Abstract
Viperin is an IFN-stimulated gene (ISG)-encoded protein that was identified in human primary macrophages treated with IFN-γ and in human primary fibroblasts infected with cytomegalovirus (CMV). This protein plays multiple roles in various cell types. It inhibits viral replication, mediates signaling pathways, and regulates cellular metabolism. Recent studies have shown that viperin inhibits IFN expression in macrophages, while it enhances TLR7 and TLR9-mediated IFN production in plasmacytoid dendritic cells, suggesting that viperin can play different roles in activation of the same pathway in different cell types. Viperin also controls induction of ISGs in macrophages. However, the effect of viperin on induction of ISGs in cell types other than macrophages is unknown. Here, we show that viperin differentially induces ISGs in 2 distinct cell types, macrophages and fibroblasts isolated from wild type and viperin knockout mice. Unlike in bone marrow-derived macrophages (BMDMs), viperin downregulates the expression levels of ISGs such as bone marrow stromal cell antigen-2, Isg15, Isg54, myxovirus resistance dynamin like GTPase 2, and guanylate binding protein 2 in murine embryonic fibroblasts (MEFs) treated with type I or II IFN. However, viperin upregulates expression of these ISGs in both BMDMs and MEFs stimulated with polyinosinic-polycytidylic acid or CpG DNA and infected with murine CMV. The efficiency of viral entry is inversely proportional to the expression levels of ISGs in both cell types. The data indicate that viperin differentially regulates induction of ISGs in a cell type-dependent manner, which might provide different innate immune responses in distinct cell types against infections.
Keywords: Viperin, Interferons, ISG, Macrophages, Fibroblasts, Cytomegalovirus
INTRODUCTION
The IFN response is the first line of host defense against diverse pathogens. Pattern-recognition receptors such as TLRs and RIG-I-like receptors recognize infectious agents and activate transcription factors, IFN-regulatory factors (IRFs) and NF-κB (1). The transcription factors subsequently mediate production of IFNs and pro-inflammatory cytokines. The secreted IFNs trigger induction of a large number of IFN-stimulated genes (ISGs) including 2′5′-oligoadenylate synthetase (Oas), ribonuclease L, IFN-inducible dsRNA-dependent protein kinase (Pkr), myxovirus resistance dynamin like GTPase (Mx), and interferon-stimulated gene 15 (Isg15) through the JAK- STAT signaling pathway (1,2). The protein products of these ISGs play important roles as antipathogenic effector molecules in innate immunity (1,3).
Macrophages are innate immune cells that have functions in phagocytosis, antigen presentation, and immunomodulation (4). They can be polarized into 2 different subsets, classically activated macrophages (M1) and alternatively activated macrophages (M2) (5). M1 macrophages produce pro-inflammatory cytokines and provide a host defense against pathogens (6,7). M2 macrophages secrete anti-inflammatory cytokines and have repairing function (6,7). It has been reported that IFN responses affect the inflammatory functions of macrophages (8,9). Some ISG products expressed in macrophages promote inflammation and others inhibit (10,11,12,13,14).
Fibroblasts are ubiquitous mesenchymal cells that play roles in wound healing, antigen presentation, and maintenance of homeostasis (15,16,17). They are also important for immune responses. Fibroblasts can initiate inflammation in the presence of invading pathogens. They produce many different cytokines including IFNs and modulate extracellular matrix components against infectious pathogens (15,16,17). The ISG products expressed in fibroblasts exert their diverse antipathogenic properties (18,19,20).
Viperin (virus inhibitory protein, endoplasmic reticulum-associated, interferon-inducible) was first identified in human primary macrophages stimulated with IFN-γ and in human fibroblasts infected with human cytomegalovirus (CMV) (21,22). It is also induced in a variety of cells by treatment of type I, II, and III IFNs, ds B-form DNA, the dsRNA analog polyinosinic-polycytidylic acid (poly[I:C]), or LPS and infection of a wide range of viruses (23). Viperin protein has multiple functions in various cell types including macrophages, fibroblasts, dendritic cells, adipocytes, and astrocytes (24,25,26,27,28,29,30). This protein exhibits antiviral activity against many viruses (25,26,27,28), mediates signaling pathways or T cell development (29,31), and modulates cellular metabolism (24,30,32). It also plays a pivotal role in activation of macrophages, dendritic cells, and T cells (31,33,34,35). Recent studies have shown that viperin is a positive regulator of TLR7- and TLR9-mediated production of type I IFNs in plasmacytoid dendritic cells (pDCs) (29), while this protein is a negative regulator of mitochondrial antiviral signaling protein (MAVS)-linked IFN-β induction in macrophages (36). It suggests that viperin differentially regulates IFN induction in different cell types. Viperin also upregulates expression of most ISGs in macrophages in the absence or presence of type I IFN (36). Despite the importance of ISG products in innate immunity, the effect of viperin on induction of ISGs in cell types other than macrophages has not been examined.
In this study, we show that viperin differentially regulates ISG induction in two distinct cell types, macrophages and fibroblasts treated with type I or II IFNs. Viperin upregulates ISG expression in bone marrow-derived macrophages (BMDMs) treated with IFNs, while it downregulates ISG expression in murine embryonic fibroblasts (MEFs). Interestingly, viperin upregulates ISG expression in both BMDMs and MEFs stimulated with poly(I:C), CpG DNA, or CMV other than IFNs. The efficiency of viral entry depends on the levels of ISG expression in both cell types treated with CMV in the absence or presence of IFNs. Our data indicate that viperin differentially regulates ISG induction in a cell type-dependent manner under IFNs treatments, and in a stimulus-dependent manner through an IFN signaling pathway. It suggests that viperin-mediated differential expression of ISGs might provide different innate immune responses in distinct cell types against diverse pathogens.
MATERIALS AND METHODS
Cells, viruses, antibodies, and reagents
Murine bone marrow cells and MEFs used in the study were isolated from wild type (WT) or viperin (Rsad2) knockout (KO) C57BL/6 mice (24,34). MEFs were immortalized by serial passages as described previously (24).
The Smith strain of murine cytomegalovirus (MCMV) and monoclonal antibody Croma 101 (anti-immediate early 1 [IE1]) were kindly provided by Dr. W.J. Britt (University of Alabama at Birmingham). Viperin was detected with the monoclonal mouse antibody to viperin (MaP.VIP) described previously (21,27). The monoclonal mouse anti-ISG15 antibody (Santa Cruz Biotechnology, Inc., Dallas, TX, USA), monoclonal rat anti-GRP94 antibody (Enzo Life Sciences, Inc., Farmingdale, NY, USA), and horseradish peroxidase-conjugated goat anti-mouse or anti-rat IgG antibody (Jackson ImmunoResearch Laboratories, West Grove, PA, USA) were used. Universal type I IFN (PBL Assay Science, Piscataway, NJ, USA), recombinant mouse IFN-γ (R&D systems, Minneapolis, MN, USA), poly(I:C) (InvivoGen, San Diego, CA, USA), CpG DNA (Enzo Life Sciences, Inc.), and Lipofectamine 2000 (Thermo Fisher Scientific, Waltham, MA, USA) were also used.
Mouse M-CSF was stably expressed in CHO cells and the culture supernatants containing the secreted M-CSF were used for generation of BMDMs as described previously (37).
