow transplant, “desiring a more normal and better quality of life for the patient and family” frequently contributed to caregivers’ choice against lifesaving but burdensome treatment,9 showing that how caregivers perceive burden affects not only communication but also medical decision-making.
Caregiver-perceived burden also influences quality of life for the dyad. In adult patients with advanced cancer, supportive interventions for caregivers resulted in modest improvements to both long- and short-term quality of life.10 Further, in pediatric cancer patients, social and financial family burden has been identified as a key mediator of the relationship between low socioeconomic status and poor quality of life, implying a possible amplification effect of burden.11 Associations between burdens and outcomes demonstrate that caregivers’ perception of care-related burden — beyond solely the financial burden itself — moderates detrimental health-related effects of care. Our study explores what drives families’ perceptions about the perceived burden of given care encounter.
This mixed-methods study analyzed caregiver comments, cost, and demographic data from a cross-sectional survey of cost and burden data among caregivers of pediatric hematologic/oncologic patients at a tertiary care center in Houston, Texas. Inpatient and outpatient caregivers responded to an open-ended prompt about areas they considered most burdensome to their current medical encounter and rated their burden for that day. We explored these comments for themes contributing to caregiver burden, specifically assessing whether any themes were disproportionately associated with self-rated burden or other quantitative metrics.
METHODS
Survey Design and Implementation
Details of the development and implementation of this survey have been described previously and were approved by the Baylor College of Medicine (Houston, TX) institutional review board.7 In brief, clinical researchers and social workers developed the survey, and parents of patients with cancer or hematologic diseases reviewed the survey for usability. The survey included multiple-choice and short-answer questions; a sample of relevant questions is included in Table 1.
Table 1.
Representative Sample of Relevant Survey Questions
| Domain | Question | Answer |
|---|---|---|
| Caregiver sociodemographics | 1. How are you related to the patient? | Mother Father Other |
| Patient information | 2. What is your child’s diagnosis? | Leukemia or lymphoma Brain tumor Solid tumor Other cancer Sickle cell Bleeding disorder Other blood diagnosis |
| Perception of burden | 3. How difficult was it for you to come to clinic today? | This clinic visit made little or no impact on my/my family’s life This clinic visit caused some changes to my/my family’s life This clinic visit was inconvenient This clinic visit was difficult but manageable This clinic visit required major changes to my/my family’s life |
| Qualitative | 4. Do you have any comments that you feel would help us understand how having a child visit clinic affects you or your family? |
A paper version of the survey was given to one caregiver for every patient checking into Texas Children’s Cancer and Hematology Center’s outpatient clinic for a week. Caregivers were informed verbally and via cover letter about the research objective and voluntary nature of the survey. Caregivers completed and returned the survey by hand while in the clinic. The survey also was repeated for caregivers of patients staying in the hospital as inpatients. One caregiver for each patient admitted to the hospital during 1 of 14 days was approached to participate. For brevity, only short-answer survey components are included herein.
Quantitative Self-Rating of Burden
Respondents were asked to rate their perception of burden associated with that day’s medical encounter using a 5-point Likert scale, responding to the prompt, “How difficult was it for you [or your family] to [come to clinic/be in the hospital] today?” (Table 1). This information was used to stratify respondents into high-burden (4–5 out of 5), intermediate-burden (3 out of 5), and low-burden (1–2 out of 5) groups.
Qualitative Analysis
The survey included an open-ended prompt for caregivers about areas that caregivers considered the most burdensome to their current medical encounter. Responses in Spanish were translated into English by H.A. All 4 authors independently read each comment and labeled any core themes invoked, using an inductive emergent theme identification approach.15,16 Inpatient responses were additionally given primary theme codes during an in-person consensual coding session.17 All primary theme codes were then extracted and grouped into theme categories. H.A, H.R., and M.H. met to agree on a set of secondary subtheme codes chosen from the primary code categories and individually recoded each comment by the secondary theme codes. The authors met to review the results of secondary coding and agree on final consensus theme codes and thematic categories for each comment.
