Abstract
BACKGROUND
Complications of Crohn’s disease such as intestinal obstruction, fistula or perforation often need surgical treatment. Nearly 70%-80% patients with Crohn’s disease would receive surgical treatment during the lifetime. However, surgical treatment is incurable for Crohn’s disease. The challenge of recurrence postoperatively troubles both doctors and patients. Over 50% patients would suffer recurrence postoperatively. Some certain risk factors are associated with recurrence of Crohn’s disease.
AIM
To evaluate the risk factors for endoscopic recurrence and clinical recurrence after bowel resection in Crohn’s disease.
METHODS
Patients diagnosed Crohn’s disease and received intestinal resection between April 2007 and December 2013 were included in this study. Data on the general demographic information, preoperative clinical characteristics, surgical information, postoperative clinical characteristics were collected. Continuous data are expressed as median (inter quartile range), and categorical data as frequencies and percentages. Kaplan-Meier method was applied to estimate the impact of the clinical variables above on the cumulative rate of postoperative endoscopic recurrence and clinical recurrence, then log-rank test was applied to test the homogeneity of those clinical variables. Multivariate Cox proportional hazard regression analysis was performed to identify the risk factors of postoperative endoscopic recurrence and clinical recurrence.
RESULTS
A total of 64 patients were included in this study. The median follow-up time for the patients was 17 (9.25-25.75) mo. In this period, 41 patients (64.1%) had endoscopic recurrence or clinical recurrence. Endoscopic recurrence occurred in 34 (59.6%) patients while clinical recurrence occurred in 28 (43.8%) patients, with the interval between the operation and recurrence of 13.0 (8.0-24.5) months and 17.0 (8.0-27.8) mo, respectively. In univariate analysis, diagnosis at younger age (P < 0.001), disease behavior of penetrating (P = 0.044) and preoperative use of anti-tumor necrosis factor (TNF) (P = 0.020) were significantly correlated with endoscopic recurrence, while complication with perianal lesions (P = 0.032) and preoperative use of immunomodulatory (P = 0.031) were significantly correlated with clinical recurrence. As to multivariate analysis, diagnostic age (P = 0.004), disease behavior (P = 0.041) and preoperative use of anti-TNF (P = 0.010) were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions (P = 0.023) was an independent prognostic factor for clinical recurrence.
CONCLUSION
Diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were independent risk factors for postoperative recurrence in Crohn’s disease.
Keywords: Risk factor, Endoscopic recurrence, Clinical recurrence, Bowel resection, Crohn’s disease
Core tip: Our study aimed at evaluating the risk factors for recurrence after bowel resection in Crohn’s disease. This study included 64 patients diagnosed Crohn’s disease and received intestinal resection. The result showed that diagnosis at younger age, disease behavior of penetrating and preoperative use of anti-tumor necrosis factor were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions was an independent prognostic factor for clinical recurrence.
INTRODUCTION
Crohn’s disease, one kind of inflammatory bowel disease, is a chronic inflammatory disorder in the digestive tract, with an incidence and prevalence of 6-15 and 50-200 per 100000 persons, respectively[1]. Although there has been significant improvement in the diagnosis and conservative medical treatment, the risk of surgical resection for Crohn’s disease could be as high as 70% to 80% during the lifetime[2,3]. Unlike the curability of operation for ulcerative colitis, surgical treatment can only help to resolve the complications of Crohn’s disease, such as intestinal obstruction, fistula or perforation. In other words, surgical treatment is incurable for Crohn’s disease. The challenge of recurrence postoperatively troubles both doctors and patients.
Buisson et al[4] reviewed the rates and risk factors for clinical and endoscopic recurrence in population-based studies, and found that approximately half of patients experienced clinical recurrence at 10 years. And Watanabe et al[5] found that overall 5-year and 10-year cumulative reoperation rates were 31.4% and 61.2% in Japan, respectively. Many factors were found related with postoperative recurrence, such as disease behavior, use of medicine and technique of surgery[6-8]. Most these studies were about population from Caucasians and Southeast Asia such as Japan and South Korea. Our study aims to evaluate the risk factors for recurrence after bowel resection in patients with Crohn’s disease, from a tertiary care center in China.