Generation of BMDMs
To generate BMDMs, the bone marrow cells from femurs and tibias of mice were harvested and plated in culture medium (RPMI [Hyclone Laboratories Inc., South Logan, UT, USA], 10% FBS [Hyclone Laboratories Inc.], 1% penicillin/streptomycin [Sigma-Aldrich, St. Louis, MO, USA]) containing 10% M-CSF supernatants for 7 days. BMDMs cultured in M-CSF conditioned media were washed and re-plated in cell culture dishes (SPL Life Sciences, Pocheon, Korea) containing culture medium without M-CSF for 24 h.
Stimulation of BMDMs and MEFs
BMDMs and MEFs were treated with 1000 U/ml IFN-I (PBL Assay Science) or 100 ng/ml IFN-γ (R&D systems) for 24 h. The cells were transfected with 1 μg/ml poly(I:C) (InvivoGen) or 1 μg/ml CpG DNA (Enzo Life Sciences, Inc.) using Lipofectamine 2000 (Thermo Fisher Scientific). The cells were infected with MCMV at the initial multiplicity of infection (MOI) of 0.2 or 2 in the absence or presence of IFNs, and incubated for 24 h.
Immunoblot analysis
Cells were harvested and lysed in lysis buffer (1% Triton X-100 in TRIS-buffered saline) containing proteinase inhibitors. Supernatants of lysates were collected, and the concentration of proteins was measured by bicinchoninic acid (BCA) assay (Thermo Fisher Scientific). The proteins were separated on 15% SDS-PAGE gels and transferred to polyvinylidene fluoride membranes (Millipore, Burlington, MA, USA). The blots were blocked with 5% skim milk and 0.05% Tween in PBS for 1 h, incubated with primary antibodies for 1 day, probed with horseradish peroxidase-conjugated secondary antibodies for 1 h, followed by incubation with enhanced chemiluminescence reagents (Thermo Fisher Scientific). The intensity of bands was analyzed using ImageJ software.
Immunofluorescence
Cells were grown in 24-well cell culture plates containing a 13-mm-diameter coverslip. The coverslips were harvested by washing cells with PBS and then fixing cells with 3% paraformaldehyde in PBS for 45 min at room temperature. The coverslips were washed with PBS and permeabilized with 0.1% Triton X-100 and 0.01% SDS in PBS for 7 min. The coverslips were then blocked with 0.2% Tween in PBS containing 10% normal goat serum (Thermo Fisher Scientific) for 20 min at room temperature, followed by the addition of the monoclonal mouse antibody Croma 101 (anti-IE1), and incubated for 1 h at room temperature. The coverslips were washed with 0.2% Tween in PBS and incubated with anti-mouse Ig secondary antibody conjugated to dye (Thermo Fisher Scientific) for 45 min at room temperature. The coverslips were washed with 0.2% Tween in PBS, rinsed once in PBS, and mounted with ProLong Gold Antifade reagent (Molecular Probes, Eugene, OR, USA). The images were acquired with a Zeiss LSM700 scanning laser confocal microscope (Carl Zeiss AG, Oberkochen, Germany) and analyzed using Zeiss ZEN 2012 software and ImageJ software.
RNA extraction, cDNA preparation, and quantitative real-time PCR
Cells were collected and total RNA were extracted using RNeasy Mini kit (Qiagen, Hilden, Germany). The cDNA was synthesized with 1 μg RNA using Prime script RT reagent kit according to the manufacturer's instructions (Takara Bio, Kusatsu, Japan). The cDNA obtained from cells was quantified by quantitative real-time PCR (qRT-PCR) using TB Green Fast qPCR reagent kit (Takara Bio). The sequences of primers for the PCR are listed in Supplementary Table 1. The reaction included 95°C for 5 min, which was followed by a 3-step PCR program of 95°C for 30 s, 60°C for 5 s, and 72°C for 15 s repeated for 40 cycles. The PCR was performed in triplicate for each sample. The quantitation of the results was performed by the comparative Ct (2−ΔΔCt) method. The Ct value for each sample was normalized by the value for β-actin gene. Three independent experiments were analyzed statistically for differences in the mean values, and p values are indicated in the figures.
Statistical analysis
The data are presented as mean±SEM. Statistical significance was determined with unpaired 2-tailed Student's t-test using GraphPad Prism 5 software. The p values less than 0.05 were considered significant.
RESULTS
Viperin differentially regulates expression of ISGs in 2 different cell types treated with IFNs
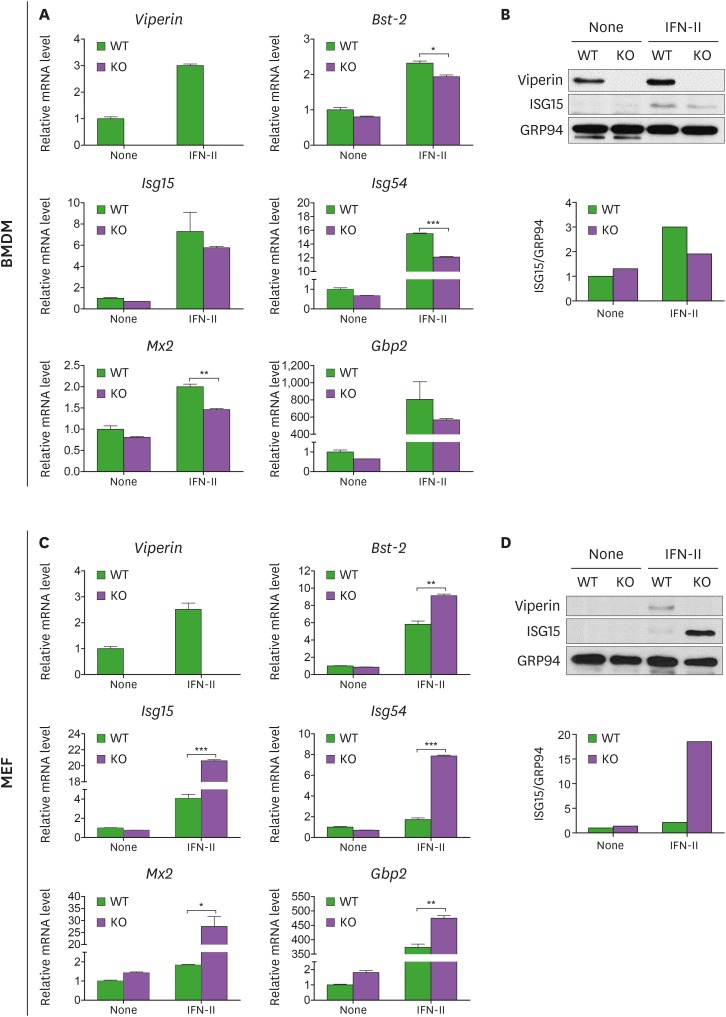
Viperin enhances ISG expression in macrophages in the absence or presence of type I IFN (36), but its effect on cell types other than macrophages has not been examined. We therefore investigated the role of viperin in ISG induction in 2 distinct cell types, macrophages and fibroblasts. Bone marrow cells were isolated from WT and viperin KO mice and differentiated into BMDMs in M-CSF conditioned media. MEFs were also isolated from these mice and immortalized as described previously (24). The expression levels of ISGs, Viperin, bone marrow stromal cell antigen-2 (Bst-2), Isg15, Isg54, myxovirus resistance dynamin like GTPase 2 (Mx2), guanylate binding protein 2 (Gbp2), and Isg56 that are known to be highly increased in cells upon IFN stimulation (36,38,39,40,41), were measured in WT and viperin KO BMDMs or MEFs (Fig. 1). Consistent with previous studies (36), the increases in expression levels of these ISGs were greater in WT BMDMs compared with viperin KO BMDMs treated with type I IFN (Fig. 1A and Supplementary Fig. 1). The expression level of ISG15 protein in WT BMDMs was also higher than that of ISG15 in viperin KO BMDMs treated with type I IFN (Fig. 1B). Viperin was basally expressed in WT BMDMs and highly increased upon type I IFN stimulation (Fig. 1B) (34). In contrast, the increases in expression levels of these ISGs, except for Isg56, were less in WT MEFs compared with viperin KO MEFs treated with type I IFN (Fig. 1C and Supplementary Fig. 1). The expression level of ISG15 in WT MEFs was also lower than that of ISG15 in viperin KO MEFs treated with type I IFN (Fig. 1D). Viperin was not basally expressed in MEFs, but it was highly induced in WT MEFs treated with type I IFN (Fig. 1D). The results indicated that viperin affects the expression of ISGs in type I IFN-mediated signaling pathway and its effects are dependent on cell type.