RESULTS
Inpatient and Outpatient Findings
Patient demographics are shown in Table 2. In this study population, inpatient caregivers reported higher overall burden on average and were more likely to include financial and emotional burdens of care (Table 3).
Table 2.
Demographics of Survey Respondents
| Outpatient (n=278)* | Inpatient (n=42)* | |
|---|---|---|
| Respondent, n (%) | ||
| Mother | 213 (76.9%) | 33 (78.6%) |
| Father | 37 (13.4%) | 4 (9.5%) |
| Other | 21 (7.6%) | 4 (9.5%) |
| Patient’s diagnosis, n (%) | ||
| Cancer | ||
| Leukemia or lymphoma | 97 (34.9%) | 20 (47.6%) |
| Brain tumor | 19 (6.8%) | 3 (7.1%) |
| Solid tumor | 19 (6.8%) | 8 (19.0%) |
| Other cancer | 34 (12.2%) | 4 (9.5%) |
| Hematology | ||
| Sickle cell | 29 (10.4%) | 4 (9.5%) |
| Bleeding disorder | 12 (4.3%) | 1 (2.4%) |
| Other blood diagnosis | 51 (18.3%) | 1 (2.4%) |
| Race/Ethnicity, n (%) | ||
| White/Caucasian, non-Hispanic | 83 (30.0%) | 14 (33.3%) |
| Black/African American | 46 (16.6%) | 9 (21.4%) |
| Hispanic | 131 (47.3%) | 18 (42.9%) |
| Asian | 10 (3.6%) | 0 (0.0%) |
| Other | 4 (1.4%) | 0 (0.0%) |
| Patient’s age, n (%) | ||
| Less than 5 years old | 90 (32.4%) | 10 (23.8%) |
| 5 to 9 years old | 63 (22.7%) | 12 (28.6%) |
| 10 to 14 years old | 81 (29.1%) | 12 (28.6%) |
| 15 years old or older | 41 (14.8%) | 7 (16.7%) |
| Payer, n (%) | ||
| Medicaid/CHIP | 146 (52.5%) | 22 (52.4%) |
| Private | 117 (42.1%) | 14 (33.3%) |
| Other | 9 (3.2%) | 5 (11.9%) |
| None | 5 (1.8%) | 0 (0.0%) |
Not all respondents completed all demographic questions.
CHIP, Children’s Health Insurance Program.
Table 3.
Reported Burden of Analyzed Comments by Thematic Category
| Total,* n (%) | OP,* n (%) | IP,* n (%) | Mean Burden Score | Mean Word Count | OP With Low Burden, n (%) | OP With Intermediate Burden, n (%) | OP With High Burden, n (%) | IP With Low Burden, n (%) | IP With Intermediate Burden, n (%) | IP With High Burden, n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Logistics | 64 (52%) | 48 (56%) | 16 (43%) | 2.89 | 43 | 30 (63%) | 2 (4%) | 16 (33%) | 2 (13%) | 2 (13%) | 12 (75%) |
| Life disruption | 54 (44%) | 32 (37%) | 22 (59%) | 3.20 | 50 | 18 (56%) | 2 (6%) | 12 (38%) | 4 (18%) | 1 (5%) | 17 (77%) |
| Care delivery system | 46 (37%) | 33 (38%) | 13 (35%) | 2.67 | 35 | 25 (76%) | 1 (3%) | 7 (21%) | 1 (8%) | 1 (8%) | 11 (85%) |
| Parking | 37 (30%) | 21 (24%) | 16 (43%) | 2.86 | 38 | 16 (76%) | 1 (5%) | 4 (19%) | 1 (6%) | 2 (13%) | 13 (81%) |
| Financial burden | 32 (26%) | 20 (23%) | 12 (32%) | 3.09 | 49 | 12 (60%) | 1 (5%) | 7 (35%) | 2 (17%) | 0 (0%) | 10 (83%) |
| Emotional burden | 26 (21%) | 16 (19%) | 10 (27%) | 3.42 | 54 | 8 (50%) | 0 (0%) | 8 (50%) | 1 (10%) | 0 (0%) | 9 (90%) |
Total number of analyzed comments = 123; OP comments = 86; IP comments = 37.
