Abstract
Background
Multiparametric MRI (mpMRI) became recognised in investigating those with suspected prostate cancer between 2010 and 2012; in the USA, the preventative task force moratorium on PSA screening was a strong catalyst. In a few short years, it has been adopted into daily urological and oncological practice. The pace of clinical uptake, born along by countless papers proclaiming high accuracy in detecting clinically significant prostate cancer, has sparked much debate about the timing of mpMRI within the traditional biopsy-driven clinical pathways. There are strongly held opposing views on using mpMRI as a triage test regarding the need for biopsy and/or guiding the biopsy pattern.
Objective
To review the evidence base and present a position paper on the role of mpMRI in the diagnosis and management of prostate cancer.
Methods
A subgroup of experts from the ESUR Prostate MRI Working Group conducted literature review and face to face and electronic exchanges to draw up a position statement.
Results
This paper considers diagnostic strategies for clinically significant prostate cancer; current national and international guidance; the impact of pre-biopsy mpMRI in detection of clinically significant and clinically insignificant neoplasms; the impact of pre-biopsy mpMRI on biopsy strategies and targeting; the notion of mpMRI within a wider risk evaluation on a patient by patient basis; the problems that beset mpMRI including inter-observer variability.
Conclusions
The paper concludes with a set of suggestions for using mpMRI to influence who to biopsy and who not to biopsy at diagnosis.
Key Points
• Adopt mpMRI as the first, and primary, investigation in the workup of men with suspected prostate cancer.
• PI-RADS assessment categories 1 and 2 have a high negative predictive value in excluding significant disease, and systematic biopsy may be postponed, especially in men with low-risk of disease following additional risk stratification.
• PI-RADS assessment category lesions 4 and 5 should be targeted; PI-RADS assessment category lesion 3 may be biopsied as a target, as part of systematic biopsies or may be observed depending on risk stratification.
Electronic supplementary material
The online version of this article (10.1007/s00330-019-06166-z) contains supplementary material, which is available to authorized users.
Keywords: Prostate cancer, Magnetic resonance imaging, Biopsy, Risk assessment, Observer variation
Introduction
In 2012, the European Society of Urogenital Radiology (ESUR) prostate committee promoted the use of multiparametric MRI (mpMRI) in the routine management of men with suspected or confirmed prostate cancer [1]. That proposal has gained widespread acceptance. The debate has now moved to when mpMRI should be used.
Expressions of interest were sought from the 58 members of the ESUR Prostate MRI Working Group at the European Congress of Radiology (ECR) in March 2017 in contributing to a position statement on the use of mpMRI in prostate cancer diagnosis. Each of the 7 initial positive respondents was invited to contribute but based on the relative contributions, the final author list was revised to 5 ensuring due representation of the group’s European composition; a sixth contributor joined at ECR, March 2018. The final contributors were from the UK, France, The Netherlands, Denmark, Italy, and Belgium.
The approach was to review published evidence, supplemented by knowledge of completed cohort studies in the process of being published (having been accepted for publication). In this way, there was very little intra-author disagreement. On the specific topic of biopsy planning—the pros and cons of systematic versus targeted-driven approach—there was some variation in how strongly the argument for targeted biopsy over systematic biopsy could be worded. As the paper neared completion, the results from on-going studies became known to the author group, such that a consensus position was reached.
Evaluating clinically significant prostate cancer
Evaluating clinically significant prostate cancer in the pre-MRI era
Urologists and oncologists gauge prostate cancer aggressiveness by combining DRE findings, serum PSA levels and data derived from systematic biopsy findings.
Men with suspected prostate cancer are categorised into risk groups (see EAU risk classification in EAU guidelines on prostate cancer [2]). This classification is based on the grouping of patients with a similar risk of biochemical recurrence after radical treatment [3]. Tables and nomograms have been developed to predict the likelihood of extraprostatic spread, seminal vesicle invasion and lymph node involvement, and some even state recurrence-free survival rates at 3 and 5 years [4–8].
There is, however, still no consensus of what constitutes a clinically significant prostate cancer (csPCa) [9]. Current argument centres on Gleason category 7 pattern 3 or 4 dominance, ISUP grades 2 and 3, respectively. While the 2014 grading system differentiates Gleason 7 by dominant pattern, all Gleason 7 is classed intermediate risk, albeit with the qualification that emerging clinical data support the distinction between favourable (ISUP grade 2) and unfavourable-risk (ISUP grade 3) patient categories within the intermediate-risk group [2, 10, 11].
Evaluating csPCa in the post-MRI era
mpMRI can detect and localise cancers with a Gleason score ≥ 7 more easily than lower-grade cancers [12–15], relying on the lower signal intensity of higher-grade cancers on T2-weighted imaging (T2w), more impeded diffusion on diffusion-weighted imaging (DWI), early enhancement on dynamic contrast sequences (DCE), and (previously) higher choline over citrate ratios on spectroscopic imaging [16–18]. mpMRI evaluates lesion volume with reasonable accuracy, at least for aggressive tumours [19]. In one study, correlations between lesion volume estimated on T2-weighted images, ADC maps, and DCE-MR images with pathology were 0.91 and 0.93, respectively [20].
In 2012, the ESUR proposed a standardised reporting tool called ‘PI-RADS’ (Prostate Imaging Reporting and Data System) [1] in an attempt to align mpMRI findings with the risk of having csPCa. In 2015, an updated version (PI-RADS v2) was published in collaboration with the American College of Radiology and the AdMeTech Foundation [21, 22] (Table 1). PI-RADS 2 has been validated in a meta-analysis of 21 studies including over 3857 patients. This demonstrated a pooled sensitivity of 89% and a pooled specificity of 73% [23].
Table 1.
Comparison of Prostate Imaging and Reporting and Data System versions 1 and 2 (adapted from Barentsz et al [22])
| PI-RADS version 1 | PI-RADS version 2 |
|---|---|
| A sum score of 3–15 (20 with MRSI) for T2W + DWI + DCE (+ MRSI) is suggested | 1–5 point dominant score |
| For peripheral zone, DWI is dominant | |
| For transition zone, T2W is dominant | |
| Equal role for DCE (5-point scale) | Secondary role for DCE (positive or negative) |
| For DWI: ADC images are mandatory | For DWI: ADC and high b value images (b value > 1400) are mandatory |
| 27-sector map | 39-sector map |
| MRSI can be included | MRSI is not included |
| Size is not used for T2W + DWI | Size (> 15 mm) is used for T2W + DWI to separate PI-RADS scores 4 and 5 |
The EAU/ESTRO/ESUR/SIOG recommends using mpMRI before repeat biopsy, combining a TRUS-directed diagnostic approach with the addition of the mpMRI and subsequently targeted biopsies [2, 24]. Neither the European (EAU/ESTRO/SIOG/ESUR) nor the American (NCCN) guidelines endorse wholeheartedly mpMRI in biopsy-naïve men [2, 24].
The NICE guideline CG175 [25] has been updated and is due for publication in April 2019 [https://www.nice.org.uk/guidance/indevelopment/gid-ng10057]; it recommends pre-biopsy mpMRI, putting mpMRI as the primary method to investigate those with suspected prostate cancer based on PSA and/or DRE findings. Revised in November 2018, the French guidelines now also recommend pre-biopsy mpMRI for all, including biopsy-naive [26]. Appendix 1, which includes in addition to references cited in the main text citations to PROTECT trial [27], Belgian National Guidance [28] and recently updated French National Guidance [29].
Eligibility criteria to have an mpMRI (in place of biopsy) should be based on the EAU and/or National current recommendations for biopsy referrals. Following suitable clinical evaluation for acute or chronic reasons not to be investigated, the reasons to offer mpMRI would mirror those currently used to offer biopsy.
Pre-biopsy mpMRI advantages
The problem with any approach dominated by TRUS-guided systematic biopsy (SBx) is that it is organ rather than lesion based, introducing two major limitations: overdiagnosis of clinically insignificant prostate cancers (cisPCa) and under-diagnosis of csPCa.
