Abstract
The tumor microenvironment (TME) is the primary arena where tumor cells and the host immune system interact. Bidirectional communication between tumor cells and the associated stromal cell types within the TME influences disease initiation and progression, as well as tumor immunity. Macrophages and natural killer (NK) cells are crucial components of the stromal compartment and display either pro- or anti-tumor properties, depending on the expression of key regulators. MicroRNAs (miRNAs) are emerging as such regulators. They affect several immune cell functions closely related to tumor evasion of the immune system. This review discusses the role of miRNAs in the differentiation, maturation, and activation of immune cells as well as tumor immunity, focusing particularly on macrophages and NK cells.
Keywords: miRNA, tumor immunity, macrophages, natural killer cells
1. Introduction
Bidirectional communication between cells and their microenvironment is crucial for normal tissue homeostasis as well as tumor growth [1]. The interactions between tumor cells and associated stromal cells represent an especially dynamic relationship that affects disease initiation and progression [2]. The tumor microenvironment (TME) is the primary site where tumor cells and the host immune cells interact. There are multiple stromal cell types within the TME. Among them, macrophages and natural killer (NK) cells are the most prevalent. They not only serve as the first barrier against pathogen infection, but also play vital roles in tumor progression.
Macrophages are cells involved in innate immunity, and they are a key player in linking innate and adaptive immunity. During pathogen infection or in the presence of a tumor cell-specific antigen, pattern-recognition receptors (PRRs) expressed in macrophages recognize components of the pathogen or the antigen and produce type I interferon (IFN I). This induces IFN-stimulated genes (ISGs), causes the expression of immune response mediators (cytokines and chemokines), and enhances antigen presentation against pathogen infection, tumor growth, or tumor invasion [3]. NK cells are also effectors of the innate immune system. They provide an early cellular defense against pathogens or tumor cells by synthesizing cytokines and chemokines, and causing cytotoxicity in tumor or infected cells to limit their spread and subsequent tissue damage. In addition, recent studies highlight that NK cells also regulate several types of immune cells, including macrophages; thus, NK cells also play a role in controlling inflammatory and autoimmune disorders [4]. However, once tumor cells or infected cells circumvent the first barrier of immune defense, a tumorigenic primary niche will form and develop further. Meanwhile, the TME converges to re-educate stromal cells to support pathogen infection and tumor progression (macrophages are the most prevalent) [1], which is partially mediated by microRNAs (miRNAs) and their downstream transcriptional factors [5].
MicroRNAs (miRNAs) are a large family of small (~23 nt) endogenous non-coding RNAs. They negatively regulate gene expression at the post-transcriptional level by binding to the 3′-untranslated region (UTR) of target mRNAs, which degrades the mRNAs or represses their translation [6]. Decades of studies have demonstrated that miRNAs participate in nearly every biological process, including immune cell development and maturation, as well as tumor immunity.
As differences in the TME among different cancer types are more fully understood [7], studies examining the relationship between the TME and stromal cells have increased in recent years. Herein, we summarize the functions of miRNAs in the development, maturation, activation, and tumor immunity with a specific focus on macrophages and NK cells.
2. The Role of miRNAs in Macrophages
Macrophages are essentially present in all tissues, and they are crucial effectors of wound healing, homeostasis, cancer, and immune responses [1,8]. Most macrophages derive from hematopoietic stem cells (HSCs). They sequentially differentiate into lymphoid-myeloid progenitors (LMP), granulocyte-macrophage progenitors (GMP), and then monocytes, which migrate to various tissues to become mature macrophages [1,9,10]. However, tissue-resident macrophages are derived from yolk-sac-derived erythro-myeloid progenitors [11,12]. Diversity and plasticity are the foremost characteristics of cells derived from a monocyte–macrophage lineage, especially for tumor-associated macrophages (TAMs) [13]. TAMs can rapidly alter their polarization states to accommodate different tissue microenvironment, which explains why macrophages have such disparate roles during normal homeostasis and tumorigenesis [1]. Classically activated (M1) macrophages display anti-tumorigenic activities by producing type I pro-inflammatory cytokines and participating in antigen presentation [14]. In contrast, alternatively activated (M2) macrophages secrete type II cytokines, which improve anti-inflammatory responses and display pro-tumorigenic activities [14]. M2 macrophages are further divided into four subtypes: M2a, M2b, M2c [15], and M2d (TAMs belong to this subtype) [16]. Decades of research show that several transcriptional factors control the activation of these various phenotypes, and the activities of these transcriptional factors are partially controlled by miRNAs.
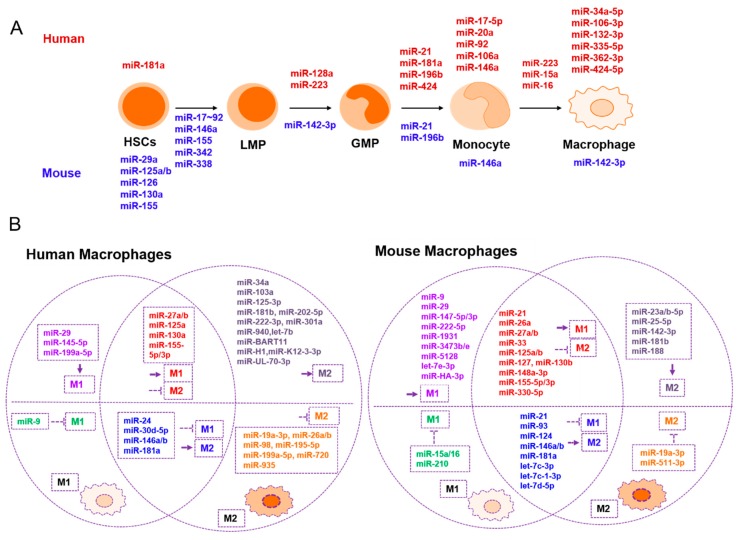
A specific set of miRNAs are implicated in hematopoietic stem cell (HSC) differentiation and maturation. Conditional ablation of Dicer in HSCs showed that mmu-miR-29a, mmu-miR-126, mmu-miR-130a, mmu-miR-155, and mmu-miR-125a/b control the differentiation of HSCs by targeting different genes [17]. For example, mmu-miR-125a significantly increased stem cell quantities by targeting BAK1 [18], and mmu-miR-126 targeted PI3K/AKT/GSK3β to exert the same function [19]. Transcription factor PU.1 is a key factor in lympho-myeloid development and stimulates the differentiation of HSCs into LMPs by inducing the expression of four miRNAs (mmu-miR-146a, mmu-miR-342, mmu-miR-338, and mmu-miR-155). By transiently occupying the binding sites within regulatory chromatin regions adjacent to their genomic coding loci, PU.1 induces HSCs to differentiate into macrophages. In addition, in vivo development assays conducted in mouse and zebrafish models show that miR-146a directs the selective differentiation of HSCs into functional macrophages [20]. Meanwhile, PU.1 suppresses the expression of the mmu-miR-17-92 cluster to force the premature differentiation of stem and progenitor cells into a myeloid lineage. They likely block the c-MYC-mediated proliferation of progenitor cells to ensure correct terminal differentiation [21]. The CCAAT/enhancer-binding protein alpha (C/EBPα) plays an essential role in differentiating LMPs into GMPs by directly binding to the promoter of hsa-miR-223 to increase its expression, which promotes granulocytic differentiation [22]. On the other hand, hsa-miR-424 promotes the differentiation of GMPs into monocytes in humans [23], while miR-21 and miR-196b play the same roles in both human and mouse models [24]. Recent research has shown that the knockdown of hsa-miR-128a induces Lin28a expression and reverts myeloid differentiation blockage in acute myeloid leukemia [25], but hsa-miR-181a reduces granulocytic and macrophage-like differentiation as well as hematopoietic stem/progenitor cell accumulation by targeting and down-regulating the expression of PRKCD, CTDSPL, and CAMKK1 [26]. Moreover, hsa-miRs-17-5p/20a/106a clusters suppress blast proliferation and inhibit monocyte differentiation and maturation by targeting AML1 [27]. Furthermore, next-generation SOLiD sequencing shows that hsa-miR-106-3p, hsa-miR-132-3p, hsa-miR-335-5p, hsa-miR-34a-5p, hsa-miR-362-3p, and hsa-miR-424-5p are up-regulated in macrophages when compared to monocytes [28], which implies that these miRNAs are involved in the maturation of macrophages.
miRNAs are also involved in macrophage polarization and activation. Recently, it was discovered that many genes and their related signaling pathways function in the transition of macrophage phenotypes. These transcription factors include cytokines, kinases, phosphatases, receptors, and miRNAs [13,29,30]. To investigate the role of miRNAs in macrophage phenotype switching, Lu et al. investigated the time-dependent miRNA–mRNA transcriptomic changes between the M1 and M2 transitions [31]. They found that mmu-miR-155-3p, mmu-miR-155-5p, mmu-miR-145-3p, and mmu-miR-9-5p are the four highest expressed miRNAs in M1 macrophages, and that mmu-miR-27a-5p, mmu-let-7c-1-3p, mmu-miR-23a-5p, and mmu-miR-23b-5p are the four highest expressed miRNAs in M2 macrophages derived from the bone marrow of mice. In addition, they found that mmu-miR-1931, mmu-miR-3473e, and mmu-miR-5128 function as early-response miRNAs. However, the role of miRNAs in human macrophage polarization at different times is still unclear. Other miRNAs involved in macrophage polarization and activation are shown in Table 1 and Figure 1.
Table 1.