Low burden = 1–2, intermediate burden = 3, high burden = 4–5; on 5-point Likert scale.
IP, inpatient, OP, outpatient.
Differences in inpatient versus outpatient experience were most notable in the theme categories of logistical and parking burden: for inpatient families, parking was mentioned by a greater proportion of families and more frequently invoked anger and a sense of limitation imposed by parking. For outpatient families, parking was more often an inconvenience requiring extra logistical steps. Similarly, in outpatient respondents the logistics of reaching clinic were more often related to transportation, whereas for inpatient families logistical concerns tied into balancing other aspects of family life.
Thematic Findings
We identified 6 thematic categories in caregivers’ responses, then analyzed subthemes and factors associated with high and low self-rated burden within these categories. In order of frequency, the 6 thematic categories were logistics, life disruption, the care delivery system, parking, financial burden, and emotional burden, with subcategories as shown in Figure 1.
Figure 1.
Theme categories and subcategories.
Logistics
Families who reported a high-burden score (4–5 out of 5) and invoked logistical concerns frequently brought up the difficulty of simultaneously managing medical and home life, and often identified specific logistical issues that led to burden. Many high-burden respondents sounded an overwhelmed note: “It is a lot to have a patient here and a family and home to take care of elsewhere,” one wrote. Others agreed: “It is hard having … to make arrangements [for the other children];” and “It is hard to balance.” Some caregivers voiced their angst by enumerating the many hurdles associated with just one visit:
“My son misses school every time he has an appointment. He misses a lot of learning from school. Every appointment my son has I have to bring his sister with us. Our lives have changed ever since. When we/my son has a long day at the clinic, I have to rush home and cook and pay attention to my other two children. … It’s been hard on our lives, every time my son has an appointment we are in a hurry the entire day.”
Travel, family scheduling, and time cost featured heavily in these comments.
By contrast, comments about logistical concerns associated with overall low self-rated burden (1–2 out of 5) were more likely to describe solutions to the logistical challenges and focus solely on transportation. One low-burden respondent noted: “It was harder when I didn’t have a vehicle.” Another concluded: “Traffic [is] always horrible, but we seem to manage.” In these comments, although logistics presented challenges, they are mentioned in context of a solution or accommodation.
Life Disruption
Unresolved home-medical tension also contributed to the second-most invoked thematic category, life disruption. High-burden responses from inpatient families often touched on the anguish of separating one caretaker and child from the rest of the family. One respondent described: “Emotionally it is hard because it separates my son and whichever of us is here with him from the rest of our family because all five of us can’t be here at once.” High-burden outpatient families were more likely to describe disruption in terms of both organizational and emotional strain:
“A lot of preparation is required, and the stress on the patient and our family is great. We have four children and the collective stress on visit day 5 is damaging to the family dynamic. We accept this in stride as part of the situation and try to adjust. We do not [complain] because [this is] not about us; this is about our son and his treatment. I am [close] to losing my job over visits but we will figure it out. We have to.”
Siblings’ and parents’ ties are fractured in these families experiencing high burden and life disruption — caregivers are isolated from each other and their other children, stretched thin to maintain a semblance of family life.
As compared to respondents with these emotionally fraught, unresolved disruptions, respondents who cited life-disrupting burden but rated their overall burden as low were more likely to have working solutions to the disruption and more likely to cite institutional or support network assistance. “My [employer] is working with me while I am here, to schedule … around my schedule,” explained one caregiver. Another described the largest disruptions, “paying for parking and not sleeping in my own bed,” were mitigated because “luckily his grandfather came to relieve me the other day so I could go home and shower and get a change of clothes.”