The case for excluding men from biopsy based on mpMRI
Avoiding or deferring biopsy (possibly indefinitely) if mpMRI suggests low likelihood of csPCa would reduce the burden to men and to their health systems of initial diagnostic workup and low-grade prostate cancer follow-up. Such an approach may also improve the cost efficiency of the diagnostic workup [30]. Accepting that the results are subject to assumptions around test costs, sensitivity of mpMRI-influenced biopsies, and long-term outcomes of men with PCa, recent analysis of a UK population concluded mpMRI first followed by up to 2 rounds of biopsy is more cost effective than current practice [31]. This strategy requires a high negative predictive value (NPV) of mpMRI in excluding csPCa.
A recent systematic review (9613 men) in conjunction with the EAU-ESTRO-ESUR Prostate Cancer Guidelines panel revealed a median mpMRI NPV of 82% (interquartile range (IQR), 69–92%) for overall cancer exclusion and of 88% (IQR, 86–92%) for csPCa exclusion [32]. The critical issue highlighted in this review is that the reported range of the NPV for mpMRI is extreme and varies according to definitions and risk categorisation used.
A key variable of the NPV is the prevalence of cancer within the population being monitored: when the prevalence doubles from 30 to 60%, the NPV of mpMRI (scores 1–2 taken as ‘negative’) falls from 88 to 67% (for any cancer grade) (Table 2) [32]. NPV therefore is bound to be variable as it depends on whether mpMRI is being used in a low-risk screening setting or in a selected high-risk cohort. Furthermore, the prevalence will alter according to the definition of csPCa (Table 3).
Table 2.
Negative predictive estimates for pre-biopsy mpMRI as a function of prostate cancer prevalence (adapted from Molovan et al [32])
| PCa prevalence | NPV |
|---|---|
| 0.30 | 0.88 (0.77–0.99) |
| 0.40 | 0.82 (0.70–0.94) |
| 0.50 | 0.76 (0.64–0.88) |
| 0.60 | 0.67 (0.56–0.79) |
| 0.70 | 0.57 (0.47–0.67) |
Table 3.
Diagnostic accuracy results from mpMRI for different definitions of clinically significant prostate cancer (adapted from PROMIS study [33])
| Definition of csPCa | Prevalence (%) | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|
| Gleason score ≥ 3 + 4 or cancer core length ≥ 4 mm, | 57 (53–62) | 87 (83–90) | 47 (40–53) | 69 (64–73) | 72 (65–79) |
| Gleason score ≥ 3 + 4 | 53 (49–58) | 88 (84–91) | 45 (39–51) | 65 (60–69) | 76 (69–82) |
| Gleason score ≥ 4 + 3 or cancer core length ≥ 6 mm | 40 (36–44) | 93 (88–96) | 41 (36–46) | 51 (46–56) | 89 (83–94) |
Three pivotal multicentre trials on the use of mpMRI in biopsy-naïve men inform this review: PROMIS, PRECISION [33, 34], and the 4M study by van der Leest [35].
The PROMIS trial assessed mpMRI, 12-core SBx and template transperineal biopsy (TTP Bx) in 576 prospectively included biopsy-naïve men [33]. Forty percent of patients had csPCa (defined as Gleason score ≥ 4 + 3 or cancer core length ≥ 6 mm) at TTP (Table 3). Using TTP Bx as a reference test, the NPV for detecting csPCa was 0.89 (95%CI, 0.83–0.94) for mpMRI compared with 0.74 (0.69–0.78) for TRUS SBx (csPCa prevalence,: 40% (95%CI, 36–44%)). mpMRI failed to report 7% (17/230) Gleason 3 + 4 cancers with core lengths between 6 and 12 mm, but no Gleason 4 + 3 or worse cancers. When accepting missing this 7%, mpMRI (used as a triage test) could have avoided 27% of primary biopsies, while detecting 18% more csPCa and ‘missing’ 5% of cisPCa [33]. The definition of csPCa propagated by the START consortium is GS ≥ 3 + 4 [36]. The usage of this definition in the PROMIS study showed an increase in the prevalence of csPCa to 53% (49–58%); the NPV dropped to 76% (69–82%). mpMRI failed to report 12% Gleason 3 + 4 prostate cancers, but still could have avoided 27% of primary biopsies.
Similar results were reported in the more recent multicentre, randomised, noninferiority PRECISION trial, in which 500 biopsy-naïve men were randomised to undergo either mpMRI with or without targeted biopsy, or standard transrectal ultrasonography-guided biopsy [34]. Using mpMRI as a triage test could have avoided 28% of primary biopsies, while detecting 12% more csPCa (defined as Gleason score ≥ 3 + 4) than SBx and ‘missing’ 13% of cisPCa. These results were obtained in 25 centres (academic and non-academic) with mixed experience in both mpMRI and MR-targeted biopsy, and without restrictions on the use of a 1.5-T or a 3.0-T system, endorectal coil, or biopsy technique (visual registration, software-assisted registration or in-bore).
The 4M study included 626 biopsy-naïve patients; all patients underwent systematic biopsy, and those with a positive mpMRI (PI-RADS 3–5, 51%) underwent additional in-bore MRI-TBx. SBx performed in PI-RADS 1–2 cases detected csPCa in only 3% of the patients while detecting cisPCa in 20%, with an 89% reduction in total biopsy cores [35].
In a clinical follow-up study (median follow-up of 41 months) of a mixed population of biopsy-naïve, repeat biopsies, and active surveillance (n = 300), who had undergone a negative in-bore MR-guided biopsy for PI-RADS 3–5 lesions, only 1.7% (5/300) had csPCa subsequently diagnosed by any kind of follow-up histology in 82 men (any biopsy or radical prostatectomy), and in 218 without any histology confirmation [37]. In another cohort of 1255 patients with negative mpMRI, the csPCa-free survival rates at 48 months were 95% in originally biopsy-naïve patients and 96% in patients with a prior negative biopsy [38].
Improving detection of csPCa
Pre-biopsy mpMRI in men with suspected prostate cancer is justified further if it improves the detection of csPCa through targeted biopsies of any suspicious lesion suggested by mpMRI.
Radiologic-pathologic correlations with whole-mounts have shown that mpMRI is highly sensitive for locating aggressive cancers, with 80–86% of Gleason 7 and 93–100% of Gleason ≥ 8 detected [12]. Correlation studies of mpMRI with TBx or radical prostatectomy specimens performed after the introduction of PI-RADS showed that the location of the index lesion was correctly assessed by mpMRI in 95% of patients [39] and that mpMRI missed 10% csPCa on a per-lesion basis [40]. mpMRI results, whether expressed as subjective (Likert) scoring [41–43], PI-RADS v1 [44, 45], or PI-RADS v2 scoring [46], were found significant predictors of the presence of csPCa at biopsy.
A recent systematic review of mostly retrospective studies showed that TBx performed under MR/TRUS fusion detected more csPCa than SBx, with a median detection rate of 33.3% (range, 13.2–50%) versus 23.6% (range, 4.8–52%), respectively. The absolute difference in the detection rates between the two approaches was a median of 6.8% (range, 0.9–41.4%) and always in favour of TBx. The median number of biopsy cores to detect one man with csPCa was 37.1 (IQR, 32.6–82.8) and 9.2 (IQR, 4–37.7) for SBx and TBx, respectively [47]. Another systematic review (focussing on MRI positive men only), including studies that used MR/TRUS fusion, cognitive guidance, or in-bore guidance for TBx, also found that TBx has a higher rate of detection of csPCa than SBx with a sensitivity of 0.91 (95%CI, 0.87–0.94) and 0.76 (95%CI, 0.64–0.84), respectively, in a mixed population of biopsy-naïve men and men with previous negative biopsies [48]. The sensitivity (detection) ratio was 1.10 (95%CI, 1.00–1.22) and significantly in favour of TBx for biopsy-naïve men only, and 1.54 (95%CI, 1.05, 2.26) in men with previous negative biopsies. In a head-to-head comparison in 223 men with elevated PSA and/or abnormal DRE, mpMRI-influenced biopsy outperformed systematic 12-core TRUS biopsy in detecting csPCa on a patient basis (42% vs 35%) and on a lesion basis (74% vs 61%) with a ‘miss rate for significant lesions’ of ~ 18% in the MRI biopsy group versus ~ 26% rate in the TRUS biopsy group [49].
