Abstract
Background
Multiple studies have shown a link between cumulative adverse experiences in childhood and a wide variety of psychosocial problems in later life. There have not been any pertinent representative studies of the German population until now. The goal of this study is to determine the frequency of adverse childhood experiences (ACE), the extent to which they manifest themselves in patterns of co-occurrence, and their possible connection to psychosocial abnormalities in the German population.
Methods
2531 persons (55.4% female) aged 14 years and up (mean [M] = 48.6 years, standard deviation [SD] = 18) were retrospectively studied for ACE and psychosocial abnormalities by means of the Patient Health Questionnaire-4 (PHQ-4) and further questions on aggressiveness and life satisfaction. The frequency of ACE and their cumulative occurrence were analyzed in descriptive terms. Patterns of simultaneously occurring types of ACE were studied with latent class analysis. Associations between ACE and psychosocial abnormalities were tested with logistic regression analyses.
Results
43.7% of the respondents reported at least one ACE; 8.9% reported four or more. The most commonly reported ones were parental separation and divorce (19.4%), alcohol consumption and drug abuse in the family (16.7%), emotional neglect (13.4%), and emotional abuse (12.5%). Four ACE patterns were identified by latent class analysis: no/minimal ACE, household dysfunction, child maltreatment, and multiple ACE. In the cumulative model, the high-risk group with four or more ACE displayed a significantly elevated risk for depressiveness (odds ratio [OR] = 7.8), anxiety (OR = 7.1), physical aggressiveness (OR = 10.5), and impaired life satisfaction (OR = 5.1).
Conclusion
Adverse childhood experiences are common, and their cumulation is associated with markedly increased negative sequelae for the affected persons. Preventive approaches are needed that extend beyond the area of child maltreatment alone and address other problems in the parental home, such as mental illness in the parents. Data acquisition by self-reporting is a limitation of this study.
Adverse childhood experiences (ACEs) include various childhood experiences that can have a persistent negative effect on health and wellbeing (1). The ACE Study investigated the correlation between adverse childhood experiences and negative impacts on those affected. The concept of adverse childhood experiences includes household dysfunction in addition to child maltreatment; this is because, unless problems in the household are included, the long-term effect is attributed only to individual types of abuse, and the cumulative effect of multiple adverse childhood experiences is not examined (1).
A number of studies have investigated the association between combinations of adverse childhood experiences and negative health outcomes (2). There are strong correlations between adverse childhood experiences and alcohol and drug use (odds ratio [OR] = 10.2, 95% confidence interval: [7.6; 13.7]) and suicide attempts (OR = 37.5 [22.2; 63.3]). The framework model and the assumed underlying mechanism of action are shown in the ACE Pyramid (3). At the center of the framework model are maladaptive behaviors, i.e. behaviors that are unfavorable/harmful to health and that are seen as coping strategies and make illnesses or social problems more likely (1, 3). Consequences of adverse childhood experiences can be immediate, such as symptoms of posttraumatic stress following sexual abuse, but may also occur after a lengthy delay (this is particularly common with physical consequences), like those associated with risky behaviors such as smoking. The United Nations have set themselves Sustainable Development Goals to be achieved by the year 2030. In connection with the United Nation’s Development Goals 3 (reduce premature mortality) and 16.2 (end all forms of violence against children) (4), this study provides the first estimates of the frequency of adverse childhood experiences in Germany and their effects through adulthood.
A recent meta-analysis (2) of the long-term consequences of adverse childhood experiences investigated the strength of the correlation between adverse childhood experiences and a range of issues, on the basis of 37 studies. The strongest correlations (OR = 6) were between adverse childhood experiences and alcohol consumption, drug abuse, and interpersonal and self-directed violence. The total prevalence of at least one adverse childhood experience was 57% (43%; 88%). The prevalence of 4 or more adverse childhood experiences was 13% (1%; 38%). While current figures on the frequency of child maltreatment are available for Germany (5, 6) and correlations between individual and multiple forms of abuse and neglect on the one hand and illnesses on the other have been described (7), this study is the first to provide data on the frequency of adverse childhood experiences. This data goes beyond child maltreatment and examines the correlation between abuse and psychosocial issues such as low life satisfaction and aggression, which have received little attention to date. A recent meta-analysis (2) shows no published representative studies conducted in either Germany or continental western Europe.
The studies on the correlation between adverse childhood experiences and negative consequences follow a cumulative risk model (8). The identification of patterns of co-occurring adverse childhood experiences (9) and of correlations between these and psychosocial issues in those affected is also significant.
This study therefore investigates the prevalence of individual adverse childhood experiences in the German population and correlations between these and the outcome variables depression, anxiety, physical aggression, life satisfaction, and equivalent income. In addition to these analyses, which target correlations between psychosocial issues and individual adverse childhood experiences, the theoretical model of adverse childhood experiences also estimates the cumulative effect and patterns of co-occurring adverse childhood experiences in terms of correlations between these and psychosocial issues in those affected.
Methods
Data collection and study participants
The study included 2531 participants. Nationwide data collection was performed via an independent institute for polling and social research (USUMA, Berlin) between November 2017 and February 2018. The inclusion criteria were a minimum age of 14 years and sufficient knowledge of German (see eMethods for details of the study design). Informed consent was a requirement for study participation. The study was approved by the Ethics Committee of the Faculty of Medicine of Leipzig University.
Tools
Sociodemographic information such as age, sex, marital status, number of children, level of education, and religious affiliation was taken from all participants. Equivalent income according to the OECD (Organisation for Economic Co-operation and Development) (10) was also calculated.
Adverse childhood experiences were recorded using the German version (11) of the ACE Questionnaire (1). This consists of 10 items on child maltreatment and problems in the parental home, with yes/no answers (ebox 1). As in previous studies, a total score was used to investigate the risk of an effect of combined adverse childhood experiences (2, 12).
eBOX 1. Sample ACE questions.