These families with low burden more often referenced how they were able to patch the disruptions associated with their child’s care.
Care Delivery System
Commentary on aspects of hospital-adjacent life comprised the third-largest theme category, the care delivery system. High-burden respondents who found the care delivery system to be burdensome often linked this to care coordination and hospital amenities; however, many acknowledged the need for the system despite inefficiencies. “Clinic visits are not preventable, this is where we get chemo,” one wrote, “however, the length of time spent here could be [shortened] if the clinic was more efficient.” The frustration with perceived inefficiencies rarely outweighed the importance of the visit for commenters. As an intermediate-burden respondent explained, “We feel that the trip is time well spent, if it results in her getting the treatment she needs.” These caregivers pointed out both broad and specific ways that they felt the health care system was creating burden for their families.
Low-burden respondents commenting on the care delivery system were less likely to invoke specific complaints, citing smaller logistical items rather than larger coordination concerns. One caregiver exclaimed: “[The hospital] is doing an awesome job!! [However], we can’t wait for [closer location] to be open.” The overall tone of these low-burden comments was appreciative. As one respondent noted, “It will always be painful to have a child diagnosed with leukemia. … Of course I am grateful for everything that you do for her and all of the children.” These comments about the care delivery system, in contrast to comments from high-burden families, were more limited in scope and frustration.
Parking
One specific feature of the clinical encounter prompted many comments and much consternation, parking. Burden associated with parking inspired frank outrage from caregivers with both high and low self-rated burden. Many caregivers who rated their burden in the high categories framed their resentment of parking burden in terms of other burdens of care. One wrote, “The parking is outrageous. We already have to pay for medical bills and are trying to take care of our sick child … and then we have to pay for parking on top of all of that. It is a lot.” Another respondent explained the limitations posed by parking burden, describing it as “major, [unfair], very expensive[,] limiting freedom to come and go [and be visited by] family and friends.” Still other high-burden respondents wrote, “The parking is outrageous;” “The cost of parking is outrageous;” and “The parking rates are extremely [high] and take advantage of long-term patients.”
Respondents who mentioned parking but rated their overall burden as low were equally likely to mention outrage and cost but were less likely to describe logistical limitation imposed by parking or frame parking in terms of an overwhelming list of burdens. “Parking is expensive for us, especially because I have to miss work for [appointments],” one caregiver wrote. An intermediate-burden respondent noted, “Parking is very expensive, so I don’t even park here, I have people drop me off.”
Financial Burden
As alluded to in comments about parking, financial burdens comprised a fifth theme category. Financial considerations often were associated with high overall burden when they influenced families’ long-term economic stability. For many, these financial burdens were devastating. One caregiver described:
“Gas money and [other] costs while I am here has drained my savings and is taking money for household bills. Extra food costs [are] financially [draining] as well. I have had to put off or make alternate arrangements for bills, borrow [money] from family members, etc. The [money] that I had in savings was to buy a house (down payment) for my children so they would be safer than living in the federal housing unit we currently live in. I had almost reached my goal amount when my son was diagnosed.”
Financial burdens also could stretch families and caregivers to a breaking point. “Unless you plan to quit your job and go on public assistance there is no help for families,” a caregiver noted, “we are harassed by billing constantly. … It’s not right to make families choose between financial ruin and their child’s life.” This threat to financial stability also frequently affected respondents’ employment: “I have never been made full time at my job of [>15 years] because of her condition, since I have to leave unexpectedly and spend weeks in the hospital.” Caregivers with high overall burden and financial concerns fretted over how disastrous the long-term financial implications of care could be.
When financial burdens were associated with lower overall burden, they were more often invoked in the terms of manageable losses or finite costs. “We have lost things that money can get back,” one low-burden respondent wrote, “so we are starting again.”