Targeted versus systematic biopsy versus combined approach for clinically significant prostate cancer detection
mpMRI-targeted biopsies detect about 90% of all csPCa [12, 33, 48]. This, however, also means that about 10% of csPCa are missed if only a targeted approach is adopted. Indeed, histological correlation highlights that Gleason ≥ 7 cancers can be invisible on mpMRI [12]. It therefore may seem prudent, on first thoughts, to supplement targeted biopsies with systematic biopsies to ‘capture’ any csPCa that is missed by mpMRI (usually low grade 4 and organ-confined [50], located in the dorsolateral or apical segments of the peripheral zone [49]).
The combination of SBx and MRI-targeted biopsies (TBx) comes at a cost: over-detection of cisPCa [51, 52]. In a systematic review of 16 studies comparing TBx and SBx in mixed populations of biopsy-naïve men and men with previous negative biopsies, this overdiagnosis was almost halved by omitting SBx [48]. In the PRECISION trial, 13% (95% CI, − 19 to − 7%; p < 0.001) fewer men were diagnosed with cisPCa in the MRI-targeted biopsy group (in total 9%) than in the standard biopsy group (in total 22%); again, this diagnosis was more than halved by omitting SBx. Likewise, in a prospective non-randomised trial of 1003 men who underwent both TBx and SBx, adding SBx to TBx identified an additional 103 (22%) prostate cancers, 83% of which were low-grade [53].
Excluding SBx in the MRI-negative men in the 4M would have avoided biopsies in 49% in this study population at a small expense of missing csPCa [35].
The MRI-FIRST multicentre study [54] recruited biopsy-naïve men (n = 251) under 75 years with a PSA ≤ 20 ng/ml. All patients had 12-core SBx plus 2 optional cores to hypoechoic lesions by one operator blinded to mpMRI results, and TBx (up to 2 targeted lesions, 3 cores per lesion) by another operator. SBx and TBx detection rates for ISUP grade ≥ 2 tumours were 29.9% and 32.3%, respectively (p = 0.38; detection ratio 1.08). ISUP grade ≥ 2 cancers would have been missed in 7.6% (95%CI, 4.6–11.6%) of patients if TBx had not been taken, and in 5.2% (95%CI, 2.8–8.7%) of patients if SBx had not been performed. TBx detected significantly more ISUP grade ≥ 3 tumours than SBx (19.9% vs 15.1%, p = 0.0095; detection ratio, 1.32). ISUP grade ≥ 3 cancers would have been missed in 6.0% (95%CI, 3.4–9.7%) of patients if TBx had not been taken, but in only 1.2% (95%CI, 0.2–3.5%) of patients if SBx had not been performed. These data indicate that predominantly ISUP grade 2 prostate cancers were detected by the inclusion of SBx.
Technology that allows mapping exactly the biopsy needle path has suggested that the median number of systematic cores sampling the same region selected for target is 2. If these ‘isometric’ systematic cores are disregarded, systematic biopsy has a modest benefit only: 3% cancer detection instead of benign diagnosis and ~ 1% from cisPCa to csPCa [55].
There are few data comparing TBx to TTP Bx. TTP Bx should be considered in patients at high risk with negative mpMRI and in some patients at low-risk with persistently elevated PSA and a negative MRI.
Biopsy strategy in the ‘mpMRI first’ era
It is impossible to brush aside that the range of published mpMRI NPV figures is broad and that csPCa prevalence (i.e. pre-MRI probability of csPCa) has a major impact on NPV [9, 32]. Therefore, there is a need to refine the biopsy planning process by incorporating the mpMRI findings within a larger nomogram containing clinical data to determine an individual’s likelihood of having csPCa.
In a recent multivariate logistic regression analysis to predict likelihood of csPCa for biopsy-naive and previously biopsied men, the PI-RADS classification contributed significantly to a newly developed risk model (p < 0.001) in combination with the ERSPC-RCs (www.prostatecancer-riskcalculator.com) based on the European Randomised Study of Screening for PCa (ERSPC) [56, 57]. For biopsy-naive men, the risk model reached a higher AUC (0.83), compared with ERSPC-RC3 (0.81), refitted RC3 (0.80), and PI-RADSv1.0 (0.76). The risk model AUC was comparable with that of ERSPC-RC3 + PI-RADSv1.0 (0.84). Likelihood ratio test results similarly showed that the risk-models may perform significantly better compared with (refitted) ERSPCs and PI-RADS alone. Others have confirmed these results [58].
PI-RADS 3 lesions and risk stratification and biopsy
PI-RADS assessment category 3 is assigned when the probability of prostate cancer is uncertain. The percentage of patients assigned a PI-RADS assessment category of 3 is extremely variable in the different published cohorts [59]. As expected, the biopsy positivity rate is also highly variable in these lesions; the cumulative total of high-grade PCa (GS ≥ 3 + 4) in the PI-RADS category 3 has been reported 21% (range 4–27%) in biopsy-naïve men and 16% (range 10–19%) men with previous negative biopsies [59]. Another paper lists overall cancer detection 16–67% and proportion of Gleason ≥ 7 cancers 0–43% [46]. Based on these data, the authors concluded that the prevalence of PI-RADS 3 index lesions in the diagnostic workup is not negligible, varying between one in five (22%) and one in three (32%) men, depending on patient cohort of the first biopsies or previous negative biopsies. The actual prevalence of csPCa after TBx in PI-RADS category 3 lesions varies between patient groups from one in five (21%) and one in six (16%), depending on previous biopsy status. Although this prevalence is lower in comparison to PI-RADS category 4 and PI-RADS category 5 lesions, still a considerable proportion of men harbour significant disease.
Biopsy strategy and patient risk
Biopsy decisions should first be based on mpMRI findings, favouring avoiding biopsy in ‘negative’ (any/all lesions PI-RADS 2 or less) studies and targeting PI-RADS 4 or 5 lesions. For some ‘negative’ studies and most PI-RADS 3 lesions, a second assessment incorporating clinical (age, DRE, family history for example) and biochemical (PSA density and velocity) parameters should be applied to see if systematic biopsy alone or in addition to targets to the low-grade PI-RADS lesions are indicated.
The use of PSA density may improve the patient selection for biopsy [32, 35, 56, 57, 60–65]. Two studies using either the PI-RADS V1 scoring [66] or a mix of PI-RADS v1 and v2 systems [37] suggested that PSA density could discriminate among PI-RADS 3 patients, those who need to undergo prostate biopsy from those who can be followed up. In a multicentre study of biopsy-naïve men, PI-RADS category 3 lesions were further categorised into PSA density of < 0.10, 0.10–0.20, and > 0.20: the detection of GS ≥ 3 + 4 PCa was 18%, 31%, 46%, respectively [67].
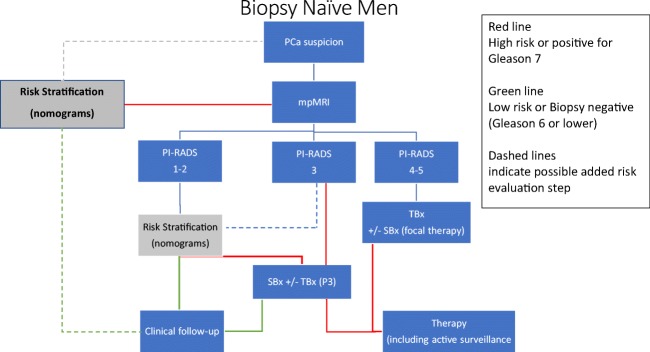
In patients stratified into a priori low-to-intermediate risk (Table 1), the mpMRI NPV is probably sufficiently high to avoid SBx in case of negative mpMRI [34]. Systematic biopsy results would be expected to be less influential on patient management in the setting of a positive mpMRI with a suspicious lesion than in a negative mpMRI. In high-risk patients, however, patients with negative mpMRI will probably still need SBx [34]; even in expert centres, mpMRI may ‘miss’ 10–12% csPCa. The recommended shift towards an MRI-directed and risk-stratified approach to seeking csPCa is captured in the flowchart (Fig. 1). A shift in emphasis away from SBx with additional MRI-TBx to MRI-TBx for high-probability mpMRI examinations is recommended, accepting the modest price of missing csPCa [33, 68–75].