A list of miRNAs involved in macrophage development, macrophage polarization, and tumor immunity.
| Development and Maturation | Promotes M1 | Suppresses M1 | Promotes M2 | Suppresses M2 | Related to Tumor Immunity |
|---|---|---|---|---|---|
| mmu-miR-29a [17](+) |
hsa-miR-155 [39,40] mmu-miR-155-3p/5p [31] |
mmu-miR-124 [41] |
hsa-miR-27a [40] mmu-miR-27a-5p [31] |
hsa-miR-130a [42] mmu-miR-130b [43] |
hsa-miR-3570 [37](–) |
| mmu-miR-126 [19](+) |
hsa-miR-125a/b-5p [40] mmu-miR-125a-3p [31,44] mmu- miR-125b [45] |
hsa-miR-181a [46] mmu-miR-181a [46] |
mmu-miR-23a/b-5p [31] |
hsa-miR-27b [47] mmu-miR-27a [48] |
hsa-miR-3614-5p [49](–) |
| mmu-miR-130a [17](+) |
hsa-miR-29b [40] mmu-miR-29b-1-5p [31] |
hsa-miR-9 [50] | mmu-miR-188 [31] | mmu-miR-21 [51] | hsa-miR-29 [52](+) |
| mmu-miR-155 [17,20](+) |
hsa-miR-145-5p [28] mmu-miR-145-5p [31] |
mmu-let-7c [53] mmu-let-7d-5p [54] |
mmu-let-7c-1-3p [31] mmu-let-7c [53] mmu-let-7d-5p [54] |
mmu-miR-23a [55] | mmu-let-7d-5p [54](–) |
| mmu-miR-125a/b [17,18](+) | mmu-miR-147-5p/3p [31] | mmu-miR-210 [56] | hsa-miR-26a [40] | hsa-miR-155 [57,58] |
mmu-miR-155 [33](+) |
|
mmu-miR-146a [20](+) hsa/mmu-miR-146a [59](+) |
mmu-miR-9-5p/3p [31] | mmu-miR-93 [60] |
hsa-miR-146a/b [40] mmu-miR-146b [61] |
hsa-miR-720 [62] | mmu-miR-223 [63](+) |
| mmu-miR-342 [20](+) | mmu-miR-21 [51] |
hsa-miR-146b [64] mmu-miR-146b [61] |
hsa-miR-222-3p [40] |
mmu-miR-125a-3p [31,44] mmu- miR-125b [45] |
hsa-miR-23a-3p [65](–) |
| mmu-miR-338 [20](+) | mmu-miR-33 [66] | mmu-miR-15a/16 [67] | mmu-miR-127 [68] |
mmu-miR-26a [69] hsa-miR-26a/b [70,71] |
hsa-miR-146a [59](+) |
|
mmu-miR-17-92 cluster [21] (–) hsa-miR-17-5p-20a-106a-92 [27](–) |
mmu-miR-330-5p [72] | hsa-miR-30d-5p [73] |
hsa-miR-181a [46] mmu-miR-181a [46] |
hsa-miR-19a-3p [74] mmu-miR-19a-3p [74] |
hsa-miR-17/20a/106a [75](+) |
| hsa-miR-223 [22](+) | mmu-let-7e-3p [31] | hsa-miR-24 [76] | hsa-miR-145-3p [77] | mmu-miR-33 [66] | mmu-miR-142-3p [32](+) |
| hsa-miR-424 [23](+) | mmu-miR-1931 [31] | mmu-miR-223 [78] | mmu-miR-223 [78] | mmu-miR-330-5p [72] | hsa-miR-34a [79](–) |
| hsa/mmu-miR-21 [24](+) | mmu-miR-3473e [31] | mmu-miR-21 [80,81] |
hsa-miR-181b [82] mmu-miR-181b [82] |
mmu-miR-127 [68] | hsa-miR-195-5p [83](+) |
| hsa/mmu-miR-196b [24](+) | mmu-miR-5128 [31] | hsa-miR-103a [84] | hsa-miR-935 [85] | hsa-miR-301a [86](–) | |
| hsa-miR-128a [25](–) | mmu-miR-222-5p [31] | hsa-miR-30d-5p [73] | mmu-miR-148a-3p [87] | hsa-miR-375 [88](+) | |
| mmu-miR-3473b [31] | mmu-miR-124 [89] | mmu-miR-511-3p [90] | miR-HA-3p [38](+) | ||
| mmu-miR-142-3p [32](–) | hsa-miR-199a-5p [91] | mmu-miR-142-3p [32] | mmu-miR-378-3p [92] | BART miRNA [34](–) | |
| mmu-miR-127 [68] | hsa-miR-940 [93] | hsa-miR-98 [94] | ebv-miR-BART11 [36](–) | ||
| hsa-miR-106-3p [28](+) | mmu-miR-148a-3p [87] | hsa-miR-24 [76] | hsa-miR-195-5p [83] | ||
| hsa-miR-132-3p [28](+) |
hsa-miR-130a [42] mmu-miR-130b [43] |
hsa-miR-202-5p [95] | hsa-miR-199a-5p [91] | ||
| hsa-miR-335-5p [28](+) |
hsa-miR-27b [47] mmu-miR-27a [48] |
hsa-let-7b [96] | |||
| hsa-miR-34a-5p [28](+) | mmu-miR-26a [69] | hsa-miR-34a [79] | |||
| hsa-miR-362-3p [28](+) | miR-HA-3p [38] | hsa-miR-301a [86] | |||
| hsa-miR-424-5p [28](+) | mmu-miR-21 [80,81] | ||||
| hsa-miR-223/15a/16 [97](–) | BART miRNAs [34] | ||||
| miR-H1 [34] | |||||
| miR-K12-3-3p [34] | |||||
| miR-UL-70-3p [34] | |||||
| ebv-miR-BART11 [36] |
Note: (+), promote the process; (–), suppress the process.
Figure 1.
miRNAs are involved in macrophage development, polarization, and tumor immunity. (A) miRNAs involved in mouse and human macrophage development and maturation. miRNAs listed without arrows participate in each step of cell differentiation or maturation, while miRNAs listed with arrows function in the developmental transition. (B) The role of miRNAs in classical M1 macrophage activation or M2 macrophage alternative activation in humans and mice. Different colors indicate the different roles that miRNAs play in macrophage polarization. HSCs, hematopoietic stem cells; LMP, common lymphoid progenitor; GMP, granulocyte-macrophage progenitor; M1, classically activated macrophages; M2, alternatively activated macrophages.
Tumor-derived miRNAs play crucial roles in macrophage functions and tumor immunity. For example, mmu-miR-142-3p is down-regulated in tumor filtered myeloid CD11b+ cells, promotes macrophage differentiation, and determines the acquisition of their immunosuppressive function in tumors [32]. In a mouse breast cancer model, mmu-miR-155 is up-regulated in CD11c+ pro-inflammatory TAMs and actively mediates tumor immunity, especially during the early stages of breast carcinogenesis [33].
Virus-encoded or virus infection-induced miRNAs also regulate macrophage activities in the tumor microenvironment. BamHI fragment A rightward transcript (BART) miRNA derived from Epstein Barr Virus (EBV)-infected Akata-lymphoblastoid cell lines converts macrophages into TAMs by partially regulating TNF-α, IL-10, and arginase 1 (ARG1) expression [34]. Virus-encoded miRNAs (e.g., miR-H1, miR-K12-3-3p, miR-UL-70-3p, and EBV-miR-BART11) that are incorporated into macrophages alter cellular gene expression (including miRNA expression) and convert M1 stage macrophages into M2 stage macrophages, which facilitates tumor development and metastasis [34,35,36].
Finally, many miRNAs also suppress tumor immunity by blocking the expression of key regulators involved in the activation of innate immunity pathways. For example, Xu et al. showed that rhabdovirus infection significantly induced miR-3750 expression in macrophages by targeting MAVS, which is an adaptor gene involved in RIG-I pathway activation [37]. However, some viral-encoded miRNAs contribute to tumor immunity. The H5N1 influenza virus-encoded miRNA miR-HA-3p promotes cytokine production in human macrophages by targeting poly(rC) binding protein 2 (PCBP2), which is a negative regulator of RIG-I-mediated antiviral innate immunity [38]. miRNAs involved in tumor immunity or immunity activation are summarized in Table 1.
3. The Role of miRNAs in NK Cells
Natural killer (NK) cells are cytotoxic innate lymphoid cells and are critical mediators of early host defense against pathogen infection, immune homeostasis, and tumor surveillance [98]. NK cells originate in bone marrow and complete their maturation in peripheral organs, which leads to their phenotypical and functional heterogeneity [99]. The amount and type of receptors on the surface of NK cells determine their functionality [100,101]. Based on the number of CD56 and CD16 surface markers, human NK cells are divided into two subsets: CD56bright/CD16–/dim and CD56dim/CD16bright. The latter is the main form of circulating NK cells [102]. CD56bright cells regulate the activation and function of NK cells, as well as other immune cells, by secreting cytokines such as IFN-γ and TNF-α. However, CD56dim cells release lytic molecules such as perforin and granzyme B, to exert highly cytotoxic effects. CD56dim cells are also crucial for antibody-mediated cytotoxicity [99].