Figure 1. Viperin differentially regulates ISG expression in BMDMs and MEFs treated with type I IFN. (A-D) The effect of viperin on expression of ISGs in BMDMs and MEFs upon type I IFN treatment. The bone marrow cells isolated from WT and viperin KO C57BL/6 mice were differentiated into BMDMs in M-CSF conditioned media for 7 days. The BMDMs were washed and plated in media without M-CSF for 24 h (A, B). MEFs were isolated from these mice and immortalized (C, D). The cells were treated with or without type I IFN (1,000 U/ml) for 24 h. The mRNA expression levels of ISGs in the cells were measured by qRT-PCR and normalized to β-actin mRNA (A, C). Data are presented as mean ± SEM of triplicate samples and are representative of three individual experiments. Expression of viperin and ISG15 proteins in the cells was detected by immunoblot using anti-viperin (MaP.VIP) or anti-ISG15 antibody (B, D). GRP94 served as a protein-loading control. Quantitation of ISG15 protein level was normalized to GRP94.
*p<0.05; **p<0.01; ***p<0.001.
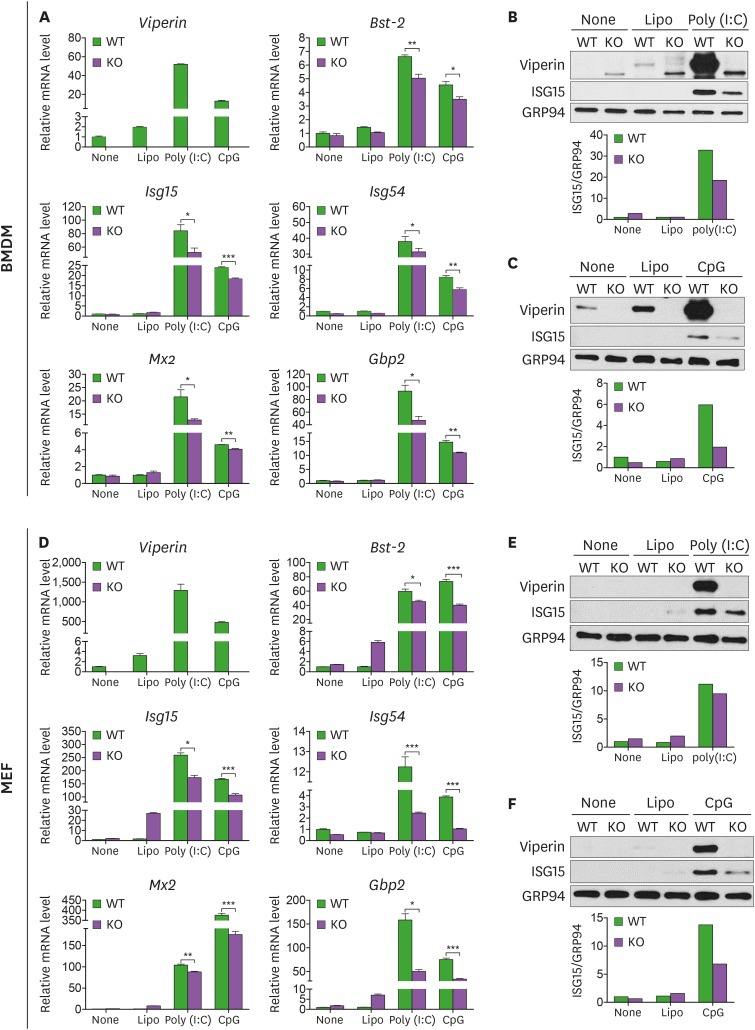
Both type I and type II IFNs are cytokines that have potent antiviral inhibitory effects on innate immune response. Although they bind to different receptors, the type I IFN receptor (IFNAR1-IFNAR2 subunits) and the type II IFN receptor (IFNGR1-IFNGR2 subunits), they commonly activate the JAK/STAT pathway and induce expression of ISGs (42). To examine whether viperin affects type II IFN-mediated signaling pathway, the expression levels of ISGs were measured in WT and viperin KO BMDMs or MEFs upon IFN-γ stimulation (Fig. 2). Similar to the results from type I IFN treatment, viperin differently affects ISG expression in BMDMs and MEFs treated with IFN-γ (Fig. 2). The results suggested that viperin is a cell type-specific regulator of ISG expression in type I or II IFN-mediated signaling pathway.
Figure 2. Viperin differently induces ISG expression in BMDMs and MEFs treated with type II IFN. (A-D) The effect of viperin on expression of ISGs in BMDMs and MEFs upon type II IFN treatment. WT and viperin KO BMDMs (A, B) or MEFs (C, D) were treated with or without IFN-γ (100 ng/ml) for 24 h. The mRNA expression levels of ISGs in the cells were measured by qRT-PCR and normalized to β-actin mRNA (A, C). Data are presented as mean±SEM of triplicate samples and are representative of three individual experiments. Expression of viperin and ISG15 proteins in the cells was detected by immunoblot using anti-viperin (MaP.VIP) or anti-ISG15 antibody (B, D). GRP94 served as a protein-loading control. Quantitation of ISG15 protein level was normalized to GRP94.
*p<0.05; **p<0.01; ***p<0.001.
Viperin enhances expression of ISGs in cells treated with poly(I:C) or CpG DNA.
