Abstract
Introduction
Acne scarring is a common undesirable complication of acne vulgaris. Fractional erbium-yttrium aluminum garnet (YAG) 2940 nm laser and platelet-rich plasma have been used in treating acne scars with variable outcomes. The objective of this study is to assess the efficacy of fractional erbium-YAG 2940 nm laser and platelet-rich plasma as a single line of treatment in comparison with combined treatment in atrophic postacne scars.
Methods
Seventy-five patients were included in this trial and randomized into three equal groups (25 each). Group A was subjected to six sessions of erbium-YAG laser for 6 months, group B was treated with 12 sessions of platelet-rich plasma over the same period, and group C was subjected to six sessions of erbium-YAG laser plus 12 sessions of platelet-rich plasma over the same period. Each subject was evaluated by acne scar grading, photography, and subjective evaluation.
Results
Both treatment modalities showed improvement of acne scars, but the improvement with combined treatment was better than that with erbium-YAG laser or platelet-rich plasma alone regarding scar grade improvement (P = 0.007 and 0.001), clinical improvement (P = 0.001 and 0.001), and patient satisfaction (P = 0.005 and 0.001), respectively.
Conclusions
The combination of platelet-rich plasma plus erbium-YAG laser is superior to either treatment alone for acne scars, with trivial side effects for all treatment modalities.
Trial Registration
ClinicalTrials.gov identifier; NCT03933033.
Keywords: Acne scars, Erbium-YAG laser, Platelet-rich plasma
Introduction
Acne is a skin disease affecting up to 80% of young adults and up to 5% of older adults. Many causes are involved in the pathogenesis of acne, including increased sebum production, follicular hyperkeratinization, colonization with Propionibacterium acnes, inflammatory response, and other unproven factors such as vitamin D deficiency [1, 2].
Acne scars occur as a consequence of inflammatory disorders in the dermis around the hair follicle. They are broadly classified into three types: atrophic, hypertrophic, and keloidal scars. Atrophic scars are the most common type, which can be further classified according to their depth, width, and three-dimensional architecture into rolling, icepick, and boxcar scars [1, 3].
Severe psychological depression and social withdrawal can result from acne scarring, which represent undesirable complications of acne vulgaris [3]. Acne scars can be assessed using many scoring systems, such as the Qualitative Global Grading System presented by Goodman and Baron, which considers the form, type, intensity, and evolution period of the scar [4, 5].
Fractional nonablative resurfacing laser treatment relies on a unique mechanism of action that repairs a fraction of the skin at a time. Laser is used to resurface the epidermis and at the same time heat the dermis to promote formation of new collagen [6]. Fractional erbium-YAG laser 2940 nm (Er-YAG) treatment targets both the epidermis and dermis, creating small zones of microdamage separated by zones of nondamaged tissue that favor a rapid healing process and treatment of acne scarring. It has minimal complications and side effects such as erythema and postinflammatory hyperpigmentation (PIH) [5, 7].
Platelet-rich plasma (PRP) is an autologous concentration of human platelets in a small volume of plasma. It contains growth factors, especially epidermal growth factor, platelet-derived growth factor, transforming growth factor beta (TGF-b), and vascular endothelial growth factor [8]. These factors are known to regulate various processes including cell migration, attachment, proliferation, and differentiation and to promote extracellular matrix production by binding to specific cell surface receptors [9]. It is used in many fields of dermatology nowadays to promote wound healing and accelerate new collagen formation. It can also be used as a treatment option in acne scarring [10–12]. PRP has minor side effects such as erythema and painful injection [3, 10, 11].
Although there are many choices for treatment of acne scarring, to date there is no standard line of therapy. The aim of the current study is to compare the efficacy and safety of combined autologous PRP with Er-YAG laser for treatment of atrophic acne scars versus Er-YAG or PRP alone.
Methods
Patients
This randomized clinical trial (RCT) was performed at the Outpatient Clinic of Dermatology, Venerology and Andrology Department, South Valley University on 75 patients with atrophic postacne scars in the period from June 2017 to August 2018.
The sample size calculation was carried out using G*Power-3 software [13]. A minimum sample size of 75 acne scar patients (divided into three equal groups: 25 PRP, 25 Er-YAG laser, and 25 combined treatment) was calculated to detect an effect size of 0.3 in the percentage improvement, with an error probability of 0.05 and 90% power in a two-tailed test.