Fig. 1.
Proposed flowchart for investigating men suspected having prostate cancer, beginning with mpMRI. Using mpMRI as the primary investigation in prostate cancer diagnostic workup following clinical suspicion, men will be stratified into PI-RADS assessment categories 1–2, 3, and 4–5. Capitalising on the high negative predictive value of mpMRI, assessment category 1–2 may indicate clinical follow-up avoiding systematic biopsy, or indicate further risk stratification with developing risk calculators (nomograms). Assessment category 3 may indicate MR-targeted biopsy (TBx) combined with systematic biopsy (SBx) to gain maximal diagnostic yield. Alternatively, risk stratification may sub-differentiate these men into high-risk and low-risk; the low-risk group may defer systematic biopsy. Assessment category 4–5 may indicate MR-targeted biopsy. Systematic biopsy could be performed in direct combination or secondary, depending on biopsy workflow. In assessment category 5, the added value of systematic biopsy would be limited. When prostate cancer has not been identified, additional risk stratification could be performed to indicate or avoid additional systematic and targeted biopsy. Green arrows, low-risk; red arrows, intermediate-/high-risk. Dotted lines indicate research in progress. PCa, prostate cancer; MRI, magnetic resonance; PI-RADS, prostate imaging reporting and data system = suspicion MRI score (1–5); TBx, MRI-targeted biopsy; SBx, transrectal/transperineal ultrasound-guided systematic biopsy; AS, active surveillance
Inter-reader variability
There are three difficulties with the widespread introduction of pre-biopsy mpMRI: the variable NPV of mpMRI, the variable accuracy of using mpMRI with TRUS to target suspicious lesions regardless of their location within the prostate gland, and inter-reader variability. The results from studies addressing the variability between 2013 and 2017 are summarised in Table 4.
Table 4.
Inter-reader reproducibility of prostate MRI scoring systems
| Inter-reader agreement | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pt no | Histology standard | Analysis level | No readers | Reader experience | Cancer prevalence (1) | Metric used | Likert | PI-RADS V1 | PI-RADS V2 | |
| Rosenkrantz 2013 [76] | 70 | RRP | Per region (18 regions) | 3 | 6 years each |
PZ, 22.1% (279/1260) TZ, 26.5% (223/840) Both, 13.3% (56/420) |
Mean kappa across combinations of readers |
PZ, 0.56 [0.51–0.61] TZ, 0.59 [0.56–0.62] Both, 0.45 [0.37–0.57] |
PZ, 0.51 [0.41–0.49] TZ, 0.29 [0.24–0.34] Both, 0.51 [0.47–0.55] |
– |
| Rosenkrantz 2013 [77] | 55 | RRP | Per region (18 regions) | 3 |
R1, 6 years R2, 4 years R3, junior |
ND | Mean concordance correlation coefficient across combinations of readers |
PZ: R1-R2, 0.63 [0.58–0.67] R1-R3, 0.47 [0.42–0.53] R2-R3, 0.54 [0.49–0.59] TZ: R1-R2, 0.52 [0.44–0.59] R1-R3, 0.40 [0.30–0.48] R2-R3, 0.29 [0.20–0.37] Both: R1-R2, 0.61 [0.57–0.64] R1-R3, 0.47 [0.43–0.51] R2-R3, 0.50 [0.45–0.54] |
PZ: R1-R2, 0.68 [0.63–0.72] R1-R3, 0.54 [0.48–0.59] R2-R3, 0.47 [0.42–0.52] TZ: R1-R2, 0.38 [0.29–0.45] R1-R3, 0.28 [0.22–0.34] R2-R3, 0.09 [0.05–0.14] Both: R1-R2, 0.61 [0.57–0.65] R1-R3, 0.48 [0.43–0.52] R2-R3, 0.34 [0.30–0.38] |
|
| Vaché 2014 [78] | 215 | RRP | Per lesion | 3 |
R1, 11 years R2, 1 year R3, junior |
Overall cancer: R1, 58.5% (254/434) R2, 59.6% (226/379) R3, 48.3% (187/387) Gleason ≥ 7: R1, 40.1% (187/387) R2, 43.3% (164/379) R3, 36.4% (141/387) |
Kappa for pairs of readers |
Overall cancer: R1-R2, 0.52 [0.44–0.60] R1-R3, 0.51 [0.43–0.58] R2-R3, 0.47 [0.38–0.55] Gleason ≥ 7: R1-R2, 0.44 [0.33–0.55] R1-R3, 0.50 [0.37–0.64] R2-R3, 0.37 [0.31–0.50] |
Overall cancer: R1-R2, 041 [0.34–0.46] R1-R3, 0.44 [0.37–0.50] R2-R3, 0.38 [0.31–0.44] Gleason ≥ 7: R1-R2, 0.38 [0.28–0.47] R1-R3, 0.39 [0.29–0.49] R2-R3, 0.34 [0.28–0.47] |
|
| Thompson 2014 [79] | 165 | TBx | Per patient | 2 | > 1000 MRIs each | 61.3% (101/165) | Kappa | 0.63 [0.52–0.72] | ||
| Renard-Penna 2015 [80] | 50(2) | TBx | Per patient | 2 | > 10 years each |
ND for the 50 pts. 58.5% for the cohort of 118 pts |
Kappa | 0.80 [0.69–0.91] | 0.73 [0.61–0.85] | |
| Muller 2015 [81] | 101 | TBx | Per lesion | 5 | 6 months–12 years | 54.3% (88/162) | Mean kappa across combinations of readers | 0.46 ± 0.03 | ||
| Kasel-Siebert 2016 [82] | 82(3) | TBx | Per lesion | 2 |
R1, 10 years R2, < 1 year |
PZ, 69.2% (27/39) TZ, 12.4% (12/97) Both, 28.7% (39/136) |
Kappa |
PZ, 0.49 [0.30–0.48] TZ, 0.62 [0.46–0.79] Both, 0.55 [0.41–0.68] |
PZ, 0.69 [0.56–0.81] TZ, 0.68 [0.45–0.9] Both, 0.68 [0.56–0.80] |
|
| Zhao 2016 [83] | 372 | TBx | Per patient | 2 | ND | 49.7% (185/372) | Kappa | 0.48 | ||
| Rosenkrantz 2016 [84] | 120(4) | TBx | Per lesion | 6 | 4–9 years | 47.6% (30/63) |
Mean kappa across combinations of readers(5) Percent agreement(5,6) |
PZ/PI-RADS ≥ 3, 0.53 PZ/PI-RADS ≥ 4, 0.59 TZ/PI-RADS ≥ 3,0.39 TZ/PI-RADS ≥ 4, 0.51 Both/PI-RADS ≥ 3, 0.46 Both/PI-RADS ≥ 4, 0.56 PZ/PI-RADS ≥ 3, 81.9% PZ/PI-RADS ≥ 4, 80.1% TZ/PI-RADS ≥ 3, 76.4% TZ/PI-RADS ≥ 4, 75.4% Both/PI-RADS ≥ 3, 79.2% Both/PI-RADS ≥ 4, 77.8% |
||
| Polanec 2016 [85] | 65 | TBx | Per patient | 2 | > 150 MRIs/year each | 50.8% (33/65) | Kappa | 0.81 | 0.71 | |
| Tewes 2016 [86] | 54 | TBx | Per patient | 2 | 2–5 years | 57.4% (31/54) | Kappa |
All lesions, 0.39 Cancers, 0.14 Benign lesions, 0.50 |
All lesions, 0.56 Cancers, 0.56 Benign lesions, 0.26 |
|
| Greer 2017 [87] | 35 | RRP | Per lesion | 5 |
2 expd, 8–15 years 3 less expd, 2 years |
Average of 2.1 lesions per patient. Average of 1.7 true positives per patient (81%) |
Average index of specific agreement |
Overall: global scoring, 0.58 ± 0.04 PI-RADS ≥ 4, 0.72 ± 0.03 Expd: global scoring, 0.70 ± 0.04 PI-RADS ≥ 4, 0.81 ± 0.04 Less expd: global scoring, 0.53 ± 0.04 PI-RADS ≥ 4, 0.68 ± 0.04 |
||
Pts, patients; Ref. Std, reference standard; RRP, retropubic radical prostatectomy; TBx, targeted biopsy; expd, experienced
(1)Prevalence for overall cancer, unless specified otherwise
(2)Randomly selected from a cohort of 118 pts. with a single lesion prospectively scored Likert ≥ 3/5; these patients were re-evaluated by two readers
(3)Patients with at least one lesion prospectively scored PI-RADS V1 ≥ 3/5
(4)Retrospective selection of 120 lesions (one per patient) consisting of 15 lesions with Likert scores 2–5 in PZ and in TZ
(5)Average value of two interpretation sessions separated by a training intervention
(6)Fraction of all 15 possible pair-wise reader combinations with a concordant reading
The conclusions from the studies are succinctly captured by Hansen et al [88]: (1) mpMRI exams are more often called negative in subspecialist reads (41% vs 20%); (2) second readings of prostate mpMRI by subspecialist uroradiologists significantly improve NPV and PPV; (3) reporter experience may reduce overcalling and avoid over targeting of lesions; and (4) greater education and training of radiologists in prostate mpMRI interpretation are advised. Many European countries are, in collaboration with ESUR and EAU, working to address this training need.