German version of the ACE Questionnaire:
Copyright and citations: Ingo Schäfer, Katja Wingenfeld, and Carsten Spitzer (2009) ACE-D; German version of the Adverse Childhood Experience (ACE) Questionnaire. University of Hamburg (11). The whole questionnaire can be obtained from Prof. Dr. Ingo Schäfer.
| Before your 18th birthday: | Yes | No |
| 1. Did a parent or other adult in your household often or very often… …push, grab, hit, or throw something at you? or …ever hit you so hard that you had marks or were injured? | ||
| 2. Was your mother or stepmother… …often or very often pushed, grabbed, hit, or did she have something thrown at her? or …sometimes, often, or very often kicked, bitten, punched, or hit with a hard object? or …ever hit repeatedly for several minutes or more or threatened with a gun or knife? | ||
| 1: sample question under the heading of abuse, on physical abuse 2: sample question under the heading of problems in the parental home, on witnessing domestic violence |
Depression and anxiety were recorded using the Patient Health Questionnaire-4 (PHQ-4) (12– 14) (details in eBox 2).
eBOX 2. Information on PHQ-4.
PHQ-4 (Patient Health Questionnaire-4) consists of 2 items from PHQ-9 (13) on symptoms of depression and 2 items from the Generalized Anxiety Disorder Screener (GAD-7) (14) on symptoms of generalized anxiety disorder. Participants are required to assess whether these symptoms have occurred in the past 2 weeks using a 4-point answer scale. PHQ-4 was found to have good reliability and validity in a German validation study (13). In the sample used in this study, the subscales of PHQ-4 show sufficient reliability in relation to the shortness of the subscales (depression scale: Cronbach’s alpha = 0.79; anxiety scale: Cronbach’s alpha = 0.78). To estimate the prevalence of depression and anxiety, the validated cut-off point =3 was used for both subscales (14).
Physical aggression was investigated using the question “Have you physically attacked (e.g. hit, slapped in the face, pulled hair, threatened with a weapon or other object) anyone in the past 12 months?” The answers to this question were either yes or no.
Life satisfaction was recorded using the question “This question is about your general life satisfaction. How satisfied are you at the moment with your life in general?” The participants could answer this question using an 11-point scale ranging from “not at all satisfied” to “completely satisfied.”
Statistical analyses
Statistical analyses were performed using SPSS, version 21. Patterns of co-occurring adverse childhood experiences were found via latent class analysis (LCA) using MPlus, version 7 (15). The eMethods section contains a detailed description of the LCA procedure.
Where data on certain participants was missing within individual subanalyses, these participants were excluded from the subanalysis in question. The number of missing data points ranged from 2 to a maximum of 20 (0.8%) per subanalysis, depending on the variables included. Correlations were calculated using odds ratios; adjusted odds ratios were calculated using regression.
Results
Of the 2531 study participants, 1401 (55.4%) were female and 1130 (44.6%) male. The mean age was 48.6 years (standard deviation [SD] = 18, [49; 93]). The sample is described in Table 1.
Table 1. Description of sample and sociodemographic characteristics of the 2531 participants in the representative population survey.
| Variable | n (SD) or M (SD) |
| Age (M, SD) | 48.6 (18.0) |
| Sex (n, %) | |
| Female | 1401 (55.4) |
| Male | 1130 (44.6) |
| Marital status | |
| Married, living together | 1066 (42.1) |
| Married, living apart | 65 (2.6) |
| Single | 821 (32.4) |
| Divorced | 341 (13.5) |
| Widowed | 227 (9.0) |
| Not stated | 11 (0.4) |
| No. of children (M, SD) | 1.15 (1.14) |
| German citizenship (n, %) | 2429 (96.0) |
| Highest level of school education (n, %) | |
| School student | 65 (2.6) |
| No school graduation | 56 (2.2) |
| Volks- or Hauptschulabschluss (year 9 lower secondary school certificate |
730 (28.8) |
| Mittlere Reife (year 10 lower secondary school certificate) | 842 (33.3) |
| Graduated from PHS* | 199 (7.9) |
| Graduated from technical college with no accreditation | 88 (3.5) |
| Entrance qualification for technical college/university | 307 (12.1) |
| College/university studies completed | 233 (9.2) |
| Not stated or other | 11 (0.4) |
| Religious affiliation | |
| Protestant | 935 (36.9) |
| Catholic | 748 (29.6) |
| Muslim | 61 (2.4) |
| Other (Jewish, Buddhist, Hindu) | 47 (1.9) |
| No religious affiliation | 640 (25.3) |
| Not stated | 100 (4.0) |
| Equivalent monthly income*2 | |
| Under €500 | 4 (0.2) |
| €500 to €1000 | 209 (8.3) |
| €1000 to €1500 | 518 (20.5) |
| €1500 to €2500 | 1105 (43.7) |
| €2500 to €3500 | 283 (11.2) |
| €3500 to €5000 | 311 (12.3) |
| Over €5000 | 17 (0.7) |
| Not stated | 84 (3.3) |
*1 PHS: Polytechnical high school
*2 Equivalent income: monthly household income in relation to number of individuals in household
SD: Standard deviation; M: Arithmetic mean
A mean of 1.03 (SD = 1.70, [1; 10]) adverse childhood experiences were reported. Table 2 shows the prevalences of individual adverse childhood experiences. The most common were parental divorce/separation (19.4%) and alcohol/drug abuse in the family (16.7%). For individual adverse childhood experiences, there were moderate to strong correlations with depression, anxiety, physical aggression, and low life satisfaction. These associations were weaker when co-occurrence of the other 9 adverse childhood experiences was controlled for. There were moderate correlations between individual adverse childhood experiences and equivalent income.
Table 2. Prevalences of individual adverse childhood experiences (ACEs), odds ratios, and relative odds ratios adjusted for co-occurrence of various adverse childhood experiences, for depression, anxiety, physical aggression, life satisfaction, and monthly income in a representative German sample (n = 2531).