Patients with no active acne or only atrophic postacne scars as classified based on Goodman and Baron’s qualitative classification were included in this trial. Moreover, patients with positive history of keloidal tendency, bleeding tendency, platelet disorder, any acute infection on the face (herpes or folliculitis), human immunodeficiency virus (HIV), hepatitis B surface antigen (HBsAg), or autoimmune diseases, or on immunosuppressive drugs or topical or systemic acne treatments, or who had undergone interventions such as microdermabrasion and needling in the 3 months prior to the study were excluded from the trial.
Randomization
Eligible participants were divided into three equal groups based on randomized coded cards. Randomization was carried out using tables of random numbers arranged in consecutive order. The allocation of patients and follow-up was performed by assistants.
Treatment Protocol
Each group was treated according to the following regimens: Group A was subjected to 12 sessions of intradermal injection of PRP at 2-week intervals. Group B was subjected to six fractional nonablative Er-YAG laser (FotonaXs Dynamis, Slovenia) sessions at 4-week intervals. Group C was subjected to the combination of the two treatment modalities.
Laser Parameters
Five passes in vertical, horizontal, and oblique directions were applied over the scar areas. Parameters for each setting were kept constant for all patients. The first pass was conducted on the entire face area with parameters of energy of 600 mJ in micro-short pulse mode (MSP) with spot size of 7 mm diameter and frequency of 5 Hz. The second pass was applied with the same parameters but to the scar area only. The third pass was applied on the entire face area with parameters of energy of 1000 mJ in short pulse mode (SP) with spot size of 7 mm diameter and frequency of 5 Hz. The fourth pass was applied on the scar area only with parameters of energy of 1200 mJ in short pulse mode (SP) with spot size of 7 mm diameter and frequency of 5 Hz. The fifth pass was applied to the scar area only with parameters of energy of 1500 mJ in extra-long pulse mode (XLP) with spot size of 7 mm diameter and frequency of 5 Hz.
PRP Preparation and Injection
Venous blood (10 mL) was obtained under sterile conditions and collected in sterile tubes containing sodium citrate 3.8%. Each tube was centrifuged at 2000 (rpm) for 7 min. The plasma and buffy coat were gently aspirated from each tube and transferred to another tube (plain tube without anticoagulant). Further centrifugation was carried out at 4000 rpm for 7–10 min, thus obtaining a two-part plasma: an uppermost part consisting of platelet-poor plasma (PPP), and a lower part consisting of PRP.
The mean blood platelet level was 200,000 ± 5000/μL. Although the platelet count of PRP has not been optimized, a platelet concentration of more than 1 million/μL (equal to four to seven times mean levels) is generally regarded as a suitable therapeutic concentration [11]. PRP was injected in acne scars under aseptic precautions using a disposable 27-gauge needle. Treatments were given every 2 weeks for 6 months with a total of 12 sessions.
Outcomes Assessment
Qualitative Scarring Grading System of Goodman and Baron
Patients were evaluated using the pretreatment and posttreatment qualitative scarring grading system for each patient to determine the degree of improvement [4].
Clinical Assessment
Standardized high-resolution digital photographs obtained using identical camera settings (Samsung, Seoul, South Korea) were obtained before the start of treatment and after the end of treatment.
Clinical Improvement
Two nontreating blinded physicians assessed the grade of improvement of skin smoothness by comparing photographs on a four-point scale as grade 4 (> 75%) = excellent, grade 3 (51–75%) = marked, grade 2 (26–50%) = moderate, and grade 1 (0–25%) = minimal improvement.
Clinical Satisfaction
Patient satisfaction was recorded on a four-point scale as grade 4 (highly satisfied), grade 3 (satisfied), grade 2 (neutral), and grade 1 (dissatisfied).
Assessment of Complications
Follow-up for all patients was carried out after 1 week of each session for early complications. The degree of facial erythema was evaluated according to the Clinician Erythema Assessment (CEA) scale, graded as clear, almost clear, mild, and moderate.
Statistical Analysis
Data were verified, coded by the researcher, and analyzed using IBM-SPSS version 21 (©IBM-SPSS Inc., Armonk, NY, USA, 2012). Descriptive statistics (means, standard deviations, and percentages) were calculated. The chi-square test was used to test the significance of differences in the distribution of frequencies among different groups. For continuous variables, the analysis of variance (ANOVA) test was applied to test the mean differences of the data that followed a normal distribution, and the post hoc test was calculated using Bonferroni corrections. P values equal to or less than 0.05 are considered significant.