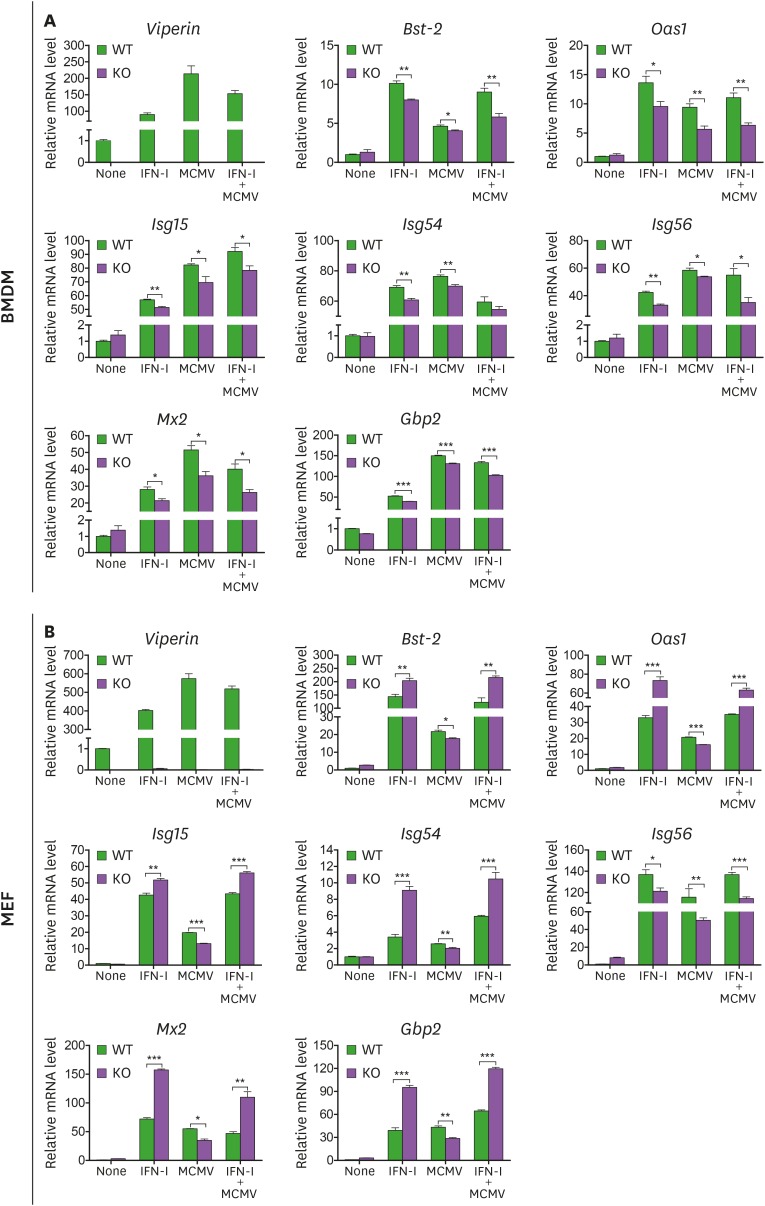
Viperin can modulate production of IFN in various cells such as pDCs, T cells, and BMDMs (29,31,36). To investigate whether viperin regulates ISG expression in cells treated with certain stimuli which induce IFN production, the expression levels of ISGs, Viperin, Bst-2, Isg15, Isg54, Mx2, and Gbp2 were measured in WT and viperin KO BMDMs or MEFs transfected with poly(I:C) or CpG DNA (Fig. 3). The increases in expression levels of these ISGs were significantly greater in WT BMDMs compared with viperin KO BMDMs treated with poly(I:C) or CpG DNA (Fig. 3A). The expression level of ISG15 in WT BMDMs was also higher than that of ISG15 in viperin KO BMDMs treated with poly(I:C) or CpG DNA (Fig. 3B and C). Like in BMDMs, viperin enhances ISG expression in MEFs treated with poly(I:C) or CpG DNA (Fig. 3D-F). The results suggested that viperin plays a role as a positive regulator on expression of ISGs in response to certain stimuli which mediate IFN production.
Figure 3. Viperin enhances ISG expression in both BMDMs and MEFs transfected with poly(I:C) or CpG DNA. (A-F) The effect of viperin on expression of ISGs in BMDMs and MEFs upon poly(I:C) or CpG DNA treatment. WT and viperin KO BMDMs (A-C) or MEFs (D-F) were treated with lipofectamine 2000 (Lipo), or transfected with poly(I:C) (1 μg/ml) or CpG DNA (1 μg/ml) for 24 h. The mRNA expression levels of ISGs in the cells were measured by qRT-PCR and normalized to β-actin mRNA (A, D). Data are presented as mean±SEM of triplicate samples and are representative of three individual experiments. Expression of viperin and ISG15 proteins in the cells was detected by immunoblot using anti-viperin (MaP.VIP) or anti-ISG15 antibody (B, C, E, F). GRP94 served as a protein-loading control. Quantitation of ISG15 protein level was normalized to GRP94.
*p<0.05; **p<0.01; ***p<0.001.
Viperin differentially regulates expression of ISGs in different cell types upon viral infection and/or IFN treatment
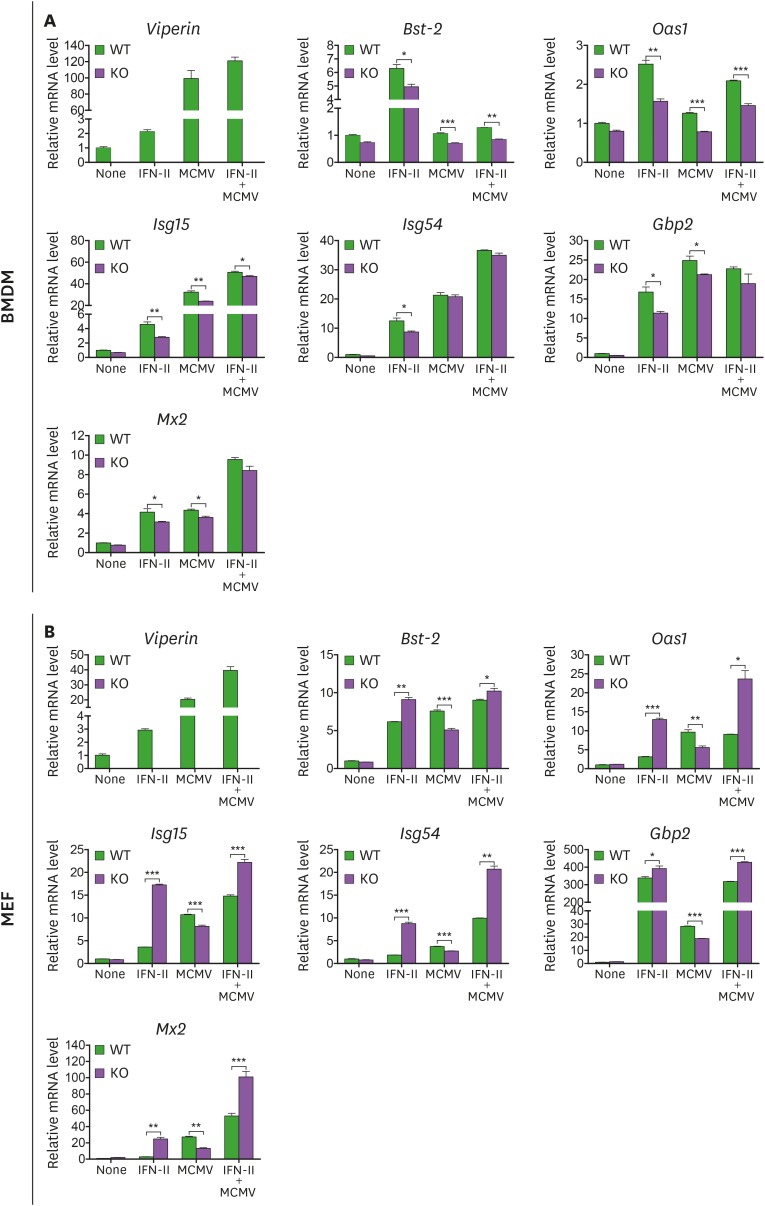
To examine the effects of viperin on ISG expression in cells infected with virus, the expression levels of ISGs, Viperin, Bst-2, Oas1, Isg15, Isg54, Isg56, Mx2, and Gbp2 were measured in WT and viperin KO BMDMs or MEFs infected with MCMV in the absence or presence of type I IFN (Fig. 4). The increases in expression levels of these ISGs were greater in WT BMDMs compared with viperin KO BMDMs infected with MCMV both in the absence and presence of type I IFN (Fig. 4A). While the increases in expression levels of these ISGs were greater in WT MEFs compared with viperin KO MEFs infected with MCMV in the absence of type I IFN, those of these ISGs except for Isg56 were less in WT MEFs compared with viperin KO MEFs infected with MCMV in the presence of type I IFN (Fig. 4B). Similar results were obtained from BMDMs and MEFs infected with MCMV in the absence or presence of IFN-γ (Fig. 5A and B). The data indicated that like in CpG DNA treatment, viperin enhances ISG expression of both BMDMs and MEFs after DNA virus infection. However, the effects of viperin on ISG expression by viral infection in MEFs were overwhelmed by IFN treatment, resulting in that viperin differentially regulates ISG expression in these 2 cell types.
