Abstract
Purpose:
Exposures to favorable environments in childhood, including those in schools, are associated with healthy habits among children. In this study, we developed a series of indices aimed at measuring students’ exposure to different dimensions of the school food and physical activity (PA) environment. We implemented these indices to investigate how different aspects of the school food and PA environment changed over time and examined their correspondence with known changes in relevant policies and programs.
Methods:
All public schools (n= 141) in four school districts in New Jersey provided detailed food and PA environment data for each school year from 2010–11 to 2015–16. Seven food environment indices, three PA environment indices, and two additional indices that capture health-promoting initiatives at the school-level and at the state or federal level were developed.
Results:
While the school PA environment largely remained unchanged, several dimensions of the school food environment changed between 2010 and 2015. Overall, the number of healthy items increased over time in vending machines (p<.001), a la carte (p<.05), or through reimbursable school lunches (p<.001); decreases in number of unhealthy items were only detected in school lunches (p<.05). For most food indices, both the number of items offered and the trend over time varied across school levels.
Conclusions:
Schools are a key venue for implementing policy and environment interventions aimed to promote healthy behaviors. Indices developed from easy-to-use survey questions captured multiple dimensions of the school food and PA environments and were sensitive to policy changes over time.
INTRODUCTION
Exposure to environments that promote healthy eating and physical activity (PA) can contribute to healthful dietary patterns and PA behaviors among school children [1,2]. With most 5–18 year olds spending a considerable part of their day—and consuming up to 58% of their daily calories [3]—in school, it is not surprising that the school food environment is associated with children’s food purchasing and dietary patterns [4–6], as well as weight status [7]. In addition, the PA environment in school, whether related to physical education (PE), intra and extramural sports, recess, or other unstructured PA during and outside of school hours [8,9], plays an important role in contributing to the 60 minutes per day of moderate-to-vigorous PA recommended for youth [10,11]. Recognizing the roles schools can play, over the last decade, a number of policies and programs aimed at improving food and PA behaviors among youth have focused on schools as a means to reach a considerable share of their target population.
Food-related policies and programs
One of the most significant vehicles for change in the school food environment was the Healthy Hunger Free Kids Act (HHFKA) of 2010 that required the United States Department of Agriculture (USDA) to update guidelines for foods offered as part of reimbursable school meals and as competitive foods [12]. In this first major update to school meal requirements since 1995, starting in school year (SY) 2012–2013, HHFKA required the National School Lunch Program (NSLP) to incrementally expand the offering of healthy foods, with more whole grains and a larger amount and greater variety of fruits and vegetables, while limiting fat, sugars, and sodium [13]. Similar guidelines were mandated for the School Breakfast Program (SBP) and were implemented in SY 2013–2014. Smart Snacks in Schools, the most recently implemented HHFKA school food policy (SY 2014–2015), specifically addresses the nutritional quality of all foods and beverages outside of reimbursable school meals, which includes all items sold a la carte, in vending machines, school stores, or through fundraising events [14]. Other policies and programs, less pervasive in reach, also aimed to improve the school food environment. For instance, the USDA’s Team Nutrition program offers technical assistance to schools to provide healthy meals to students [15]; various Farm to School Programs encourage schools to purchase and provide locally grown food as part of reimbursable school meals [16]; the USDA’s Fresh Fruit and Vegetable Program offers a fresh fruit or vegetable as a snack outside the school meal programs to elementary school children [17]; and the Alliance for a Healthier Generation provides technical assistance and resources for schools to implement school wellness policies and improve the food and PA environments [18].
PA-related policies and programs
Similarly, a number of policies and programs have been implemented to create opportunities for school-age youth to increase their PA levels. Of the 39 states with laws requiring PE in elementary schools, 19 states, including New Jersey, specify a minimum amount of active participation time [19]. The highly publicized “Let’s Move!” initiative, launched in 2009, uses public-private partnerships and collaborations among leading health, education, and private sector organizations to promote healthy lifestyle behaviors, and encourages PA participation among youth by providing specific recommendations for schools and communities [20]. The Safe Routes to School (SRTS) program, which is eligible to compete for federal funding [21], also promotes PA among youth, with the specific goal of creating a safe environment around schools so students can actively commute to school.
The current study
Robust measures to capture the school’s food and PA environments are needed to track changes over time, to assess the impact of school-focused policies and programs, and assess the impact of changes in the environment on children’s wellbeing. Based on established survey questions [22–25], this study developed a series of indices to measure different dimensions of food and PA environments in schools. Using these newly developed measures, we examined whether and to what extent different aspects of school food and PA environments changed over time. Because various policies and programs can affect students in different grade levels differentially, we also explored whether such changes differed among elementary (or primary) versus middle and high (hereafter secondary) schools. We monitored the trends in these indices over a six-year period in a sample of 141 New Jersey public schools from four districts serving largely minority students from lower income households. Finally, we examined whether the observed trends corresponded with key changes in relevant policies and programs over the same time period.