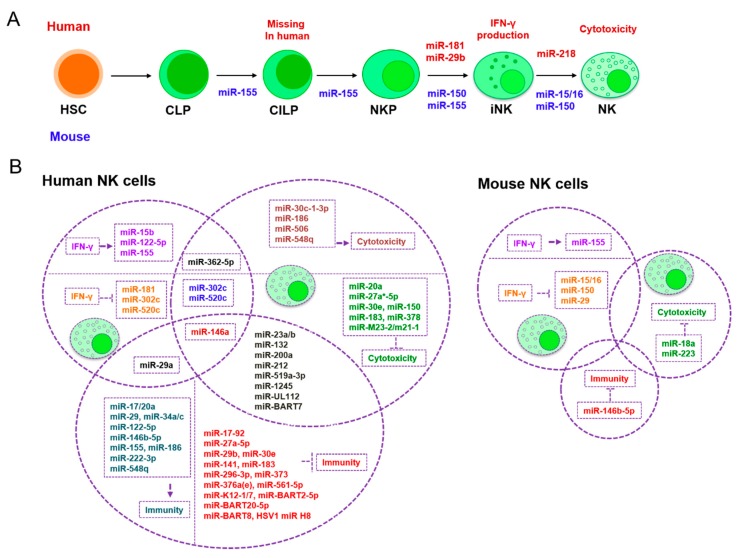
The development and maturation of human NK cells can be divided into two primary stages. In stage 1, NK cells are derived from bone marrow HSCs and progress through common lymphoid progenitors (CLPs), CD34 pro-NK, CD122 pre-NK, and committed immature NK cells (iNKs) stages, which finishes their NK lineage commitment. At this time, NK cells lose the capacity for T-cell or dendritic cells (DC) development [103]. In stage 2, iNK cells move to peripheral tissues such as the spleen or liver to complete their differentiation and maturation. In those peripheral tissues, iNKs convert into functional CD56bright or CD56dim NK cells [104]. In contrast, the development of mouse NK cells is different from human NK cells in several ways. CLPs firstly differentiate into common innate lymphoid progenitors (CILPs) with the help of transcriptional factor Nifil3. They then gradually develop into NK-cell precursors (NKPs), iNKs, and mouse mature NK cells (mNKs) [105]. Many transcriptional factors are necessary during the development and maturation of NK cells [105]. Accordingly, several studies have revealed that miRNAs are important in the regulation of fundamental NK cell processes such as activation, cytotoxicity, proliferation, development, and maturation by targeting the receptors or factors involved in transcriptional expression [106,107,108]. Through next-generation sequencing (NGS), many miRNAs have been discovered, and their roles in regulating NK cell development and maturation as well as disease progression have been verified.
A recent microarray study compared the expression of miRNA between mouse splenic NK cells (NK1.1+TCRβ−) and human peripheral blood NK cells (CD56+CD3–). Aimee et al. discovered the 14 conserved miRNAs with the highest expression levels in both groups: miR-150, miR-23b, miR-29a, miR-23a, miR-16, miR-21, let-7a, let-7f, miR-24, miR-15b, miR-720, let-7g, miR-103, and miR-26a [109]. This implies that these miRNAs should be crucial for NK cell functionality. Other previous studies have revealed that mmu-miR-150 and hsa-miR-181 promote the differentiation of pre-NKs into iNKs by targeting c-Myb or the Notch signaling inhibitor Nemo-like kinase (NLK), respectively [110,111]. Furthermore, mmu-miR-150 and mmu-miR-15/16 assist in the maturation of iNKs into mNKs by targeting the same gene, c-Myb [111,112]. During the activation of mature NKs, hsa-miR-155, mmu-miR-150, mmu-miRs-15/16, hsa-miR-181, and mmu-miR-29 suppress IFN-γ production in CD56bright NK cells. Mechanistically, mmu-miRs-15/16 and mmu-miR-29 directly target IFN-γ 3′UTR [113,114], and hsa-miR-181 indirectly represses upstream targets [110] to reduce IFN-γ translation. However, miR-155 regulates IFN-γ production in human and mouse NK cells by modulating the expression of the phosphatase SHIP-1, inhibiting T-bet/Tim-3, or by decreasing the activation of several signaling pathways such as those involving PI3K, NF-κB, and calcineurin [115,116,117]. hsa-miR-181 promotes IFN-γ production in primary CD56(+) NK cells [110]. miR-150 not only targets c-Myb to facilitate NK cell development and maturation [111], but it also represses PIK3AP1 and AKT2, which is a part of the PI3K-AKT pathway, and up-regulates Bim and p53 to assist in NK cell apoptosis [118]. In addition, miR-223, miR-27a-5p, miR-150, miR-378, and miR-30e suppress the cytotoxic capabilities of CD56dim NK cells. Mechanistically, mmu-miR-233 directly binds to the 3′UTR of granzyme B [119], and hsa-miR-150 targets the perforin 3′UTR [120]. hsa-miR-27a*-5p [121], hsa-miR-378, and hsa-miR-30e [122] repress the 3′UTR of granzyme B and perforin to repress the cytotoxic capacity of NK cells. miRNAs functioning in NK cell development, maturation, and activation are listed in Table 2 and Figure 2.
Table 2.
A list of miRNAs involved in NK cell development, NK cell activation, and tumor immunity.
| Development and Maturation | Classical Activation | NK Cell-Related Tumor Immunity Escape |
|
|---|---|---|---|
| IFN-γ Production | Cytotoxicity | ||
| mmu-miR-155 [127](+) | hsa-miR-155 [115,116,117](+) | hsa-miR-1245 [123](–) | hsa-miR-155 [117](–) |
| mmu-miR-150 [111](+) | hsa-miR-146a [125](-) | hsa-miR-183 [124](–) | hsa-miR-1245 [123](+) |
| hsa-miR-181 [110](+) | hsa-miR-122/15b [128](+) | hsa-miR-519a-3p [126](–) | hsa-miR-183 [124](+) |
| mmu-miR-15/16 [112](+) | mmu-miR-155 [127](+) | mmu-miR-223 [119](–) | hsa-miR-519a-3p [126](+) |
| hsa-miR-29b [129](–) | mmu-miR-15/16 [113](-) | hsa-miR-150 [120](–) | hsa/mmu-miR-146b-5p [130](–) |
| hsa-miR-218 [131](–) | mmu-miR-150 [111](–) | hsa-miR-27a*-5p [121](–) | hsa-miR-296-3p [132](+) |
| hsa-miR-181 [110](–) | hsa-miR-378 [122](–) | hsa-miR-146a [133](+) | |
|
mmu-miR-29 [114](–) hsa-miR-29a [134](–) |
hsa-miR-30e [122](–) | hsa-miR-376a(e) [135](+) | |
| hsa-miR-362-5p [136](+) | hsa-miR-20a [137](–) | hsa-miR-186 [138](–) | |
| hsa-miR-302c/520c [139](–) | hsa-miR-362-5p [136](+) | hsa-miR-122-5p [138](–) | |
| hsa-miR-122-5p [140](+) | hsa-miR-30c-1-3p [141](+) | hsa-miR-222-3p [138](–) | |
|
hsa-miR-132 [142](–) hsa-miR-212 [142](–) hsa-miR-200a [142](–) |
hsa-miR-146a [133](–) |
hsa-miR-29b [129](+) hsa-miR-29 [143](–) mmu-miR-29b [144](+) |
|
| hsa-miR-302c/520c [139](–) | hsa-miR-519a-3p [126](+) | ||
| hsa-miR-186 [138](+) | hsa-miR-141 [145](+) | ||
| hsa-miR-519a-3p [126](–) | hsa-miR-548q [146](–) | ||
| hsa-miR-23a [147](–) | hsa-miR-23a [147](+) | ||
| hsa-miR-10b [148](–) |
hsa-miR-17-92 [149](+) hsa-miR17/20a [150](–) |
||
| hsa-miR-506 [151](+) | hsa-miR-373 [152](+) | ||
| hsa-miR-548q [146](+) | hsa-miR-23b [148](+) | ||
| hsa-miR-152 [153](+) | hsa-miR-27a-5p [154](+) | ||
| mmu-miR-18a [155](–) | hsa-miR-561-5p [156](+) | ||
| hsa-miR-132/212/200a [142](–) | hsa-miR-132/212/200a [142](+) | ||
| ebv-miR-BART7 [157](–) | hsa-miR-34a/c [158](–) | ||
|
miR-M23-2 [159](–) miR-m21-1 [159](–) |
hsa-miR-30e [160](+) | ||
| miR-UL112 [161](–) | miR-J1-3p [162](–) | ||
| miR-J1-3p [162](+) | hcmv-miR-UL112 [163](+) | ||
| hcmv-miR-UL112 [163](–) |
miR-K12-7 [164](+) miR-BART2-5p [164](+) |
||
|
EBV-miR-BART20-5p [165](+) EBV-miR-BART8 [165](+) |
|||
| HSV1-miR-H8 [166](+) | |||
| ebv-miR-BART7 [157](+) | |||
| kshv-miR-K12-1 [167](+) | |||
Note: (+), promote the process; (–), suppress the process.
Figure 2.
miRNAs involved in NK cell development, NK cell activation, and tumor immunity. (A) miRNAs involved in mouse and human NK cell development and maturation. miRNAs listed with arrows regulate each developmental transition of NK cells. Note that human NK cell development, unlike mouse NK cell development, lacks a CILP stage. (B) miRNAs involved in IFN-γ production, NK cell cytotoxic capacity, and immune escape in human and mouse systems, respectively. CLP, common lymphoid progenitor; CILP, common innate lymphoid progenitor; NKP, NK-cell precursor; iNK, immature NK; NK, natural killer cell.
