Abstract
Background
Epidural block approach and drugs are common options for improving the sensory and motor block duration and postoperative pain management.
Objectives
The study aimed to compare the analgesic effects of dexmedetomidine and morphine as adjuvants to bupivacaine for epidural anesthesia in leg fracture surgery.
Methods
This prospective clinical trial was conducted on patients (n = 80, age range: 18 - 60 years) categorized as ASA class I or II. After a clinical examination, the patients were allocated to receive either lumbar epidural bupivacaine + morphine (BM) (12 mL bupivacaine 0.5% + morphine 2 mg) or bupivacaine + dexmedetomidine (BD) (12 mL bupivacaine 0.5% + dexmedetomidine 1 µg/kg). After drug administration, the sensory block level was assessed at 2-min intervals using the Cold Swab method until it reached the T12 level. At the T12 level of sensory block, the surgery began when motor block reached grade 3 of the modified Bromage scale.
Results
The BD group had a significantly shorter time to reach the sensory and motor block than the BM group (P < 0.001). The duration of sensory and motor block was significantly longer in the group BD than in the BM group (P < 0.001). Moreover, the BD group showed lower VAS scores (P < 0.0001) and longer time to first analgesia demand than the BM group.
Conclusions
Combined bupivacaine + dexmedetomidine prolongs the sensory and motor block duration and controls postoperative pain more effectively, indicating that it is an appropriate combination for epidural anesthesia.
Keywords: Bupivacaine, Dexmedetomidine, Epidural Anesthesia, Morphine
1. Background
Anesthesiologists always try to develop new methods of improving the quality of postoperative pain management as their main goal. Lower limb surgery is performed under local, regional, or general anesthesia. Epidural anesthesia is a local anesthetic technique used in lower limb surgery (1-4). Modern orthopedic surgery aims at a faster onset of postoperative activity, mobility, and rehabilitation along with the least pain and discomfort. To achieve these objectives, different local anesthetics are used. Bupivacaine is a common agent in lower extremity surgery due to the long blockage, separation of the sensory block from the motor block, non-absolute absence of tachyphylaxis, and limited placental transmission in this type of surgery (5, 6).
Research shows that intrathecal bupivacaine had a short onset of sensory blockade (7). An increase in the dose of bupivacaine reduces the intensity of postoperative pain, reduces the opiate administration time to first analgesic demand, and decreases the incidence of nausea and vomiting (8). Intrathecal injection of alpha 2 agonists, such as dexmedetomidine, as adjuncts to topical anesthetics, can enhance the effects of anesthetic drugs and reduce their demand (5, 9-11). Dexmedetomidine as an adjunct directly increases the block time through the direct modulating of receptors on motor neurons and posterior horn sensory neurons of the spinal cord or their synapses (12, 13). The analgesic effects of epidural bupivacaine when administered alone last almost 4 - 6 h, but epidural morphine is effective for 12 - 24 h (14). The comparison of dexmedetomidine and fentanyl as intrathecal adjuvant drugs to bupivacaine showed that dexmedetomidine could prolong motor and sensory blockade and reduce the anesthetics consumption during the initial 24 h post-surgery (15). The addition of dexmedetomidine to ketorolac, compared to its addition to paracetamol, caused a further reduction in the postoperative pain score and resulted in a greater satisfaction rate (16). Combined bupivacaine-morphine also resulted in greater analgesic effects than morphine alone (17). Moreover, while the nerve impulse transmission is blocked by local anesthetics in the spinal cord dorsal horn μ-opioid receptors, opioids modulate pain (18).
Studies have shown that opioids could induce a lowersensory and motor maturity onset in T6 than lidocaine did, whereas they caused a higher sensory blockade level. The time to first analgesia demand was longer and the average consumption of meperidine was lower (19). Dexmedetomidine as an adjuvant to local anesthetics improves epidural efficacy without complications such as urinary detention that are usually accompanied by opioid drugs. Moreover, epidural dexmedetomidine is widely available (20).
2. Objectives
The present study aimed to comparatively investigate the analgesic effects of combined bupivacaine-morphine (BM) and bupivacaine-dexmedetomidine (BD) on the sensory and motor block onset, the sensory and motor block duration, postoperative pain control, time to first analgesic demand, and hemodynamic stability in patients undergoing leg fracture surgery under epidural anesthesia.
