Abstract
An accurate diagnosis of clinically distinct subgroups of aggressive mature B cell lymphomas is crucial for the choice of proper treatment. Presently, precise recognition of these disorders relies on the combination of morphological, immunophenotypical, and cytogenetic/molecular features. The diagnostic workup in such situations implies the application of costly and time-consuming analyses, which are not always required, since an intensified treatment option is reasonably reserved to fit patients. The Italian Group of Haematopathology proposes herein a practical algorithm for the diagnosis of aggressive mature B cell lymphomas based on a stepwise approach, aimed to select cases deserving molecular analysis, in order to optimize time and resources still assuring the optimal management for any patient.
Keywords: HGBL, Double hit, DLBCL, Diagnosis, FISH, MYC
Introduction
Diffuse large B cell lymphomas not otherwise specified (DLBCL NOS) represent a spectrum of malignancies associated with diversified clinical outcomes. Characterization of molecular features of clinical importance, such as the cell of origin (COO) and the rearrangements of MYC, BCL2, and BCL6 genes, has been incorporated as a new requirement in the revised World Health Organization (WHO) classification of tumors of hematopoietic and lymphoid tissues [1].
Gene expression profiling (GEP) or surrogated immunohistochemical algorithms allow subclassification of DLBCL NOS mainly into the germinal center (GCB) and the activated (ABC) or non-GCB types based on the cell of origin, with ABC lymphomas displaying poorer prognosis than GCB ones [2]. pt?>Fluorescence in situ hybridization (FISH) is required to distinguish among high-grade B cell lymphomas with double or triple hit rearrangement (HGBL DH/TH), high-grade B cell lymphomas not otherwise specified (HGBL NOS), and DLBCL NOS. HGBL DH/TH are aggressive mature B cell lymphomas with variable morphology, ranging from pleomorphic large cells to medium-sized cells with features intermediate between DLBCL and Burkitt lymphoma (BCLU), to blastoid cells (Fig. 1), where FISH analyses identify MYC gene rearrangement in association with BCL2 and/or BCL6 gene rearrangements (Fig. 2). Notably, HGBL DH/TH account for approximately 5% of all cases with DLBCL morphology and generally have a low complete response rate with R-CHOP that advises for more intensive chemotherapy regimens [1, 3]. HGBL NOS includes cases with neoplastic B cells having either blastoid morphology or histopathological features intermediate between DLBCL and Burkitt Lymphoma (BCLU) that do not carry a double or a triple rearrangement. Recently, gene expression signatures and mutational profiles identified high-risk patients with DLBCL comprising double hit lymphomas [4].
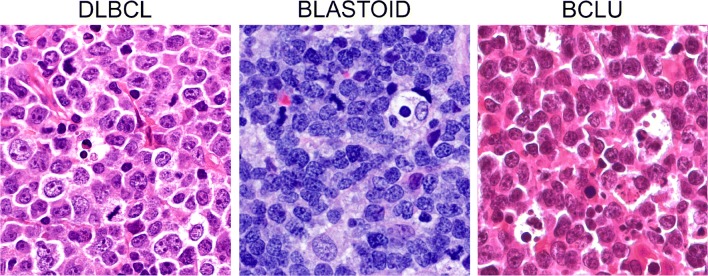
Fig. 1.
Morphological features of aggressive mature B cell lymphomas. In DLBCL, the cells are pleomorphic with centroblastic and/or immunoblastic features. Blastoid cells are medium-sized cells with a fine chromatin pattern and inconspicuous nucleoli. Cases with features overlapping between BL and DLBCL (BCLU) show medium-sized cells, less monomorphic than in classical BL, with multiple paracentrally located nucleoli and frequent starry sky pattern
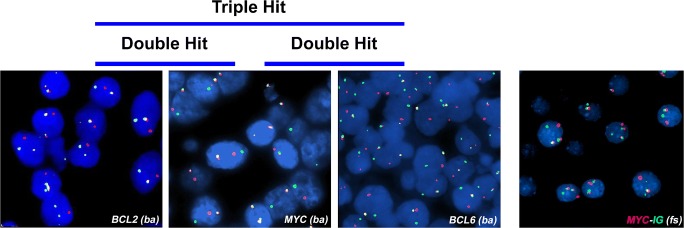
Fig. 2.