| Total sample | Depression*1 | Anxiety*2 | Physical aggression in the past 12 months | Low life satisfaction*3 | Equivalent income less than €1500 per month | |
| Type of ACE |
n
(%) [95% CI] |
n
(%)OR, OR adj |
n
(%)OR, OR adj |
n
(%)OR, OR adj |
n
(%)OR, OR adj |
n (%)OR. OR adj |
| ACE 1: emotional abuse (n = 2521) | 311 (12.5) [11.2; 13.9] |
88 (28.5) 3.96; 1.84 |
83 (26.3) 4.28; 2.28 |
32 (10.1) 2.3; 2.33 |
117 (37.6) 3.38; 1.71 |
123 (38.9) 1.68; 0.76 |
| ACE 2: physical abuse (n = 2517) | 230 (9.1) [7.9; 10.3] |
65 (28.5) 3.74; 1.19 |
61 (26.5) 3.95; 1.14 |
28 (12.2) 7.11; 2.05 |
92 (40.7) 3.67; 1.28 |
105 (45.7) 2.25; 1.62 |
| ACE 3: sexual abuse (n = 2518) | 109 (4.3) [3.5; 5.1] |
34 (31.5) 3.94; 1.8 |
26 (23.9) 3.03; 1.31 |
9 (8.3) 3.35; 1.04 |
36 (34.0) 2.46; 1.19 |
50 (45.9) 2.16; 1.41 |
| ACE 4: emotional neglect (n = 2514) | 338 (13.4) [12.1; 14.8] |
92 (27.2) 3.83; 1.92 |
84 (24.9) 3.97; 2.01 |
22 (6.5) 2.97; 0.60 |
112 (33.9) 2.82; 1.36 |
135 (39.9) 1.78; 1.20 |
| ACE 5: physical neglect (n = 2515) | 109 (4.3) [3.5; 5.1] |
29 (26.6) 3.04; 0.76 |
26 (23.9) 3.03; 0.70 |
12 (11.1) 4.88; 1.11 |
45 (42.9) 3.70; 1.38 |
52 (47.7) 2.35; 1.38 |
| ACE 6: parental divorce/separation (n = 2520) |
488 (19.4) [17.7; 20.9] |
88 (18.1) 2.04; 1.21 |
82 (16.8) 2.21; 1.34 |
29 (6.0) 2.93; 1.50 |
163 (33.4) 1.61; 1.01 |
29 (6.0) 1.30; 1.00 |
| ACE 7: witnessed domestic violence (n = 2518) |
248 (9.8) [8.6; 11.1] |
48 (19.4) 2.05; 0.98 |
42 (16.9) 2.01; 0.97 |
23 (9.3) 4.63; 1.87 |
99 (39.9) 2.29; 1.26 |
23 (9.3) 1.74; 1.17 |
| ACE 8: alcohol and drug abuse in the household (n = 2526) |
421 (16.7) [15.1; 18.3] |
91 (21.7) 2.70; 1.32 |
69 (16.4) 2.04; 0.81 |
32 (7.6) 4.24; 1.76 |
178 (42.3) 2.24; 1.24 |
32 (7.6) 2.07; 1.63 |
| ACE 9: mental illness in the household (n = 2513) |
267 (10.6) [9.4; 11.9] |
75 (28.1) 3.80; 2.22 |
65 (24.3) 3.57; 2.26 |
19 (7.1) 3.17; 1.27 |
109 (40.8) 2.66; 1.61 |
19 (7.1) 1.83; 1.32 |
| ACE 10: incarcerated family member (n = 2519) |
88 (3.5) [2.8; 4.3] |
20 (22.7) 2.42; 0.82 |
22 (25.0) 3.21; 1.41 |
12 (13.6) 6.34; 1.43 |
39 (44.3) 2.85; 1.08 |
12 (13.6) 2.03; 1.00 |
%: Valid percentage; 95% CI: 95% confidence interval; OR: Odds ratio; ORadj: Odds ratio adjusted for all other ACEs
*1 Evidence of depression = PHQ-4 (Patient Health Questionnaire-4) cut-off point ≥3
*2 Evidence of anxiety = PHQ-4 cut-off point ≥3 (see eBox 2)
*3 Low life satisfaction = 1 standard deviation below mean
Odds ratios whose 95% confidence interval does not include 1 are shown in bold. Values for 95% confidence intervals are shown in eTable 1.
Table 3 provides an overview of the prevalence of combined adverse childhood experiences. More than half of participants (56.3%) reported no such experiences, which means that a total of 43.7% had at least one adverse childhood experience. A fifth of participants (20.7%) reported one adverse childhood experience, 8.6% reported 2, and 5.4% reported 3. The high-risk group of individuals reporting 4 or more adverse childhood experiences included 8.9% of participants. There was a cumulative effect with very high correlations in the high-risk group (=4 adverse childhood experiences) versus the group with no adverse childhood experiences for depression (OR = 7.8), anxiety (OR = 7.1), increased physical aggression (OR = 10.5), and low life satisfaction (OR = 5.1).
Table 3. Prevalences of combined adverse childhood experiences (ACEs), latent classes of co-occurring ACEs*1, and odds ratios for depression, anxiety, physical aggression, life satisfaction, and equivalent monthly income in a representative German sample (n = 2531).
| Total sample | Depression*1 | Anxiety*2 |
Physical aggression in the last 12 months |
Low life satisfaction*3 |
Equivalent income less than €1500 per month |
|
| n (%) |
n(%) OR |
n(%) OR |
n(%) OR |
n(%) OR |
n(%) OR |
|
| No. of ACEs (n = 2511) | ||||||
| 0 | 1426 (56.3) [54.4; 58.3] |
82 (5.7) 1 |
78 (5.5) 1 |
19 (1.3) 1 |
169 (12.2) 1 |
349 (24.5) 1 |
| 1 | 525 (20.7) [19.1; 22.2] |
56 (10.7) 1.95 |
48 (9.2) 1.73 |
12 (2.3) 1.73 |
83 (16.3) 1.40 |
150 (28.6) 1.23 |
| 2 | 218 (8.6) [7.5; 9.8] |
35 (16.1) 3.14 |
32 (14.7) 2.96 |
7 (3.2) 2.46 |
62 (29.0) 2.94 |
78 (35.8) 1.72 |
| 3 | 136 (5.4) [4.5; 6.2] |
40 (29.4) 6.95 |
29 (21.3) 4.66 |
6 (4.4) 3.41 |
38 (28.4) 2.85 |
47 (34.6) 1.63 |
| ≥ 4 | 226 (8.9) [7.9; 10.2] |
73 (32.3) 7.79 |
66 (29.2) 7.09 |
2 (12.4) 10.45 |
92 (41.6) 5.14 |
107 (47.3) 2.78 |
| Patterns of various adverse childhood experiences (n = 2529) | ||||||
| Group 1: no/minimal adverse childhood experiences | 1949 (77.1) | 143 (7.3) 1 |
130 (6.7) 1 |
30 (1.5) 1 |
253 (13.3) 1 |
499 (25.6) 1 |
| Group 2: problems in the parental home | 271 (10.7) | 62 (23.0) 3.76 |
46 (17.0) 2.85 |
10 (3.7) 2.46 |
74 (27.9) 2.52 |
105 (38.7) 1.84 |
| Group 3: child maltreatment | 188 (7.4) | 45 (24.2) 4.02 |
42 (22.3) 4.01 |
11 (5.9) 3.97 |
65 (35.1) 3.52 |
62 (33.0) 1.43 |
| Group 4: multiple adverse childhood experiences | 121 (4.8) | 36 (29.8) 5.34 |
35 (28.9) 5.68 |
21 (17.4) 13.42 |
52 (43.7)5.04 | 64 (52.9) 3.26 |
*1 See Figure 1
*2 Evidence of depression = PHQ-4 (Patient Health Questionnaire-4) cut-off point ≥3 (see eBox 2)
*3 Evidence of anxiety = PHQ-4 cut-off point ≥3; low life satisfaction = 1 standard deviation below mean
Odds ratios whose 95% confidence interval does not include 1 are shown in bold. Values for 95% confidence intervals are shown in eTable 2.