METHODS
Dataset
As part of the New Jersey Child Health Study, a 96 item survey was developed, using questions from previous research [22–25], to capture information on specific aspects of food and PA environments in schools. We selected items that measured aspects of the environment with the potential to affect obesogenic behaviors among students. Data on food offerings, PA opportunities, and health promoting policies and practices were collected on two separate occasions, during SY 2012–13 and 2015–16. Each administration of the survey applied the questions to the current and the two preceding school years. Thus, we collected data for each SY from 2010–11 to 2015–16. For simplicity, throughout the text we will refer to SY 2010–11 as 2010, SY 2011–12 as 2011, and so on. Surveys were distributed to all public schools that included any grade from K to 12 in all four districts in our study cities (Camden, Newark, New Brunswick, and Trenton). The four cities were initially targeted by the Robert Wood Johnson Foundation for investment in policy, systems, and environmental approaches to combat childhood obesity. As such, they are apt settings for documenting changes in the environment and studying the impact of those changes on weight status over time. Surveys were distributed through school nurses, who were asked to draw upon their own knowledge as well as consult with school food and physical education staff to complete specific sections. In-service training and instructions for completing data collection were provided by study staff, coordinated by nursing divisions within each district. To ensure a high response rate, nurses were given a $50 incentive upon completion of the survey. The response rate averaged 92.5% across the four districts, ranging from 89.8% in Newark to 100% in New Brunswick. Overall, we collected data on 141 schools—93 primary schools and 48 secondary schools. The largest district was Newark, where 71 schools were located, followed by Camden, Trenton, and New Brunswick, with 29, 27, and 14 schools, respectively. Of the 141 schools included in our study, 96 were surveyed at both data collection points, 31 were surveyed only during the first round of data collection and 14 during only the second round. The major reasons for the lack of overlap across the two data collection periods included non-participation (17) and schools that existed only during one of the two time periods (28). Table 1 reports the number of schools sampled, by district and grade-level, and other descriptive statistics.
Table 1.
Description of Schools Included in the Sample (2010–2015)
| Variable | Elementary | Secondary | Total |
|---|---|---|---|
| Average Enrollment | 515 | 722 | 582 |
| Free/Reduced Lunch | 86.6% | 78.5% | 83.9% |
| Race/Ethnicity | |||
| Hispanic | 48.7 % | 38.6 % | 45.4 % |
| African American | 46.6% | 55.2% | 49.4% |
| White | 3.6% | 5.3% | 4.2% |
| Other | 1.0% | 0.9% | 1.0% |
| City (number of schools) | |||
| Camden | 18 | 11 | 29 |
| Newark | 51 | 20 | 71 |
| New Brunswick | 9 | 5 | 14 |
| Trenton | 15 | 12 | 27 |
|
N |
93 |
48 |
141 |
The format and content of the questionnaire were field tested with school administrators and modified to ensure clarity and ease of completion. In its final form, the survey had three main content sections addressing (1) nutrition at school, (2) physical activity at school, and (3) school level practices and program participation. Examples of questions, their response options, and sources are provided in Supplementary Table S1. For the nutrition section (completed in consultation with food service staff), respondents were asked to provide information for each year on foods offered as part of reimbursable school lunches, a la carte during lunch time, and in vending machines. In the section on PA at school (completed in consultation with PE staff), questions assessed frequency of recess in elementary schools (3rd grade used as indicator grade); frequency of PE classes (3rd, 7th, and 10th grades used as indicator grades); activity breaks; intramural, extramural, nontraditional sports; and before and after-school activities. Respondents reported on the availability of various PA facilities and their accessibility to the community for non-school sponsored activities. Under school level practices, respondents were asked about the presence of free water in the cafeteria, a full service kitchen, a school garden, as well as the school’s participation in federal or state level programs, such as Safe Routes to School (SRTS), USDA’s Team Nutrition, and others. Surveys were made available in a paper format as well as online using Qualtrics© (Provo, UT). The Institutional Review Boards of Arizona State University and Rutgers University approved study protocols.
Index Development
Coinciding with the three main sections of the survey, we developed 12 indices; seven on the school food environment, three on the PA environment, and two on health-promoting initiatives. Each index is the sum of a battery of N conceptually related items, previously used in similar investigations [22–25], with items present in schools counting as 1, and items not present in schools counting as 0. Thus, each index can assume any integer value from 0 to N, with N varying from 3 to 12 across indices. Table 2 lists the specific items included in each index. School food environment is measured through seven indices: NSLP – Healthy (0–9); NSLP – Unhealthy (0–4); Vending Machines – Healthy (0–4); Vending Machines – Unhealthy (0–9); Availability of Vending machines (0–3); A la Carte – Healthy (0–9); A la Carte – Unhealthy (0–12). The numbers reported in parentheses represent the range of possible index scores. School PA environment is measured through three indices: Indoor Facilities (0–4); Outdoor Facilities (0–6); PA Opportunities (0–7). Lastly, we created two additional indices aimed at measuring policies and initiatives that can impact either the school food or the school PA environment: School-level Health Promotion Initiatives (08); Federal and State-level Health Promotion Programs (0–5).