Compliance with Ethics Guidelines
Approval for this study was obtained from the institutional review board (IRB) of the Faculty of Medicine-South Valley University prior to study execution. The trial was registered on the clinical trial registration website (https://clinicaltrials.gov/, NCT03933033). The study was performed in accordance with the Declaration of Helsinki of 1964 and its later amendments. In addition, all participants were asked to sign a written consent form prior to participation. The informed consent was clear and indicated the purpose, process, benefits, and risks of the study, as well as their freedom to participate or withdraw at any time without any obligation. Furthermore, participant confidentiality and anonymity were ensured by assigning each participant a code number for the purpose of analysis only. The study was not based on any incentives or rewards for the participants.
Results
This trial included 75 patients with atrophic acne scars. Participant age ranged from 18 to 38 years with a mean of 26.7 ± 5.1 years. Twenty-seven patients were male (36%), and 48 patients were female (64%). The mean duration of their postacne scars was 4.6 ± 1.9 (range 1–8 years). There were no statistically significant differences in basic characteristics between the two study groups (Table 1). Moreover, there was no significant difference between the study groups regarding scar duration, skin type, or scar type (Table 1).
Table 1.
Baseline characteristics of the studied groups
| PRP (n = 25) | Er-YAG laser (n = 25) | Both (n = 25) | |
|---|---|---|---|
| Age (years) | 26.68 ± 5.1 | 25.68 ± 5.3 | 26.60 ± 5.4 |
| Sex | |||
| Male | 8 (32%) | 10 (40%) | 9 (36%) |
| Female | 17 (68%) | 15 (60%) | 16 (64%) |
| Occupation | |||
| Working | 10 (40%) | 8 (32%) | 11 (44%) |
| Not working | 15 (60%) | 17 (68%) | 14 (56%) |
| Marital status | |||
| Single | 10 (40%) | 11 (44%) | 10 (40%) |
| Married | 13 (52%) | 13 (52%) | 13 (52%) |
| Divorced | 2 (8%) | 1 (4%) | 2 (8%) |
| Smoking | 4 (16%) | 5 (20%) | 4 (16%) |
| Previous treatment | |||
| Topical | 5 (20%) | 6 (24%) | 5 (20%) |
| Isotretinoin | 0 (0%) | 0 (0%) | 0 (0%) |
| Intervention | 6 (24%) | 4 (16%) | 6 (24%) |
| Duration of scar (years) | 4.72 ± 1.7 | 4.56 ± 1.9 | 4.76 ± 1.6 |
| P value** | P1 = 0.747 | P2 = 0.687 | P3 = 0.936 |
| Skin type | |||
| III | 8 (32%) | 7 (28%) | 9 (36%) |
| IV | 17 (68%) | 18 (72%) | 16 (64%) |
| Scar type | |||
| Boxcar | 9 (36%) | 10 (40%) | 10 (40%) |
| Icepick | 10 (40%) | 7 (28%) | 9 (36%) |
| Rolling | 6 (24%) | 8 (32%) | 6 (24%) |
** Non significant difference
Likewise, the difference between the three groups in pretreatment acne scar grade was not statistically significant (P = 0.831). On the other hand, the three treated groups showed significant improvement in acne scar grading with a significant decrease in the severity of acne scars. Comparing the groups, patients treated with both Er-YAG laser and PRP showed a significant improvement compared with those treated with Er-YAG laser or PRP alone (P = 0.007 and P < 0.001, respectively). Also, patients treated with Er-YAG laser showed more marked improvement than those treated with PRP (P < 0.001) (Table 2).
Table 2.