MATERIALS AND METHODS
Patients selection
Patients diagnosed Crohn’s disease and received intestinal resection between April 2007 and December 2013 at the Sixth Affiliated Hospital, Sun Yat-Sen University were enrolled in this study. Data on the general demographic information, preoperative clinical characteristics, surgical information, postoperative clinical characteristics were obtained by careful chart review, including sex, diagnostic age, disease-behavior, anatomical site of disease, perianal lesions, preoperative body mass index, preoperative laboratory examinations, preoperative medication [corticosteroid, immunosuppressant, anti-tumor necrosis factor (TNF)], preoperative duration of disease, indication of operation, postoperative laboratory examinations, postoperative colonoscopy, time of endoscopic recurrence and clinical recurrence. Endoscopic recurrence was defined as the presence of aphthous ulcer, deep and large ulcer, nodular hyperplasia and stenosis at the anastomotic site and in the intestinal wall of the anastomotic site confirmed by postoperative colonoscopy. Clinical recurrence was defined as symptom recurrence including obvious abdominal pain, diarrhea, abdominal mass and extraintestinal manifestations, accompanied with imaging and endoscopic lesions; or complications such as abdominal abscess, fistula formation and intestinal obstruction which may require a second operation.
Statistical analysis
Data analyses were performed with the Statistical Package for Social Science software, version 21.0 (SPSS Inc., Chicago, IL, United States). Continuous data are expressed as median (inter quartile range), and categorical data as frequencies and percentages. Kaplan-Meier method was applied to estimate the impact of the clinical variables above on the cumulative rate of postoperative endoscopic recurrence and clinical recurrence, then log-rank test was applied to test the homogeneity of those clinical variables. Multivariate Cox proportional hazard regression analysis was performed to identify the risk factors of postoperative endoscopic recurrence and clinical recurrence. The differences were considered statistically significant when the two-sided P values were < 0.05.
RESULTS
Patient characteristics and surgical variables
A total of 64 patients were included in our study. The average age at diagnosis was 29.23 years old, while the gender ratio was 2.76:1 (male:female 47/17). The distribution of diagnostic age was single-peak curve, with the peak age of 22-36 years old. As to the Montreal classification, 49 (76.6%) patients were A2 subtype; L3 subtype account for 73.4% (47 patients); and most patients manifested B2 subtype (25/39.1%) or B3 subtype (37/57.8%) of disease behavior. 22(34.4%) patients complicated with perianal lesions. Preoperative use of medication was found in 29 patients (45.3%), including 23 cases of steroid, 24 cases of immunomodulator and 4 cases of anti-TNF. The clinicopathological characteristics of the patients are summarized in Table 1.
Table 1.
Demographic and clinical characteristics of the patients, n (%)
| Variables | Number of patients |
| Gender | |
| Male | 47 (73.4) |
| Female | 17 (26.6) |
| Age at diagnosis | 27.5 (8, 78) |
| Disease period before operation | 9.5 (2.0, 48.0) |
| Montreal classification | |
| Age, yr | |
| A1 (≤ 16) | 6 (9.4) |
| A2 (17-40) | 49 (76.6) |
| A3 (> 40) | 9 (14.1) |
| Behavior | |
| B1 (Inflammatory) | 2 (3.1) |
| B2 (Stricturing) | 25 (39.1) |
| B3 (Penetrating) | 37 (57.8) |
| Location | |
| L1 (Terminal ileum) | 9 (14.1) |
| L2 (Colon) | 1 (1.6) |
| L3 (Ileocolon) | 47 (73.4) |
| L4 (Upper disease) | 7 (10.9) |
| Perianal disease | 22 (34.4) |
| Preoperative use of medication | 29 (45.3) |
| Steroid | 23 (35.9) |
| Immunomodulator | 24 (37.5) |
| Anti-TNF | 4 (6.2) |
TNF: Tumor necrosis factor.