3. Methods
This was a prospective randomized clinical trial (IRCT20180602039954N1) conducted on patients (n = 80; age range = 18 to 60 years) with ASA class I or II hospitalized at Imam Khomeini Hospital, Ahvaz, Iran. We calculated a sample size of 32 patients in each group considering the type I error of 0.05 (confidence interval of 95%) and margin of error of 0.90 using Equation 1. To account for the possible dropout rate, we selected 40 patients for each group.
| Equation 1. |
The experimental procedure was approved by the Local Ethics Committee of Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (registration code: IR.AJUMS.REC.1396.938). Patients who were hospitalized for leg fracture surgery under epidural anesthesia were recruited for this study. The exclusion criteria included a history of any addiction, coagulation or neurological disorders, localized infection at the site of the epidural block, a need for analgesics during surgery, failed epidural blocks leading to general anesthesia, pregnancy, allergy to the study drugs, and con received anti-thrombotic medications. All patients were randomly allocated to either the BD group or the BM group (40 patients in each group).
Initially, we recorded the preoperative pulse rate (PR), non-invasive systolic blood pressure (SBP) and diastolic blood pressure (DBP), and saturation O2 (SatO2). Good IV access was secured in the operating room. The patients were preloaded with 10-mL ringer solution per kg body weight over 15 - 20 min. The epidural block was performed with a Tuohy needle (Episure, indigo ore, USA) at the L3 - L4 interspace. The site of epidural space was confirmed by the loss-of-resistance technique. After we injected a test dose with 3 mL of lidocaine 2% and epinephrine 1/200,000 in the BD group, the patients received 12 mL of bupivacaine 0.5% (AstraZeneca, UK) (21) + dexmedetomidine 1 μg/kg (Hospira, USA) (22). This dose was chosen based on previous studies reporting that the average dose of 1 - 2 mL of bupivacaine is needed for the epidural block of each segment.
In the BM group II, the patients received 12 mL of bupivacaine 0.5% plus 2 mg morphine (Darou Pakhsh, Iran) (21). Then, we started measuring the PR, SBP, DBP, and SatO2 and continuously monitored the readings. Immediately after the block, we recorded PR, SBP, DBP, and SatO2 at 5-min intervals for the initial 30 min, followed by 15-min intervals until the end of the sensory and motor block.
The hypotension was defined as SBP < 90 mmHg or SBP reduction of more than 20% of baseline. Hypotensive patients were treated with serum therapy using 5 mg ephedrine. If patients experienced bradycardia (HR < 55), 0.5 mg atropine was administered IV. Then, the sensory level was monitored every 2 min with the Cold Swab method until it reached the T12 level of sensory block, at which surgery began when motor block reached grade 3 of the modified Bromage scale. The sensory block duration was measured at 15-min intervals until it reached the L5 level. The motor block was recorded at 5-min intervals for the initial 30 min of the epidural block, followed by 30-min intervals until the modified Bromage scale reached zero. The onset time and duration of complete motor block, as well as the time of complete reversal, were recorded in the same time course. When sensory block reached the L5 level, postoperative pain was scored using a 10-point VAS (0 = no pain to 10 = worst pain imaginable) at 30-min intervals until the first demand of analgesic drug. When the VAS was greater than 4, if the patient requested analgesia, a postoperative 30-mg incremental dose of IV meperidine was administered and recorded.
The adverse effects and complications during and after surgery including itching, dry mouth, tremor, nausea, and vomiting were recorded. Itching and tremor were recorded as presence/absence. In the case of any complication, 1 mg ondansetron was administered IV. Dry mouth was also recorded as presence/absence. Nausea and vomiting were measured using the Verbal Rating Scale (VRS) scale and if it scored moderate to high, 1 mg ondansetron was administered IV.
The level of sensory block was monitored until it returned to the L5 level. The motor block was monitored until the modified Bromage scale returned to zero. The hemodynamic status was monitored until the end of the sensory and motor block. The VAS was recorded until the first analgesic demand and the complications were monitored for 12 h.
The collected data were analyzed with SPSS (version 20, SPSS Inc., Chicago, IL, USA) using independent sample t-test and the chi-square test. Statistical significance was set at 0.05 for all analyses.