Acne scar grading according to Goodman and Baron
| PRP (n = 25) | Er-YAG laser (n = 25) | Both (n = 25) | P value | |
|---|---|---|---|---|
| Pretreatment | 0.831a | |||
| Macular | 0 (0%) | 0 (0%) | 0 (0%) | |
| Mild | 4 (16%) | 5 (20%) | 3 (12%) | |
| Moderate | 13 (52%) | 14 (56%) | 14 (56%) | |
| Severe | 8 (32%) | 6 (24%) | 8 (32%) | |
| Posttreatment | 0.004a* | |||
| Macular | 2 (8%) | 5 (20%) | 3 (12%) | |
| Mild | 7 (28%) | 11 (44%) | 17 (68%) | |
| Moderate | 11 (44%) | 7 (28%) | 5 (20%) | |
| Severe | 5 (20%) | 2 (8%) | 0 (0%) | |
| P valuea | P1 = 0.001 | P2 = 0.007 | P3 < 0.001 |
* Significant
aChi-square test was used to compare the proportion difference between groups
P1 = PRP versus laser, P2 = laser versus both, P3 = PRP versus both
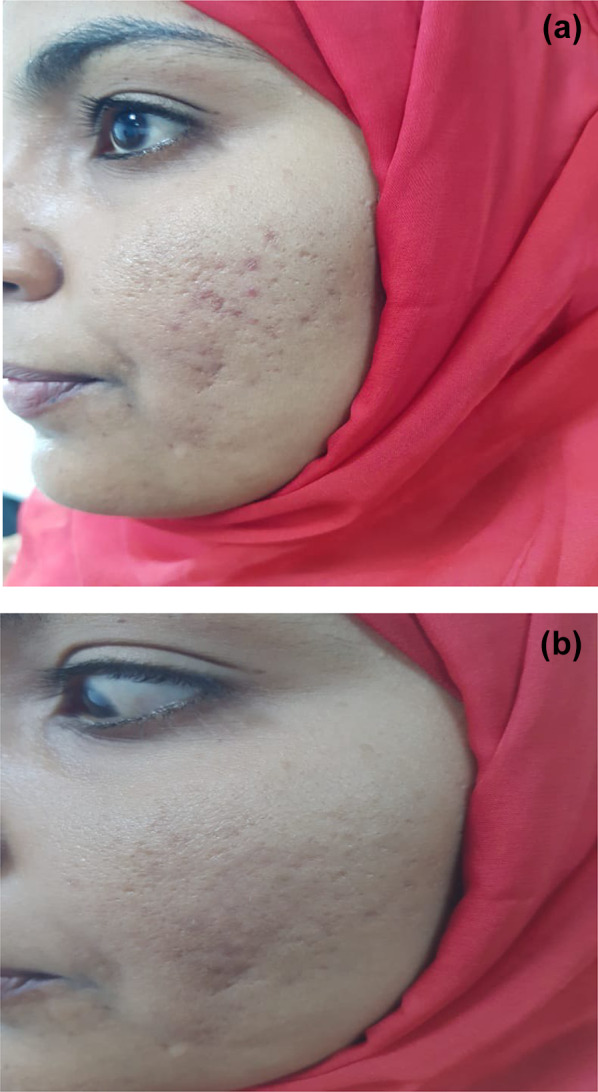
Regarding clinical improvement, in group A, the improvement was minimal in 12 patients (48%), moderate in 9 patients (36%), marked in 3 patients (12%), and excellent in 1 patient (4%). Likewise, in group B, it was excellent in 1 patient (4%), marked in 12 patients (48%), moderate in 9 patients (36%), and minimal in 3 patients (12%). In group C, the improvement was excellent in 8 patients (32%), marked in 11 patients (44%), moderate in 5 patients (20%), and minimal in 1 patient (4%) The overall improvement was significantly greater in group C compared with group A or group B (P < 0.001). Also, group B showed significantly greater clinical improvement than group A (P < 0.012) (Table 3) (Figs. 1, 2, 3).
Table 3.
Treatment efficacy among the studied cohort
| PRP (n = 25) | Er-YAG laser (n = 25) | Both (n = 25) | P value | |
|---|---|---|---|---|
| Clinical improvement | ||||
| Minimal | 12 (48%) | 3 (12%) | 1 (4%) | |
| Moderate | 9 (36%) | 9 (36%) | 5 (20%) | < 0.001a |
| Marked | 3 (12%) | 12 (48%) | 11 (44%) | |
| Excellent | 1 (4%) | 1 (4%) | 8 (32%) | |
| P valuea | P1 = 0.012 | P2 < 0.001 | P3 < 0.001 | |
| Patient satisfaction | ||||
| Dissatisfied | 9 (36%) | 3 (12%) | 2 (8%) | |
| Neutral | 9 (36%) | 7 (28%) | 5 (20%) | < 0.001a |
| Satisfied | 6 (24%) | 12 (48%) | 11 (44%) | |
| Highly satisfied | 1 (4%) | 3 (12%) | 7 (28%) | |
| P valuea | P1 = 0.009 | P2 = 0.005 | P3 < 0.001 | |
aChi-square test was used to compare the proportion difference between groups
P1 = PRP versus laser, P2 = laser versus both, P3 = PRP versus both. P < 0.05 is significant
Fig. 1.