Interphase FISH showing rearrangements of MYC, BCL2, and BCL6 genes using dual color break-apart (BA) probes. MYC/IGH translocation is detected using a dual color dual fusion FISH probe
GEP and FISH studies, which are the elective technologies for the definition of the COO, of gene rearrangements and of high-risk lymphomas are expensive, time consuming, and not available in all laboratories. To date, no guidelines are available driving both pathologists and clinicians in the selection of aggressive mature B cell lymphomas deserving molecular analyses in a cost-effective management of the patients. The use of immunohistochemistry, cheaper and widely applicable, as surrogate tool for the assessment of the COO and the presence of MYC gene rearrangements in DLBCLs have been proposed [5–8]. However, this approach bears intrinsic limitations. Although HGBL-DH overexpress MYC and BCL2 proteins in most instances, they only account for a small proportion of the so-called double expressors DLBCL (DE DLBCL). In addition, HGBL carrying MYC and BCL2 gene rearrangements almost exclusively belong to the GCB category, while the majority of DE DLBCL fall into the non-GCB group [3, 8]. Of note, nearly 20% of GCB DLBCL carrying MYC rearrangement do not express MYC protein [8].
On the other hand, molecular subtyping all DLBCLs to identify all HGBL DH/TH may be unnecessary, since treatment choice is also driven by patient’s age, comorbidities, and performance status, with dose-intense treatment options being usually reserved to fit and young (age < 60 years) patients.
The purpose of this article is to propose a stepwise, working algorithm aimed at the rationalization of the diagnostic efforts in aggressive mature B cell lymphomas. The attempt is to provide minimal required criteria to select cases deserving FISH analysis, in order to save time and resources still assuring the optimal management for any patient.
Sample requirements
This diagnostic workflow applies to any nodal/extranodal, aggressive mature B cell lymphoma that does not fulfill the diagnostic criteria of any specific DLBCL entity (e.g., EBV+ DLBCL, primary mediastinal B cell lymphoma, primary central nervous system DLBCL, T cell histiocyte-rich DLBCL) as recommended by the revised version of the World Health Organization classification of lymphoid malignancies.
In order to enable all the required immunohistochemical and molecular analyses and avoid pre-analytical biases, samples should contain an adequate amount of tissue embedded in paraffin within 24 h of formalin fixation. Since core needle biopsies might not be fully informative to render an accurate diagnosis of lymphoma, excisional lymph node biopsies should be favored whenever possible.
Diagnostic workflow
An initial diagnosis of an aggressive mature B cell lymphoma should incorporate the assessment of cytological and immunohistochemical features, including the COO, and the percentage of MYC- and BCL2-expressing cells. Whenever a B cell lymphoma with a DLBCL morphology displays either a GCB COO and/or a double expression of MYC and BCL2 proteins (in more than 40% and 50% of neoplastic cells, respectively) (DE DLBCL), analysis of MYC, BCL2, and BCL6 gene rearrangements by FISH is indicated in order to rule out the possibility of a HGBL DH/TH. Although there is no complete agreement about the percentage of MYC protein-expressing cells that accurately predicts the presence of MYC gene rearrangement [6, 9, 10], the cutoff value of 70% has been recently reported to be reproducible among different centers and of clinical value in identifying patients with a worse prognosis [7].
Before proceeding with FISH analysis, in DLBCL cases, it is highly recommended to discuss upfront with the referring hematologist the results of immunohistochemical screening in order to verify patient’s fitness and potential eligibility to undergo intensified therapy for HGBL DH/TH.