Table 2.
List of item included in indices capturing food and physical activity environments in K-12 schools List of indices and items included.
| Food Environment Indices | |
|---|---|
| Index name and score range | Items included |
| National School Lunch Program (NSLP) Healthy (0–9) | At least Half Whole Grains |
| Whole Grains | |
| Variety of Vegetables | |
| Modified Pizza | |
| Fat free / 1% Milk | |
| Fat free Flavored Milk | |
| Fresh Fruit | |
| Raw Vegetables | |
| Salad Bar | |
| National School Lunch Program (NSLP) Unhealthy (0–5) | Fries |
| Pizza | |
| Dessert | |
| Full fat / 2% Milk | |
| Full / 1% Flavored Milk | |
| Availability of vending machines (0–3) | Before and after school |
| During school but not during lunch | |
| During lunch time | |
| Vending Machine Healthy (0–4) | Bottled Water |
| 100% Juice | |
| Fat free / 1% Unflavored Milk | |
| Fat-free Flavored Milk | |
| Vending Machine Unhealthy (0–9) | Juice Drink |
| Diet Soda | |
| Soda | |
| Energy or Sports Drinks | |
| Full fat / 2% Unflavored Milk | |
| Full fat / 2% / 1% Flavored Milk | |
| Salty snacks | |
| Cookies, cakes | |
| Candy | |
| A La Carte Healthy (0–9) | Bottled Water |
| 100% Juice | |
| Fat free / 1% Unflavored Milk | |
| Fat-free Flavored Milk | |
| Dairy Foods, Lower in Fat | |
| Raw FV | |
| Salad Bar | |
| Sandwiches | |
| Pizza - Healthier | |
| A La Carte Unhealthy (0–12) | Juice Drinks |
| Diet Soda | |
| Soda | |
| Energy or Sports Drinks | |
| Full fat / 2% Unflavored Milk | |
| Full fat / 2% / 1% Flavored Milk | |
| Salty Snacks | |
| Fried Potatoes | |
| Pizza | |
| Cookies, Cakes | |
| Frozen Desserts | |
| Candy | |
|
Physical Activity (PA) Indices | |
| Index name and range | Items included |
| Indoor Facilities (0–4) | Gymnasium |
| Indoor Pool | |
| Weight room | |
| Other (Cafeteria, auditorium, etc…) | |
| Outdoor Facilities (0–6) | Playground equipment |
| Track | |
| Sports courts | |
| Baseball/softball fields | |
| General | |
| Parking lot | |
| PA Opportunities (0–6) | Intramural sports |
| Extramural sports | |
| Non-competitive, school-sponsored | |
| Non-traditional PE activities | |
| Recess (for 3rd grade) | |
| Physical Education (0=0,1 days; 1=2+ days) | |
|
Health Promotion Initiatives and Programs | |
| Index name and range | Items included |
| School-level health promotion initiatives (0–8) | Health/Wellness advisory council |
| Free water in cafeteria | |
| Full service kitchen | |
| Garden | |
| BMI (Body Mass Index) shared with parents | |
| School breakfast promotion program | |
| Indoor facilities made available during non-school hours | |
| Outdoor facilities made available during non-school hours | |
| Federal- and state-level health promotion programs (0–5) | Team Nutrition |
| Farm to School | |
| FFVP (Fresh Fruit and Vegetable Program) | |
| Alliance for a healthier generation | |
| Safe routes to school (Program participation) | |
Indices measure the level of exposure to different aspects of school food and PA environments (i.e. exposure to food options; physical activity opportunities; programs and policies), with lower scores indicative of lower exposure. In some instances, for example Vending Machine – Unhealthy, a score of 0 may indicate that school vending machines did not offer any of the surveyed items, or that the school did not have any vending machines at all. For our purposes, these two situations are considered equivalent, as both indicate that students were not exposed to this set of unhealthy items in vending machines.