Emotional Burden
Emotional burden made up the final theme category. Stress and unrest were common themes described by high-burden respondents who discussed emotional burden. “It is devastating,” one caregiver wrote, “it causes a lot of emotional turmoil amongst the family. It is very unrestful. Can’t get any rest here.” Another comment exemplified the way that emotional burden amplifies the other aspects of burden: “[It is] hard to arrange all [the] visits, hard to afford all of the costs, but harder on our hearts and souls. To live with this disease is the [hardest] thing on everyone!” These laments tied emotional exhaustion to their sense of high overall burden.
Among comments about emotional burden of care, low overall burden was associated with contextualization of comparative burden and invocation of faith. One caregiver with low self-rated burden framed their emotional struggle in terms of other caregivers’ experiences: “It is painful to have a child in this condition, the same as everyone else feels, psychologically.” Another framed their strife in terms of faith: “God is good and only He knows why these things happen, but you must learn to trust the [savior].” These comments expressed an attempt to sublimate emotional burden into faith or understanding.
DISCUSSION
The results of our study demonstrate that cancer care imposes numerous burdens on families that impart varying degrees of distress. Understanding which stressors correlate with the greatest perceived burden may help identify opportunities for efficient intervention.
Inpatient and Outpatient Findings
Previous research in this population demonstrates that financial burden increases with increasing treatment complexity and days of care at specialty referral centers.5 Accordingly, in our study population, inpatient caregivers reported higher overall burden and were more likely to invoke financial and emotional burdens of care. The heightened emotional burden and prevalence of logistical and parking concerns demonstrate the need for unique assistance programs targeted at supporting families during this phase of care.
Thematic Findings
Logistics
Previous qualitative studies of direct costs incurred in pediatric cancer treatment describe travel and food costs as most common.18 Our results confirm that these logistical concerns, which make up a large portion of the economic burden, translate to how caregivers perceive burden. Further, our analysis shows that the highest overall burden associated with logistical concerns involved a sense of having no avenue for resolving difficulties or inability to juggle medical and nonmedical life. These findings indicate a need to focus logistical resources on providing family caregivers with resources for coordinating patients’ care with sibling and family life. The mitigating effect of logistical workarounds on burden may point to the value of connecting caregivers with each other to share logistical solutions.
Life Disruption
The tension between home and medical life also featured heavily in the life disruption theme category. Previous literature describes significant unmet sibling needs in some pediatric oncology subpopulations19 and major strain on parents’ relationship during pediatric cancer treatment.20 Our findings expand and specify prior findings in that high-burden respondents in the inpatient setting were more likely to describe disruption in terms of both caregiver-family and patient-family disruption, whereas in the outpatient setting disruption was more often described in terms of organizational difficulty. Interventions in inpatient populations, then, should be aimed toward the physical and emotional distance between family members imposed by hospitalization, whereas outpatient-oriented interventions may focus more on logistical disruptions of family life such as addressing sibling care and home/work responsibilities.
Care Delivery System
Caregiver frustration or burden associated with the care delivery system has not been specifically studied in the pediatric oncology cost-assessment sphere. However, data suggest that a family-centered care approach may improve parental satisfaction.21 Our data show that burden associated with the care delivery system centered around perceived inefficiency, hospital amenities, and care coordination. To ameliorate these burdens, clinics may consider improving coordination or communication surrounding clinic processes.
Parking
Parking was overrepresented in caregivers’ descriptions of care burden relative to its portion of absolute costs in the same study population. In particular, parking was associated with the highest overall burden when commenters felt that parking limited family mobility. As such, efforts to reduce parking burden may be most efficient by reducing parking reentry costs. Given the outsize effect that parking appears to have on overall perception of burden, these efforts to reduce parking burden may present a unique opportunity to reduce caregiver burden by providing discounted parking or supportive funding for caregivers who return frequently. This issue, while it is specific to centers in which patient families must pay for parking, represented an outsized subjective burden for patient families in our center.