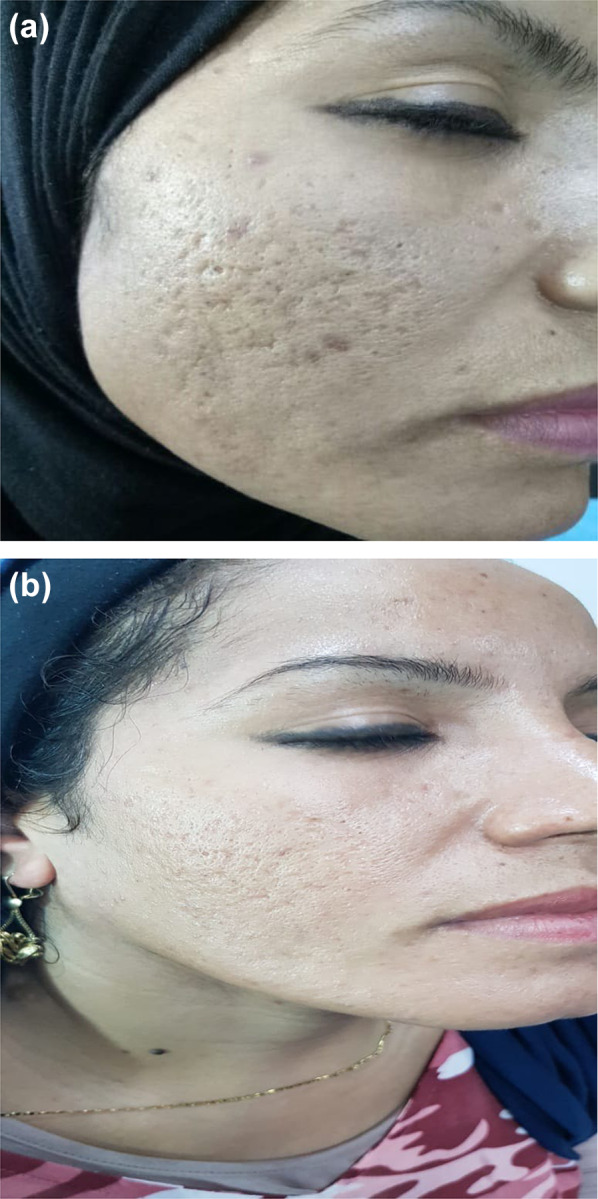
A 27-year-old female patient treated with combined Er-YAG 2940 nm laser and PRP sessions: a pretreatment, b posttreatment
Fig. 2.

A 25-year-old female patient treated with PRP sessions: a pretreatment, b posttreatment
Fig. 3.
A 24-year-old female patient treated with Er-YAG 2940 nm laser sessions only: a pretreatment, b posttreatment
Regarding patient satisfaction, in group A, about one-third of patients were either dissatisfied or neutral, a quarter of them were satisfied, while only one patient was highly satisfied. Meanwhile, in group B, 3 patients (12%) were highly satisfied, 12 (48%) were satisfied, 7 (28%) were neutral, and 3 (12%) were dissatisfied. Patients in group C were distributed as follows: 7 (28%) were highly satisfied, 11 (44%) were satisfied, 5 (20%) were neutral, and 2 (8%) were dissatisfied. In pairwise comparisons, patients in group C were more satisfied with their results than those in group A or B (P < 0.001 and P = 0.005, respectively). Likewise, patients treated with Er-YAG laser were markedly more satisfied than those treated with PRP (P = 0.009) (Table 3).
There were no statistically significant differences between the two study groups regarding any of the posttreatment complications (Table 4).
Table 4.
Complications of treatment modalities in studied groups
| PRP (n = 25) | Er-YAG laser (n = 25) | Both (n = 25) | P value | |
|---|---|---|---|---|
| Posttreatment facial erythema | 0.323* | |||
| Clear | 9 (36%) | 10 (40%) | 8 (32%) | |
| Almost clear | 13 (52%) | 15 (60%) | 15 (60%) | |
| Mild | 3 (12%) | 0 (0%) | 2 (8%) | |
| Posttreatment PIH | ||||
| 5 (20%) | 2 (8%) | 4 (16%) | 0.451* | |
| Posttreatment acne-form eruption | ||||
| 2 (12%) | 1 (4%) | 1 (4%) | 0.260* | |
* Non significant
Discussion
Although there is no standard protocol for treatment of acne scars, many therapeutic interventions have been used, with variable clinical success and complications, including dermabrasion, microdermabrasion, microneedling, PRP, and ablative and nonablative fractional lasers [14].