Statistical Analysis
All analyses were conducted in Stata 15. Missing survey items among completed surveys were dealt with through multiple imputations based on a chained equations procedure [26]. Extent of missing data varied between 0 and 18% for most variables within each survey. Following recommended practices from previous research [27,28], we created a set of 50 imputed datasets. Exploratory analyses showed that a larger number of imputed datasets did not correspond to any further improvement, as both the point estimates and standard errors were unaltered. Models were run on each single imputed dataset and then combined by using Rubin’s combination rule [29], which accounts for the variability within and across datasets. Growth curve models taking into account multiple observations for each school and nesting of schools within districts were used to analyze the trend of each index over time. We built two sets of models that are equivalent in all aspects but one— how we operationalized time. First, we treated time as a continuous variable to obtain the overall linear trend over the 6-year period under investigation. This set of models included an interaction term between time and school level to formally test whether the linear trend of the indices differed across school level. Then, we treated time as a categorical variable, which allowed us to obtain the adjusted mean of the index for each single year (2010–2015). We did so by using the margins command [30], which calculates the predicted mean of the outcome variable (i.e., the index), while controlling for all covariates, which are fixed at their mean values over the 6-year period. Each model adjusted for school level (elementary vs secondary school), total number of students enrolled, proportion of students eligible for free or reduced price meals, and proportion of students with different race/ethnicity and whether the school was included in both rounds of data collection. School demographics were drawn from the National Center for Education Statistics (NCES) common core data repository [31]. To test whether our results were robust and not driven by the unbalance in the sample, we ran sensitivity analyses restricting the sample to the 96 schools for which we have data at all 6 time points. Our results were entirely consistent1.
RESULTS
Table 3 displays the results from multivariate regression and shows the predicted mean values of the indices for each year between 2000 and 2015, along with the linear trends for all schools combined and by school level. Overall, the linear trends reveal that while no significant change occurred in the PA environment over the six years, several aspects of the food environment showed significant changes. Over the study period, schools expanded their offerings of healthy items, with an increase in NSLP, a la carte, and vending machine items. Concurrently, schools also increased their offerings of unhealthy a la carte items and made vending machines more available to students. Lastly, between 2010 and 2015, the number of school-level health promotion initiatives was stable, whereas the average number of federal- and state-level health promotion programs significantly declined from 1.66 in 2010 to 1.17 in 2015.
Table 3.
Adjusted Mean Scores for School Food and Physical Activity Environment Indices by Year and Summary Statistics for Linear Trends.
| Indices | Adjusted means - All schools | Linear trend | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Food Environment | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | All schools | Primary | Secondary | Difference |
| NSLPa – Healthy | 6.50 | 6.77 | 6.84 | 7.40 | 7.29 | 7.33 | 0.18*** | 0.19*** | 0.15* | NS |
| NSLPa – Unhealthy | 3.47 | 3.35 | 3.29 | 3.31 | 3.19 | 3.13 | −0.06* | −0.05 | −0.09^ | NS |
| A La Carte – Healthy | 2.56 | 3.05 | 3.13 | 3.27 | 3.30 | 3.33 | 0.15* | 0.07 | 0.30** | ^ |
| A La Carte – Unhealthy | 2.19 | 2.68 | 2.58 | 2.56 | 2.72 | 2.71 | 0.09^ | -0.04 | 0.33*** | ** |
| Vending Machine – Healthy | 0.46 | 0.53 | 0.49 | 0.79 | 0.77 | 0.87 | 0.08*** | 0.10*** | 0.04 | NS |
| Vending Machine – Unhealthy | 0.82 | 0.84 | 0.74 | 1.24 | 1.11 | 0.70 | 0.01 | 0.12** | −0.19** | *** |
| Presence of Vending Machines | 0.60 | 0.63 | 0.62 | 0.88 | 0.88 | 0.90 | 0.07** | 0.12*** | −0.03 | *** |
| Physical Activity (PA) Environment | ||||||||||
| Indoor Facilities | 1.97 | 1.95 | 2.00 | 2.00 | 1.94 | 1.97 | 0.00 | -0.01 | 0.01 | NS |