4. Results
The patients’ demographic characteristics are presented in Table 1. There were no significant differences between the groups in age, weight, and height of the patients. The majority of the patients in both groups were male.
Table 1. Patients’ Demographic Characteristics and Baseline Values of the Block.
| Parameter | Group BD (I) | Group BM (II) | P Value |
|---|---|---|---|
| Mean age, y | 39.5 ± 2.0 | 34.3 ± 1.7 | 0.868 |
| BMI | 25.6 ± 0.6 | 24.8 ± 0.5 | 0.129 |
| Male (%) | 34 (85) | 27 (67.5) | 0.057 |
| Female (%) | 6 (15) | 13 (32.5) | 0.057 |
The postoperative scores of block showed statistically significant differences between the two groups (Table 2).
Table 2. Baseline Parameters of the Block in the Two Study Groupsa.
| Initial Characteristics of the Block | Group I (BD) | Group II (BM) | P Value |
|---|---|---|---|
| Time to the sensory level T12, min | 18.8 ± 0.6 | 27.7 ± 0.7 | P < 0.001b |
| Time to motor block onset, min | 24.5 ± 0.9 | 34.6 ± 0.7 | P < 0.001b |
| Time to the sensory level L5, min | 255.2 ± 6.2 | 219.4 ± 7.7 | P < 0.001b |
| Duration of complete motor block, min | 266.9 ± 5.9 | 237.8 ± 4.0 | P < 0.001b |
| Time to first analgesic demand, min | 470.4 ± 8.5 | 381.1 ± 5.1 | P < 0.001b |
aData are expressed as means ± SEM.
bP < 0.001 with independent sample t-test.
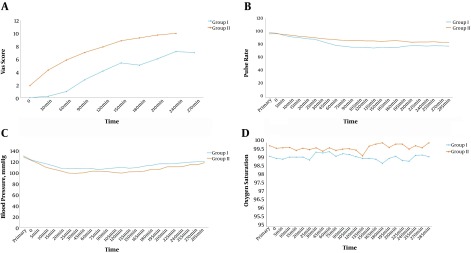
The VAS score was lower in the BD group than in the BM group, indicating the better performance of dexmedetomidine in postoperative pain control in the former group (Figure 1A). The PR was not significantly different between the two groups (Figure 1B). The BP (blood pressure) mean arterial pressure (MAP) was not significantly different between the two groups (Figure 1C). Moreover, the SatO2 was not significantly different between the two groups (Figure 1D).
Figure 1. The mean VAS score (A), PR (B), MAP (C), and SatO2 (D) in the two groups.
Although both adjuvants improved the postoperative analgesia parameters, dexmedetomidine was more effective than morphine. The BD combination showed a greater pain reduction than the BM combination in our population (Table 3).
Table 3. The Mean VAS Score, PR, BP, MAP, and SatO2 in the Two Study Groupsa.
| Groups | VAS Score | PR | MAP | SatO2 |
|---|---|---|---|---|
| BD | 2.7 ± 0.1 | 82.2 ± 1.8 | 112.0 ± 1.3 | 99.2 ± 0.1 |
| BM | 6.3 ± 0.01 | 88.2 ± 1.2 | 106.2 ± 0.6 | 99.2 ± 0.02 |
| P value | P < 0.0001b | 0.097 | 0.052 | 0.062 |
aData are expressed as means ± SEM.
bP < 0.001 with independent sample t-test
The frequency of complications in the two groups intraoperatively and postoperatively is presented in Table 4. The frequency of dry mouth was significantly different between the BD and BM groups (P = 0.031).
Table 4. Side Effects Seen in Both Groups Intraoperatively and Postoperativelya.
| Side Effect | BD Group (I) | BM Group (II) | P Value |
|---|---|---|---|
| None | 32 (80%) | 29 (72.5%) | 0.031b |
| Nausea | 3 (7.5%) | 4 (10%) | > 0.05 |
| Dry mouth | 5 (12.5%) | 0 (0%) | 0.031b |
| Tremor | 0 (0%) | 2 (5%) | > 0.05 |
| Itching | 0 (0%) | 4 (10%) | 0.031b |
| Vomiting | 0 (0%) | 1 (2.5%) | > 0.05 |
aData are expressed as means ± SEM.
bP < 0.05 with independent sample t-test
5. Discussion
In this study, dexmedetomidine was better than morphine as an adjuvant in local epidural anesthesia and resulted in shorter time to attain the sensory and motor block, longer sensory and motor block duration, more effective postoperative pain control (lower VAS scores), and longer time to first analgesic demand. The MAP, PR, and SatO2 were not significantly different between the two groups. In terms of side effects, dry mouth was observed only in the BD group while tremor, itching, and vomiting were observed in the BM group.