As to the indications of operation, most patients had to receive operation because of intestinal obstruction (27 cases, 42.3%) and intestinal fistula (34cases, 53.1%). 47 patients who exhibited disease in the ileocolon (L3) mentioned above received ileocolonic resection and 15 patients received intestinal resection. Detail about the surgery was showed in Table 2.
Table 2.
Surgical details, n (%)
| Variables | Number of patients |
| Indication of surgery | |
| Intestinal obstruction | 27 (42.3) |
| Intestinal fistula | 34 (53.1) |
| Abscess | 2 (3.2) |
| Bleeding | 1 (1.6) |
| Site of resection | |
| Ileocolon | 47 (73.4) |
| Intestine | 15 (23.4) |
| Colon | 1 (1.6) |
Recurrence
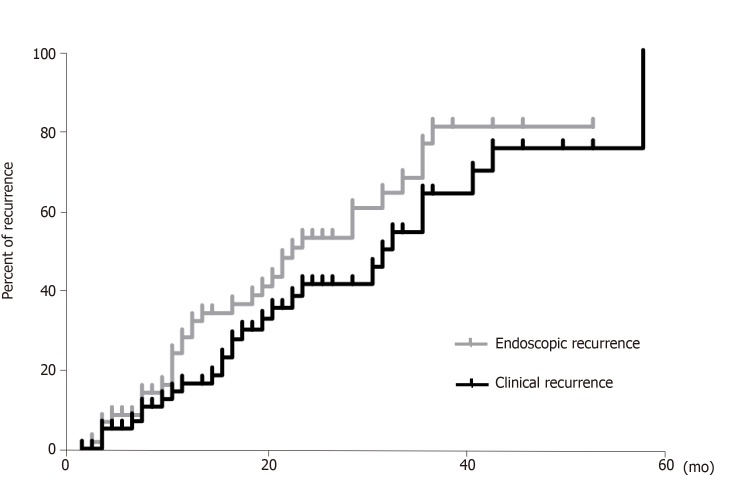
The median follow-up time for the patients was 17 (9.25-25.75) mo. In this period, 41 patients (64.1%) had endoscopic recurrence or clinical recurrence. Endoscopic recurrence occurred in 34 (59.6%) patients while clinical recurrence occurred in 28 (43.8%) patients, with the interval between the operation and recurrence of 13.0 (8.0-24.5) mo and 17.0 (8.0-27.8) mo, respectively. 6 (9.4%) patients needed reoperation because of recurrence. The cumulative rate of endoscopic recurrence was 37.0%, 60.0% and 90.0% at 12, 24 and 36 mo, respectively, after intestinal resection. And the cumulative rate of clinical recurrence was 18.0%, 44.0% and 67.0% at 12, 24 and 36 mo, respectively. The cumulative incidence curve was showed in Figure 1.
Figure 1.
Kaplan–Meier curves for endoscopic recurrence and clinical recurrence.
The endoscopic recurrence rate for patients with age ≤ 16, between 17-40 and > 40 was 100.0%, 63.0% and 12.5%, respectively; and diagnosis at younger age was significantly correlated with endoscopic recurrence (P < 0.001). The endoscopic recurrence rate for patients with B1, B2 and B3 subtype of disease behavior was 0.0%, 50.9%, 73.2%, respectively; and disease behavior of penetrating was significantly correlated with endoscopic recurrence (P = 0.044). Moreover, preoperative use of anti-TNF (P = 0.020) were significantly correlated with endoscopic recurrence, while complication with perianal lesions (P = 0.032) and preoperative use of immunomodulatory (P = 0.031) were significantly correlated with clinical recurrence. As to multivariate analysis, diagnostic age [Hazard ratio (HR) 0.323, 95% confidence interval (CI): 0.148-0.703, P = 0.004], disease behavior (HR 1.969, 95%CI: 1.028-3.775, P = 0.041) and preoperative use of anti-TNF (HR 4.414, 95%CI: 1.424-13.682, P = 0.010) were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions (HR 2.956, 95%CI: 1.163-7.513, P = 0.023) was an independent prognostic factor for clinical recurrence. Results of univariate and multivariate analyses were showed in Table 3.