| Outdoor Facilities | 2.81 | 2.67 | 2.67 | 2.78 | 2.80 | 2.89 | 0.02 | 0.05 | 0.04 | NS |
| PA Opportunities | 3.24 | 3.37 | 3.43 | 3.22 | 3.44 | 3.48 | 0.04 | 0.08^ | −0.05 | ^ |
| Additional Indices | ||||||||||
| School-level health promotion initiatives | 4.57 | 4.75 | 4.60 | 4.38 | 4.50 | 4.52 | −0.03 | −0.01 | −0.07 | NS |
| Federal- and state-level health promotion programs |
1.66 |
1.56 |
1.51 |
1.37 |
1.24 |
1.17 |
−0.10** |
−0.15*** |
−0.00 |
* |
| Total number of observations (N) | 127 | 127 | 127 | 110 | 110 | 110 | 711 | 480 | 231 | |
p<0.10
p<0.05
p<0.01
p<0.001
NSLP: National School Lunch Program
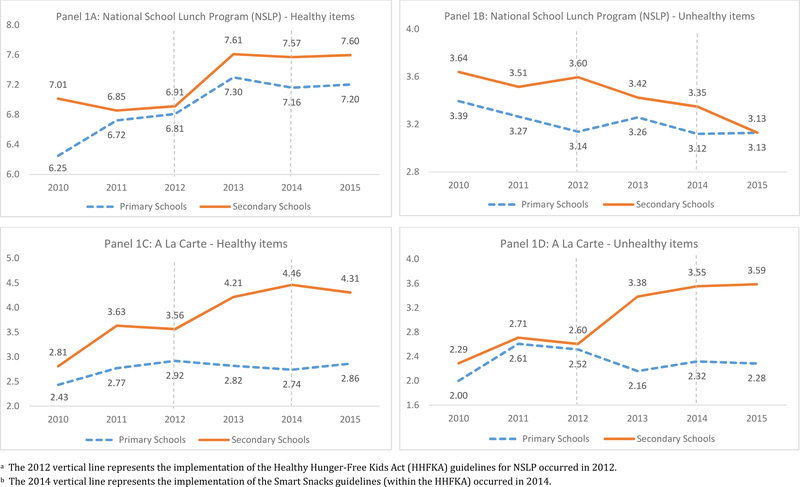
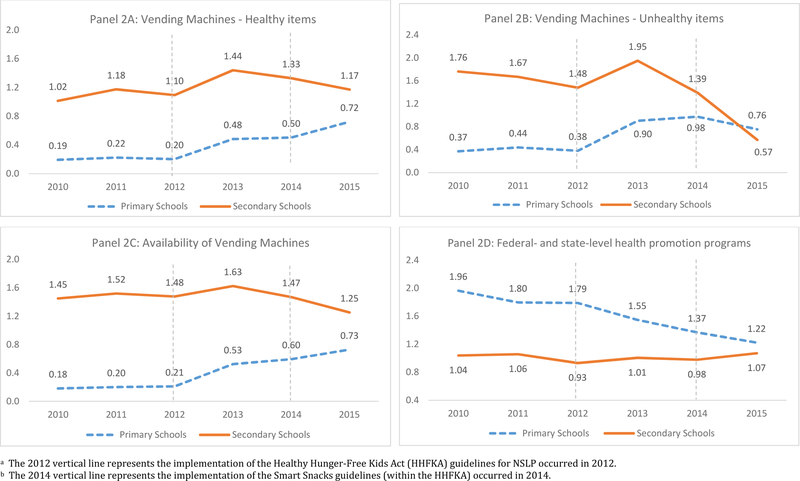
Our analysis also reveals that some of the changes over the study period were different across school level. For instance, while the trend in NSLP healthy and unhealthy items were similar for primary and secondary schools (Figure 1, Panels A and B), for both healthy and unhealthy a la carte items, the increase occurred only in secondary schools (Figure 1, Panels C and D). Differences across school level are also identified by the differences in the linear trend of the indices, reported in the last column of Table 3. Figure 2 reveals marked differences across school levels in the offering of vending machine items. For instance, in elementary schools, we observed a positive linear trend in the number of both healthy and unhealthy items offered (panel A and B). The timing and the magnitude of this trend closely resembles the trend of vending machine availability in elementary schools (panel C). By contrast, secondary schools experienced a decline in the number of unhealthy items, while the number of healthy items remained approximately stable. Lastly, the overall downward trend for the federal- and state-level health promotion programs (table 3) was entirely driven by the decreasing number of programs implemented in elementary schools, whereas the trend is flat for secondary schools (Figure 2, Panel D). Additional analysis (Supplementary Table S2) showed that this drop was due primarily to the declining presence of “Alliance for a Healthier Generation” and, to a lesser extent, “Safe Routes to School”.
Figure 1.
a,b: Trend of selected indices (1)
Figure 2.
a,b: Trend of selected indices (2)
DISCUSSION
Schools are key venues for implementing interventions that promote healthy food and PA behaviors. To evaluate such interventions, robust and sensitive measures are necessary. This study fills an important gap by developing a set of indices to track changes in different aspects of food and PA environments in schools. One of the advantages of this set of indices is that they are simple to implement and can be easily adapted to different settings. Using these indices, we find that the school food environment changed significantly between 2010 and 2015 with healthier foods being offered in both elementary and secondary schools, paralleling new policies that were implemented during this time. No changes in PA environments were observed.
Other studies have used a similar approach of developing summary measures to assess how policy changes are related to the healthfulness of the school environment [32,33], but have focused on only specific aspects and have been less comprehensive in assessing them. For instance, Nanney and colleagues [32] developed two ‘food scales’ indicating (1) the fruit or vegetable availability and (2) the availability of less-heathy foods and drinks in vending machines or food stores, as well as a PA scale that includes two items—whether physical education was a requirement and whether intramural activities were offered. Between 2010 and 2015, the school PA environment remained mostly unchanged but several dimensions of the school food environment underwent significant changes. In the NSLP, while the number of unhealthy items offered decreased slightly over the study period, the number of healthy items increased significantly. The most notable one-year change, observed in both elementary and secondary schools, occurred between 2012 and 2013. This trend coincided with the implementation of the HHFKA, which required the NSLP to expand the offering of specific healthy foods, such as fruits and vegetables, whole grains, and fat-free and low-fat milk— items which were all included in our survey and captured by the ‘NSLP – Healthy’ index.