Pathogen- and tumor-induced miRNAs also regulate NK cell activities in the tumor microenvironment. For example, Cheng et al. found that Hepatitis C virus (HCV) infection down-regulates hsa-miR-155 in NK cells. The down-regulation of hsa-miR-155 releases T-bet/Tim-3, which suppresses IFN-γ production and leads to HCV evading immune clearance [117]. Importantly, TGF-β, a key mediator in the TME, post-transcriptionally increases mature hsa-miRNA-1245 expression. This miRNA suppresses NKG2D expression, which blocks NKG2D-mediated immune responses in NK cells and supports the TME [123]. TGF-β also induces hsa-miR-183 to abrogate the tumor cell-killing function of NK cells by targeting DNAX activating protein 12kDa (DAP12) [124]. In addition, hsa-miR-146a intervenes in NK cell IFN-γ synthesis by down-regulating RAK1 and TRAF6 expression [125]. hsa-miR-519a-3p impairs NK cell function by down-regulating the NKG2D ligands ULBP2 and MICA on the surface of tumor cells, and also affects granzyme B-induced apoptosis and caspase-7 activation in breast cancer [126]. More information about these miRNAs is summarized in Table 2 and Figure 2.
4. Conclusions and Further Perspectives
Extensive studies have contributed to the characterization of the TME and improved our understanding of cancer. Only now are we beginning to understand how the stromal cell-mediated immune response determines cancer initiation and progression. There are many factors involved in this process, including miRNAs. miRNAs not only regulate the development and maturation of immune cells, but they also control the activation of immune cells and their subsequent actions as pro- or anti-tumor factors (Figure 1 and Figure 2).
All known major miRNAs involved in macrophage development, polarization, and tumor immunity are summarized in Table 1 and Figure 1. By analyzing these data, we find that miRNAs such as miR-146a/b [59,61,64], miR-17-92 cluster [21,27], miR-181a/b [46,82], and miR-155 [31,40], whether they are derived from mouse or human models, usually have similar effects on macrophage development and polarization. Many miRNAs can regulate M1 and M2 states at the same time; for instance, miR-181a [46], miR-146b [61], and mmu-let-7c/d [53,54] simultaneously promote M2 activation and suppress M1 activation. miR-27a/b and miR-125a promote M1 activation while inhibiting M2 activation [31,40]. It is worth noting that the same miRNA may have conflicting functions in controlling macrophage transitions. For example, one report mentions that mmu-miR-21 increases M1 activation and inhibits M2 functioning [51]. However, according to other results, mmu-miR-21 restrains M1 activation and promotes M2 macrophage polarization [80,81]. These discrepancies might exist because miR-21 may exert different influences on macrophage polarization depending on the cell type, cancer type, and TME, since host tissues contain various types and quantities of stromal cells, which are determinants of tumor immunity [7]. Furthermore, the diversity and complexity of the TME may be the main reason why so many miRNAs are necessary and why a single, key miRNA that regulates macrophage functioning has not been found. Therefore, to further clarify the exact role of each miRNA in tumor immunity, more studies examining different cancers, organs, and tissues are necessary to estimate the multiple types of stromal cells functioning in each system.
Of note, Table 2 only lists a handful of miRNAs that contribute to NK cell development. This may be due, in part, to discrepancies in the microarray and small RNA-seq data that were used to uncover miRNAs involved in NK cell development or activation [108,109,119,122,168]. For example, miR-150 displays the greatest expression in the human microarray data [109], but it is not even among the top 15 [122] or top 25 miRNAs [108] being expressed, according to the NGS data. This might be due to the variability between the two methods, or the small RNA library construction approaches. Furthermore, the miR-150 profile is distinct between human and mouse NK cells when using NGS, which may be due to interspecies or experimental replications variation. Although the same method was used to obtain human NK cells (CD56+CD3–), miR-150 expression results were inconsistent between NGS and microarray studies, which is likely caused by variability between the two methods. Fehniger’s group proved that all miRNAs detected by SOLiD can be verified using qRT-PCR or a microarray [119]. However, approximately 25% of miRNAs detected by NGS cannot be verified by qRT-PCR or a microarray [119], implying that NGS may be uncovering many potential novel miRNA precursor genes. Therefore, more reasonable and more reliable detection methods are urgently needed to precisely interpret the role of miRNA in NK cell biology.
In this review, we described the roles of miRNAs in the development, maturation, activation, and tumor immunity of macrophages and NK cells (Table 1 and Table 2). We also mentioned the different activities displayed by human miRNAs and mouse miRNAs in all of the above processes. Our data show that certain miRNAs have different roles in various cell functions. For example, both human and mouse miR-146a inhibit IFN-γ production and the cytotoxicity of NK cells, and associate with tumor cells to escape immune surveillance. However, miR-146a promotes the development and maturation of human macrophages, and it promotes immune system activities. This phenomenon implies that the effectiveness of one miRNA treatment is limited, and this may be the reason why only a handful of miRNAs are successful at treating cancer, even though a large number of miRNAs participate in immune cell functions. Some miRNAs such as hsa-miR-181a, mmu-miR-150, and mmu-miR-155 influence multiple stages in various immune cells, making them good candidates for drug development. Considering that several miRNAs are potential therapeutic options for the treatment of different cancers, it is likely that a cocktail of miRNAs, instead of a single miRNA, may be more effective as a therapeutic option. Importantly, more studies are needed to discover miRNAs that may be involved in stromal cell development and maturation, and enhance the effect of immunotherapy by attracting more functional immune cells. Finally, more effective approaches such as cross-linking immunoprecipitation (CLIP) need to be developed or applied to accurately reveal miRNAs that influence stromal cells and tumor immunity in the tumor microenvironment.
Acknowledgments
We would like to thank Sinae Kim and Eunji Lee (Department of Biomedical Science, University of Ulsan School of Medicine, Asan Medical Center) for their helpful discussion.
Author Contributions
S.J.X. prepared and wrote the manuscript, drew figures, and made tables; H.T.H. revised the manuscript, figures, and tables; H.L.L. supervised, oversaw project administration, and acquired funding; S.C. supervised, acquired funding, oversaw project administration, and reviewed and edited the manuscript.
Funding
This research was funded by an internal grant of the University of Ulsan, College of Medicine (Physician Scientist Program), and supported by a grant from the Korean National Research Foundation (KNRF), grant number 2018024101.
Conflicts of Interest
The authors declare that they have no conflicts of interests.
References
- 1.Quail D.F., Joyce J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013;19:1423–1437. doi: 10.1038/nm.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joyce J.A., Pollard J.W. Microenvironmental regulation of metastasis. Nat. Rev. Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ivashkiv L.B., Donlin L.T. Regulation of type I interferon responses. Nat. Rev. Immunol. 2014;14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vivier E., Tomasello E., Baratin M., Walzer T., Ugolini S. Functions of natural killer cells. Nat. Immunol. 2008;9:503–510. doi: 10.1038/ni1582. [DOI] [PubMed] [Google Scholar]
- 5.Cao W., Cheng W., Wu W. MicroRNAs Reprogram Tumor Immune Response. MicroRNA Cancer. 2018;1699:67–74. doi: 10.1007/978-1-4939-7435-1_4. [DOI] [PubMed] [Google Scholar]
- 6.Bartel D.P. MicroRNA Target Recognition and Regulatory Functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salmon H., Remark R., Gnjatic S., Merad M. Host tissue determinants of tumour immunity. Nat. Rev. Cancer. 2019;19:215–227. doi: 10.1038/s41568-019-0125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ovchinnikov D.A. Macrophages in the embryo and beyond: Much more than just giant phagocytes. Genesis. 2008;46:447–462. doi: 10.1002/dvg.20417. [DOI] [PubMed] [Google Scholar]