Bajwa et al. in a clinical trial compared the effects of dexmedetomidine and fentanyl as adjuvants in patients undergoing lower limb orthopedic surgery under epidural anesthesia (23). They reported that dexmedetomidine could better act in terms of hemodynamic stability, time to sensory block onset, sensory and motor block duration, the duration of postoperative analgesia effects, the need for postoperative local anesthetics, and sedation score (23). Our findings were consistent with the findings of Bajwa et al. study. Our findings also showed that dexmedetomidine resulted in a shorter time to reach sensory and motor block than morphine did. The sensory and motor block duration was longer in the BD group than in the BM group and the time to first analgesic demand was longer in the BD group than in the BM group. In conclusion, our study indicated that dexmedetomidine as an additive to bupivacaine in epidural anesthesia could result in longer sensory and motor block duration, more hemodynamic stability, and more effective postoperative analgesia; it induced longer anesthesia and lowered the need for additional perioperative and postoperative analgesics.
Rahimzadeh et al. compared the efficacy of dexmedetomidine and fentanyl as additives to intrathecal bupivacaine in lower limb orthopedic surgery. When they used dexmedetomidine rather than fentanyl as an adjuvant to bupivacaine for spinal anesthesia in lower limb surgery, they achieved longer sensory and motor block and longer postoperative analgesia (3). In another study, Imani et al. evaluated the effects of adding dexmedetomidine to paracetamol or ketorolac on post-cesarean pain and its associated complications. Their findings indicated that dexmedetomidine added to ketorolac, compared to its addition to paracetamol, induced further reduction in the postoperative pain score and resulted in higher rates of satisfaction (16).
In another study, Eskandar and Ebeid investigated the effects of epidural doses of dexmedetomidine plus bupivacaine on analgesia after knee joint replacement surgery 24. They concluded that epidural injection of bupivacaine plus dexmedetomidine is ideal for postoperative pain management in patients undergoing knee joint replacement surgery (24). Their findings showed that bupivacaine plus dexmedetomidine resulted in prolonged sensory and motor block and effective postoperative pain control. Therefore, they suggested dexmedetomidine plus bupivacaine as an appropriate combined drug.
The most commonly used technique in leg fracture surgery is epidural anesthesia, which provides both perioperative surgical anesthesia and postoperative analgesia. Early postoperative mobilization and rehabilitation along with minimal pain and discomfort are the main objectives of the modern orthopedic surgery (14, 25-27).
It should be noted that the present study had some limitations. Small sample size and lack of a placebo group were the main limitations of this study. Moreover, we used the VAS for the assessment of pain. This measure is vulnerable to between-individual variations since it largely depends on the threshold of pain and pain perception that may vary from person to person. Therefore, we suggest that randomized clinical trials be conducted with large sample sizes to measure pain and compare the efficacy of the two analgesics.
5.1. Conclusions
The findings of this study showed that bupivacaine-dexmedetomidine combination results in prolonged sensory and motor block and effective postoperative pain control. Thus, this combination could be appropriate for epidural anesthesia in leg fracture surgery.
Acknowledgments
The author would like to acknowledge the financial support from Ahvaz Jundishapur University of Medical Sciences (AJUMS) [IR.AJUMS.REC.1396.938] and Pain Research Center, AJUMS, Ahvaz, Iran.
Footnotes
Authors' Contribution: Mohammadreza Gousheh participated in original conceptualization, study design, implementation, data analysis, and manuscript writing. Reza Akhondzadeh participated in study design, implementation, and manuscript revision. Fatemeh Moftakhar took part in study design, implementation, data analysis, and manuscript writing. Alireza Olapour and Mahbobe Rashidi took part in study implementation and manuscript revision.
Clinical Trial Registration Code: The study was registered at clinicaltrials.gov (IRCT20180 602039954N1).
Conflicts of Interests: The authors declare no conflicts of interest.