These findings, using a comprehensive set of indices measured over a long period of time, are consistent with previous research that was conducted over narrower window of time or that examined selected food offerings, showing an overall positive impact of the HHFKA on the healthfulness of foods offered through the NSLP [1,34–36]. The Youth, Education, and Society annual survey—a nationally representative study of public secondary schools—revealed reductions in the availability of candy/regular fat snacks, higher-fat milk, and french fries, and greater access to fat-free milk, whole grains, and fresh fruits and vegetables through the NSLP, from 2011 to 2013 [35]. Another national survey conducted by the Centers for Disease Control and Prevention, the School Health Policies and Practices Study (SHPPS), observed healthier meals in schools, including the availability of more nonfried vegetables at lunch from 2000 to 2014 [36]. Bergman et al. used nutrient intake from students’ consumption data, [34] to compare NSLP lunches in the spring of 2012 (prior to enactment of the HHFKA) to NSLP lunches at the same schools in spring of 2013. They also found post-HHFKA meals to be significantly healthier.
In the current study, the number of a la carte items increased from 2010 to 2015 for both healthy and unhealthy items, but only in secondary schools. As with NSLP healthy items, in 2013, there was a notable increase in availability of both healthy and unhealthy a la carte items. It is possible that this expansion in availability coincided with implementation of the HHFKA, considering that food service purchasing decisions are made well in advance in schools. Thus, food items in inventory may have no longer been NSLP-compliant, but still compliant if sold a la carte. Additionally, food service directors may have been concerned that students would not find the healthier meals appealing, as was suggested in the media [37], and responded to a possible decline in lunch participation by increasing a la carte options.
Along with NLSP and a la carte offerings, the implementation of HHFKA arguably affected the items available in vending machines as well. For instance, unhealthy vending items in both elementary and secondary schools increased over the study period, particularly in 2013. Notably, in 2014, following implementation of the Smart Snacks guidelines that specifically targeted all competitive foods sold in schools, the number of unhealthy items dropped, especially in secondary schools. This trend continued in 2015, when for the first time in secondary schools the number of healthy items sold in vending machines exceeded the number of unhealthy items.
Our findings on availability of competitive foods (a la carte and in vending machines) are contrary to those of a recent study on Massachusetts middle schools, where competitive food items decreased in 2013 [38]. However, the state of Massachusetts instituted a law in 2012 regulating nutrition standards for competitive foods—regulations that closely mirrored but preceded the implementation of Smart Snacks (2014). In New Jersey, the lag between implementation of HHFKA and Smart Snacks may have been responsible for the increase we observed in unhealthy a la carte as well as vending items, as it allowed schools to comply with HHFKA guidelines for the NSLP while continuing to provide foods outside of the lunch program that did not meet nutrition standards.
Limitations of our study include, first, that the indices capture exposure to different aspects of the school food and PA environment, but not actual food consumption or participation in PA activities. Second, because of limited sample size, we combined middle and high schools into a single category. Third, the questionnaire did not include an open-ended option to fill in additional school-, state-, or federal-level health promotion initiatives. Based on our knowledge of these communities we chose to include programs that were implemented in at least some of the schools. Fourth, because respondents were asked questions about the current as well as the two preceding school years, it is possible that responses for the current year were somewhat more accurate, for both rounds of data collection. Lastly, respondents might also have been subject to desirability bias, whereby they may tend to over report positive facets of the environment and underreport negative ones.
Implications for Policy
School food and PA environments can play a critical role in influencing student behaviors and health outcomes. Changes in these environments in response to policies and programs is an important first step to improve student health. In this study, using newly developed indices, we find that school food environments in urban low-income New Jersey schools improved significantly between 2010 and 2015. During this period, the HHFKA was implemented, requiring schools to offer healthier options in both reimbursable school meals and as competitive foods. These findings are important, especially in light of recent roll-backs to some of the guidelines in response to assumptions about their cost and feasibility [39]. Our results indicate that policies such as the HHFKA are likely to result in school food offerings that are healthier and should therefore be supported and continued.
Conclusion
These analyses describe a newly developed set of indices to measure children’s exposure to different dimensions of school food and PA environments over a 6-year period, between SY 2010–11 and 2015–16. The indices, computed from established survey questions, successfully tracked changes that likely resulted from key policy efforts, and were sensitive to implementation or withdrawal of specific programs, conferring confidence in their effectiveness. Significant improvements were noted in the school food environment, corresponding to implementation of specific policies targeting food offerings in various school venues. While the observed trends may only be generalizable to different settings, the indices can be applied to measure and monitor the change in several dimensions of school food and PA environment in all regions. Future research can build on the current study to validate, expand, or refine these indices. Instruments that provide robust measures of different components of school food and PA environments are valuable for policy evaluation and can help make evidence-based decisions.