Financial Burden
Existing literature firmly ties financial toxicity with health-related quality of life for cancer patients.1 In our data set, financial burdens were associated with the highest overall burden when they contributed to long-term financial destabilization of the family and associated with lower burden when associated with specific and recoverable losses. Programs addressing this facet of caregiver burden, then, may be most effective by preemptively informing families of cost and working with employers and insurers to help caregivers plan for their child’s illness.
Emotional Burden
Our study describes emotional elements associated with high overall burden, weariness and stress. By contrast, emotional elements associated with low overall burden, faith and comparative burden, may indicate goals for emotional counseling of caregivers. The association between low self-rated burden and acknowledgement of comparative burden may indicate an opportunity for hospitals to improve not just logistical but also emotional burden by connecting caregivers with one another during the treatment process.
Limitations
Limitations of this study include institutional and regionally specific factors. While our study population listed parking as disproportionate source burden relative to its cost, for example, patients at other centers may not experience the same parking costs and burden. Further, these specific experiences reflect a group of caregivers at a large academic tertiary care center and may not be applicable to populations at smaller centers, without further research. Lastly, these data are limited in sample size and context within length of stay or visits per week because we did not specifically ask families to rate the individual contribution of each stressor to their overall perception of burden but rather examined the association between these independently assessed measures.
Future research should focus on understanding these established theme categories as they contribute to burden in other pediatric hematology/oncology care centers, further quantifying the relative contribution of each individual type of stressor, and assessing for variation in these themes by caregiver factors, such as support network, number of other children at home, gender, ethnicity, and income, as well as care-related factors like length of stay and outpatient visits per week.
CONCLUSIONS
Pediatric hematology/oncology care generates burdens for families that extend beyond cost. The data obtained in this study establishes 6 themes for future study of caregiver-perceived burden in pediatric hematologic/oncologic encounters, demonstrates that certain components of cost contribute disproportionately to caregivers’ overall sense of care-related burden, and finds areas within each of 6 categories that can be best targeted to alleviate caregiver burden. By identifying which areas of cost and instability generate the greatest burden for families, pediatric hematology/oncology centers may better plan programing to mitigate cancer care burden and newly diagnosed patients’ families may better understand and plan for the stressors they will face during care.
Patient-Friendly Recap.
Families whose children have cancer or serious blood diseases face stress due to the logistics, life disruption, health care delivery, parking, financial burden, and emotional burden associated with care.
Some stressors, such as parking or logistics, may contribute disproportionately to families’ stress relative to how much they cost.
These areas are opportunities for hospital systems to improve patients’ and families’ experiences more efficiently than funds directed at other less stressful or more costly areas of patient care.
Footnotes
Author Contributions
Study design: Russell, Hellsten. Data acquisition or analysis: all authors. Manuscript drafting: Abrams. Critical revision: Russell, Hellsten.
Conflicts of Interest
None.