Ethical Approval: This study was approved by the Local Research Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (AJUMS) (IR.AJUMS.REC.1396.938).
Financial Disclosure: The authors declare that they have no financial interests related to the materials in the manuscript or any part of it.
Funding/Support: Ahvaz Jundishapur University of Medical Sciences (AJUMS) [IR.AJUMS.REC.1396.938] and Pain Research Center, AJUMS, Ahvaz, Iran financially supported this study.
Patient Consent: Informed consent was obtained.
Contributor Information
Mohammadreza Gousheh, Email: rgousheh@gmail.com.
Reza Akhondzadeh, Email: rezaakh@hotmail.com.
Mahbobe Rashidi, Email: rashidimahbobe@yahoo.com.
Alireza Olapour, Email: alirezaolapour29@gmail.com.
Fatemeh Moftakhar, Email: dr.fmoftakhar@gmail.com.
References
- 1.Chatrath V, Attri JP, Bala A, Khetarpal R, Ahuja D, Kaur S. Epidural nalbuphine for postoperative analgesia in orthopedic surgery. Anesth Essays Res. 2015;9(3):326–30. doi: 10.4103/0259-1162.158004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verma D, Naithani U, Jain DC, Singh A. Postoperative analgesic efficacy of intrathecal tramadol versus nalbuphine added to bupivacaine in spinal anaesthesia for lower limb orthopaedic surgery. J Evol Med Dent Sci. 2013;2(33):6196–206. doi: 10.14260/jemds/1118. [DOI] [Google Scholar]
- 3.Rahimzadeh P, Faiz SHR, Imani F, Derakhshan P, Amniati S. Comparative addition of dexmedetomidine and fentanyl to intrathecal bupivacaine in orthopedic procedure in lower limbs. BMC Anesthesiol. 2018;18(1):62. doi: 10.1186/s12871-018-0531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akhondzade R, Nesioonpour S, Gousheh M, Soltani F, Davarimoghadam M. The effect of magnesium sulfate on postoperative pain in upper limb surgeries by supraclavicular block under ultrasound guidance. Anesth Pain Med. 2017;7(3):e14232. doi: 10.5812/aapm.14232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sathyanarayana LA, Heggeri VM, Simha PP, Narasimaiah S, Narasimaiah M, Subbarao BK. Comparison of epidural bupivacaine, levobupivacaine and dexmedetomidine in patients undergoing vascular surgery. J Clin Diagn Res. 2016;10(1):UC13–7. doi: 10.7860/JCDR/2016/17344.7079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarkar A, Bafila NS, Singh RB, Rasheed MA, Choubey S, Arora V. Comparison of epidural bupivacaine and dexmedetomidine with bupivacaine and fentanyl for postoperative pain relief in lower limb orthopedic surgery. Anesth Essays Res. 2018;12(2):572–80. doi: 10.4103/aer.AER_70_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Derakhshan P, Imani F, Koleini ZS, Barati A. Comparison of adding sufentanil and low-dose epinephrine to bupivacaine in spinal anesthesia: A randomized, double-blind, clinical trial. Anesth Pain Med. 2018;8(5):e69600. doi: 10.5812/aapm.69600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahimzadeh P, Imani F, Sayarifard A, Sayarifard S, Faiz SH. Ultrasound-guided fascia iliaca compartment block in orthopedic fractures: Bupivacaine 0.2% or 0.3%? Med J Islam Repub Iran. 2016;30:433. [PMC free article] [PubMed] [Google Scholar]
- 9.Pennefather SH, Quarterman CPJ, Klinger RY, Kanellakos GW. Pain management after thoracic surgery. In: Slinger P, editor. Principles and practice of anesthesia for thoracic surgery. Springer, Cham; 2019. pp. 981–1027. [DOI] [Google Scholar]
- 10.Akhondzadeh R, Rashidi M, Gousheh M, Olapour A, Baniahmad A. The effect of adding dexmedetomidine as an adjuvant to lidocaine in forearm fracture surgeries by supraclavicular block procedure under ultrasound-guided. Anesthesiol Pain Med. 2018;8(4) doi: 10.5812/aapm.74355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hetta DF, Fares KM, Abedalmohsen AM, Abdel-Wahab AH, Elfadl GMA, Ali WN. Epidural dexmedetomidine infusion for perioperative analgesia in patients undergoing abdominal cancer surgery: randomized trial. J Pain Res. 2018;11:2675–85. doi: 10.2147/JPR.S163975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tong Y, Ren H, Ding X, Jin S, Chen Z, Li Q. Analgesic effect and adverse events of dexmedetomidine as additive for pediatric caudal anesthesia: A meta-analysis. Paediatr Anaesth. 2014;24(12):1224–30. doi: 10.1111/pan.12519. [DOI] [PubMed] [Google Scholar]