Supplementary Material
Acknowledgements:
This research was supported by Grant 1R01HD071583-01A1 and 1R01HL137814-01 from the National Institutes of Health. The funding source had no role in the design or conduct of the study. Everyone who significantly contributed to this work has been listed as an author. We would like to thank Michael Todd for many helpful suggestions.
Funding Source: Funded by the National Institutes of Health (NIH), grant numbers 1R01HD071583-01A1 and 1R01HL137814-01.
Abbreviations:
- PA
(Physical Activity)
- HHFKA
(Healthy Hunger-Free Kids Act)
- SY
(School Year)
- SRTS
(Safe Routes To School)
- NSLP
(National School Lunch Program)
- USDA
(U.S. Department of Agriculture)
- FFVP
(Fresh Fruit and Vegetable Program)
- BMI
(Body Mass Index)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: All authors have indicated they have no potential conflicts of interest to disclose.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
IMPLICATIONS AND CONTRIBUTION
Food and PA environments in schools can affect students’ health behaviors. While established items measuring such environments exist, they have not been incorporated into composite measures. The present study developed 12 indices characterizing aspects of the school food and PA environments and demonstrated their usefulness in tracking changes over time.
Not presented here but available upon request.
REFERENCES
- 1.Johnson DB, Podrabsky M, Rocha A, Otten JJ. Effect of the Healthy Hunger-Free Kids Act on the Nutritional Quality of Meals Selected by Students and School Lunch Participation Rates. JAMA Pediatr 2016;170(1):e153918. [DOI] [PubMed] [Google Scholar]
- 2.Lobstein T, Jackson-Leach R, Moodie M, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385(9986):2510–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cullen KW, Chen T The contribution of the USDA school breakfast and lunch program meals to student daily dietary intake. Prev Med Rep 2017;5:82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry CL, Bishop DB, Taylor GL, Davis M, Story M, Gray C, Bishop SC, Mays RA, Lytle LA, Harnack L. A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health Educ Behav 2004;31(1):65–76. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz MB, Novak SA, Fiore SS. The impact of removing snacks of low nutritional value from middle schools. Health Educ Behav 2009;36(6):999–1011. [DOI] [PubMed] [Google Scholar]
- 6.Story M, Nanney MS, Schwartz MB. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. Milbank Q 2009;87(1):71–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubik MY, Lytle LA, Story M. Schoolwide food practices are associated with body mass index in middle school students. Arch Pediatr Adolesc Med 2005. December 1;159(12):1111–4. [DOI] [PubMed] [Google Scholar]
- 8.Erwin H, Abel M, Beighle A, Noland MP, Worley B, Riggs R. The contribution of recess to children’s school-day physical activity. J Phys Act Health 2012;9(3):442–8. [DOI] [PubMed] [Google Scholar]
- 9.Morton KL, Atkin AJ, Corder K, Suhrcke M, van Sluijs EM. The school environment and adolescent physical activity and sedentary behaviour: a mixed-studies systematic review. Obes Rev 2016;17(2):142–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO Global Strategy on Diet, Physical Activity and Health. 2004. Food Nutr Bull 2004;25(3):292. [DOI] [PubMed] [Google Scholar]
- 11.SHAPE America. Shape of the nation report: Status of physical education in the USA 2010. Reston, VA: National Association for Sport and Physical Education. [Google Scholar]
- 12.USDA. U.S. Department of Agriculture, Food and Nutrition Service. Healthy, Hunger-Free Kids Act Available at: http://www.fns.usda.gov/cnd/Governance/Legislation/CNR_2010.htm. Accessed June 4, 2018.
- 13.USDA. U.S. Department of Agriculture, Food and Nutrition Service. School Meals Available at: https://www.fns.usda.gov/school-meals/nutrition-standards-school-meals. Accessed December 11, 2018.
- 14.USDA. U.S. Department of Agriculture, Food and Nutrition Service. A guide to smart snacks in schools Available at https://www.fns.usda.gov/tn/guide-smart-snacks-schools. Accessed December 11, 2018.
- 15.USDA. U.S. Department of Agriculture, Food and Nutrition Service. Team Nutrition Available at https://www.fns.usda.gov/tn/team-nutrition. Accessed December 11, 2018.
- 16.National Farm to School Network. Available at http://www.farmtoschool.org/. Accessed December 11, 2018.
- 17.USDA. U.S. Department of Agriculture, Food and Nutrition Service. Fresh Fruit and Vegetable Program Available at https://www.fns.usda.gov/ffvp/fresh-fruit-and-vegetable-program. Accessed December 11, 2018.