In the current work, the efficacy and safety of PRP, factional Er-YAG laser, and their combination for treatment of atrophic acne scars were compared. The results reveal marked efficacy of PRP in treating acne scars with an improvement in scar grade, clinical appearance, and patient satisfaction compared with their baseline measurements. These results coincide with previous studies that compared the efficacy of PRP, trichloroacetic acid, and microneedling for acne scars, which found significant efficacy of PRP with nonsignificant difference from the other lines [15–17]. In their work, Ibrahim et al. found that PRP was more effective than microneedling while combined treatment was more effective than either line alone [16]. This can be explained by the fact that platelets contain alpha-granules and secrete several growth factors, such as transforming growth factor-beta, platelet-derived growth factor, vascular endothelial growth factor, and others [17]. These growth factors and other proteins, such as adhesion molecules and chemokines, interact with the local environment to promote cell differentiation, proliferation, and regeneration and enhance proliferation of human adipose-derived stem cells, human-derived fibroblasts, and type 1 collagen [18].
Moreover, patients treated with fractional Er-YAG laser showed a significant improvement in their acne scar grade, clinical appearance, and satisfaction as compared with their baseline, and also their improvement was significantly better than those treated with PRP alone, indicating a higher efficacy of fractional Er-YAG laser than PRP. These findings could be due to the fact that fractional Er-YAG laser provides less ablation and coagulation depth than fractional CO2 laser, yielding comparable efficacy with lower downtime and less side effects [19]. Furthermore, the Er-YAG laser wavelength is 2940 nm, corresponding to the peak absorption coefficient of water, and is absorbed 12 times or more by cutaneous water-containing tissue than the 10,600 nm wavelength of the CO2 laser [20].
The efficacy and safety of fractional Er-YAG laser in treatment of atrophic acne scars were investigated by Kirmal et al., who found it to be a highly effective and safe treatment modality for atrophic acne scars [21]. In their pilot study, Firooz et al. reported that fractional Er-YAG laser was an effective and minimally invasive method for treatment of atrophic acne scars [22]. The effect of Er-YAG laser was found to be greater in early scars than in those with long duration [23]. It has been postulated that the coagulation mode of the fractional Er-YAG laser delivers energy more precisely without excessive thermal injury to adjacent tissue, which allows faster healing and an easy, effective, and safe method for acne scar treatment [24].
In the present trial, patients who were treated with combined PRP and fractional Er-YAG laser showed significant improvement in their acne scar grade, clinical evaluation, and satisfaction compared with their baseline, and also when compared with those treated with either modality alone.
Although many data have been published on combined treatments for acne scars, few works on this combination (PRP and fractional Er-YAG laser) have been published. In their study, Zhu et al. found that PRP combined with erbium fractional laser therapy was a safe and effective approach for treating acne scars, with less side effects [25]. The combination of PRP and fractional CO2 laser was found to be a more effective treatment modality for acne scars compared with PRP or CO2 laser alone [26]. These better results (improvement of acne scars and fewer side effects) can be attributed to the synergistic effect when using both modalities simultaneously. Indeed, PRP enhances proliferation of human adipose-derived stem cells, human-derived fibroblasts, and type 1 collagen, which accelerates healing of laser-induced lesions [25]. On the other hand, poor efficacy of fractional ablative laser in treating acne scars has been reported [27, 28].
Notwithstanding, no significant difference was detected between the groups regarding complications or side effects. These results are consistent with those of Gawdat et al., who did not report PIH after treatment with PRP, whereas it was reported in 13.3% of patients who received fractional CO2 laser alone; they concluded that the combination of topical PRP and fractional CO2 laser is an effective and safe modality for treatment of atrophic acne scars with shorter downtime than fractional CO2 laser alone and better tolerability than fractional CO2 laser combined with PRP [29]. This may be because the faster repair of the basement membrane might reduce pigmentary incontinence, resulting in less pigmentation after laser. Another explanation might be that TGF-b, which is released by PRP, is also known to decrease melanogenesis. We believe that this action gives the combined protocol an advantage.
Limitations
The main limitation of the present trial is the short follow-up period.
Conclusions
Both PRP and fractional Er-YAG laser were found to be effective and safe for treatment of acne scars, but their combination was found to be superior to either line of treatment alone, with better results and higher tolerability and patient satisfaction.