Table 3.
Univariate and multivariate analysis of factors associated with endoscopic recurrence and clinical recurrence
| Variable |
Endoscopic recurrence |
Clinical recurrence |
||
| Univariate | Multivariate | Univariate | Multivariate | |
| Gender | 0.683 | 0.939 | ||
| Diagnostic age | 0.000b | 0.004b | 0.422 | |
| Disease behavior | 0.044a | 0.041a | 0.686 | |
| Disease location | 0.146 | 0.315 | ||
| Perianal disease | 0.357 | 0.032a | 0.023a | |
| Preoperative use of steroid | 0.739 | 0.700 | ||
| Preoperative use of immunomodulator | 0.085 | 0.031a | 0.092 | |
| Preoperative use of anti-TNF | 0.020a | 0.010a | 0.438 | |
| Preoperative body mass index level | 0.230 | 0.705 | ||
| Preoperative leukocytosis | 0.760 | 0.627 | ||
| Preoperative C-reactive protein level | 0.290 | 0.917 | ||
| Preoperative erythrocyte sedimentation rate level | 0.078 | 0.247 | ||
| Preoperative albumin level | 0.368 | 0.271 | ||
P < 0.05,
P < 0.01. TNF: Tumor necrosis factor.
DISCUSSION
Crohn’s disease is characterized by relapsing episodes of active inflammation alternating with remission of disease[9]. Recurrence is a common but intractable problem for the patients with Crohn’s disease even if they received surgical therapy. It is well known that anastomotic recurrence occurs endoscopically as early as several months after bowel resection and anastomosis, followed by symptomatic recurrence[10]. The rate of postoperative recurrence varied in different studies. Endoscopic studies have shown that up to 70% patients developed endoscopic recurrence within 1 year and nearly all the patients would have new lesions in the neoterminal ileum at 3 years after resection[11,12]. Rutgeerts reported that about 20%-30% patients would have a clinical recurrence within the first year after curative resection of the ileum or ileocolon with ileocolonic anastomosis, with a 10% increase after each subsequent year[13]. In our study, the cumulative rate of endoscopic recurrence was 37.0%, 60.0% and 90.0% at 12, 24 and 36 mo after intestinal resection and the cumulative rate of clinical recurrence was 18.0%, 44.0% and 67. 0% respectively. The recurrence rate in our study was similar to the previous reported results.
Many prognostic factors have been investigated to predict postoperative recurrence. The presence of perianal disease has been proved one of the predictors of postoperative recurrence by many previous studies. Bernell et al[14] found perianal fistulas increased the relative risk (RR) of recurrence after resection in Crohn’s disease (RR 1.4, 95%CI, 1.2-1.7). Beaugerie et al[15] found the presence of perianal disease significantly associated with subsequent 5-year disease disabling course (overall risk 1.8, 95%CI, 1.2-2.8), which meant more patients with perianal disease required early intensive therapy and suffered from disabling chronic symptoms. Another study from Korea showed patients with perianal Crohn’s disease had a higher risk of reoperation[16]. In our study, we also found preoperative complication with perianal lesions was an independent prognostic factor for clinical recurrence.