Conclusion
Current national guidelines in Europe highlight the worth of mpMRI in the management of men with suspected PCa. The case for using mpMRI to help in selecting which men with suspected PCa should have a biopsy—and which need not—and to then select the regions of the prostate to biopsy (and which regions can be ignored) is compelling. The evidence base, including level 1 studies, is overpowering as are the arguments for patient benefit, avoiding either biopsy or overdiagnosis of clinically insignificant cancer.
Patients contemplating a biopsy are becoming aware that imaging by means of mpMRI may permit avoidance of biopsy in some cases and targeting in others. These patients will be understandably anxious to avoid the risks of biopsy, or at least minimise the risks by having fewer biopsy samples. Going away from ‘default’ SBx to premeditated TBx judiciously and selectively complimented by SBx using a two-step risk evaluation offers the best compromise to reduce biopsy rates and reduce overdiagnosis of cisPCa while minimising the chances of missing csPCa. The evidence to expect to avoid SBx altogether even in the era of pre-biopsy mpMRI is weak [54].
Our summary suggestions are presented in Table 5.
Table 5.
Suggestions for the use of mpMRI as a triage test in those with suspected prostate cancer
| 1. mpMRI should be the first investigation in the workup of men with suspected prostate cancer (Fig. 1) | |
| 2. PI-RADS assessment categories 1 and 2 have a high predictive value in excluding significant disease, and systematic biopsy may be postponed, especially in men with low-risk of disease following additional risk stratification (see 7 below) | |
| 3. PI-RADS assessment category lesions 4 and 5 should be targeted | |
| 4. PI-RADS assessment category lesion 3 may be targeted and systematic biopsied depending on risk stratification | |
| 5. Targeted biopsy (cognitive, MRI/US fusion, or ‘in-bore’) should be available for biopsy of focal lesions | |
| 6. Systematic biopsies in addition to targeted biopsy should be used judiciously rather than as a default, for example in cases being considered for focal therapy or nerve-sparing surgery | |
| 7. Where clinical risk parameters including age, family history, DRE findings, PSA velocity, and PSA density are of concern, SBx should be considered even in the setting of a negative mpMRI |
Electronic supplementary material
(DOCX 30.8 kb)
Abbreviations
- ADC
Apparent diffusion coefficient
- AUC
Area under the ROC curve
- CI
Confidence interval
- cisPCa
Clinically insignificant prostate cancer
- csPCa
Clinically significant prostate cancer
- DCE
Dynamic contrast-enhanced
- DRE
Digital rectal examination
- DWI
Diffusion-weighted imaging
- EAU
European Association of Urology
- EPE
Extraprostatic extension
- ERSPC
European Randomised Study of Screening for PCa
- ESO
European Society of Oncology
- ESUR
European Society of Urogenital Radiology
- GG
Grade grouping
- GS
Gleason score
- IQR
Interquartile range
- mpMRI
Multiparametric magnetic resonance imaging
- MRSI
Magnetic resonance spectroscopic imaging
- NPV
Negative predictive value
- PI-RADS
Prostate Imaging Reporting and Data System
- PI-RADS v1
Prostate Imaging Reporting and Data System version 1
- PI-RADS v2
Prostate Imaging Reporting and Data System version 2
- PPV
Positive predictive value
- PSA
Prostate-specific antigen
- PSAd
Prostate-specific antigen density
- SBx
Systematic biopsies
- T2W
T2 weighted
- TBx
MRI-targeted biopsies
- TBx
Targeted biopsy
- TRUS
Transrectal ultrasound
- TTP Bx
Template transperineal biopsy
- Trial
PRIAS
- Trial
PROTECT
- Trial
PRECISION
- Trial
PROMIS
Funding
The authors state that this work has not received any funding.
Compliance with ethical standards
Guarantor
The scientific guarantor of this publication is Jonathan Richenberg, MA BM Bch MRCP FRCR Hon Sen Lect BSMS, on behalf of ESUR Prostate Working Group.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
No human subjects involved.
Ethical approval
Institutional Review Board approval was not required because this is a review article of evidence published.
Methodology
• Literature review and evidence analysis.
• Multicentre study—ESUR Working Group, Prostate Cancer with representatives from the UK, France, Denmark, Italy, and Netherlands
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barentsz Jelle O., Richenberg Jonathan, Clements Richard, Choyke Peter, Verma Sadhna, Villeirs Geert, Rouviere Olivier, Logager Vibeke, Fütterer Jurgen J. ESUR prostate MR guidelines 2012. European Radiology. 2012;22(4):746–757. doi: 10.1007/s00330-011-2377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mottet N, van den Bergh RCN, Briers E et al (2018) Guidelines on prostate cancer. https://uroweb.org/guideline/prostate-cancer/?type=archive
- 3.D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–974. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 4.D'Amico AV, Renshaw AA, Cote K, et al. Impact of the percentage of positive prostate cores on prostate cancer-specific mortality for patients with low or favorable intermediate-risk disease. J Clin Oncol. 2004;22:3726–3732. doi: 10.1200/JCO.2004.01.164. [DOI] [PubMed] [Google Scholar]
- 5.Linson PW, Lee AK, Doytchinova T, et al. Percentage of core lengths involved with prostate cancer: does it add to the percentage of positive prostate biopsies in predicting postoperative prostate-specific antigen outcome for men with intermediate-risk prostate cancer. Urology. 2002;59:704–708. doi: 10.1016/S0090-4295(01)01665-X. [DOI] [PubMed] [Google Scholar]
- 6.Freedland SJ, Aronson WJ, Csathy GS, et al. Comparison of percentage of total prostate needle biopsy tissue with cancer to percentage of cores with cancer for predicting PSA recurrence after radical prostatectomy: results from the SEARCH database. Urology. 2003;61:742–747. doi: 10.1016/S0090-4295(02)02525-6. [DOI] [PubMed] [Google Scholar]
- 7.Hu JC, Chang E, Natarajan S, et al. Targeted prostate biopsy in select men for active surveillance: do the Epstein criteria still apply? J Urol. 2014;192:385–390. doi: 10.1016/j.juro.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Epstein JI. An update of the Gleason grading system. J Urol. 2010;183:433–440. doi: 10.1016/j.juro.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 9.Fütterer JJ, Briganti A, De Visschere P, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol. 2015;68:1045–1053. doi: 10.1016/j.eururo.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Epstein JI, Zelefsky MJ, Sjoberg DD, et al. A contemporary prostate cancer grading system: a validated alternative to the Gleason score. Eur Urol. 2016;69:428–435. doi: 10.1016/j.eururo.2015.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gulati R, Cheng HH, Lange PH, Nelson PS, Etzioni R. Screening men at increased risk for prostate Cancer diagnosis: model estimates of benefits and harms. Cancer Epidemiol Biomarkers Prev. 2017;26:222–227. doi: 10.1158/1055-9965.EPI-16-0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bratan F, Niaf E, Melodelima C, et al. Influence of imaging and histological factors on prostate cancer detection and localisation on multiparametric MRI: a prospective study. Eur Radiol. 2013;23:2019–2029. doi: 10.1007/s00330-013-2795-0. [DOI] [PubMed] [Google Scholar]