%: Valid percentage; OR: Odds ratio (versus no ACEs or group 1, no/minimal adverse childhood experiences)
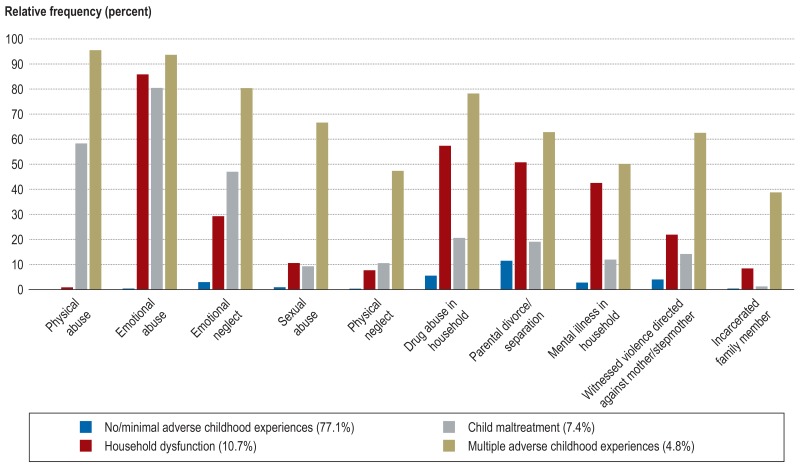
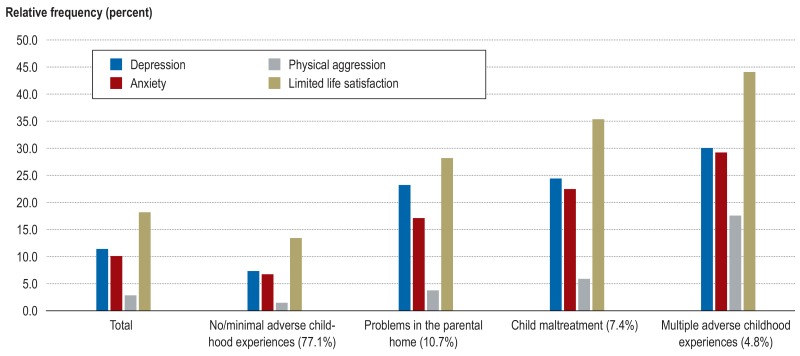
When indicators for adjustment of the model and interpretation of the findings are examined, a model with 4 prototypical patterns best describes the overall occurrence of adverse childhood experiences (etable 3). Figure 1 shows the 4 groups. The frequency of psychosocial issues in the sample as a whole and in the individual groups is shown in Figure 2. The probability of classification in the first group, “no/minimal adverse experiences,” was 0.96; for the second group, “problems in the parental home,” it was 0.78; for the third group, “child maltreatment,” it was 0.80; and for the fourth group, “multiple adverse childhood experiences,” it was 0.91. In group 4, “multiple adverse childhood experiences,” there were high odds ratios for current depression (OR = 5.3), anxiety (OR = 5.7), physical aggression (OR = 13.4), and low life satisfaction (OR = 5.0).
eTable 3. Fit indices for latent class analyses with 1, 2, 3, 4, 5, and 6 groups (n = 2529).
| Model | Log likelihood | AIC*1 | BIC*1 | SSaBIC*1 | Entropy*2 | BLRT*3 | groups: n (%) |
| 1 group | –8030.333 | 16 080.666 | 16 139.022 | 16 107.249 | – | – | 1: n = 2529 (100) |
| 2 groups | –6764.784 | 13 571.567 | 13 694.114 | 13 627.392 | 0.904 | –8030.333*4 | 1: n = 391 (15.5) 2: n = 2138 (84.5) |
| 3 groups | –6653.215 | 13 370.430 | 13 557.169 | 13 455.496 | 0.801 | –6764.784*4 | 1: n = 1959 (77.5) 2: n = 246 (9.7) 3: n = 324 (12.8) |
| 4 groups | –6566.711 | 13 219.421 | 13 470.351 | 13 333.729 | 0.840 | –6653.215*4 |
1: n = 1949 (77.1) 2: n = 271 (10.7) 3: n = 188 (7.4) 4: n = 121 (4.8) |
| 5 groups | –6548.141 | 13 204.282 | 13 519.404 | 13 347.831 | 0.843 | –6566.711*3 | 1: n = 110 (4.4) 2: n = 240 (9.5) 3: n = 157 (6.2) 4: n = 76 (3) 5: n = 1964 (76.9) |
| 6 groups | –6536.087 | 13 202.173 | 13 581.486 | 1374.964 | 0.851 | –6548.770 | 1: n = 24 (1) 2: n = 88 (3.5) 3: n = 214 (8.5) 4: n = 1946 (77.0) 5: n = 148 (5.9) 6: n = 109 (4.3) |
AIC: Akaike Information Criteria; BIC: Bayesian Information Criteria; BLRT: Bootstrap Likelihood Ratio Test
*1 Lower AIC, BIC, and sample-adjusted BIC (SSaBIC) indicate better fit of the model
*2 Entropy should be lower than 0,7; values close to 1 indicate better fit of the model
*3 p <0.05
*4 p <0.001 The model with the best fit is shown in bold.
Figure 1.
Prototypical patterns of co-occurring adverse childhood experiences, based on latent class analysis (LCA)
Figure 2.
Frequency of psychosocial issues in the total sample and individual groups. This shows that there are substantially more psychosocial issues in all groups— particularly the group with multiple adverse childhood experiences—than in the group with no/minimal adverse childhood experiences.