- 9.Baltimore D., Boldin M.P., O’Connell R.M., Rao D.S., Taganov K.D. MicroRNAs: new regulators of immune cell development and function. Nat. Immunol. 2008;9:839–845. doi: 10.1038/ni.f.209. [DOI] [PubMed] [Google Scholar]
- 10.Terry R.L., Miller S.D. Molecular control of monocyte development. Cell. Immunol. 2014;291:16–21. doi: 10.1016/j.cellimm.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perdiguero E.G., Klapproth K., Schulz C., Busch K., Azzoni E., Crozet L., Garner H., Trouillet C., de Bruijn M.F., Geissmann F., et al. Tissue-resident macrophages originate from yolk-sac-derived erythro-myeloid progenitors. Nature. 2015;518:547–551. doi: 10.1038/nature13989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perdiguero E.G. Tissue-resident macrophages originate from yolk sac-derived erythro-myeloid progenitors. Immunology. 2014;143:26. doi: 10.1016/j.exphem.2015.06.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li H., Jiang T., Li M.-Q., Zheng X.-L., Zhao G.-J. Transcriptional Regulation of Macrophages Polarization by MicroRNAs. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.01175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biswas S.K., Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat. Immunol. 2010;11:889–896. doi: 10.1038/ni.1937. [DOI] [PubMed] [Google Scholar]
- 15.Mantovani A., Sica A., Sozzani S., Allavena P., Vecchi A., Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Chanmee T., Ontong P., Konno K., Itano N. Tumor-Associated Macrophages as Major Players in the Tumor Microenvironment. Cancers. 2014;6:1670–1690. doi: 10.3390/cancers6031670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Connell R.M., Chaudhuri A.A., Rao D.S., Gibson W.S.J., Balazs A.B., Baltimore D. MicroRNAs enriched in hematopoietic stem cells differentially regulate long-term hematopoietic output. Proc. Nat. Acad. Sci. USA. 2010;107:14235–14240. doi: 10.1073/pnas.1009798107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo S., Lu J., Schlanger R., Zhang H., Wang J.Y., Fox M.C., Purton L.E., Fleming H.H., Cobb B., Merkenschlager M., et al. MicroRNA miR-125a controls hematopoietic stem cell number. Proc. Nat. Acad. Sci. USA. 2010;107:14229–14234. doi: 10.1073/pnas.0913574107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lechman E.R., Gentner B., Van Galen P., Giustacchini A., Saini M., Boccalatte F.E., Hiramatsu H., Restuccia U., Bachi A., Voisin V., et al. Attenuation of miR-126 Activity Expands HSC In Vivo without Exhaustion. Cell Stem Cell. 2012;11:799–811. doi: 10.1016/j.stem.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghani S., Riemke P., Schönheit J., Lenze D., Stumm J., Hoogenkamp M., Lagendijk A., Heinz S., Bonifer C., Bakkers J., et al. Macrophage development from HSCs requires PU.1-coordinated microRNA expression. Blood. 2011;118:2275–2284. doi: 10.1182/blood-2011-02-335141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pospisil V., Vargova K., Kokavec J., Rybarova J., Savvulidi F., Jonasova A., Nečas E., Zavadil J., Laslo P., Stopka T. Epigenetic silencing of the oncogenic miR-17-92 cluster during PU.1-directed macrophage differentiation. EMBO J. 2011;30:4450–4464. doi: 10.1038/emboj.2011.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fazi F., Rosa A., Fatica A., Gelmetti V., De Marchis M.L., Nervi C., Bozzoni I. A minicircuitry comprised of MicroRNA-223 and transcription factors NFI-A and C/EBPα regulates human granulopoiesis. Cell. 2005;123:819–831. doi: 10.1016/j.cell.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 23.Rosa A., Ballarino M., Sorrentino A., Sthandier O., De Angelis F.G., Marchioni M., Masella B., Guarini A., Fatica A., Peschle C., et al. The interplay between the master transcription factor PU.1 and miR-424 regulates human monocyte/macrophage differentiation. Proc. Nat. Acad. Sci. USA. 2007;104:19849–19854. doi: 10.1073/pnas.0706963104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velu C.S., Baktula A.M., Grimes H.L. Gfi1 regulates miR-21 and miR-196b to control myelopoiesis. Blood. 2009;113:4720–4728. doi: 10.1182/blood-2008-11-190215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Luca L., Trino S., Laurenzana I., Tagliaferri D., Falco G., Grieco V., Bianchino G., Nozza F., Campia V., D’Alessio F., et al. Knockdown of miR-128a induces Lin28a expression and reverts myeloid differentiation blockage in acute myeloid leukemia. Cell Death Dis. 2017;8 doi: 10.1038/cddis.2017.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su R., Lin H.S., Zhang X.H., Yin X.L., Ning H.M., Liu B., Zhai P.F., Gong J.N., Shen C., Song L., et al. MiR-181 family: regulators of myeloid differentiation and acute myeloid leukemia as well as potential therapeutic targets. Oncogene. 2015;34:3226–3239. doi: 10.1038/onc.2014.274. [DOI] [PubMed] [Google Scholar]
- 27.Fontana L., Pelosi E., Greco P., Racanicchi S., Testa U., Liuzzi F., Croce C.M., Brunetti E., Grignani F., Peschle C. MicroRNAs 17-5p-20a-106a control monocytopoiesis through AML1 targeting and M-CSF receptor upregulation. Nat. Cell Biol. 2007;9:775–787. doi: 10.1038/ncb1613. [DOI] [PubMed] [Google Scholar]
- 28.Jiménez V.C., Bradley E.J., Willemsen A.M., Van Kampen A.H.C., Baas F., Kootstra N.A. Next-generation sequencing of microRNAs uncovers expression signatures in polarized macrophages. Physiol. Genom. 2014;46:91–103. doi: 10.1152/physiolgenomics.00140.2013. [DOI] [PubMed] [Google Scholar]
- 29.Murray P.J. Macrophage Polarization. Annu. Review Physiol. 2017;79:541–566. doi: 10.1146/annurev-physiol-022516-034339. [DOI] [PubMed] [Google Scholar]
- 30.Curtale G. MiRNAs at the Crossroads between Innate Immunity and Cancer: Focus on Macrophages. Cells. 2018;7:12. doi: 10.3390/cells7020012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu L., McCurdy S., Huang S., Zhu X., Peplowska K., Tiirikainen M., Boisvert W.A., Garmire L.X. Time Series miRNA-mRNA integrated analysis reveals critical miRNAs and targets in macrophage polarization. Sci. Rep. 2016;6 doi: 10.1038/srep37446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sonda N., Simonato F., Peranzoni E., Cali B., Bortoluzzi S., Bisognin A., Wang E., Marincola F.M., Naldini L., Gentner B., et al. miR-142-3p prevents macrophage differentiation during cancer-induced myelopoiesis. Immunity. 2013;38:1236–1249. doi: 10.1016/j.immuni.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Zonari E., Pucci F., Saini M., Mazzieri R., Politi L.S., Gentner B., Naldini L. A role for miR-155 in enabling tumor-infiltrating innate immune cells to mount effective antitumor responses in mice. Blood. 2013;122:243–252. doi: 10.1182/blood-2012-08-449306. [DOI] [PubMed] [Google Scholar]
- 34.Higuchi H., Yamakawa N., Imadome K.-I., Yahata T., Kotaki R., Ogata J., Kakizaki M., Fujita K., Lu J., Yokoyama K., et al. Role of exosomes as a proinflammatory mediator in the development of EBV-associated lymphoma. Blood. 2018;131:2552–2567. doi: 10.1182/blood-2017-07-794529. [DOI] [PubMed] [Google Scholar]
- 35.Naqvi A.R., Shango J., Seal A., Shukla D., Nares S. Viral miRNAs alter host cell miRNA profiles and modulate innate immune responses. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Song Y., Li X., Zeng Z., Li Q., Gong Z., Liao Q., Li X., Chen P., Xiang B., Zhang W., et al. Epstein-Barr virus encoded miR-BART11 promotes inflammation-induced carcinogenesis by targeting FOXP1. Oncotarget. 2016;7:36783–36799. doi: 10.18632/oncotarget.9170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu T., Chu Q., Cui J., Bi D. Inducible microRNA-3570 feedback inhibits the RIG-I-dependent innate immune response to rhabdovirus in teleost fish by targeting MAVS/IPS-1. J. Virol. 2018;92 doi: 10.1128/JVI.01594-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X., Fu Z., Liang H., Wang Y., Qi X., Ding M., Sun X., Zhou Z., Huang Y., Gu H., et al. H5N1 influenza virus-specific miRNA-like small RNA increases cytokine production and mouse mortality via targeting poly(rC)-binding protein 2. Cell Res. 2018;28:157–171. doi: 10.1038/cr.2018.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.He M., Xu Z., Ding T., Kuang D.-M., Zheng L. MicroRNA-155 Regulates Inflammatory Cytokine Production in Tumor-associated Macrophages via Targeting C/EBPβ. Cell. Mol. Immunol. 2009;6:343–352. doi: 10.1038/cmi.2009.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Graff J.W., Dickson A.M., Clay G., McCaffrey A.P., Wilson M.E. Identifying Functional MicroRNAs in Macrophages with Polarized Phenotypes. J. Boil. Chem. 2012;287:21816–21825. doi: 10.1074/jbc.M111.327031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yu A., Zhang T., Duan H., Pan Y., Zhang X., Yang G., Wang J., Deng Y., Yang Z. MiR-124 contributes to M2 polarization of microglia and confers brain inflammatory protection via the C/EBP-alpha pathway in intracerebral hemorrhage. Immunol. Lett. 2017;182:1–11. doi: 10.1016/j.imlet.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 42.Lin L., Lin H., Wang L., Wang B., Hao X., Shi Y. miR-130a regulates macrophage polarization and is associated with non-small cell lung cancer. Oncol. Rep. 2015;34:3088–3096. doi: 10.3892/or.2015.4301. [DOI] [PubMed] [Google Scholar]