Figure 4. Viperin differentially regulates ISG expression in BMDMs and MEFs treated with MCMV and/or type I IFN. (A, B) The effect of viperin on expression of ISGs in BMDMs and MEFs infected with MCMV in the absence or presence of type I IFN. WT and viperin KO BMDMs (A) or MEFs (B) were treated with or without type I IFN (1,000 U/ml) for 8 h and then infected with MCMV at an MOI of 0.2 for 24 h. The mRNA expression levels of ISGs in the cells were measured by qRT-PCR and normalized to β-actin mRNA. Data are presented as mean ± SEM of triplicate samples and are representative of three individual experiments.
*p<0.05; **p<0.01; ***p<0.001.
Figure 5. Viperin differently induces ISG expression in BMDMs and MEFs treated with MCMV and/or type II IFN. (A, B) The effect of viperin on expression of ISGs in BMDMs and MEFs infected with MCMV in the absence or presence of type II IFN. WT and viperin KO BMDMs (A) or MEFs (B) were treated with or without IFN-γ (100 ng/ml) for 8 h and then infected with MCMV at an MOI of 0.2 for 24 h. The mRNA expression levels of ISGs in the cells were measured by qRT-PCR and normalized to β-actin mRNA. Data are presented as mean±SEM of triplicate samples and are representative of three individual experiments.
*p<0.05; **p<0.01; ***p<0.001.
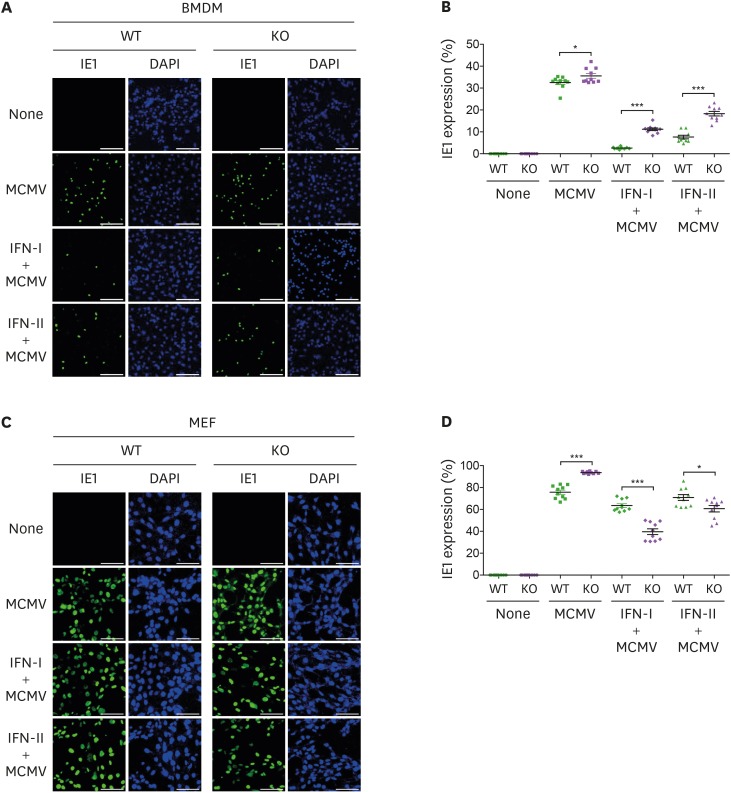
MCMV entry depends on viperin-mediated ISG expression
To determine whether viperin-mediated ISG expression affects viral infection, the efficiency of MCMV entry into WT and viperin KO BMDMs or MEFs were measured (Fig. 6). WT and viperin KO BMDMs were infected with MCMV for 24 h in the absence or presence of type I or II IFN (Fig. 6A and B). Cells expressing an MCMV protein, IE1 protein, were monitored (Fig. 6A). The efficiency of viral entry was quantitated by the percentage of cells expressing IE1 protein (Fig. 6B). The number of IE1-positive cells was less in WT BMDMs compared with viperin KO BMDMs infected with MCMV in the absence or presence of IFNs. Similar patterns of viral entry were also obtained from BMDMs infected with MCMV at low multiplicity of infection (Supplementary Fig. 2). While the number of IE1-positive cells was less in WT MEFs compared with viperin KO MEFs infected with MCMV in the absence of IFNs, that was greater in WT MEFs compared with viperin KO MEFs infected with MCMV in the presence of IFNs (Fig. 6C and D). The results indicated that the efficiency of viral entry is inversely proportional to the expression levels of ISGs mediated by viperin in both cell types.
Figure 6. MCMV entry is inversely proportional to viperin-mediated ISG expression. (A-D) The efficiency of MCMV entry into BMDMs and MEFs infected with MCMV in the absence or presence of IFNs. WT and viperin KO BMDMs (A, B) or MEFs (C, D) were treated with or without type I IFN (1,000 U/ml) or IFN-γ (100 ng/ml) for 8 h and then infected with MCMV at an MOI of 2 for 24 h. The cells were stained with antibody specific to the MCMV protein IE1 (green) to identify infected cells. Nuclei were stained with DAPI (blue). A representative image from two individual experiments was shown (scale bar=100 μm) (A, C). The efficiency of MCMV entry into the cells was quantitated (B, D). The infected cells were counted in each image (n=10). The percentage of MCMV positive cells per total cells in each image was calculated. Data are presented as mean±SEM.
*p<0.05; ***p<0.001.