Discussion
This study investigated the frequency of adverse childhood experiences, combinations of these, and patterns of co-occurrence in the population, and correlations between these and psychosocial issues. Its findings underline the dose–effect relationship, as the risk for various outcomes rises with an increasing number of adverse childhood experiences. A total of 8.9% of study participants reported at least 4 adverse childhood experiences and are thus at high risk of developing psychosocial issues. The most common were parental divorce and separation, alcohol and drug abuse, and emotional neglect and abuse. These figures are within average range for international studies (2). When compared to studies on the frequency of child maltreatment in Germany (5, 6), the overall prevalence of adverse childhood experiences exceeds the reported prevalence of 31%. The frequencies identified here for physical abuse and emotional abuse are higher than those found in studies on abuse. For sexual abuse, prevalence is lower. For emotional and physical neglect, the frequencies are substantially lower than the prevalence figures reported in the 2 studies on the frequency of child maltreatment in Germany based on the Childhood Trauma Questionnaire (CTQ) (5, 6). Here it must be borne in mind that the CTQ answers allow for various levels of severity, and higher prevalence rates are identified depending on which severity levels are considered in the analysis. Differences between frequencies can also be attributed to different data collection methods. Overall, this study shows that adverse childhood experiences are approximately as common in the general German population as in other, international studies (2). It thus provides an initial frame of reference for Germany on the prevalence of adverse childhood experiences there.
Correlation with psychosocial issues
This study shows clearly that any form of adverse childhood experience is associated with psychosocial issues (table 2) and that ACEs often co-occur. As a result, some individual effects have no significant impact in the adjusted model but do continue to play a role in a cumulative dose–effect model. Because different adverse childhood experiences often co-occur, the effects of individual adverse childhood experiences are less pronounced if co-occurrence is controlled for. High adjusted odds ratios therefore also play a greater role in a cumulative risk model when other adverse childhood experiences co-occur. Odds ratios of less than one, however, have no protective effect in this regard. After controlling for co-occurrence, the largest effects remain for emotional abuse, emotional neglect, and mental illness in one parent or other another member of the household. These ACEs are particularly associated with psychosocial issues for those affected, so prevention and intervention measures in these fields are important. However, there are differential effects: for example, after controlling for combinations of adverse childhood experiences, there remains a correlation between sexual abuse and depression (OR = 1.8) and between emotional abuse and anxiety (OR = 2.3).
According to the literature (2), the risk of psychosocial issues increases with the accumulation of adverse childhood experiences (table 3). At the same time, it must be emphasized that individual events such as divorce are very common and can often be coped with successfully (16). Individual adverse childhood experiences thus differ in terms of their impact on psychosocial functioning. It must also be noted that there are potential genetic predispositions connected with adverse childhood experiences such as mental illness in the parental home and associated psychosocial issues such as depression.
The risk of symptoms of depression, anxiety, physical aggression, and limited life satisfaction have not yet been well researched (2). Compared to the findings of a recent meta-analysis (2), the findings described here on the correlation between 4 or more adverse experiences and depression, anxiety, and physical aggression are very strong, while the association between these and limited life satisfaction is moderate. This should be emphasized, because the wording of the question on physical aggression suggests there may be a tendency to give socially desirable answers. This study provides evidence that there is a significant correlation here that may be underestimated in these findings.
Prototypical patterns of adverse childhood experiences
Four prototypical patterns of co-occurring adverse childhood experiences were identified. The pattern characterized by experiences under the heading “problems in the parental home” represents the largest group of individuals who reported adverse childhood experiences. Psychosocial issues in those affected seem to be similarly negative and wide-ranging to those in patients who have experienced child maltreatment. It is therefore important to record adverse childhood experiences beyond child maltreatment when examining mental issues in a clinical context and when estimating costs in the framework of models for health economics. The strongest correlation was found for the group with multiple adverse childhood experiences. This group accounts for a substantial proportion of the general population, 4.8%.
Limitations of the study
Adverse childhood experiences were self-reported retrospectively and may therefore be subject to biases and suggestibility. The possibility of false negative answers when recording adverse childhood experiences has been discussed in the literature (17). In addition, the Adverse Childhood Experience Questionnaire contains questions concerning specific experiences, but the wording of the questions allows room for interpretation. This means subjective assessments are recorded, so in principle there is a risk of false positive answers too. In our view, however, this risk should be assessed as low, due to the existing evidence (17). In addition, individual adverse childhood experiences are recorded using only a few questions. Studies show that the prevalence of specific forms of abuse rises with the number of questions used (18). The prevalence of some adverse childhood experiences may therefore be underestimated. It should also be noted that the number of reported adverse childhood experiences varies in line with the number of family members. The approach selected for this study may also have systematically excluded potential high-risk populations. Because questionnaires were used, individuals with insufficient knowledge of German were systematically excluded, so people with German citizenship are substantially overrepresented and those from a background of migration are potentially underrepresented. However, care was taken to ensure that the sample was as representative as possible; differences between the sample and the general population are shown in eTable 4. This should be taken into account when interpreting the study findings.
eTable 4. Differences between the sample and the general German population, based on data from the German Federal Statistical Office (Statistisches Bundesamt).
| Sample (%) | General population (%) | |
| Sex | ||
| Female | 55.4 | 51.2 |
| Male | 44.6 | 48.8 |
| Marital status | ||
| Married | 44.7 | 43.4 |
| Single | 32.4 | 41.4 |
| Divorced | 13.5 | 7.5 |
| Widowed | 9.0 | 6.9 |
| German citizenship | 96.0 | 88.5 |
| Highest level of school education | ||
| School student | 2.6 | 3.6 |
| No school graduation | 2.2 | 4.0 |
| Volks- or Hauptschulabschluss (year 9 lower secondary school certificate | 28.8 | 30.4 |
| Mittlere Reife (year 10 lower secondary school certificate) | 33.3 | 23.1 |
| Graduated from PHS* | 7.9 | 6.6 |
| Entrance qualification for technical college/university | 21.3 | 31.9 |
| Religious affiliation | ||
| Protestant | 36.9 | 26.6 |
| Catholic | 29.6 | 28.6 |
*PHS: Polytechnical high school
Conclusion
In addition to child maltreatment, adverse childhood experiences under the heading “problems in the parental home” are common in the general German population (43.7% report at least one such experience). In particular, the high-risk group with 4 or more such experiences shows a high risk of various issues, health problems, and increased mortality (2); 8.9% of the German population fall into this category. The findings shown here highlight the correlation between adverse childhood experiences and psychosocial issues concerning life satisfaction, psychopathology, and interpersonal aggression.