On the contrary, FISH analyses should be performed in any case of:
B cell lymphomas with blastoid morphology, with the exclusion of TdT+ lymphoblastic lymphoma or cyclin D1+ pleomorphic/blastoid mantle cell lymphoma (Fig. 3). In these cases, FISH analysis for MYC, BCL2, and BCL6 genes allows classification of the malignancy as HGBL DH/TH or HGBL NOS. CCDN1 translocations should also be investigated to rule out cyclin D1-expressing DLBCL.
B cell lymphomas with morphological features intermediate between DLBCL and Burkitt lymphoma (BCLU). In these cases, independently of the immunophenotype exhibited by tumor cells, MYC, BCL2, and BCL6 rearrangements should be investigated for the differential diagnosis among HGBL DH/TH, HGBL NOS, and Burkitt lymphoma (Fig. 3). In cases without MYC translocation, FISH analysis for chromosome 11q is required to identify Burkitt-like lymphomas with 11q aberrations.
Fig. 3.
Diagnostic workflow for the diagnosis of aggressive mature B cell lymphomas . The workflow applies to DLBCLs that don’t fulfill the inclusion criteria for the specific DLBCL entities (i.e. primary mediastinal B cell lymphoma (PMBCL), intravascular DLBCL, EBV+ DLBCL, T cell rich histiocyte rich B cell lymphoma (TCRHRBCL), etc (*) and to blastoid lymphomas excluding lymphoblastic lymphomas and mantle cell lymphomas (**). In DLBCL discussion with the referring hematologist is highly recommended before proceeding with FISH analyses (***).
Immunohistochemistry
Aggressive mature B cell lymphomas should express B cell–associated antigens (e.g., CD20, CD19, CD79a) and lack cyclin D1. In the case of a cyclin D1+ large B cell lymphoma, immunohistochemistry for CD5, SOX11, and FISH analysis with a CCND1 break-apart probe must be performed in order to rule out a pleomorphic/blastoid mantle cell lymphoma [1]. The use of CD5 is also encouraged to identify de novo CD5+ DLBCLs, which might display an unfavorable outcome [11].
The COO of DLBCL can be investigated by gene expression profiling (GEP) or, alternatively, by immunohistochemistry (IHC) following algorithms suggested by the 2017 WHO Classification [1]. Among these, the most popular is Hans algorithm, which splits DLBCLs in germinal center (GCB) and non-germinal center (non-GCB) type based on the expression of CD10, BCL6, and IRF4/MUM1 proteins [12]. Its output shows reasonable correlation with the GEP, although some cases of DLBCL GCB type are misclassified as non-GCB type by IHC [5]. In addition to its role in discriminating different DLBCL prognostic subgroups (non-GCB carrying worse prognosis in comparison with GCB type), determination of COO might help in identifying those cases potentially harboring rearrangements of MYC, BCL2, and BCL6. Indeed, almost all the HGBL DH/TH fall within the GCB subtype with less than 1% of ABC harboring MYC and BCL2 and 2% MYC and BCL6 rearrangements [3].
Immunohistochemical investigation of MYC and BCL2 protein expression in DLBCL is highly recommended since overexpression of these proteins is associated with shorter survival [10, 13, 14]. Moreover, HGBL DH without MYC or BCL2 overexpression display a more favorable outcome than double expressor HGBL DH [7, 10, 13, 14]. Cutoff values for MYC and BCL2 that have been significantly associated with survival are 40% and 50%, respectively (independently of the intensity of the staining) [9]. Whenever the IHC staining is not homogeneously distributed across the section, the percentage of positive cells should be calculated as the average, and the occurrence of hot spots with MYC > 70% should be reported. A high percentage of MYC+ cells is more likely to be associated with MYC translocation [6, 7, 9]. Some pathologists have advocated the use of Ki67 staining, although the proliferative fraction is variable in HGBL DH/TH and it cannot be considered a reliable marker for screening patients that require FISH [1, 10].