- 43.Zhang M., Zhou Z., Wang J., Li S. MiR-130b promotes obesity associated adipose tissue inflammation and insulin resistance in diabetes mice through alleviating M2 macrophage polarization via repression of PPAR-γ. Immunol. Lett. 2016;180:1–8. doi: 10.1016/j.imlet.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 44.Zhao J.-L., Huang F., He F., Gao C.-C., Liang S.-Q., Ma P.-F., Dong G.-Y., Han H., Qin H.-Y. Forced Activation of Notch in Macrophages Represses Tumor Growth by Upregulating miR-125a and Disabling Tumor-Associated Macrophages. Cancer Res. 2016;76:1403–1415. doi: 10.1158/0008-5472.CAN-15-2019. [DOI] [PubMed] [Google Scholar]
- 45.Chaudhuri A.A., So A.Y.-L., Sinha N., Gibson W.S.J., Taganov K.D., O’Connell R.M., Baltimore D. MiR-125b potentiates macrophage activation1. J. Immunol. 2011;187:5062–5068. doi: 10.4049/jimmunol.1102001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bi J., Zeng X., Zhao L., Wei Q., Yu L., Wang X., Yu Z., Cao Y., Shan F., Wei M. miR-181a Induces Macrophage Polarized to M2 Phenotype and Promotes M2 Macrophage-mediated Tumor Cell Metastasis by Targeting KLF6 and C/EBPalpha. Mol. Ther. Nucleic Acids. 2016;5 doi: 10.1038/mtna.2016.71. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 47.Jennewein C., Von Knethen A., Schmid T., Brüne B. MicroRNA-27b Contributes to Lipopolysaccharide-mediated Peroxisome Proliferator-activated Receptor γ (PPARγ) mRNA Destabilization. J. Boil. Chem. 2010;285:11846–11853. doi: 10.1074/jbc.M109.066399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yao F., Yu Y., Feng L., Li J., Zhang M., Lan X., Yan X., Liu Y., Guan F., Zhang M., et al. Adipogenic miR-27a in adipose tissue upregulates macrophage activation via inhibiting PPARγ of insulin resistance induced by high-fat diet-associated obesity. Exp. Cell Res. 2017;355:105–112. doi: 10.1016/j.yexcr.2017.03.060. [DOI] [PubMed] [Google Scholar]
- 49.Diosa-Toro M., Echavarría-Consuegra L., Flipse J., Fernandez G.J., Kluiver J., Berg A.V.D., Urcuqui-Inchima S., Smit J.M. MicroRNA profiling of human primary macrophages exposed to dengue virus identifies miRNA-3614-5p as antiviral and regulator of ADAR1 expression. PLoS Negl. Trop. Dis. 2017;11 doi: 10.1371/journal.pntd.0005981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thulin P., Wei T., Werngren O., Cheung L., Fisher R.M., Grander D., Corcoran M., Ehrenborg E. MicroRNA-9 regulates the expression of peroxisome proliferator-activated receptor δ in human monocytes during the inflammatory response. Int. J. Mol. Med. 2013;31:1003–1010. doi: 10.3892/ijmm.2013.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Z., Brandt S., Medeiros A., Wang S., Wu H., Dent A., Serezani C.H. MicroRNA 21 Is a Homeostatic Regulator of Macrophage Polarization and Prevents Prostaglandin E2-Mediated M2 Generation. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0115855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou Y., Wang X., Sun L., Zhou L., Ma T.-C., Song L., Wu J.-G., Li J.-L., Ho W.-Z. Toll-like receptor 3-activated macrophages confer anti-HCV activity to hepatocytes through exosomes. FASEB J. 2016;30:4132–4140. doi: 10.1096/fj.201600696R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Banerjee S., Xie N., Cui H., Tan Z., Yang S., Icyuz M., Abraham E., Liu G. microRNA let-7c regulates macrophage polarization. J. Immunol. 2013;190:6542–6549. doi: 10.4049/jimmunol.1202496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baer C., Squadrito M.L., Laoui D., Thompson D., Hansen S.K., Kiialainen A., Hoves S., Ries C.H., Ooi C.H., De Palma M. Suppression of microRNA activity amplifies IFN-gamma-induced macrophage activation and promotes anti-tumour immunity. Nat. Cell Biol. 2016;18:790–802. doi: 10.1038/ncb3371. [DOI] [PubMed] [Google Scholar]
- 55.Ma S.S., Liu M., Xu Z.B., Li Y.S., Guo H., Ge Y.H., Liu Y.X., Zheng D.X., Shi J. A double feedback loop mediated by microRNA-23a/27a/24-2 regulates M1 versus M2 macrophage polarization and thus regulates cancer progression. Oncotarget. 2016;7:13502–13519. doi: 10.18632/oncotarget.6284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qi J., Qiao Y., Wang P., Li S., Zhao W., Gao C. microRNA-210 negatively regulates LPS-induced production of proinflammatory cytokines by targeting NF-κB1 in murine macrophages. FEBS Lett. 2012;586:1201–1207. doi: 10.1016/j.febslet.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 57.Martinez-Nunez R.T., Louafi F., Sanchez-Elsner T. The Interleukin 13 (IL-13) Pathway in Human Macrophages Is Modulated by MicroRNA-155 via Direct Targeting of Interleukin 13 Receptor alpha 1 (IL13R alpha 1) J. Biol. Chem. 2011;286:1786–1794. doi: 10.1074/jbc.M110.169367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang Y.Y., Zhang M.Y., Li X.Q., Tang Z.S., Wang X.M., Zhong M., Suo Q.F., Zhang Y., Lv K. Silencing MicroRNA-155 Attenuates Cardiac Injury and Dysfunction in Viral Myocarditis via Promotion of M2 Phenotype Polarization of Macrophages. Sci. Rep. 2016;6 doi: 10.1038/srep22613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Etzrodt M., Cortez-Retamozo V., Newton A., Zhao J., Ng A., Wildgruber M., Romero P., Wurdinger T., Xavier R., Geissmann F., et al. Regulation of monocyte functional heterogeneity by miR-146a and Relb. Cell Rep. 2012;1:317–324. doi: 10.1016/j.celrep.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ganta V.C., Choi M.H., Kutateladze A., Fox T.E., Farber C.R., Annex B.H. A MicroRNA93-Interferon Regulatory Factor-9-Immunoresponsive Gene-1-Itaconic Acid Pathway Modulates M2-Like Macrophage Polarization to Revascularize Ischemic Muscle. Circulation. 2017;135:2403–2425. doi: 10.1161/CIRCULATIONAHA.116.025490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peng L., Zhang H., Hao Y., Xu F., Yang J., Zhang R., Lu G., Zheng Z., Cui M., Qi C.-F., et al. Reprogramming macrophage orientation by microRNA 146b targeting transcription factor IRF5. EBioMedicine. 2016;14:83–96. doi: 10.1016/j.ebiom.2016.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhong Y., Yi C. MicroRNA-720 suppresses M2 macrophage polarization by targeting GATA3. Biosci. Rep. 2016;36 doi: 10.1042/BSR20160105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen L., Song Y., He L., Wan X., Lai L., Dai F., Liu Y., Wang Q. MicroRNA-223 Promotes Type I Interferon Production in Antiviral Innate Immunity by Targeting Forkhead Box Protein O3 (FOXO3) J. Boil. Chem. 2016;291:14706–14716. doi: 10.1074/jbc.M115.700252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen L., Dai Y.-M., Ji C.-B., Yang L., Shi C.-M., Xu G.-F., Pang L.-X., Huang F.-Y., Zhang C.-M., Guo X.-R. MiR-146b is a regulator of human visceral preadipocyte proliferation and differentiation and its expression is altered in human obesity. Mol. Cell. Endocrinol. 2014;393:65–74. doi: 10.1016/j.mce.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 65.Liu J., Fan L., Yu H., Zhang J., He Y., Feng D., Wang F., Li X., Liu Q., Li Y., et al. Endoplasmic Reticulum Stress Causes Liver Cancer Cells to Release Exosomal miR-23a-3p and Up-regulate Programmed Death Ligand 1 Expression in Macrophages. Hepatology. 2019;70:241–258. doi: 10.1002/hep.30607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ouimet M., Ediriweera H.N., Gundra U.M., Sheedy F.J., Ramkhelawon B., Hutchison S.B., Rinehold K., Van Solingen C., Fullerton M.D., Cecchini K., et al. MicroRNA-33–dependent regulation of macrophage metabolism directs immune cell polarization in atherosclerosis. J. Clin. Investig. 2015;125:4334–4348. doi: 10.1172/JCI81676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jia X.Q., Hu X.Y., Han S., Miao X., Liu H., Li X.M., Lin Z.J., Wang Z.B., Gong W.J. Increased M1 macrophages in young miR-15a/16(−/−) mice with tumour grafts or dextran sulphate sodium-induced colitis. Scand. J. Immunol. 2018;88 doi: 10.1111/sji.12703. [DOI] [PubMed] [Google Scholar]
- 68.Ying H., Kang Y., Zhang H., Zhao D., Xia J., Lu Z., Wang H., Xu F., Shi L. MiR-127 modulates macrophage polarization and promotes lung inflammation and injury by activating the JNK pathway. J. Immunol. 2015;194:1239–1251. doi: 10.4049/jimmunol.1402088. [DOI] [PubMed] [Google Scholar]