DISCUSSION
ISG products play critical roles in innate immunity against infectious pathogens (1,3). ISGs are induced by various stimuli including pathogens and IFNs. It suggested that ISG expression can be regulated by two distinct signaling pathways, the signaling pathways to induce IFN production and the JAK/STAT pathway to induce IFN-mediated ISG expression (1,3). Viperin is a highly induced ISG protein in many cell types including macrophages and fibroblasts (23). Our study showed that viperin differentially regulates ISG expression in BMDMs and MEFs in responses to IFNs. Viperin promoted the increases in ISG expression of BMDMs, while it diminished the increases in ISG expression of MEFs treated with IFNs. Some ISGs including viperin have cell type-specific property (11,43). Therefore, our data indicated that viperin modulates ISG expression in a cell type-dependent manner in response to excessive IFN treatment. Previous studies have shown that viperin interacts with IL-1 receptor associated kinase 1 (IRAK1) and TNF receptor associated factor 6 (TRAF6) at lipid droplet in pDCs, and MAVS at mitochondria in BMDMs to regulate the signaling pathway for IFN production (29,36). However, viperin interactions to modulate the JAK/STAT pathway for ISG induction under IFN treatment are unknown. The possible interactions between viperin and the signaling pathway components such as JAK protein kinases, STAT proteins, and STAT-IRF complexes may affect viperin-mediated and cell type-dependent ISG expression. Recently, it has been reported that both type I IFN and IFN-γ cause promoter binding of STAT1-STAT2-IRF9 complexes, a complete IFN-stimulated gene factor 3 (ISGF3) complex of the JAK-STAT pathway and highly induce expression of ISGs, while STAT2-IRF9 complexes control basal expression of ISGs in the steady state (44). It suggested that viperin may interact with the ISGF3 complex at different efficiency in BMDMs and MEFs treated with IFNs, resulting in different phenotypes of innate immune responses in these cell types. STAT proteins regulate the interplay between transcriptional activators, such as Src homology 2 domain and p300/CBP and the transcriptional activators contribute to selective expression of ISGs (45). It suggested that possible interactions of viperin and STAT proteins may determine expression of a set of ISGs in different cell types. The mechanism of viperin-mediated and cell type-dependent ISG expression needs to be further elucidated.
Our study also showed that viperin augments the increases in ISG expression of both BMDMs and MEFs treated with poly(I:C) or CpG DNA and infected with MCMV. However, viperin differently regulates production of type I IFN in different cell types (29,36). Upon TLR7- and TLR9 stimulation, viperin enhances K63-linked ubiquitination of IRAK1 by TRAF6, activates IRF7, and leads to production of type I IFN in pDCs (29). Upon poly(I:C) stimulation, viperin interacts with MAVS and restricts IRF3-dependent production of IFN-β in BMDMs (36). Therefore, our data indicated that viperin differentially regulates two distinct signaling pathways for IFN production and IFN-mediated ISG expression.
In addition, we have previously shown that viperin decreases expression of M1 macrophage cytokines including Tnf-a, Il-1b, and Il-6 in BMDMs treated with IFN-γ and LPS (34), while it increases expression of ISGs in BMDMs treated with IFN-γ. IL-1β limits production of type I IFN through direct transcriptional downregulation and prostaglandin-endoperoxide synthase 2-dependent prostaglandin E2 production. Inversely, type I IFN modulates the inflammatory microenvironment and suppresses production of cytokines (8,9,46). The balance of immune responses is important to prevent tissue damage and autoimmunity (9,46). Therefore, our data suggested that viperin may be involved in maintenance of a balance between ISGs and cytokines in inflammatory responses of macrophages.
The efficiency of MCMV entry was dependent on viperin-mediated ISG expression levels in cells infected with MCMV in the absence or presence of IFNs. The viral entry was less in both WT BMDMs and MEFs compared with viperin KO cells after MCMV infection. However, in the presence of IFNs, unlike in BMDMs, the viral entry was greater in WT MEFs compared with viperin KO MEFs after MCMV infection. Our data indicated that the efficiency of viral entry is inversely proportional to the expression levels of ISGs shown in both cell types. Our data also suggested that although viperin increases viral replication by modulating cellular metabolism in the late stage of human cytomegalovirus infection (24,32), the expression levels of ISGs mediated by viperin may determine viral infectivity in the early stage of CMV infection. Alternatively, the efficiency of MCMV entry in cells infected with MCMV in the presence of IFNs may be affected by viperin itself. Upon a combined treatment of CMV and IFN, viperin is highly induced and its antiviral or proviral activity may differently acts on BMDMs and MEFs.
In conclusion, we demonstrated that viperin differentially regulates expression of ISGs in distinct cell types. The data suggested that viperin is a key regulator in production of inflammatory molecules such as IFNs, ISGs, and cytokines in innate immune responses, and its regulation mechanism is dependent on cell type or stimulus. Our findings may provide a clue to develop new strategies of IFN therapy in immune-mediated or infection-associated diseases.
ACKNOWLEDGEMENTS
This study was supported by grants from the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2019R1H1A2079735 and 2013M3A9D5072550) and a faculty research grant from Yonsei University College of Medicine for 2018 (6-2018-0168) to J.-Y. Seo, and the Brain Korea 21 PLUS Project for Medical Science, Yonsei University.
Abbreviations
- BCA
bicinchoninic acid
- BMDM
bone marrow-derived macrophages
- Bst-2
bone marrow stromal cell antigen-2
- CMV
cytomegalovirus
- Gbp2
guanylate binding protein 2
- IE1
immediate early 1
- IRAK1
IL-1 receptor associated kinase 1
- IRF
IFN-regulatory factor
- ISG
interferon-stimulated gene
- Isg15
interferon-stimulated gene 15
- ISGF3
IFN-stimulated gene factor 3
- KO
knockout
- M1
classically activated macrophages
- M2
alternatively activated macrophages
- MAVS
mitochondrial antiviral signaling protein
- MCMV
murine cytomegalovirus
- MEF
murine embryonic fibroblasts
- MOI
multiplicity of infection
- Mx2
myxovirus resistance dynamin like GTPase 2
- Oas
2′5′-oligoadenylate synthetase
- pDC
plasmacytoid dendritic cell
- Pkr
IFN-inducible dsRNA-dependent protein kinase
- Poly(I:C)
polyinosinic-polycytidylic acid
- qRT-PCR
quantitative real-time PCR
- TRAF6
TNF receptor associated factor 6
- WT
wild type
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Kim JJ, Seo JY.
- Data curation: Kim JJ, Seo JY.
- Formal analysis: Kim JJ, Kim KS.
- Funding acquisition: Seo JY.
- Investigation: Kim JJ, Kim KS, Eom J, Lee JB, Seo JY.
- Supervision: Seo JY.
- Validation: Kim JJ, Kim KS.
- Writing - original draft: Kim JJ.
- Writing - review & editing: Seo JY.
SUPPLEMENTARY MATERIALS
Primer sequences used for qRT-PCR
Viperin upregulates Isg56 expression in both BMDMs and MEFs treated with type I IFN. (A, B) The effect of viperin on the expression of Isg56 in BMDMs and MEFs upon type I IFN treatment. WT and viperin KO BMDMs (A) or MEFs (B) were treated with or without type I IFN (1,000 U/ml) for 24 h. The mRNA expression levels of Isg56 in the cells were measured by qRT-PCR and normalized to β-actin mRNA. Data are presented as mean±SEM of triplicate samples and are representative of three individual experiments.