There are numerous debates in German health care on subjects such as “child maltreatment” (19), “domestic violence” (20), “children of parents with addiction or mental illness” (21), etc. However, the cumulative effects of multiple adverse experiences have rarely been examined. The findings described here underline the clinical significance of emotional abuse and emotional neglect, which in Germany have to date been only marginally addressed in physicians’ debates on child protection. In view of the considerable negative consequences for those affected and the high prevalence of various adverse childhood experiences under the heading “problems in the parental home,” an increased focus on these factors in everyday clinical practice is important. Problematic characteristics in the parental home are often easier to access in clinical history than concrete evidence of abuse or neglect. Precisely because the mechanisms via which adverse childhood experiences affect health and wellbeing throughout one’s life are increasingly well researched, this knowledge must be taken into greater account in health care when designing selective, indicated prevention and intervention (including early intervention) measures (22).
Supplementary Material
eMethods
Target individuals were selected by selecting target households between November 2017 and February 2018, using a random-route procedure. This is a procedure for random sample selection. Using a given starting point, every third household is listed, and these are then contacted and asked to take part. Within the households, target individuals were selected at random using the Kish grid. This selects members of multiperson households to be surveyed at random. A total of 5160 households were found. There were 2531 evaluable datasets after removal of households that could not be included (household impossible to contact despite 4 visits [14.4%], household refused to participate [16.5%], target individual refused to participate [15.8%]). This study was part of a larger piece of research involving further questionnaires. First, sociodemographic information was recorded in interviews by trained interviewers. Most information was provided by the participants alone in self-completed questionnaires. Checks on the interviewers were performed in writing using postage-paid postcards. All answers received confirmed that interviewers worked appropriately.
Adjusted odds ratios
Because it was suspected that there would be strong correlations between individual adverse childhood experiences, a check for multicollinearity was performed before adjusted odds ratios were calculated using logistic regression. The check found that the highest correlations were between physical abuse and emotional abuse (r = 0.71) and between emotional abuse and emotional neglect (r = 0.50). All other correlations were weak. As no correlation coefficient above 0.8 was found, there is no risk of multicollinearity. Variance inflation factors (VIFs) are also well below the cut-off point of 5 (highest value: 2.24). Furthermore, the variable inclusion method was used for the model, i.e. all variables were included in the model simultaneously. All analyses were performed exploratively, so the p-level was not adjusted for multiple tests.
Statistical analyses of prototypical patterns of adverse childhood experiences
The model parameters for models with various numbers of patterns, up to 6, were calculated to identify the number of prototypical patterns. A person-centered approach was used for the latent class analysis. Five indicators were referred to in order to determine the final number of prototypical patterns: Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), sample size–adjusted Bayesian Information Criteria (SSaBIC), and entropy. The Bootstrap Likelihood Ratio Test (BLRT) (9) was also used to determine the number of prototypical patterns. The model’s classification probabilities were reported using best fit as an indicator of the reliability of the solution obtained. The classification probabilities are also given in the Results section.
Key Messages.
Of the total number of study participants, 8.9% reported 4 or more adverse childhood experiences. This is a particularly high-risk population.
The high-risk group with 4 or more adverse childhood experiences shows a significantly increased risk of depression (OR = 7.8), anxiety (OR = 7.1), physical aggression (OR = 10.5), and limited life satisfaction (OR = 5.1).
Future debates on child protection should take greater account of the cumulative effects of adverse childhood experiences.
Experiences under the heading “problems in the parental home” seem to be associated with similarly negative psychosocial issues to child maltreatment.
The findings presented here underline the clinical significance of emotional abuse and emotional neglect, which to date have been only marginally addressed in Germany, even in physicians’ debates on child protection.
eTable 1. Prevalences of individual adverse childhood experiences (ACEs) and 95% confidence intervals for odds ratios and relative odds ratios adjusted for co-occurrence of various adverse childhood experiences, for depression, anxiety, physical aggression, life satisfaction, and monthly income in a representative German sample (n = 2531).
| Total sample | Depression*1 | Anxiety*2 | Physical aggression in the past 12 months | Low life ‧satisfaction*3 | Equivalent ‧income less than €1500 per month | |