Medication is also an important predictor for recurrence of Crohn’s disease. Many studies focused on postoperative medication. Yoshida et al[17] conducted a 3-year prospective randomized open trial about the effect of postoperative scheduled infliximab monotherapy on recurrence of Crohn’s disease, and the result showed that an early intervention with infliximab monotherapy should prevent clinical, serological, and endoscopic Crohn’s disease recurrence following ileocolic resection. Yang et al[8] found postoperative use of anti-TNF agents could reduce the risk of reoperation. Immunomodulators such as 6-MP or azathioprine are also widely used postoperatively and were found independently associated with reduction in surgical rate[18,19]. In our study, we focused on the preoperative medication and found preoperative use of anti-TNF was significantly associated with endoscopic recurrence and preoperative use of immunomodulatory seemed correlated with clinical recurrence. The opposite effects of postoperative and preoperative medication on postoperative recurrence of Crohn’s disease might be due to different severity of disease as in our hospital, preoperative medication especially anti-TNF tended to be used in patients with more aggravated disease.
Other risk factors for postoperative recurrence which have been found in published studies included younger diagnostic age, perforating type of disease, sex, smoking and so on[7,20]. In our study, we also found diagnosis at younger age and disease behavior of penetrating were associated with an increased risk for endoscopic recurrence.
In conclusion, this retrospective study of Crohn’s disease in China revealed that diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were independent risk factors for postoperative recurrence.
ARTICLE HIGHLIGHTS
Research background
Nearly 70%-80% patients with Crohn’s disease would receive surgical treatment during the lifetime. However, surgical treatment is incurable for Crohn’s disease. The challenge of recurrence postoperatively troubles both doctors and patients. Over 50% patients would suffer recurrence postoperatively.
Research motivation
A great amount of patients with Crohn’s disease would receive surgical treatment but over one half patients would suffer recurrence postoperatively. It is important to recognize the risk factor for postoperative recurrence. Further clinical research base on certain risk factor would favor the prognosis.
Research objectives
This study aims to evaluate the risk factor of endoscopic recurrence and clinical recurrence after bowel resection for Crohn’s disease. Further relative clinical research could focus on the risk factor found in this study and help to improve the prognosis for certain patients.
Research methods
Patients diagnosed Crohn’s disease and received intestinal resection were included in this study. Data on the general demographic information, preoperative clinical characteristics, surgical information, postoperative clinical characteristics were collected. Continuous data are expressed as median (inter quartile range), and categorical data as frequencies and percentages. Kaplan-Meier method was applied to estimate the impact of the clinical variables above on the cumulative rate of postoperative endoscopic recurrence and clinical recurrence, then log-rank test was applied to test the homogeneity of those clinical variables. Multivariate Cox proportional hazard regression analysis was performed to identify the risk factors of postoperative endoscopic recurrence and clinical recurrence.
Research results
Diagnosis at younger age, disease behavior of penetrating and preoperative use of anti-tumor necrosis factor (TNF) were significantly correlated with endoscopic recurrence, while complication with perianal lesions and preoperative use of immunomodulatory were significantly correlated with clinical recurrence. As to multivariate analysis, diagnostic age, disease behavior and preoperative use of anti-TNF were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions was an independent prognostic factor for clinical recurrence. The result of this study discovered some risk factors for recurrence in patients with Crohn’s disease after bowel resection. Prospective clinical study with more patients remains to be performed to confirm the result.
Research conclusions
Diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were independent risk factors for postoperative recurrence in Crohn’s disease. Patients with younger diagnostic age, disease behavior of penetrating and preoperative use of anti-TNF tended to have endoscopic recurrence, while patients with perianal lesions tended to suffer from clinical recurrence. Some certain factors are associated with postoperative recurrence of Crohn’s disease. In this study, diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were proved as independent prognostic factors. The recurrence rate of Crohn’s disease after bowel resection is high and some certain clinical factors have been proved associated with postoperative recurrence. In this study, we found diagnostic age, disease behavior and preoperative use of anti-TNF were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions was an independent prognostic factor for clinical recurrence. Diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were related with postoperative recurrence in Crohn’s disease. This study adopts the classical methods. Endoscopic recurrence occurred in 34 (59.6%) patients while clinical recurrence occurred in 28 (43.8%) patients, with the interval between the operation and recurrence of 13.0 (8.0-24.5) mo and 17.0 (8.0-27.8) mo, respectively. Diagnostic age, disease behavior and preoperative use of anti-TNF were independent prognostic factors for endoscopic recurrence, while complication with perianal lesions was an independent prognostic factor for clinical recurrence. Diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were related with postoperative recurrence in Crohn’s disease. Patients with such risk factors should be strictly followed up and receive appropriate medical therapy if necessary.