- 69.Sahu S.K., Kumar M., Chakraborty S., Banerjee S.K., Kumar R., Gupta P., Jana K., Gupta U.D., Ghosh Z., Kundu M., et al. MicroRNA 26a (miR-26a)/KLF4 and CREB-C/EBP beta regulate innate immune signaling, the polarization of macrophages and the trafficking of Mycobacterium tuberculosis to lysosomes during infection. PLoS Pathog. 2017;13 doi: 10.1371/journal.ppat.1006410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pello O.M., De Pizzol M., Mirolo M., Soucek L., Zammataro L., Amabile A., Doni A., Nebuloni M., Swigart L.B., Evan G.I., et al. Role of c-MYC in alternative activation of human macrophages and tumor-associated macrophage biology. Blood. 2012;119:411–421. doi: 10.1182/blood-2011-02-339911. [DOI] [PubMed] [Google Scholar]
- 71.Li J., Liang Y., Lv H., Meng H., Xiong G., Guan X., Chen X., Bai Y., Wang K. miR-26a and miR-26b inhibit esophageal squamous cancer cell proliferation through suppression of c-MYC pathway. Gene. 2017;625:1–9. doi: 10.1016/j.gene.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 72.Sun J., Huang Q., Li S., Meng F., Li X., Gong X. miR-330-5p/Tim-3 axis regulates macrophage M2 polarization and insulin resistance in diabetes mice. Mol. Immunol. 2018;95:107–113. doi: 10.1016/j.molimm.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 73.Jiang M., Wang H., Jin M., Yang X., Ji H., Jiang Y., Zhang H., Wu F., Wu G., Lai X., et al. Exosomes from MiR-30d-5p-ADSCs Reverse Acute Ischemic Stroke-Induced, Autophagy-Mediated Brain Injury by Promoting M2 Microglial/Macrophage Polarization. Cell. Physiol. Biochem. 2018;47:864–878. doi: 10.1159/000490078. [DOI] [PubMed] [Google Scholar]
- 74.Yang J., Zhang Z., Chen C., Liu Y., Si Q., Chuang T.H., Li N., Gomez-Cabrero A., Reisfeld R.A., Xiang R., et al. MicroRNA-19a-3p inhibits breast cancer progression and metastasis by inducing macrophage polarization through downregulated expression of Fra-1 proto-oncogene. Oncogene. 2014;33:3014–3023. doi: 10.1038/onc.2013.258. [DOI] [PubMed] [Google Scholar]
- 75.Zhu D., Pan C., Li L., Bian Z., Lv Z., Shi L., Zhang J., Li D., Gu H., Zhang C.-Y., et al. MicroRNA-17/20a/106a modulate macrophage inflammatory responses through targeting signal-regulatory protein α. J. Allergy Clin. Immunol. 2013;132:426–436. doi: 10.1016/j.jaci.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang J.J., Zhang N., Wu W., Guo Q.H., Wang W.J., Wang P., Wang X.P. MicroRNA-24 Modulates Staphylococcus aureus-Induced Macrophage Polarization by Suppressing CHI3L1. Inflammation. 2017;40:995–1005. doi: 10.1007/s10753-017-0543-3. [DOI] [PubMed] [Google Scholar]
- 77.Huang Y., Du K.L., Guo P.Y., Zhao R.M., Wang B., Zhao X.L., Zhang C.Q. IL-16 regulates macrophage polarization as a target gene of mir-145-3p. Mol. Immunol. 2019;107:1–9. doi: 10.1016/j.molimm.2018.12.027. [DOI] [PubMed] [Google Scholar]
- 78.Zhuang G.Q., Meng C., Guo X., Cheruku P.S., Shi L., Xu H., Li H.G., Wang G., Evans A.R., Safe S., et al. A Novel Regulator of Macrophage Activation miR-223 in Obesity-Associated Adipose Tissue Inflammation. Circulation. 2012;125:2892–2903. doi: 10.1161/CIRCULATIONAHA.111.087817. [DOI] [PubMed] [Google Scholar]
- 79.Weng Y.S., Tseng H.Y., Chen Y.A., Shen P.C., Al Haq A.T., Chen L.M., Tung Y.C., Hsu H.L. MCT-1/miR-34a/IL-6/IL-6R signaling axis promotes EMT progression, cancer stemness and M2 macrophage polarization in triple-negative breast cancer. Mol. Cancer. 2019;18 doi: 10.1186/s12943-019-0988-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lu T.X., Munitz A., Rothenberg M.E. MicroRNA-21 is up-regulated in allergic airway inflammation and regulates IL-12p35 expression1. J. Immunol. 2009;182:4994–5002. doi: 10.4049/jimmunol.0803560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Caescu C.I., Guo X., Tesfa L., Bhagat T.D., Verma A., Zheng D., Stanley E.R. Colony stimulating factor-1 receptor signaling networks inhibit mouse macrophage inflammatory responses by induction of microRNA-21. Blood. 2015;125:e1–e13. doi: 10.1182/blood-2014-10-608000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.An T.H., He Q.W., Xia Y.P., Chen S.C., Baral S., Mao L., Jin H.J., Li Y.N., Wang M.D., Chen J.G., et al. MiR-181b Antagonizes Atherosclerotic Plaque Vulnerability Through Modulating Macrophage Polarization by Directly Targeting Notch1. Mol. Neurobiol. 2017;54:6329–6341. doi: 10.1007/s12035-016-0163-1. [DOI] [PubMed] [Google Scholar]
- 83.Lin X.B., Wang S.Y., Sun M., Zhang C.X., Wei C., Yang C.G., Dou R.Z., Liu Q., Xiong B. miR-195-5p/NOTCH2-mediated EMT modulates IL-4 secretion in colorectal cancer to affect M2-like TAM polarization. J. Hematol. Oncol. 2019;12 doi: 10.1186/s13045-019-0708-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 84.Hsu Y.L., Hung F.Y., Chang W.A., Jian S.F., Lin Y.S., Pan Y.C., Wu C.Y., Kuo P.L. Hypoxic Lung-Cancer-Derived Extracellular Vesicle MicroRNA-103a Increases the Oncogenic Effects of Macrophages by Targeting PTEN. Mol. Ther. 2018;26:568–581. doi: 10.1016/j.ymthe.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang B.K., Du Y., He Y.Q., Liu Y.W., Zhang G.L., Yang C.X., Gao F. INT-HA induces M2-like macrophage differentiation of human monocytes via TLR4-miR-935 pathway. Cancer Immunol. Immunother. 2019;68:189–200. doi: 10.1007/s00262-018-2261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang X., Luo G., Zhang K., Cao J., Huang C., Jiang T., Liu B., Su L., Qiu Z. Hypoxic Tumor-Derived Exosomal miR-301a Mediates M2 Macrophage Polarization via PTEN/PI3Kγ to Promote Pancreatic Cancer Metastasis. Cancer Res. 2018;78:4586–4598. doi: 10.1158/0008-5472.CAN-17-3841. [DOI] [PubMed] [Google Scholar]
- 87.Huang F., Zhao J.L., Wang L., Gao C.C., Liang S.Q., An D.J., Bai J., Chen Y., Han H., Qin H.Y. miR-148a-3p Mediates notch signaling to Promote the Differentiation and M1 activation of Macrophages. Front. Immunol. 2017;8 doi: 10.3389/fimmu.2017.01327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Frank A.-C., Ebersberger S., Fink A.F., Lampe S., Weigert A., Schmid T., Ebersberger I., Syed S.N., Brüne B. Apoptotic tumor cell-derived microRNA-375 uses CD36 to alter the tumor-associated macrophage phenotype. Nat. Commun. 2019;10 doi: 10.1038/s41467-019-08989-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Taj S.H., Kho W., Riou A., Wiedermann D., Hoehn M. MiRNA-124 induces neuroprotection and functional improvement after focal cerebral ischemia. Biomaterials. 2016;91:151–165. doi: 10.1016/j.biomaterials.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 90.Squadrito M.L., Pucci F., Magri L., Moi D., Gilfillan G.D., Ranghetti A., Casazza A., Mazzone M., Lyle R., Naldini L., et al. miR-511-3p Modulates Genetic Programs of Tumor-Associated Macrophages. Cell Rep. 2012;1:141–154. doi: 10.1016/j.celrep.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 91.Jia Y., Zheng Z., Xue M., Zhang S., Hu F., Li Y., Yang Y., Zou M., Li S., Wang L., et al. Extracellular Vesicles from Albumin-Induced Tubular Epithelial Cells Promote the M1 Macrophage Phenotype by Targeting Klotho. Mol. Ther. 2019;27 doi: 10.1016/j.ymthe.2019.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ruckerl D., Jenkins S.J., Laqtom N.N., Gallagher I.J., Sutherland T.E., Duncan S., Buck A.H., Allen J.E. Induction of IL-4Rα–dependent microRNAs identifies PI3K/Akt signaling as essential for IL-4–driven murine macrophage proliferation in vivo. Blood. 2012;120:2307–2316. doi: 10.1182/blood-2012-02-408252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ying X., Zhu Q., Chen X., Wang X., Wu X. Exosomes derived from hypoxic epithelial ovarian cancer deliver microRNA-940 to induce macrophage M2 polarization. Oncol. Rep. 2017;38:522–528. doi: 10.3892/or.2017.5697. [DOI] [PubMed] [Google Scholar]
- 94.Li L., Sun P.F., Zhang C.S., Li Z.C., Zhou W.Y. MiR-98 suppresses the effects of tumor-associated macrophages on promoting migration and invasion of hepatocellular carcinoma cells by regulating IL-10. Biochimie. 2018;150:23–30. doi: 10.1016/j.biochi.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 95.Wang L., Liu X.Y., Song X.C., Dong L., Liu D.W. MiR-202-5p Promotes M2 Polarization in Allergic Rhinitis by Targeting MATN2. Int. Arch. Allergy Immunol. 2019;178:119–127. doi: 10.1159/000493803. [DOI] [PubMed] [Google Scholar]