| Type of ACE |
n
(%) 95% CI |
OR 95% CI OR OR adj 95% CI OR adj |
OR 95% CI OR OR adj 95% CI OR adj OR adj 95% CI OR adj R adj 95-%-KI OR adj |
OR 95% CI OR OR adj 95% CI OR adj |
OR 95% CI OR OR adj 95% CI OR adj |
OR 95% CI OR OR adj 95% CI OR adj |
| ACE 1: emotional abuse (n = 2521) | 311 (12.5) [11.2; 13.9] |
3.96 [2.97; 5.28] 1.84 [1.16; 2.90] |
4.28 [3.18; 5.75] 2.28 [1.43; 3.65] |
2.3 [3.76; 9.85] 2.33 [1.01; 5.39] |
3.38 [2.61; 4.37] 1.71 [1.14; 2.57] |
1.68 [1.32; 2.15] 0.76 [0.51; 1.12] |
| ACE 2: physical abuse (n = 2517) | 230 (9.1) [7.9; 10.3] |
3.74 [2.72; 5.15] 1.19 [0.71; 1.99] |
3.95 [2.85; 5.48] 1.14 [0.67; 1.94] |
7.11 [4.30; 11.58] 2.05 [0.84; 4.98] |
3.67 [2.75; 4.90] 1.28 [0.81; 2.04] |
2.25 [1.71; 2.96] 1.62 [1.04; 2.51] |
| ACE 3: sexual abuse (n = 2518) | 109 (4.3) [3.5; 5.1] |
3.94 [2.57; 6.04] 1.8 [1.10; 2.93] |
3.03 [1.91; 4.81] 1.31 [0.77; 2.21] |
3.35 [1.62; 6.92] 1.04 [0.46; 2.35] |
2.46 [1.62; 3.73] 1.19 [0.74; 1.89] |
2.16 [1.47; 3.18] 1.41 [0.92; 2.15] |
| ACE 4: emotional neglect (n = 2514) | 338 (13.4) [12.1; 14.8] |
3.83 [2.90; 5.08] 1.92 [1.33; 2.78] |
3.97 [2.96; 5.32] 2.01 [1.37; 2.96] |
2.97 [1.77; 4.97] 0.60 [0.29; 1.25] |
2.82 [2.18; 3.64] 1.36 [0.97; 1.90] |
1.78 [1.41; 2.26] 1.20 [0.89; 1.63] |
| ACE 5: physical neglect (n = 2515) | 109 (4.3) [3.5; 5.1] |
3.04 [1.95; 4.73] 0.76 [0.43; 1.33] |
3.03 [1.91; 4.81] 0.70 [0.39; 1.27] |
4.88 [2.54; 9.38] 1.11 [0.47; 2.58] |
3.70 [2.48; 5.53] 1.38 [0.85; 2.25] |
2.35 [1.60; 3.46] 1.38 [0.87; 2.18] |
| ACE 6: parental divorce/separation (n = 2520) |
488 (19.4) [17.7; 20.9] |
2.04 [1.55; 2.68] 1.21 [0.89; 1.66] |
2.21 [1.66; 2.94] 1.34 [0.97; 1.86] |
2.93 [1.80; 4.74] 1.50 [0.86; 2.63] |
1.61 [1.26; 2.04] 1.01 [0.77; 1.33] |
1.30 [1.05; 1.61] 1.00 [0.80; 1.27] |
| ACE 7: witnessed domestic violence (n = 2518) |
248 (9.8) [8.6; 11.1] |
2.05 [1.46; 2.89] 0.98 [0.64; 1.48] |
2.01 [1.40; 2.88] 0.97 [0.62; 1.51] |
4.63 [2.77; 7.74] 1.87 [0.98; 3.52] |
2.29 [1.70; 3.07] 1.26 [0.89; 1.79] |
1.74 [1.33; 2.28] 1.17 [0.86; 1.60] |
| ACE 8: alcohol and drug abuse in the household (n = 2526) |
421 (16.7) [15.1; 18.3] |
2.70 [2.05; 3.56] 1.32 [0.94; 1.85] |
2.04 [1.51; 2.75] 0.81 [0.55; 1.19] |
4.24 [2.63; 6.84] 1.76 [0.96; 3.23] |
2.24 [1.76; 2.86] 1.24 [0.92; 1.67] |
2.07 [1.66; 2.57] 1.63 [1.26; 2.09] |
| ACE 9: mental illness in the household (n = 2513) |
267 (10.6) [9.4; 11.9] |
3.80 [2.81; 5.14] 2.22 [1.56; 3.14] |
3.57 [2.60; 4.91] 2.26 [1.56; 3.28] |
3.17 [1.85; 5.43] 1.27 [0.68; 2.40] |
2.66 [2.01; 3.53] 1.61 [1.17; 2.24] |
1.83 [1.41; 2.38] 1.32 [0.98; 1.77] |
| ACE 10: incarcerated family member (n = 2519) |
88 (3.5) [2.8; 4.3] |
2.42 [1.44; 4.05] 0.82 [0.45; 1.51] |
3.21 [1.95; 5.30] 1.41 [0.78; 2.55] |
6.34 [3.27; 12.28] 1.43 [0.63; 3.23] |
2.85 [1.82; 4.47] 1.08 [0.63; 1.83] |
2.03 [1.32; 3.11] 1.00 [0.61; 1.64] |
%: Valid percentage; 95% CI: 95 % confidence interval; OR: Odds ratio; ORadj: Odds ratio adjusted for other ACEs
*1 Evidence of depression = PHQ-4 (Patient Health Questionnaire-4) cut-off point =3
*2 Evidence of anxiety = PHQ-4 cut-off point =3
*3 Low life satisfaction = 1 standard deviation below mean
Odds ratios whose 95% confidence interval does not include 1 are shown in bold.
eTable 2. Prevalences of combined adverse childhood experiences (ACEs) and latent classes of co-occurring ACEs and 95% confidence intervals for odds ratios for depression, anxiety, physical aggression, life satisfaction, and equivalent monthly income in a representative German sample (n = 2531).
| Total sample | Depression*1 | Anxiety*2 | Physical aggression in the past 12 months | Low life satisfaction*3 |
Equivalent income less than €1500 per month |
|
|
OR 95% CI OR |
OR 95% CI OR |
OR 95% CI OR |
OR 95% CI OR |
OR 95% CI OR |
||
| No. of ACEs (n = 2511) | ||||||
| 0 | 1426 (56.3) [54.4; 58.3] |
1 | 1 | 1 | 1 | 1 |
| 1 | 525 (20.7) [19.1; 22.2] |
1.95 [1.37; 2.78] |
1.73 [1.19; 2.52] |
1.73 [0.84; 3.59] |
1.40 [1.05; 1.86] |
1.23 [0.99; 1.55] |
| 2 | 218 (8.6) [7.5; 9.8] |
3.14 [2.05; 4.80] |
2.96 [1.90; 4.49] |
2.46 [1.02; 5.93] |
2.94 [2.09; 4.11] |
1.72 [1.27; 2.33] |
| 3 | 136 (5.4) [4.5; 6.2] |
6.95 [4.51; 10.70] |
4.66 [2.91; 7.45] |
3.41 [1.34; 8.69] |
2.85 [1.89; 4.29] |
1.63 [1.12; 2.37] |
| ≥ 4 | 226 (8.9) [7.9; 10.2] |
7.79 [5.45; 11.13] |
7.09 [4.92; 10.23] |
10.45 [5.73; 19.07] |
5.14 [3.76; 7.02] |
2.78 [2.08; 3.70] |
| Patterns of various adverse childhood experiences (n = 2529) | ||||||
| Group 1: no/minimal adverse childhood experiences | 1949 (77.1) | 1 | 1 | 1 | 1 | 1 |
| Group 2: problems in the parental home | 271 (10.7) |
3.76 [2.70; 5.23] |
2.85 [1.98; 4.10] |
2.46 [1.19; 5.09] |
2.52 [1.87; 3.39] |
1.84 [1.41; 2.40] |
| Group 3: child maltreatment | 188 (7.4) |
4.02 [2.76; 5.86] |
4.01 [2.73; 5.91] |
3.97 [1.96; 8.06] |
3.52 [2.53; 4.89] |
1.43 [1.04; 1.97] |
| Group 4: multiple adverse childhood experiences | 121 (4.8) |
5.34 [3.49; 8.17] |
5.68 [3.69; 8.74] |
13.42 [7.42; 24.28] |
5.04 [3.43; 7.41] |
3.26 [2.25; 4.73] |
95% CI: 95 % confidence interval; OR: Odds ratio (versus no ACEs or group 1, no/minimal adverse childhood experiences)
*1 Evidence of depression = PHQ-4 (Patient Health Questionnaire-4) cut-off point ≥3
*2 Evidence of anxiety = PHQ-4 cut-off point ≥3
*3 Low life satisfaction = 1 standard deviation below mean
Odds ratios whose 95% confidence interval does not include 1 are shown in bold.