Research perspectives
Diagnostic age, disease behavior, preoperative use of anti-TNF and complication with perianal lesions were independent risk factors for postoperative recurrence in Crohn’s disease. Prospective clinical study with more patients remains to be performed to confirm the results. Prospective clinical trial with multi centers and more patients would be the best method for future research.
Footnotes
Institutional review board statement: The study was approved by the ethics committee of the Sixth Affiliated Hospital, Sun Yat-Sen University.
Informed consent statement: All patients gave informed consent.
Conflict-of-interest statement: All the Authors have no conflict of interest related to the manuscript.
STROBE statement: The authors have read the STROBE Statement, and the manuscript was prepared and revised according to the STROBE Statement.
Manuscript source: Unsolicited manuscript
Peer-review started: May 23, 2019
First decision: August 1, 2019
Article in press: September 20, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D, D, D
Grade E (Poor): 0
P-Reviewer: Bramhall S, Cerwenka H, Chiu KW, Hashimoto N, Papamichael K, Vorobjova T S-Editor: Yan JP L-Editor: A E-Editor: Liu MY
Contributor Information
Ze-Xian Chen, Department of Colorectal Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China.
Yong-Le Chen, Department of Colorectal Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China.
Xiao-Ming Huang, Department of Hepatobiliary Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China.
Xu-Tao Lin, Department of Endoscopy Center, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China.
Xiao-Wen He, Department of Colorectal Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China.
Ping Lan, Department of Colorectal Surgery, the Sixth Affiliated Hospital, Sun Yat-Sen University, Guangzhou 510655, Guangdong Province, China. sumslp@163.com.
References
- 1.Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785–1794. doi: 10.1053/j.gastro.2011.01.055. [DOI] [PubMed] [Google Scholar]
- 2.Freeman HJ. Long-term natural history of Crohn's disease. World J Gastroenterol. 2009;15:1315–1318. doi: 10.3748/wjg.15.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Travis SP, Stange EF, Lémann M, Oresland T, Chowers Y, Forbes A, D'Haens G, Kitis G, Cortot A, Prantera C, Marteau P, Colombel JF, Gionchetti P, Bouhnik Y, Tiret E, Kroesen J, Starlinger M, Mortensen NJ European Crohn's and Colitis Organisation. European evidence based consensus on the diagnosis and management of Crohn's disease: current management. Gut. 2006;55 Suppl 1:i16–i35. doi: 10.1136/gut.2005.081950b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buisson A, Chevaux JB, Allen PB, Bommelaer G, Peyrin-Biroulet L. Review article: the natural history of postoperative Crohn's disease recurrence. Aliment Pharmacol Ther. 2012;35:625–633. doi: 10.1111/j.1365-2036.2012.05002.x. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe T, Sasaki I, Sugita A, Fukushima K, Futami K, Hibi T, Watanabe M. Time trend and risk factors for reoperation in Crohn's disease in Japan. Hepatogastroenterology. 2012;59:1081–1086. doi: 10.5754/hge10822. [DOI] [PubMed] [Google Scholar]
- 6.Simillis C, Yamamoto T, Reese GE, Umegae S, Matsumoto K, Darzi AW, Tekkis PP. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn's disease. Am J Gastroenterol. 2008;103:196–205. doi: 10.1111/j.1572-0241.2007.01548.x. [DOI] [PubMed] [Google Scholar]