- 13.Selnaes KM, Heerschap A, Jensen LR, et al. Peripheral zone prostate cancer localization by multiparametric magnetic resonance at 3 T: unbiased cancer identification by matching to histopathology. Invest Radiol. 2012;47:624–633. doi: 10.1097/RLI.0b013e318263f0fd. [DOI] [PubMed] [Google Scholar]
- 14.Turkbey B, Mani H, Shah V, et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186:1818–1824. doi: 10.1016/j.juro.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le JD, Tan N, Shkolyar E, et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol. 2015;67:569–576. doi: 10.1016/j.eururo.2014.08.079. [DOI] [PubMed] [Google Scholar]
- 16.Hambrock T, Hoeks C, Hulsbergen-van de Kaa C, et al. Prospective assessment of prostate cancer aggressiveness using 3-T diffusion-weighted magnetic resonance imaging-guided biopsies versus a systematic 10-core transrectal ultrasound prostate biopsy cohort. Eur Urol. 2012;61:177–184. doi: 10.1016/j.eururo.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 17.Kobus T, Hambrock T, Hulsbergen-van de Kaa CA, et al. In vivo assessment of prostate cancer aggressiveness using magnetic resonance spectroscopic imaging at 3 T with an endorectal coil. Eur Urol. 2011;60:1074–1080. doi: 10.1016/j.eururo.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Wang L, Mazaheri Y, Zhang J, Ishill NM, Kuroiwa K, Hricak H. Assessment of biologic aggressiveness of prostate cancer: correlation of MR signal intensity with Gleason grade after radical prostatectomy. Radiology. 2008;246:168–176. doi: 10.1148/radiol.2461070057. [DOI] [PubMed] [Google Scholar]
- 19.Bratan F, Melodelima C, Souchon R, et al. How accurate is multiparametric MR imaging in evaluation of prostate cancer volume. Radiology. 2015;275:144–154. doi: 10.1148/radiol.14140524. [DOI] [PubMed] [Google Scholar]
- 20.Sun C, Chatterjee A, Yousuf A, et al. Comparison of T2-weighted imaging, DWI, and dynamic contrast-enhanced MRI for calculation of prostate cancer index lesion volume: correlation with whole-mount pathology. AJR Am J Roentgenol. 2019;212:351–356. doi: 10.2214/AJR.18.20147. [DOI] [PubMed] [Google Scholar]
- 21.Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS prostate imaging - reporting and data system: 2015, version 2. Eur Urol. 2016;69:16–40. doi: 10.1016/j.eururo.2015.08.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barentsz JO, Weinreb JC, Verma S, et al. Synopsis of the PI-RADS v2 guidelines for multiparametric prostate magnetic resonance imaging and recommendations for use. Eur Urol. 2016;69:41–49. doi: 10.1016/j.eururo.2015.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woo S, Suh CH, Kim SY, Cho JY, Kim SH. Diagnostic performance of prostate imaging reporting and data system version 2 for detection of prostate cancer: a systematic review and diagnostic meta-analysis. Eur Urol. 2017;72:177–188. doi: 10.1016/j.eururo.2017.01.042. [DOI] [PubMed] [Google Scholar]
- 24.Carroll PH, Mohler JL. NCCN guidelines update: prostate cancer and prostate cancer early detection. J Nat Comp Canc Netw. 2018;16(5S):620–623. doi: 10.6004/jnccn.2018.0036. [DOI] [PubMed] [Google Scholar]
- 25.NICE (2014) Prostate cancer: diagnosis and management. Available via https://www.nice.org.uk/guidance/cg175. Accessed on 7 March 2019
- 26.Rozet F, Hennequin C, Beauval JB, et al. French ccAFU guidelines - update 2018-2020: prostate cancer. Prog Urol. 2018;28:S79–S130. doi: 10.1016/j.purol.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 27.Donovan JL, Young GJ, Walsh EI, et al. A prospective cohort and extended comprehensive-cohort design provided insights about the generalizability of a pragmatic trial: the ProtecT prostate cancer trial. J Clin Epidemiol. 2018;96:35–46. doi: 10.1016/j.jclinepi.2017.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mambourg F, Jonckheer P, Piérart J, Van Brabandt H (2012) A national clinical practice guideline on the management of localised prostate cancer. Belgian Health Care Knowledge Centre (KCE), KCE reports 194C. http://kce.fgov.be/sites/default/files/page_documents/KCE_194C_prostate_cancer_0.pdf
- 29.Rozet F, Hennequin C, Beauval JB, et al. CCAFU French national guidelines 2016-2018 on prostate cancer. Prog Urol. 2016;27(Suppl 1):S95–S143. doi: 10.1016/S1166-7087(16)30705-9. [DOI] [PubMed] [Google Scholar]
- 30.de Rooij M, Crienen S, Witjes JA, Barentsz JO, Rovers MM, Grutters JP. Cost-effectiveness of magnetic resonance (MR) imaging and MR-guided targeted biopsy versus systematic transrectal ultrasound-guided biopsy in diagnosing prostate cancer: a modelling study from a health care perspective. Eur Urol. 2014;66:430–436. doi: 10.1016/j.eururo.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 31.Faria R, Soares MO, Spackman E, et al. Optimising the diagnosis of prostate cancer in the era of multiparametric magnetic resonance imaging: a cost-effectiveness analysis based on the prostate MR imaging study (PROMIS) Eur Urol. 2018;73:23–30. doi: 10.1016/j.eururo.2017.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moldovan PC, Van den Broeck T, Sylvester R, et al. What is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate Cancer at biopsy? A systematic review and meta-analysis from the European Association of Urology Prostate cancer Guidelines Panel. Eur Urol. 2017;72:250–266. doi: 10.1016/j.eururo.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–822. doi: 10.1016/S0140-6736(16)32401-1. [DOI] [PubMed] [Google Scholar]
- 34.Kasivisvanathan Veeru, Rannikko Antti S., Borghi Marcelo, Panebianco Valeria, Mynderse Lance A., Vaarala Markku H., Briganti Alberto, Budäus Lars, Hellawell Giles, Hindley Richard G., Roobol Monique J., Eggener Scott, Ghei Maneesh, Villers Arnauld, Bladou Franck, Villeirs Geert M., Virdi Jaspal, Boxler Silvan, Robert Grégoire, Singh Paras B., Venderink Wulphert, Hadaschik Boris A., Ruffion Alain, Hu Jim C., Margolis Daniel, Crouzet Sébastien, Klotz Laurence, Taneja Samir S., Pinto Peter, Gill Inderbir, Allen Clare, Giganti Francesco, Freeman Alex, Morris Stephen, Punwani Shonit, Williams Norman R., Brew-Graves Chris, Deeks Jonathan, Takwoingi Yemisi, Emberton Mark, Moore Caroline M. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. New England Journal of Medicine. 2018;378(19):1767–1777. doi: 10.1056/NEJMoa1801993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van der Leest Marloes, Cornel Erik, Israël Bas, Hendriks Rianne, Padhani Anwar R., Hoogenboom Martijn, Zamecnik Patrik, Bakker Dirk, Setiasti Anglita Yanti, Veltman Jeroen, van den Hout Huib, van der Lelij Hans, van Oort Inge, Klaver Sjoerd, Debruyne Frans, Sedelaar Michiel, Hannink Gerjon, Rovers Maroeska, Hulsbergen-van de Kaa Christina, Barentsz Jelle O. Head-to-head Comparison of Transrectal Ultrasound-guided Prostate Biopsy Versus Multiparametric Prostate Resonance Imaging with Subsequent Magnetic Resonance-guided Biopsy in Biopsy-naïve Men with Elevated Prostate-specific Antigen: A Large Prospective Multicenter Clinical Study. European Urology. 2019;75(4):570–578. doi: 10.1016/j.eururo.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 36.Moore CM, Kasivisvanathan V, Eggener S, et al. Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: recommendations from an International Working Group. Eur Urol. 2013;64:544–552. doi: 10.1016/j.eururo.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 37.Venderink Wulphert, van Luijtelaar Annemarijke, Bomers Joyce G.R., van der Leest Marloes, Hulsbergen-van de Kaa Christina, Barentsz Jelle O., Sedelaar J.P. Michiel, Fütterer Jurgen J. Results of Targeted Biopsy in Men with Magnetic Resonance Imaging Lesions Classified Equivocal, Likely or Highly Likely to Be Clinically Significant Prostate Cancer. European Urology. 2018;73(3):353–360. doi: 10.1016/j.eururo.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 38.Panebianco Valeria, Barchetti Giovanni, Simone Giuseppe, Del Monte Maurizio, Ciardi Antonio, Grompone Marcello Domenico, Campa Riccardo, Indino Elena Lucia, Barchetti Flavio, Sciarra Alessandro, Leonardo Costantino, Gallucci Michele, Catalano Carlo. Negative Multiparametric Magnetic Resonance Imaging for Prostate Cancer: What's Next? European Urology. 2018;74(1):48–54. doi: 10.1016/j.eururo.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Baco E, Ukimura O, Rud E, et al. Magnetic resonance imaging-transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol. 2015;67:787–794. doi: 10.1016/j.eururo.2014.08.077. [DOI] [PubMed] [Google Scholar]