Acknowledgements
We acknowledge the medical staff of the dermatology, venerology and andrology department, South Valley University. It was not possible to complete this work without the help and approval of the assigned patients.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Moustafa A. El-Taieb, Hassan M. Ibrahim, Eisa M Hegazy, Ahmed K. Ibrahim, Aya M. Gamal and Essam A. Nada have nothing to disclose.
Compliance with Ethics Guidelines
Approval for this study was obtained from Institutional review board (IRB) of the Faculty of Medicine-South Valley University prior to study execution. The trial was registered on the clinical trial registration website (https://clinicaltrials.gov/ NCT03933033). The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. In addition, all participants were asked to sign a written consent form prior to participation. The informed consent was clear and indicated the purpose, process, benefits and risks of the study, also, their freedom to participate or withdraw at any time without any obligation. Furthermore, participants’ confidentiality and anonymity were assured by assigning each participant with a code number for the purpose of analysis only. The study was not based on any incentives or rewards for the participants.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.9061226.
References
- 1.Fife D. Practical evaluation and management of atrophic acne scars, tips for the general dermatologist. J Clin Aesthet Dermatol. 2011;4(8):50–57. [PMC free article] [PubMed] [Google Scholar]
- 2.El-Hamd MA, El Taieb MA, Ibrahim HM, Aly SS. Vitamin D levels in acne vulgaris patients treated with oral isotretinoin. J Cosmet Dermatol. 2018;18(1):1–5. doi: 10.1111/jocd.12503. [DOI] [PubMed] [Google Scholar]
- 3.Al Taweel A-AI, Al Refae A-AA-S, Hamed AM, Kamal AM. Comparative study of the efficacy of Platelet-rich plasma combined with carboxy therapy vs its use with fractional carbon dioxide laser in atrophic acne scars. J Cosmet Dermatol. 2018;18(1):150–155. doi: 10.1111/jocd.12561. [DOI] [PubMed] [Google Scholar]
- 4.Goodman GJ, Baron JA. Post acne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32(12):1458–1466. doi: 10.1111/j.1524-4725.2006.32354.x. [DOI] [PubMed] [Google Scholar]
- 5.Al-Saedy SJ, Al-Hilo MM, Al-Shami SH. Treatment of acne scars using fractional erbium:YAG laser. Am J Dermatol Venereol. 2014;3(2):43–49. [Google Scholar]
- 6.Omi T, Numano K. The role of the CO2 laser and fractional CO2 laser in dermatology. Laser Ther. 2014;23(1):49–60. doi: 10.5978/islsm.14-RE-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connolly D, Vu HL, Mariwalla K, Saedi N. Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10(9):12–23. [PMC free article] [PubMed] [Google Scholar]
- 8.Kumaran MS, Arshdeep A. Platelet-rich plasma in dermatology: boon or a bane? Indian J Dermatol Venereol Leprol. 2014;80(1):5–14. doi: 10.4103/0378-6323.125467. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed M, Ffrench-Constant C. Extracellular matrix regulation of stem cell behavior. Curr Stem Cell Rep. 2016;2(3):197–206. doi: 10.1007/s40778-016-0056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang BK, Lee JH, Shin MK, Kim NI. Infraorbital rejuvenation using PRP (platelet-rich plasma): a prospective, randomized, split-face trial. J Am Acad Dermatol. 2013;68:24. [Google Scholar]
- 11.El Taieb MA, Ibrahim H, Nada EA, Seif Al-Din M. Platelets rich plasma versus minoxidil 5% in treatment of alopecia areata: a trichoscopic evaluation. Dermatol Ther. 2017;30(1):1–6. doi: 10.1111/dth.12437. [DOI] [PubMed] [Google Scholar]
- 12.Abdel-Aal AM, Ibrahim IM, Sami NA, Abdel Kareem IM. Evaluation of autologous platelet-rich plasma plus ablative carbon dioxide fractional laser in the treatment of acne scars. J Cosmet Laser Ther. 2018;20(2):106–113. doi: 10.1080/14764172.2017.1368667. [DOI] [PubMed] [Google Scholar]