- 7.Fortinsky KJ, Kevans D, Qiang J, Xu W, Bellolio F, Steinhart H, Milgrom R, Greenberg G, Cohen Z, Macrae H, Stempak J, McLeod R, Silverberg MS. Rates and Predictors of Endoscopic and Clinical Recurrence After Primary Ileocolic Resection for Crohn's Disease. Dig Dis Sci. 2017;62:188–196. doi: 10.1007/s10620-016-4351-7. [DOI] [PubMed] [Google Scholar]
- 8.Yang KM, Yu CS, Lee JL, Kim CW, Yoon YS, Park IJ, Lim SB, Park SH, Ye BD, Yang SK, Kim JC. Risk factors for postoperative recurrence after primary bowel resection in patients with Crohn's disease. World J Gastroenterol. 2017;23:7016–7024. doi: 10.3748/wjg.v23.i38.7016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peyrin-Biroulet L, Loftus EV, Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn's disease in population-based cohorts. Am J Gastroenterol. 2010;105:289–297. doi: 10.1038/ajg.2009.579. [DOI] [PubMed] [Google Scholar]
- 10.Gklavas A, Dellaportas D, Papaconstantinou I. Risk factors for postoperative recurrence of Crohn's disease with emphasis on surgical predictors. Ann Gastroenterol. 2017;30:598–612. doi: 10.20524/aog.2017.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn's disease. Gastroenterology. 1990;99:956–963. doi: 10.1016/0016-5085(90)90613-6. [DOI] [PubMed] [Google Scholar]
- 12.Olaison G, Smedh K, Sjödahl R. Natural course of Crohn's disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut. 1992;33:331–335. doi: 10.1136/gut.33.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutgeerts P. Strategies in the prevention of post-operative recurrence in Crohn's disease. Best Pract Res Clin Gastroenterol. 2003;17:63–73. doi: 10.1053/bega.2002.0358. [DOI] [PubMed] [Google Scholar]
- 14.Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn's disease. Ann Surg. 2000;231:38–45. doi: 10.1097/00000658-200001000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn's disease. Gastroenterology. 2006;130:650–656. doi: 10.1053/j.gastro.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Han YM, Kim JW, Koh SJ, Kim BG, Lee KL, Im JP, Kim JS, Jung HC. Patients with perianal Crohn's disease have poor disease outcomes after primary bowel resection. J Gastroenterol Hepatol. 2016;31:1436–1442. doi: 10.1111/jgh.13310. [DOI] [PubMed] [Google Scholar]
- 17.Yoshida K, Fukunaga K, Ikeuchi H, Kamikozuru K, Hida N, Ohda Y, Yokoyama Y, Iimuro M, Takeda N, Kato K, Kikuyama R, Nagase K, Hori K, Nakamura S, Miwa H, Matsumoto T. Scheduled infliximab monotherapy to prevent recurrence of Crohn's disease following ileocolic or ileal resection: a 3-year prospective randomized open trial. Inflamm Bowel Dis. 2012;18:1617–1623. doi: 10.1002/ibd.21928. [DOI] [PubMed] [Google Scholar]
- 18.Lakatos PL, Golovics PA, David G, Pandur T, Erdelyi Z, Horvath A, Mester G, Balogh M, Szipocs I, Molnar C, Komaromi E, Veres G, Lovasz BD, Szathmari M, Kiss LS, Lakatos L. Has there been a change in the natural history of Crohn's disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012;107:579–588. doi: 10.1038/ajg.2011.448. [DOI] [PubMed] [Google Scholar]
- 19.Peyrin-Biroulet L, Oussalah A, Williet N, Pillot C, Bresler L, Bigard MA. Impact of azathioprine and tumour necrosis factor antagonists on the need for surgery in newly diagnosed Crohn's disease. Gut. 2011;60:930–936. doi: 10.1136/gut.2010.227884. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto T, Watanabe T. Strategies for the prevention of postoperative recurrence of Crohn's disease. Colorectal Dis. 2013;15:1471–1480. doi: 10.1111/codi.12326. [DOI] [PubMed] [Google Scholar]