- 40.Delongchamps Nicolas Barry, Lefèvre Arnaud, Bouazza Naïm, Beuvon Frédéric, Legman Paul, Cornud François. Detection of Significant Prostate Cancer with Magnetic Resonance Targeted Biopsies—Should Transrectal Ultrasound-Magnetic Resonance Imaging Fusion Guided Biopsies Alone be a Standard of Care? Journal of Urology. 2015;193(4):1198–1204. doi: 10.1016/j.juro.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 41.Costa DN, Lotan Y, Rofsky NM, et al. Assessment of prospectively assigned Likert scores for targeted magnetic resonance imaging-transrectal ultrasound fusion biopsies in patients with suspected prostate cancer. J Urol. 2016;195:80–87. doi: 10.1016/j.juro.2015.07.080. [DOI] [PubMed] [Google Scholar]
- 42.Habchi H, Bratan F, Paye A, et al. Value of prostate multiparametric magnetic resonance imaging for predicting biopsy results in first or repeat biopsy. Clin Radiol. 2014;69:e120–e128. doi: 10.1016/j.crad.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 43.Mozer P, Rouprêt M, Le Cossec C, et al. First round of targeted biopsies using magnetic resonance imaging/ultrasonography fusion compared with conventional transrectal ultrasonography-guided biopsies for the diagnosis of localised prostate cancer. BJU Int. 2015;115:50–57. doi: 10.1111/bju.12690. [DOI] [PubMed] [Google Scholar]
- 44.Cash H, Maxeiner A, Stephan C, et al. The detection of significant prostate cancer is correlated with the prostate imaging reporting and data system (PI-RADS) in MRI/transrectal ultrasound fusion biopsy. World J Urol. 2016;34:525–532. doi: 10.1007/s00345-015-1671-8. [DOI] [PubMed] [Google Scholar]
- 45.Schimmöller L, Quentin M, Arsov C, et al. MR-sequences for prostate cancer diagnostics: validation based on the PI-RADS scoring system and targeted MR-guided in-bore biopsy. Eur Radiol. 2014;24:2582–2589. doi: 10.1007/s00330-014-3276-9. [DOI] [PubMed] [Google Scholar]
- 46.Mertan FV, Greer MD, Shih JH, et al. Prospective evaluation of the prostate imaging reporting and data system version 2 for prostate cancer detection. J Urol. 2016;196:690–696. doi: 10.1016/j.juro.2016.04.057. [DOI] [PubMed] [Google Scholar]
- 47.Valerio M, Donaldson I, Emberton M, et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol. 2015;68:8–19. doi: 10.1016/j.eururo.2014.10.026. [DOI] [PubMed] [Google Scholar]
- 48.Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol. 2015;68:438–450. doi: 10.1016/j.eururo.2014.11.037. [DOI] [PubMed] [Google Scholar]
- 49.Schouten MG, van der Leest M, Pokorny M, et al. Why and where do we miss significant prostate cancer with multi-parametric magnetic resonance imaging followed by magnetic resonance-guided and Transrectal ultrasound-guided biopsy in biopsy-naive men? Eur Urol. 2017;71:896–903. doi: 10.1016/j.eururo.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 50.De Visschere PJ, Naesens L, Libbrecht L, et al. What kind of prostate cancers do we miss on multiparametric magnetic resonance imaging? Eur Radiol. 2016;26:1098–1107. doi: 10.1007/s00330-015-3894-x. [DOI] [PubMed] [Google Scholar]
- 51.Haffner J, Lemaitre L, Puech P, et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int. 2011;108:E171–E178. doi: 10.1111/j.1464-410X.2011.10112.x. [DOI] [PubMed] [Google Scholar]
- 52.Moore CM, Robertson NL, Arsanious N, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013;63:125–140. doi: 10.1016/j.eururo.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 53.Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–397. doi: 10.1001/jama.2014.17942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rouvière O, Puech P, Renard-Penna R, et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol. 2019;20:100–109. doi: 10.1016/S1470-2045(18)30569-2. [DOI] [PubMed] [Google Scholar]
- 55.Patel N, Cricco-Lizza E, Kasabwala K, et al. The role of systematic and targeted biopsies in light of overlap on magnetic resonance imaging ultrasound fusion biopsy. Eur Urol Oncol. 2018;1:263–267. doi: 10.1016/j.euo.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 56.Radtke JP, Wiesenfarth M, Kesch C, et al. Combined clinical parameters and multiparametric magnetic resonance imaging for advanced risk modeling of prostate cancer-patient-tailored risk stratification can reduce unnecessary biopsies. Eur Urol. 2017;72:888–896. doi: 10.1016/j.eururo.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 57.Distler FA, Radtke JP, Bonekamp D, et al. The value of PSA density in combination with PI-RADS for the accuracy of prostate cancer prediction. J Urol. 2017;198:575–582. doi: 10.1016/j.juro.2017.03.130. [DOI] [PubMed] [Google Scholar]
- 58.Mehralivand S, Shih JH, Rais-Bahrami S, et al. A magnetic resonance imaging-based prediction model for prostate biopsy risk stratification. JAMA Oncol. 2018;4:678–685. doi: 10.1001/jamaoncol.2017.5667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schoots IG. MRI in early prostate cancer detection: how to manage indeterminate or equivocal PI-RADS 3 lesions? Transl Androl Urol. 2018;7:70–82. doi: 10.21037/tau.2017.12.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Felker ER, Raman SS, Margolis DJ, et al. Risk stratification among men with prostate imaging reporting and data system version 2 category 3 transition zone lesions: is biopsy always necessary? AJR Am J Roentgenol. 2017;209:1272–1277. doi: 10.2214/AJR.17.18008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Niu XK, Li J, Das SK, Xiong Y, Yang CB, Peng T. Developing a nomogram based on multiparametric magnetic resonance imaging for forecasting high-grade prostate cancer to reduce unnecessary biopsies within the prostate-specific antigen gray zone. BMC Med Imaging. 2017;17:11. doi: 10.1186/s12880-017-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shukla-Dave A, Hricak H, Akin O, et al. Preoperative nomograms incorporating magnetic resonance imaging and spectroscopy for prediction of insignificant prostate cancer. BJU Int. 2012;109:1315–1322. doi: 10.1111/j.1464-410X.2011.10612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vilanova JC, Barceló-Vidal C, Comet J, et al. Usefulness of prebiopsy multifunctional and morphologic MRI combined with free-to-total prostate-specific antigen ratio in the detection of prostate cancer. AJR Am J Roentgenol. 2011;196:W715–W722. doi: 10.2214/AJR.10.5700. [DOI] [PubMed] [Google Scholar]