- 13.Kathuria S, Gupta S, Dhawan I. Dexmedetomidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block. Saudi J Anaesth. 2015;9(2):148–54. doi: 10.4103/1658-354X.152841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz D, Hamburger J, Gutman D, Wang R, Lin HM, Marotta M, et al. The effect of adding subarachnoid epinephrine to hyperbaric bupivacaine and morphine for repeat cesarean delivery: A double-blind prospective randomized control trial. Anesth Analg. 2018;127(1):171–8. doi: 10.1213/ANE.0000000000002542. [DOI] [PubMed] [Google Scholar]
- 15.Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A comparative study of intrathecal dexmedetomidine and fentanyl as adjuvants to Bupivacaine. J Anaesthesiol Clin Pharmacol. 2011;27(3):339–43. doi: 10.4103/0970-9185.83678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imani F, Rahimzadeh P, Faiz HR, Nowruzina S, Shakeri A, Ghahremani M. Comparison of the post-caesarean analgesic effect of adding dexmedetomidine to paracetamol and ketorolac: A randomized clinical trial. Anesth Pain Med. 2018;8(5):e85311. doi: 10.5812/aapm.85311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mugabure Bujedo B. A clinical approach to neuraxial morphine for the treatment of postoperative pain. Pain Res Treat. 2012;2012:612145. doi: 10.1155/2012/612145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumamoto E, Mizuta K, Fujita T. Opioid actions in primary-afferent fibers—involvement in analgesia and anesthesia. Pharmaceuticals. 2011;4(2):343–65. doi: 10.3390/ph4020343. [DOI] [Google Scholar]
- 19.Imani F, Entezary SR, Alebouyeh MR, Parhizgar S. The maternal and neonatal effects of adding tramadol to 2% lidocaine in epidural anesthesia for cesarean section. Anesth Pain Med. 2011;1(1):25–9. doi: 10.5812/kowsar.22287523.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bajwa SJ, Bajwa SK, Kaur J, Singh G, Arora V, Gupta S, et al. Dexmedetomidine and clonidine in epidural anaesthesia: A comparative evaluation. Indian J Anaesth. 2011;55(2):116–21. doi: 10.4103/0019-5049.79883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Cohen NH, Young WL. Miller's anesthesia e-book. Elsevier Health Sciences; 2014. [Google Scholar]
- 22.Xiang Q, Huang DY, Zhao YL, Wang GH, Liu YX, Zhong L, et al. Caudal dexmedetomidine combined with bupivacaine inhibit the response to hernial sac traction in children undergoing inguinal hernia repair. Br J Anaesth. 2013;110(3):420–4. doi: 10.1093/bja/aes385. [DOI] [PubMed] [Google Scholar]
- 23.Bajwa SJ, Arora V, Kaur J, Singh A, Parmar SS. Comparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Saudi J Anaesth. 2011;5(4):365–70. doi: 10.4103/1658-354X.87264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eskandar AM, Ebeid AM. Effects of epidural dexmedetomidine and low-volume bupivacaine on postoperative analgesia after total knee replacement. Ain-Shams J Anaesthesiol. 2014;7(2):193. doi: 10.4103/1687-7934.133440. [DOI] [Google Scholar]
- 25.Cote CJ, Lerman J, Todres ID. A practice of anesthesia for infants and children E-book. Elsevier Health Sciences; 2012. [Google Scholar]
- 26.Shadangi BK, Garg R, Pandey R. A randomized, placebo-controlled, doubleblind study of the analgesic efficacy of extraperitoneal wound instillation of bupivacaine and morphine in abdominal surgeries. Anaesth Pain Intensive Care. 2019:169–73. [Google Scholar]
- 27.Narayan VA, Kaye AD, Vadivelu N. Perioperative pain management for general and plastic surgery. Oxford University Press; 2018. [Google Scholar]