*p<0.05; ***p<0.001.
The efficiency of MCMV entry depends on viperin-mediated ISG expression. (A, B) The efficiency of MCMV entry into BMDMs infected with MCMV in the absence or presence of IFNs. WT and viperin KO BMDMs were treated with or without type I IFN (1,000 U/ml) or IFN-γ (100 ng/ml) for 8 h and then infected with MCMV at an MOI of 0.2 for 24 h. The cells were stained with antibody specific to the MCMV protein IE1 (green) to identify infected cells. Nuclei were stained with DAPI (blue). A representative image from 2 individual experiments was shown (scale bar=100 μm) (A). The efficiency of MCMV entry into the cells was quantitated (B). The infected cells were counted in each image (n=10). The percentage of MCMV positive cells per total cells in each image was calculated. Data are presented as mean±SEM.
**p<0.01; ***p<0.001.
References
- 1.Bowie AG, Unterholzner L. Viral evasion and subversion of pattern-recognition receptor signalling. Nat Rev Immunol. 2008;8:911–922. doi: 10.1038/nri2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Veer MJ, Holko M, Frevel M, Walker E, Der S, Paranjape JM, Silverman RH, Williams BR. Functional classification of interferon-stimulated genes identified using microarrays. J Leukoc Biol. 2001;69:912–920. [PubMed] [Google Scholar]
- 3.Schneider WM, Chevillotte MD, Rice CM. Interferon-stimulated genes: a complex web of host defenses. Annu Rev Immunol. 2014;32:513–545. doi: 10.1146/annurev-immunol-032713-120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425–6440. doi: 10.1002/jcp.26429. [DOI] [PubMed] [Google Scholar]
- 5.Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32:593–604. doi: 10.1016/j.immuni.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Liu YC, Zou XB, Chai YF, Yao YM. Macrophage polarization in inflammatory diseases. Int J Biol Sci. 2014;10:520–529. doi: 10.7150/ijbs.8879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease. Nature. 2013;496:445–455. doi: 10.1038/nature12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer-Barber KD, Yan B. Clash of the Cytokine Titans: counter-regulation of interleukin-1 and type I interferon-mediated inflammatory responses. Cell Mol Immunol. 2017;14:22–35. doi: 10.1038/cmi.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalliolias GD, Ivashkiv LB. Overview of the biology of type I interferons. Arthritis Res Ther. 2010;12(Suppl 1):S1. doi: 10.1186/ar2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.John SP, Sun J, Carlson RJ, Cao B, Bradfield CJ, Song J, Smelkinson M, Fraser ID. IFIT1 exerts opposing regulatory effects on the inflammatory and interferon gene programs in LPS-activated human macrophages. Cell Reports. 2018;25:95–106.e6. doi: 10.1016/j.celrep.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tecalco Cruz AC, Mejía-Barreto K. Cell type-dependent regulation of free ISG15 levels and ISGylation. J Cell Commun Signal. 2017;11:127–135. doi: 10.1007/s12079-017-0385-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fan JB, Miyauchi-Ishida S, Arimoto K, Liu D, Yan M, Liu CW, Győrffy B, Zhang DE. Type I IFN induces protein ISGylation to enhance cytokine expression and augments colonic inflammation. Proc Natl Acad Sci U S A. 2015;112:14313–14318. doi: 10.1073/pnas.1505690112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pang X, Li X, Mo Z, Huang J, Deng H, Lei Z, Zheng X, Feng Z, Xie D, Gao Z. IFI16 is involved in HBV-associated acute-on-chronic liver failure inflammation. BMC Gastroenterol. 2018;18:61. doi: 10.1186/s12876-018-0791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trahey M, Weissman IL. Cyclophilin C-associated protein: a normal secreted glycoprotein that down-modulates endotoxin and proinflammatory responses in vivo. Proc Natl Acad Sci U S A. 1999;96:3006–3011. doi: 10.1073/pnas.96.6.3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lynch MD, Watt FM. Fibroblast heterogeneity: implications for human disease. J Clin Invest. 2018;128:26–35. doi: 10.1172/JCI93555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamada A, Torre C, Drancourt M, Ghigo E. Trained immunity carried by non-immune cells. Front Microbiol. 2019;9:3225. doi: 10.3389/fmicb.2018.03225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buechler MB, Turley SJ. A short field guide to fibroblast function in immunity. Semin Immunol. 2018;35:48–58. doi: 10.1016/j.smim.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Jones PH, Mehta HV, Maric M, Roller RJ, Okeoma CM. Bone marrow stromal cell antigen 2 (BST-2) restricts mouse mammary tumor virus (MMTV) replication in vivo. Retrovirology. 2012;9:10. doi: 10.1186/1742-4690-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perwitasari O, Cho H, Diamond MS, Gale M., Jr Inhibitor of κB kinase ε (IKKε), STAT1, and IFIT2 proteins define novel innate immune effector pathway against West Nile virus infection. J Biol Chem. 2011;286:44412–44423. doi: 10.1074/jbc.M111.285205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tallóczy Z, Virgin HW, 4th, Levine B. PKR-dependent autophagic degradation of herpes simplex virus type 1. Autophagy. 2006;2:24–29. doi: 10.4161/auto.2176. [DOI] [PubMed] [Google Scholar]
- 21.Chin KC, Cresswell P. Viperin (cig5), an IFN-inducible antiviral protein directly induced by human cytomegalovirus. Proc Natl Acad Sci U S A. 2001;98:15125–15130. doi: 10.1073/pnas.011593298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu H, Cong JP, Shenk T. Use of differential display analysis to assess the effect of human cytomegalovirus infection on the accumulation of cellular RNAs: induction of interferon-responsive RNAs. Proc Natl Acad Sci U S A. 1997;94:13985–13990. doi: 10.1073/pnas.94.25.13985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seo JY, Yaneva R, Cresswell P. Viperin: a multifunctional, interferon-inducible protein that regulates virus replication. Cell Host Microbe. 2011;10:534–539. doi: 10.1016/j.chom.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seo JY, Yaneva R, Hinson ER, Cresswell P. Human cytomegalovirus directly induces the antiviral protein viperin to enhance infectivity. Science. 2011;332:1093–1097. doi: 10.1126/science.1202007. [DOI] [PubMed] [Google Scholar]
- 25.Jiang D, Guo H, Xu C, Chang J, Gu B, Wang L, Block TM, Guo JT. Identification of three interferon-inducible cellular enzymes that inhibit the replication of hepatitis C virus. J Virol. 2008;82:1665–1678. doi: 10.1128/JVI.02113-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rivieccio MA, Suh HS, Zhao Y, Zhao ML, Chin KC, Lee SC, Brosnan CF. TLR3 ligation activates an antiviral response in human fetal astrocytes: a role for viperin/cig5. J Immunol. 2006;177:4735–4741. doi: 10.4049/jimmunol.177.7.4735. [DOI] [PubMed] [Google Scholar]