- 64.Hansen NL, Barrett T, Koo B, et al. The influence of prostate-specific antigen density on positive and negative predictive values of multiparametric magnetic resonance imaging to detect Gleason score 7-10 prostate cancer in a repeat biopsy setting. BJU Int. 2017;119:724–730. doi: 10.1111/bju.13619. [DOI] [PubMed] [Google Scholar]
- 65.Washino S, Okochi T, Saito K, et al. Combination of prostate imaging reporting and data system (PI-RADS) score and prostate-specific antigen (PSA) density predicts biopsy outcome in prostate biopsy naive patients. BJU Int. 2017;119:225–233. doi: 10.1111/bju.13465. [DOI] [PubMed] [Google Scholar]
- 66.Liddell H, Jyoti R, Haxhimolla HZ. mp-MRI prostate characterised PIRADS 3 lesions are associated with a low risk of clinically significant prostate cancer - a retrospective review of 92 biopsied PIRADS 3 lesions. Curr Urol. 2015;8:96–100. doi: 10.1159/000365697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hansen NL, Barrett T, Kesch C, et al. Multicentre evaluation of magnetic resonance imaging supported transperineal prostate biopsy in biopsy-naive men with suspicion of prostate cancer. BJU Int. 2018;122:40–49. doi: 10.1111/bju.14049. [DOI] [PubMed] [Google Scholar]
- 68.Abd-Alazeez M, Kirkham A, Ahmed HU, et al. Performance of multiparametric MRI in men at risk of prostate cancer before the first biopsy: a paired validating cohort study using template prostate mapping biopsies as the reference standard. Prostate Cancer Prostatic Dis. 2014;17:40–46. doi: 10.1038/pcan.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Arsov C, Quentin M, Rabenalt R, Antoch G, Albers P, Blondin D. Repeat transrectal ultrasound biopsies with additional targeted cores according to results of functional prostate MRI detects high-risk prostate cancer in patients with previous negative biopsy and increased PSA - a pilot study. Anticancer Res. 2012;32:1087–1092. [PubMed] [Google Scholar]
- 70.de Rooij M, Hamoen EH, Fütterer JJ, Barentsz JO, Rovers MM. Accuracy of multiparametric MRI for prostate cancer detection: a meta-analysis. AJR Am J Roentgenol. 2014;202:343–351. doi: 10.2214/AJR.13.11046. [DOI] [PubMed] [Google Scholar]
- 71.Grey Alistair D.R., Chana Manik S., Popert Rick, Wolfe Konrad, Liyanage Sidath H., Acher Peter L. Diagnostic accuracy of magnetic resonance imaging (MRI) prostate imaging reporting and data system (PI-RADS) scoring in a transperineal prostate biopsy setting. BJU International. 2014;115(5):728–735. doi: 10.1111/bju.12862. [DOI] [PubMed] [Google Scholar]
- 72.Pokorny MR, de Rooij M, Duncan E, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol. 2014;66:22–29. doi: 10.1016/j.eururo.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 73.Portalez D, Mozer P, Cornud F, et al. Validation of the European Society of Urogenital Radiology scoring system for prostate cancer diagnosis on multiparametric magnetic resonance imaging in a cohort of repeat biopsy patients. Eur Urol. 2012;62:986–996. doi: 10.1016/j.eururo.2012.06.044. [DOI] [PubMed] [Google Scholar]
- 74.Rosenkrantz Andrew B., Mussi Thais C., Borofsky Michael S., Scionti Stephen S., Grasso Michael, Taneja Samir S. 3.0 T multiparametric prostate MRI using pelvic phased-array coil: Utility for tumor detection prior to biopsy. Urologic Oncology: Seminars and Original Investigations. 2013;31(8):1430–1435. doi: 10.1016/j.urolonc.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 75.Vargas HA, Akin O, Afaq A, et al. Magnetic resonance imaging for predicting prostate biopsy findings in patients considered for active surveillance of clinically low risk prostate cancer. J Urol. 2012;188:1732–1738. doi: 10.1016/j.juro.2012.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rosenkrantz AB, Kim S, Lim RP, et al. Prostate cancer localization using multiparametric MR imaging: comparison of prostate imaging reporting and data system (PI-RADS) and Likert scales. Radiology. 2013;269:482–492. doi: 10.1148/radiol.13122233. [DOI] [PubMed] [Google Scholar]
- 77.Rosenkrantz AB, Lim RP, Haghighi M, Somberg MB, Babb JS, Taneja SS. Comparison of interreader reproducibility of the prostate imaging reporting and data system and likert scales for evaluation of multiparametric prostate MRI. AJR Am J Roentgenol. 2013;201:W612–W618. doi: 10.2214/AJR.12.10173. [DOI] [PubMed] [Google Scholar]
- 78.Vaché T, Bratan F, Mège-Lechevallier F, Roche S, Rabilloud M, Rouvière O. Characterization of prostate lesions as benign or malignant at multiparametric MR imaging: comparison of three scoring systems in patients treated with radical prostatectomy. Radiology. 2014;272:446–455. doi: 10.1148/radiol.14131584. [DOI] [PubMed] [Google Scholar]
- 79.Thompson JE, Moses D, Shnier R, et al. Multiparametric magnetic resonance imaging guided diagnostic biopsy detects significant prostate cancer and could reduce unnecessary biopsies and over detection: a prospective study. J Urol. 2014;192:67–74. doi: 10.1016/j.juro.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 80.Renard-Penna R, Mozer P, Cornud F, et al. Prostate imaging reporting and data system and Likert scoring system: multiparametric MR imaging validation study to screen patients for initial biopsy. Radiology. 2015;275:458–468. doi: 10.1148/radiol.14140184. [DOI] [PubMed] [Google Scholar]
- 81.Muller BG, Shih JH, Sankineni S, et al. Prostate cancer: interobserver agreement and accuracy with the revised prostate imaging reporting and data system at multiparametric MR imaging. Radiology. 2015;277:741–750. doi: 10.1148/radiol.2015142818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kasel-Seibert M, Lehmann T, Aschenbach R, et al. Assessment of PI-RADS v2 for the detection of prostate cancer. Eur J Radiol. 2016;85:726–731. doi: 10.1016/j.ejrad.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 83.Zhao C, Gao G, Fang D, et al. The efficiency of multiparametric magnetic resonance imaging (mpMRI) using PI-RADS version 2 in the diagnosis of clinically significant prostate cancer. Clin Imaging. 2016;40:885–888. doi: 10.1016/j.clinimag.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 84.Rosenkrantz AB, Ginocchio LA, Cornfeld D, et al. Interobserver reproducibility of the PI-RADS version 2 lexicon: a multicenter study of six experienced prostate radiologists. Radiology. 2016;280:793–804. doi: 10.1148/radiol.2016152542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Polanec S, Helbich TH, Bickel H, et al. Head-to-head comparison of PI-RADS v2 and PI-RADS v1. Eur J Radiol. 2016;85:1125–1131. doi: 10.1016/j.ejrad.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 86.Tewes S, Mokov N, Hartung D, et al. Standardized reporting of prostate MRI: comparison of the prostate imaging reporting and data system (PI-RADS) version 1 and version 2. PLoS One. 2016;11:e0162879. doi: 10.1371/journal.pone.0162879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Greer MD, Brown AM, Shih JH, et al. Accuracy and agreement of PIRADSv2 for prostate cancer mpMRI: a multireader study. J Magn Reson Imaging. 2017;45:579–585. doi: 10.1002/jmri.25372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hansen NL, Koo BC, Gallagher FA, et al. Comparison of initial and tertiary centre second opinion reads of multiparametric magnetic resonance imaging of the prostate prior to repeat biopsy. Eur Radiol. 2017;27:2259–2266. doi: 10.1007/s00330-016-4635-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 30.8 kb)