FISH analysis
Rearrangements of MYC, BCL2, and BCL6 genes are generally assessed using break-apart probes. Since the definition of HGBL DH/TH requires the presence of MYC rearrangement, this could be investigated first, followed by BCL2 and BCL6 gene analyses in MYC rearranged cases. The use of dual color dual fusion IGH-MYC probes in addition to MYC break-apart probes (Fig. 2) increases the sensitivity of detection [14]. Furthermore, the definition of the partner gene (IGH or non-IGH) of MYC translocation could be clinically relevant, although this issue is still debated [9, 14, 15]. By an administrative standpoint, FISH analysis could be requested as an additional investigation either by the clinician or by the pathologist according to local rules.
Concluding remarks
In conclusion, we believe that the application of the proposed workflow could represent a useful strategy to rationalize the procedures and optimize the resources, speeding up the diagnosis of aggressive mature B cell lymphomas and allowing the more appropriate treatment option for each patient.
Acknowledgments
Di A, Napoli, Remotti D, and Ruco L are contributors on behalf of Lazio Group of Haematopathologist composed by: Anemona Lucia, Bakacs Arianna, Bianchi Antonella, Cancellario Francesca, Caruso Lia, De Vito Rita, Di Cristofano Claudio, Di Napoli Arianna, Fratoni Stefano, Giacobbi Erica, Giordano Carla, Gomes Enzo Vito, Licci-Stefano, Ruco Luigi, Macciomei-M. Cristina, Marino Mirella, Monardo-Francesca, Pescarmona Edoardo, Ramieri Maria Teresa, Remotti Daniele, Riminucci Mara, Stella Francesca, Taccogna Silvia, Uccini Stefania.
Authors’ contribution
DNA, RD, and RL conceived the study. DNA wrote the manuscript. FF provided histological and FISH images. RD, AC, AMR,AS, CA, FF, LS, LL, LM, ND, PS, PM, SE, TC, and ZA contributed in writing and revising critically the manuscript for important intellectual content. PM and RL supervised the study and revised the manuscript.
Compliance with ethical standards
Research involving human participants and/or animals
Not applicable.
Informed consent
Since this is a position paper, formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
This article is part of the Topical Collection on Quality in Pathology
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
M. Paulli and L. Ruco contributed equally to this work.
Change history
10/29/2019
The first and family names of the authors were interchanged and are now presented correctly. The original article has been corrected
References
- 1.Swerdlow SH, Campo E, Harris NL, et al. World Health Organization Classification of Tumours. Revised. 4. Lyon: International Agency of Research on Cancer; 2017. WHO classification of tumours of haematopoietic and lymphoid tissues. [Google Scholar]
- 2.Alizadeh AA, Eisen MB, Davis RE, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;03(6769):503–511. doi: 10.1038/35000501. [DOI] [PubMed] [Google Scholar]
- 3.Sesques P, Johnson NA. Approach to the diagnosis and treatment of high-grade B-cell lymphomas with MYC and BCL2 and/or BCL6 rearrangements. Blood. 2017;129(3):280–288. doi: 10.1182/blood-2016-02-636316. [DOI] [PubMed] [Google Scholar]
- 4.Chan WC. Using gene expression profiling to move beyond MYC/BCL2 rearrangements in high-grade lymphoma. J Clin Oncol. 2019;37(3):175–177. doi: 10.1200/JCO.18.01910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gutiérrez-García G, Cardesa-Salzmann T, Climent F, et al. Gene-expression profiling and not immunophenotypic algorithms predicts prognosis in patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Blood. 2011;117(18):4836–4843. doi: 10.1182/blood-2010-12-322362. [DOI] [PubMed] [Google Scholar]