- 18.Alliance for a Healthier Generation Available at https://www.healthiergeneration.org/our-work/schools. Accessed December 11, 2018.
- 19.2016 Shape of the Nation: Status of physical education in the USA. 2016. SHAPE America – Society of Health and Physical Educators at: shapeamerica org/uploads/pdfs/son/Shape-of-the-Nation-2016_web.pdf. Accessed December 12, 2018.
- 20.Let’s Move! 2017. Available at: https://letsmove.obamawhitehouse.archives.gov/. Accessed June 1, 2018.
- 21.SRTS Guide. Hisory of SRTS 2017. Available at: guide.saferoutesinfo.org/introduction/history_of_srts.cfm. Accessed June 1, 2018.
- 22.Lytle L, Kubik MY. IDEA/ECHO A La Carte, School Stores, and Vending Inventory 2006a. University of Minnesota; Minneapolis, MN. [Google Scholar]
- 23.Lytle L, Kubik MY. IDEA/ECHO Principal Survey 2006b. University of Minnesota; Minneapolis, MN. [Google Scholar]
- 24.Turner L, Sandoval A, Chaloupka F. Food and Fitness: School Health Policies and Practices Questionnaire. Chicago: Bridging the Gap, Health Policy Center, Institute for Health Policy and Research 2014a. University of Illinois; Chicago, IL: http://www.bridgingthegapresearch.org/research/elementary_school_survey/. Accessed June 3, 2018. [Google Scholar]
- 25.Turner L, Sandoval A, Chaloupka F. Youth, Education, and Society: School Health Policies and Practices Questionnaire. Chicago: Bridging the Gap, Health Policy Center, Institute for Health Policy and Research 2014b. University of Illinois; Chicago, IL: Available at: http://www.bridgingthegapresearch.org/research/secondary_school_survey/. Accessed June 3, 2018. [Google Scholar]
- 26.Royston P, White IR. Multiple Imputation by Chained Equations (MICE): Implementation in Stata. J Stat Softw 2011;45(4):1–20. [Google Scholar]
- 27.Johnson RJ, Young R. Towards Best Practices in analyzing Datasets with Missing Data: Comparisons and Recommendations. J Marriage Fam 2011;73(5):926–45. [Google Scholar]
- 28.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. 2007. Prev Sci;8:206–13. [DOI] [PubMed] [Google Scholar]
- 29.Rubin DB. Multiple imputation for non-response in surveys 1987. New York: John Wiley & Sons. [Google Scholar]
- 30.Williams R Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 2012;12(2):308–31. [Google Scholar]
- 31.NCES. National Center for Education Statistics. Common Core of Data https://nces.ed.gov/ccd/ Accessed June 2, 2018.
- 32.Nanney MS, MacLehose RF, Kubik MY, et al. School obesity prevention policies and practices in Minnesota and student outcomes: a longitudinal cohort study. Am J Prev Med 2016;51(5):656–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nanney MS, MacLehose R, Kubik MY, et al. Recommended school policies are associated with student sugary drink and fruit and vegetable intake. Prev Med 2014;62:179–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bergman E, Englund T, Cashman L, Watkins T, Taylor KW, Shaw E, Saade C, Schepman SB. The effects of the Healthy Hunger-Free Kids Act on school lunch. J Acad Nutr Diet 2014;114(9):A60. [Google Scholar]
- 35.Terry-McElrath YM, O’Malley PM, Johnston LD. Foods and beverages offered in US public secondary schools through the National School Lunch Program from 2011–2013: early evidence of improved nutrition and reduced disparities. Prev Med 2015;78:52–8. [DOI] [PubMed] [Google Scholar]
- 36.Merlo C, Brener N, Kann L, McManus T, Harris D, Mugavero K. School-level practices to increase availability of fruits, vegetables, and whole grains, and reduce sodium in school meals—United States, 2000, 2006, and 2014. MMWR Morb Mortal Wkly Rep 2015. August 28;64(33):905–8. [DOI] [PubMed] [Google Scholar]
- 37.EarthTalk. Meal Thicket. Students balk at new school lunch nutrition standards Available at: https://www.scientificamerican.com/article/new-nutrition-standards-for-schoollunches/. Accessed June 12, 2018.
- 38.Gorski MT, Cohen JF, Hoffman JA, Rosenfeld L, Chaffee R, Smith L, Rimm EB. Impact of nutrition standards on competitive food quality in Massachusetts middle and high schools. Am J Public Health 2016;106(6):1101–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.USDA. U.S. Department of Agriculture, Food and Nutrition Service. Child Nutrition Programs: Flexibilities for Milk, Whole Grains, and Sodium Requirements Available at https://www.fns.usda.gov/sites/default/files/cn/CNFlextoOFR.pdf. Accessed December 11, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.