Acknowledgments
Translated from the original German by Caroline Shimakawa-Devitt, M.A.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 3.Felitti VJ, Fink PJ, Fishkin RE, Anda RF. Ergebnisse der Adverse Childhood Experiences (ACE)-Studie zu Kindheitstrauma und Gewalt. Trauma und Gewalt. 2007;1:18–32. [Google Scholar]
- 4.United Nations Economic and Social Council. Progress towards the Sustainable Development Goals. Report of the Secretary. 2017 [Google Scholar]
- 5.Witt A, Brown RC, Plener PL, Brähler E, Fegert JM. Child maltreatment in Germany: prevalence rates in the general population. Child Adolescent Psychiatry Mental Health. 2017;11 doi: 10.1186/s13034-017-0185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Häuser W, Schmutzer G, Brähler E, Glaesmer H. Maltreatment in childhood and adolescence—results from a survey of a representative sample of the German population. Dtsch Arztebl Int. 2011;108:287–294. doi: 10.3238/arztebl.2011.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clemens V, Huber-Lang M, Plener PL, Brähler E, Brown RC, Fegert JM. Association of child maltreatment subtypes and long-term physical health in a German representative sample. Eur J Psychotraumatol. 2018;9 doi: 10.1080/20008198.2018.1510278. 1510278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olofson MW. A new measurement of adverse childhood experiences drawn from the panel study of income dynamics child development supplement. Child Indicators Research. 2018;11:629–647. [Google Scholar]
- 9.Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte CarloSimulation Study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- 10.OECD. OECD Framework for statistics on the distribution of household ncome, consumption and wealth. www.oecd.org/statistics/framework-for-statistics-on-the-distribution-of-household-income-consumption-and-wealth-9789264194830-en.htm (last accessed on 1 August 2019) 2013 [Google Scholar]
- 11.Wingenfeld K, Schäfer I, Terfehr K, et al. The reliable, valid and economic assessment of early traumatization: first psychometric characteristics of the German version of the Adverse Childhood Experiences Questionnaire (ACE) Psychother Psychosom Med Psychol. 2011;61:e10–e14. doi: 10.1055/s-0030-1263161. [DOI] [PubMed] [Google Scholar]
- 12.Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–394. doi: 10.1016/j.amepre.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 14.Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 15.Muthén LK, Muthén BO. Mplus user‘s guide: statistical analysis with latent variables:user‘s guide. Muthén & Muthén; 2004 [Google Scholar]
- 16.Amato PR. The consequences of divorce for adults and children. J Marriage Fam Ther. 2000;62:1269–1287. [Google Scholar]
- 17.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 18.Stoltenborgh M, Van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ. A global perspective on child sexual abuse: meta-analysis of prevalence around the world. Child Maltreat. 2011;16:79–101. doi: 10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- 19.Berthold O, Frericks B, John T, Clemens V, Fegert JM, von Moers A. Abuse as a cause of childhood fractures. Dtsch Arztebl Int. 2018;115:769–775. doi: 10.3238/arztebl.2018.0769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epple F, Croy I, Schellong J. Häusliche Gewalt bei Patienten - durch medizinische Fachkräfte vermutlich unterschätzt: Eine Vollerhebung bei Dresdner und Chemnitzer niedergelassenen medizinischen Fachkräften und solchen des Dresdner Universitätsklinikums. ZEFQ. 2011;105:452–458. doi: 10.1016/j.zefq.2010.09.040. [DOI] [PubMed] [Google Scholar]
- 21.Mattejat F, Remschmidt H. The children of mentally ill parents. Dtsch Arztebl Int. 2008;105:413–418. doi: 10.3238/arztebl.2008.0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hudziak JJ. Developmental psychopathology and wellness: Genetic and environmental influences. American Psychiatric Pub. 2009:267–287. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Target individuals were selected by selecting target households between November 2017 and February 2018, using a random-route procedure. This is a procedure for random sample selection. Using a given starting point, every third household is listed, and these are then contacted and asked to take part. Within the households, target individuals were selected at random using the Kish grid. This selects members of multiperson households to be surveyed at random. A total of 5160 households were found. There were 2531 evaluable datasets after removal of households that could not be included (household impossible to contact despite 4 visits [14.4%], household refused to participate [16.5%], target individual refused to participate [15.8%]). This study was part of a larger piece of research involving further questionnaires. First, sociodemographic information was recorded in interviews by trained interviewers. Most information was provided by the participants alone in self-completed questionnaires. Checks on the interviewers were performed in writing using postage-paid postcards. All answers received confirmed that interviewers worked appropriately.
Adjusted odds ratios
Because it was suspected that there would be strong correlations between individual adverse childhood experiences, a check for multicollinearity was performed before adjusted odds ratios were calculated using logistic regression. The check found that the highest correlations were between physical abuse and emotional abuse (r = 0.71) and between emotional abuse and emotional neglect (r = 0.50). All other correlations were weak. As no correlation coefficient above 0.8 was found, there is no risk of multicollinearity. Variance inflation factors (VIFs) are also well below the cut-off point of 5 (highest value: 2.24). Furthermore, the variable inclusion method was used for the model, i.e. all variables were included in the model simultaneously. All analyses were performed exploratively, so the p-level was not adjusted for multiple tests.
Statistical analyses of prototypical patterns of adverse childhood experiences
The model parameters for models with various numbers of patterns, up to 6, were calculated to identify the number of prototypical patterns. A person-centered approach was used for the latent class analysis. Five indicators were referred to in order to determine the final number of prototypical patterns: Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), sample size–adjusted Bayesian Information Criteria (SSaBIC), and entropy. The Bootstrap Likelihood Ratio Test (BLRT) (9) was also used to determine the number of prototypical patterns. The model’s classification probabilities were reported using best fit as an indicator of the reliability of the solution obtained. The classification probabilities are also given in the Results section.