- 6.Green TM, Nielsen O, de Stricker K, Xu-Monette ZY, Young KH, Møller MB. High levels of nuclear MYC protein predict the presence of MYC rearrangement in diffuse large B-cell lymphoma. Am J Surg Pathol. 2012;236(4):612–619. doi: 10.1097/PAS.0b013e318244e2ba. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosio MR, Lazzi S, Lo Bello G, et al. MYC protein expression scoring and its impact on the prognosis of aggressive B-cell lymphoma patients. Haematologica. 2019;104(1):e25–e28. doi: 10.3324/haematol.2018.195958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott DW, King RL, Staiger AM, Ben-Neriah S, Jiang A, Horn H, Mottok A, Farinha P, Slack GW, Ennishi D, Schmitz N, Pfreundschuh M, Nowakowski GS, Kahl BS, Connors JM, Gascoyne RD, Ott G, Macon WR, Rosenwald A. High-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements with diffuse large B-cell lymphoma morphology. Blood. 2018;131(18):2060–2064. doi: 10.1182/blood-2017-12-820605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copie-Bergman C, Cuilliere-Dartigues P, Baia M, Briere J, Delarue R, Canioni D, Salles G, Parrens M, Belhadj K, Fabiani B, Recher C, Petrella T, Ketterer N, Peyrade F, Haioun C, Nagel I, Siebert R, Jardin F, Leroy K, Jais JP, Tilly H, Molina TJ, Gaulard P. MYC-IG rearrangements are negative predictors of survival in DLBCL patients treated with immunochemotherapy: a GELA/LYSA study. Blood. 2015;126(22):2466–2474. doi: 10.1182/blood-2015-05-647602. [DOI] [PubMed] [Google Scholar]
- 10.Johnson NA, Slack GW, Savage KJ, Connors JM, Ben-Neriah S, Rogic S, Scott DW, Tan KL, Steidl C, Sehn LH, Chan WC, Iqbal J, Meyer PN, Lenz G, Wright G, Rimsza LM, Valentino C, Brunhoeber P, Grogan TM, Braziel RM, Cook JR, Tubbs RR, Weisenburger DD, Campo E, Rosenwald A, Ott G, Delabie J, Holcroft C, Jaffe ES, Staudt LM, Gascoyne RD. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30(28):3452–3459. doi: 10.1200/JCO.2011.41.0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu-Monette ZY, Tu M, Jabbar KJ, Cao X, Tzankov A, Visco C, Nagarajan L, Cai Q, Montes-Moreno S, An Y, Dybkaer K, Chiu A, Orazi A, Zu Y, Bhagat G, Richards KL, Hsi ED, Choi WW, van Krieken J, Huh J, Ponzoni M, Ferreri AJ, Zhao X, Møller MB, Farnen JP, Winter JN, Piris MA, Miranda RN, Medeiros LJ, Young KH. Clinical and biological significance of de novo CD5+ diffuse large B-cell lymphoma in Western countries. Oncotarget. 2015;6(8):5615–5633. doi: 10.18632/oncotarget.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan Z, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103(1):275–282. doi: 10.1182/blood-2003-05-1545. [DOI] [PubMed] [Google Scholar]
- 13.Green TM, Young KH, Visco C, Xu-Monette ZY, Orazi A, Go RS, Nielsen O, Gadeberg OV, Mourits-Andersen T, Frederiksen M, Pedersen LM, Møller MB. Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30(28):3460–3467. doi: 10.1200/JCO.2011.41.4342. [DOI] [PubMed] [Google Scholar]
- 14.Muñoz-Mármol AM, Sanz C, Tapia G, Marginet R, Ariza A, Mate JL. MYC status determination in aggressive B-cell lymphoma: the impact of FISH probe selection. Histopathology. 2013;63(3):418–424. doi: 10.1111/his.12178. [DOI] [PubMed] [Google Scholar]
- 15.McPhail ED, Maurer MJ, Macon WR, et al. Inferior survival in high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements is not associated with MYC/IG gene rearrangements. Haematologica. 2018;103(11):1899–1907. doi: 10.3324/haematol.2018.190157. [DOI] [PMC free article] [PubMed] [Google Scholar]