- 13.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 14.Thiboutot DM, Abanmi A, Araviiskaia E, Barona Cabal MI, Bettoli V. Practical management of acne for clinicians: an international consensus from the global alliance to improve outcomes in acne. J Am Acad Dermatol. 2018;2(1):1–23. doi: 10.1016/j.jaad.2017.09.078. [DOI] [PubMed] [Google Scholar]
- 15.Nofal E, Helmy A, Nofal A, Alakad R, Nasr M. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg. 2014;40:864–873. doi: 10.1111/dsu.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim ZA, El-Ashmawy AA, Shora OA. Therapeutic effect of microneedling and autologous platelet-rich plasma in the treatment of atrophic scars: a randomized study. J Cosmet Dermatol. 2017;16:388–399. doi: 10.1111/jocd.12356. [DOI] [PubMed] [Google Scholar]
- 17.Sanchez-Gonzalez DJ, Mendez-Bolaina E, Trejo-Bahena NI. Platelet-rich plasma peptides: key for regeneration. Int J Pept. 2012;2012:532519. doi: 10.1155/2012/532519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wrotniak M, Bielecki T, Gazdzik TS. Current opinion about using the platelet-rich gel in orthopaedics and trauma surgery. Ortop Traumatol Rehabil. 2007;9:227–238. [PubMed] [Google Scholar]
- 19.Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63:274–283. doi: 10.1016/j.jaad.2009.08.051. [DOI] [PubMed] [Google Scholar]
- 20.Tanzi EL, Alster TS. Single-pass carbon dioxide versus multiple pass Er:YAG laser skin resurfacing: a comparison of postoperative wound healing and side-effect rates. Dermatol Surg. 2003;29:80–84. doi: 10.1046/j.1524-4725.2003.29012.x. [DOI] [PubMed] [Google Scholar]
- 21.Nirmal B, Pai SB, Sripathi H, Rao R, Prabhu S, Kudur MH, Nayak SU. Efficacy and safety of erbium-doped yttrium aluminium garnet fractional resurfacing laser for treatment of facial acne scars. Indian J Dermatol Venereol Leprol. 2013;79:193–198. doi: 10.4103/0378-6323.107635. [DOI] [PubMed] [Google Scholar]
- 22.Firooz A, Rajabi-Estarabadi A, Nassiri-Kashani MH. Treatment of atrophic facial acne scars with fractional Er:YAG laser in skin phototype III-IV: a pilot study. J Cosmet Laser Ther. 2016;18(4):204–207. doi: 10.3109/14764172.2016.1157354. [DOI] [PubMed] [Google Scholar]
- 23.Kim SG, Kim EY, Kim YJ, Lee SI. The efficacy and safety of ablative fractional resurfacing using a 2,940-nm Er:YAG laser for traumatic scars in the early post traumatic period. Arch Plast Surg. 2012;39:232–237. doi: 10.5999/aps.2012.39.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu S, Hsiao WC, Chen MC, Huang YL, Chang SL, Shih PY, Gold MH. Ablative fractional erbium-doped yttrium aluminum garnet laser with coagulation mode for the treatment of atrophic acne scars in Asian skin. Dermatol Surg. 2011;37:939–944. doi: 10.1111/j.1524-4725.2011.02009.x. [DOI] [PubMed] [Google Scholar]
- 25.Zhu JT, Xuan M, Zhang YN. The efficacy of autologous platelet-rich plasma combined with erbium fractional laser therapy for facial acne scars or acne. Mol Med Rep. 2013;8:233–237. doi: 10.3892/mmr.2013.1455. [DOI] [PubMed] [Google Scholar]
- 26.Faghihi G, Keyvan S, Asilian A, Nouraei S, Behfar S, Nilforoushzadeh MA. Efficacy of autologous platelet-rich plasma combined with fractional ablative carbon dioxide resurfacing laser in treatment of facial atrophic acne scars: a split-face randomized clinical trial. Indian J Dermatol Venereol Leprol. 2016;82:162–168. doi: 10.4103/0378-6323.174378. [DOI] [PubMed] [Google Scholar]
- 27.Hwang YJ, Lee YN, Lee YW, Choe YB, Ahn KJ. Treatment of acne scars and wrinkles in asian patients using carbon-dioxide fractional laser resurfacing: its effects on skin biophysical profiles. Ann Dermatol. 2013;25(4):445–453. doi: 10.5021/ad.2013.25.4.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan HH, Manstein D, Yu C, Shek S, Kono T, Wei WI. The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2010;39:381–385. doi: 10.1002/lsm.20512. [DOI] [PubMed] [Google Scholar]
- 29.Gawdat HI, Hegazy RA, Fawzy MM, Fathy M. Autologous platelet rich plasma: topical versus intradermal after fractional ablative carbon dioxide laser treatment of atrophic acne scars. Dermatol Surg. 2014;40(2):152–161. doi: 10.1111/dsu.12392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.