- 27.Wang X, Hinson ER, Cresswell P. The interferon-inducible protein viperin inhibits influenza virus release by perturbing lipid rafts. Cell Host Microbe. 2007;2:96–105. doi: 10.1016/j.chom.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Burke CW, Ryman KD, Klimstra WB. Identification and characterization of interferon-induced proteins that inhibit alphavirus replication. J Virol. 2007;81:11246–11255. doi: 10.1128/JVI.01282-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saitoh T, Satoh T, Yamamoto N, Uematsu S, Takeuchi O, Kawai T, Akira S. Antiviral protein Viperin promotes Toll-like receptor 7- and Toll-like receptor 9-mediated type I interferon production in plasmacytoid dendritic cells. Immunity. 2011;34:352–363. doi: 10.1016/j.immuni.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 30.Eom J, Kim JJ, Yoon SG, Jeong H, Son S, Lee JB, Yoo J, Seo HJ, Cho Y, Kim KS, et al. Intrinsic expression of viperin regulates thermogenesis in adipose tissues. Proc Natl Acad Sci U S A. 2019;116:17419–17428. doi: 10.1073/pnas.1904480116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qiu LQ, Cresswell P, Chin KC. Viperin is required for optimal Th2 responses and T-cell receptor-mediated activation of NF-κB and AP-1. Blood. 2009;113:3520–3529. doi: 10.1182/blood-2008-07-171942. [DOI] [PubMed] [Google Scholar]
- 32.Seo JY, Cresswell P. Viperin regulates cellular lipid metabolism during human cytomegalovirus infection. PLoS Pathog. 2013;9:e1003497. doi: 10.1371/journal.ppat.1003497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jang JS, Lee JH, Jung NC, Choi SY, Park SY, Yoo JY, Song JY, Seo HG, Lee HS, Lim DS. Rsad2 is necessary for mouse dendritic cell maturation via the IRF7-mediated signaling pathway. Cell Death Dis. 2018;9:823. doi: 10.1038/s41419-018-0889-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eom J, Yoo J, Kim JJ, Lee JB, Choi W, Park CG, Seo JY. Viperin deficiency promotes polarization of macrophages and secretion of M1 and M2 cytokines. Immune Netw. 2018;18:e32. doi: 10.4110/in.2018.18.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carissimo G, Teo TH, Chan YH, Lee CY, Lee B, Torres-Ruesta A, Tan JJ, Chua TK, Fong SW, Lum FM, et al. Viperin controls chikungunya virus-specific pathogenic T cell IFNγ Th1 stimulation in mice. Life Sci Alliance. 2019;2:e201900298. doi: 10.26508/lsa.201900298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hee JS, Cresswell P. Viperin interaction with mitochondrial antiviral signaling protein (MAVS) limits viperin-mediated inhibition of the interferon response in macrophages. PLoS One. 2017;12:e0172236. doi: 10.1371/journal.pone.0172236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ryu SH, Na HY, Sohn M, Han SM, Choi W, In H, Hong S, Jeon H, Seo JY, Ahn J, et al. Reduced expression of granule proteins during extended survival of eosinophils in splenocyte culture with GM-CSF. Immunol Lett. 2016;173:7–20. doi: 10.1016/j.imlet.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 38.Lissner MM, Thomas BJ, Wee K, Tong AJ, Kollmann TR, Smale ST. Age-related gene expression differences in monocytes from human neonates, young adults, and older adults. PLoS One. 2015;10:e0132061. doi: 10.1371/journal.pone.0132061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Josset L, Tchitchek N, Gralinski LE, Ferris MT, Eisfeld AJ, Green RR, Thomas MJ, Tisoncik-Go J, Schroth GP, Kawaoka Y, et al. Annotation of long non-coding RNAs expressed in collaborative cross founder mice in response to respiratory virus infection reveals a new class of interferon-stimulated transcripts. RNA Biol. 2014;11:875–890. doi: 10.4161/rna.29442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ouda R, Sarai N, Nehru V, Patel MC, Debrosse M, Bachu M, Chereji RV, Eriksson PR, Clark DJ, Ozato K. SPT6 interacts with NSD2 and facilitates interferon-induced transcription. FEBS Lett. 2018;592:1681–1692. doi: 10.1002/1873-3468.13069. [DOI] [PubMed] [Google Scholar]
- 41.Bachu M, Tamura T, Chen C, Narain A, Nehru V, Sarai N, Ghosh SB, Ghosh A, Kavarthapu R, Dufau ML, et al. A versatile mouse model of epitope-tagged histone H3.3 to study epigenome dynamics. J Biol Chem. 2019;294:1904–1914. doi: 10.1074/jbc.RA118.005550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Platanias LC. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nat Rev Immunol. 2005;5:375–386. doi: 10.1038/nri1604. [DOI] [PubMed] [Google Scholar]
- 43.Lindqvist R, Kurhade C, Gilthorpe JD, Överby AK. Cell-type- and region-specific restriction of neurotropic flavivirus infection by viperin. J Neuroinflammation. 2018;15:80. doi: 10.1186/s12974-018-1119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Platanitis E, Demiroz D, Schneller A, Fischer K, Capelle C, Hartl M, Gossenreiter T, Müller M, Novatchkova M, Decker T. A molecular switch from STAT2-IRF9 to ISGF3 underlies interferon-induced gene transcription. Nat Commun. 2019;10:2921. doi: 10.1038/s41467-019-10970-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ooi EL, Chan ST, Cho NE, Wilkins C, Woodward J, Li M, Kikkawa U, Tellinghuisen T, Gale M, Jr, Saito T. Novel antiviral host factor, TNK1, regulates IFN signaling through serine phosphorylation of STAT1. Proc Natl Acad Sci U S A. 2014;111:1909–1914. doi: 10.1073/pnas.1314268111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Psarras A, Emery P, Vital EM. Type I interferon-mediated autoimmune diseases: pathogenesis, diagnosis and targeted therapy. Rheumatology (Oxford) 2017;56:1662–1675. doi: 10.1093/rheumatology/kew431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primer sequences used for qRT-PCR
Viperin upregulates Isg56 expression in both BMDMs and MEFs treated with type I IFN. (A, B) The effect of viperin on the expression of Isg56 in BMDMs and MEFs upon type I IFN treatment. WT and viperin KO BMDMs (A) or MEFs (B) were treated with or without type I IFN (1,000 U/ml) for 24 h. The mRNA expression levels of Isg56 in the cells were measured by qRT-PCR and normalized to β-actin mRNA. Data are presented as mean±SEM of triplicate samples and are representative of three individual experiments.
*p<0.05; ***p<0.001.
The efficiency of MCMV entry depends on viperin-mediated ISG expression. (A, B) The efficiency of MCMV entry into BMDMs infected with MCMV in the absence or presence of IFNs. WT and viperin KO BMDMs were treated with or without type I IFN (1,000 U/ml) or IFN-γ (100 ng/ml) for 8 h and then infected with MCMV at an MOI of 0.2 for 24 h. The cells were stained with antibody specific to the MCMV protein IE1 (green) to identify infected cells. Nuclei were stained with DAPI (blue). A representative image from 2 individual experiments was shown (scale bar=100 μm) (A). The efficiency of MCMV entry into the cells was quantitated (B). The infected cells were counted in each image (n=10). The percentage of MCMV positive cells per total cells in each image was calculated. Data are presented as mean±SEM.
**p<0.01; ***p<0.001.