References
- 1.de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST) Cancer. 2017;123:476–84. doi: 10.1002/cncr.30369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34:980–6. doi: 10.1200/JCO.2015.64.6620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State,1980–1997. Pediatrics. 2000;106:205–9. [PubMed] [Google Scholar]
- 4.Berry JG, Hall M, Hall DE, et al. Inpatient growth and resource use in 28 children’s hospitals: a longitudinal, multi-institutional study. JAMA Pediatr. 2013;167:170–7. doi: 10.1001/jamapediatrics.2013.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pagano E, Baldi I, Mosso ML, et al. The economic burden of caregiving on families of children and adolescents with cancer: a population-based assessment. Pediatr Blood Cancer. 2014;61:1088–93. doi: 10.1002/pbc.24904. [DOI] [PubMed] [Google Scholar]
- 6.Warner EL, Kirchhoff AC, Nam GE, Fluchel M. Financial burden of pediatric cancer for patients and their families. J Oncol Pract. 2015;11:12–8. doi: 10.1200/JOP.2014.001495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russell H, Leeds H, Abrams H, Jones A, Huynh J, Hellsten M. 2018. Estimating population level family costs of an outpatient encounter. (abstr.) Pediatr Blood Cancer. 2017;64(S1):S68. doi: 10.1002/pbc.26591. [DOI] [Google Scholar]
- 8.Long K, Sudha S, Mutran EJ. Elder-proxy agreement concerning the functional status and medical history of the older person: the impact of caregiver burden and depressive symptomatology. J Am Geriatr Soc. 1998;46:1103–11. doi: 10.1111/j.1532-5415.1998.tb06648.x. [DOI] [PubMed] [Google Scholar]
- 9.Pelletier W, Hinds PS, Alderfer MA, Fairclough DL, Stegenga K, Pentz RD. Themes reported by families as important when proceeding with pediatric hematopoietic stem cell transplantation. Pediatr Blood Cancer. 2014;61:1625–31. doi: 10.1002/pbc.25075. [DOI] [PubMed] [Google Scholar]
- 10.Lapid MI, Atherton PJ, Kung S, et al. Cancer caregiver quality of life: need for targeted intervention. Psychooncology. 2016;25:1400–7. doi: 10.1002/pon.3960. [DOI] [PubMed] [Google Scholar]
- 11.Litzelman K, Barker E, Catrine K, Puccetti D, Possin P, Witt WP. Socioeconomic disparities in the quality of life in children with cancer or brain tumors: the mediating role of family factors. Psychooncology. 2013;22:1081–8. doi: 10.1002/pon.3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsimicalis A, Stevens B, Ungar WJ, McKeever P, Greenberg M. The cost of childhood cancer from the family’s perspective: a critical review. Pediatr Blood Cancer. 2011;56:707–17. doi: 10.1002/pbc.22685. [DOI] [PubMed] [Google Scholar]
- 13.Allshouse C, Comeau M, Rodgers R, Wells N. Families of children with medical complexity: a view from the front lines. Pediatrics. 2018;141(Suppl 3):S195–S201. doi: 10.1542/peds.2017-1284D. [DOI] [PubMed] [Google Scholar]
- 14.Datz H, Tumin D, Miller R, Smith TP, Bhalla T, Tobias JD. Pediatric chronic pain and caregiver burden in a national survey. Scand J Pain. 2019;19:109–16. doi: 10.1515/sjpain-2018-0121. [DOI] [PubMed] [Google Scholar]
- 15.Smith LR, Fisher JD, Cunningham CO, Amico KR. Understanding the behavioral determinants of retention in HIV care: a qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDS. 2012;26:344–55. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 17.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 15:1277–88. doi: 10.1177/1049732305276687. 200. [DOI] [PubMed] [Google Scholar]
- 18.Tsimicalis A, Stevens B, Ungar WJ, et al. A mixed method approach to describe the out-of-pocket expenses incurred by families of children with cancer. Pediatr Blood Cancer. 2013;60:438–45. doi: 10.1002/pbc.24324. [DOI] [PubMed] [Google Scholar]
- 19.White TE, Hendershot KA, Dixon MD, et al. Family strategies to support siblings of pediatric hematopoietic stem cell transplant patients. Pediatrics. 2017;139(2):e20161057. doi: 10.1542/peds.2016-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiener L, Battles H, Zadeh S, Pelletier W, Arruda-Colli MNF, Muriel AC. The perceived influence of childhood cancer on the parents’ relationship. Psychooncology. 2017;26:2109–17. doi: 10.1002/pon.4313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shields L, Zhou H, Pratt J, Taylor M, Hunter J, Pascoe E. Family-centered care for hospitalized children aged 0–12 years. Cochrane Database Syst Rev. 2012;10:CD004811. doi: 10.1002/14651858.CD004811.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]