- 96.Wang Z.G., Xu L., Hu Y.Y., Huang Y.Q., Zhang Y.J., Zheng X.F., Wang S.S., Wang Y.F., Yu Y.R., Zhang M., et al. miRNA let-7b modulates macrophage polarization and enhances tumor-associated macrophages to promote angiogenesis and mobility in prostate cancer. Sci. Rep. 2016;6 doi: 10.1038/srep25602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Li T., Morgan M.J., Choksi S., Zhang Y., Kim Y.S., Liu Z.G. MicroRNAs modulate the noncanonical transcription factor NF-kappaB pathway by regulating expression of the kinase IKKalpha during macrophage differentiation. Nat. Immunol. 2010;11:799–805. doi: 10.1038/ni.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vivier E., Raulet D.H., Moretta A., Caligiuri M.A., Zitvogel L., Lanier L.L., Yokoyama W.M., Ugolini S. Innate or adaptive immunity? The example of natural killer cells. Science. 2011;331:44–49. doi: 10.1126/science.1198687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pesce S., Squillario M., Greppi M., Loiacono F., Moretta L., Moretta A., Sivori S., Castagnola P., Barla A., Candiani S., et al. New miRNA signature heralds human NK cell subsets at different maturation steps: Involvement of miR-146a-5p in the regulation of KIR expression. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.02360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Moretta A., Bottino C., Vitale M., Pende D., Cantoni C., Mingari M.C., Biassoni R., Moretta L. Activating receptors and coreceptors involved in human natural killer cell-mediated cytolysis. Annu. Rev. Immunol. 2001;19:197–223. doi: 10.1146/annurev.immunol.19.1.197. [DOI] [PubMed] [Google Scholar]
- 101.Moretta A., Bottino C., Vitale M., Pende D., Biassoni R., Mingari M.C., Moretta L. Receptors for HLA class-I molecules in human natural killer cells. Annu. Rev. Immunol. 1996;14:619–648. doi: 10.1146/annurev.immunol.14.1.619. [DOI] [PubMed] [Google Scholar]
- 102.Cooper M.A., Fehniger T.A., Caligiuri M.A. The biology of human natural killer-cell subsets. Trends Immunol. 2001;22:633–640. doi: 10.1016/S1471-4906(01)02060-9. [DOI] [PubMed] [Google Scholar]
- 103.Freud A.G., Caligiuri M.A. Human natural killer cell development. Immunol. Rev. 2006;214:56–72. doi: 10.1111/j.1600-065X.2006.00451.x. [DOI] [PubMed] [Google Scholar]
- 104.Sun J.C., Lanier L.L. NK cell development, homeostasis and function: parallels with CD8(+) T cells. Nat. Rev. Immunol. 2011;11:645–657. doi: 10.1038/nri3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Leong J.W., Wagner J.A., Ireland A.R., Fehniger T.A. Transcriptional and post-transcriptional regulation of NK cell development and function. Clin. Immunol. 2017;177:60–69. doi: 10.1016/j.clim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bezman N.A., Cedars E., Steiner D.F., Blelloch R., Hesslein D.G., Lanier L.L. Distinct requirements of microRNAs in NK cell activation, survival, and function. J. Immunol. 2010;185:3835–3846. doi: 10.4049/jimmunol.1000980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Leong J.W., Sullivan R.P., Fehniger T.A. Natural Killer Cell Regulation by MicroRNAs in Health and Disease. J. Biomed. Biotechnol. 2012;2012:1–12. doi: 10.1155/2012/632329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Liu X., Wang Y., Sun Q., Yan J., Huang J., Zhu S., Yu J. Identification of microRNA transcriptome involved in human natural killer cell activation. Immunol. Lett. 2012;143:208–217. doi: 10.1016/j.imlet.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 109.Beaulieu A.M., Bezman N.A., Lee J.E., Matloubian M., Sun J.C., Lanier L.L. MicroRNA function in NK-cell biology. Immunol. Rev. 2013;253:40–52. doi: 10.1111/imr.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cichocki F., Felices M., McCullar V., Presnell S.R., Al-Attar A., Lutz C.T., Miller J.S. Cutting Edge: MicroRNA-181 Promotes Human NK Cell Development by Regulating Notch Signaling. J. Immunol. 2011;187:6171–6175. doi: 10.4049/jimmunol.1100835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bezman N.A., Chakraborty T., Bender T., Lanier L.L. miR-150 regulates the development of NK and iNKT cells. J. Exp. Med. 2011;208:2717–2731. doi: 10.1084/jem.20111386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sullivan R.P., Leong J.W., Schneider S.E., Ireland A.R., Berrien-Elliott M.M., Singh A., Schappe T., Jewell B.A., Sexl V., Fehniger T.A. MicroRNA-15/16 antagonizes Myb to control natural killer cell maturation. J. Immunol. 2015;195:2806–2817. doi: 10.4049/jimmunol.1500949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sullivan R.P., Leong J.W., Schneider S.E., Keppel C.R., Germino E., French A.R., Fehniger T.A. MicroRNA Deficient NK Cells Exhibit Decreased Survival but Enhanced Function. J. Immunol. 2012;188:3019–3030. doi: 10.4049/jimmunol.1102294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ma F., Xu S., Liu X., Zhang Q., Xu X., Liu M., Hua M., Li N., Yao H., Cao X. The microRNA miR-29 controls innate and adaptive immune responses to intracellular bacterial infection by targeting interferon-γ. Nat. Immunol. 2011;12:861–869. doi: 10.1038/ni.2073. [DOI] [PubMed] [Google Scholar]
- 115.Sullivan R.P., Fogel L.A., Leong J.W., Schneider S.E., Wong R., Romee R., Thai T.-H., Sexl V., Matkovich S.J., Dorn G.W., et al. miR-155 tunes both the threshold and extent of NK cell activation via targeting of multiple signaling pathways. J. Immunol. 2013;191:5904–5913. doi: 10.4049/jimmunol.1301950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Trotta R., Chen L., Ciarlariello D., Josyula S., Mao C., Costinean S., Yu L., Butchar J.P., Tridandapani S., Croce C.M., et al. miR-155 regulates IFN-γ production in natural killer cells. Blood. 2012;119:3478–3485. doi: 10.1182/blood-2011-12-398099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cheng Y.Q., Ren J.P., Zhao J., Wang J.M., Zhou Y., Li G.Y., Moorman J.P., Yao Z.Q. MicroRNA-155 regulates interferon-gamma production in natural killer cells via Tim-3 signalling in chronic hepatitis C virus infection. Immunology. 2015;145:485–497. doi: 10.1111/imm.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Watanabe A., Tagawa H., Yamashita J., Teshima K., Nara M., Iwamoto K., Kume M., Kameoka Y., Takahashi N., Nakagawa T., et al. The role of microRNA-150 as a tumor suppressor in malignant lymphoma. Leukemia. 2011;25:1324–1334. doi: 10.1038/leu.2011.81. [DOI] [PubMed] [Google Scholar]
- 119.Fehniger T.A., Wylie T., Germino E., Leong J.W., Magrini V.J., Koul S., Keppel C.R., Schneider S.E., Koboldt D.C., Sullivan R.P., et al. Next-generation sequencing identifies the natural killer cell microRNA transcriptome. Genome Res. 2010;20:1590–1604. doi: 10.1101/gr.107995.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kim N., Kim M., Yun S., Doh J., Greenberg P.D., Kim T.-D., Choi I. MicroRNA-150 regulates the cytotoxicity of natural killers by targeting perforin-1. J. Allergy Clin. Immunol. 2014;134:195–203. doi: 10.1016/j.jaci.2014.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kim T.-D., Lee S.U., Yun S., Sun H.-N., Lee S.H., Kim J.W., Kim H.M., Park S.-K., Lee C.W., Yoon S.R., et al. Human microRNA-27a* targets Prf1 and GzmB expression to regulate NK-cell cytotoxicity. Blood. 2011;118:5476–5486. doi: 10.1182/blood-2011-04-347526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang P., Gu Y., Zhang Q., Han Y., Hou J., Lin L., Wu C., Bao Y., Su X., Jiang M., et al. Identification of Resting and Type I IFN-Activated Human NK Cell miRNomes Reveals MicroRNA-378 and MicroRNA-30e as Negative Regulators of NK Cell Cytotoxicity. J. Immunol. 2012;189:211–221. doi: 10.4049/jimmunol.1200609. [DOI] [PubMed] [Google Scholar]
- 123.Espinoza J.L., Takami A., Yoshioka K., Nakata K., Sato T., Kasahara Y., Nakao S. Human microRNA-1245 down-regulates the NKG2D receptor in natural killer cells and impairs NKG2D-mediated functions. Haematologica. 2012;97:1295–1303. doi: 10.3324/haematol.2011.058529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Donatelli S.S., Zhou J.M., Gilvary D.L., Eksioglu E.A., Chen X., Cress W.D., Haura E.B., Schabath M.B., Coppola D., Wei S., et al. TGF-beta-inducible microRNA-183 silences tumor-associated natural killer cells. Proc. Nat. Acad. Sci. USA. 2014;111:4203–4208. doi: 10.1073/pnas.1319269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang H., Zhang Y., Wu X., Wang Y., Cui H., Li X., Zhang J., Tun N., Peng Y., Yu J. Regulation of Human Natural Killer Cell IFN-gamma Production by MicroRNA-146a via Targeting the NF-kappaB Signaling Pathway. Front. Immunol. 2018;9 doi: 10.3389/fimmu.2018.00293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Breunig C., Pahl J., Kublbeck M., Miller M., Antonelli D., Erdem N., Wirth C., Will R., Bott A., Cerwenka A., et al. MicroRNA-519a-3p mediates apoptosis resistance in breast cancer cells and their escape from recognition by natural killer cells. Cell Death Dis. 2017;8 doi: 10.1038/cddis.2017.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Trotta R., Chen L., Costinean S., Josyula S., Mundy-Bosse B.L., Ciarlariello D., Mao C., Briercheck E.L., McConnell K.K., Mishra A., et al. Overexpression of miR-155 causes expansion, arrest in terminal differentiation and functional activation of mouse natural killer cells. Blood. 2013;121:3126–3134. doi: 10.1182/blood-2012-12-467597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.He S., Chu J.H., Wu L.C., Mao H.Y., Peng Y., Alvarez-Breckenridge C.A., Hughes T., Wei M., Zhang J.Y., Yuan S.Z., et al. MicroRNAs activate natural killer cells through Toll-like receptor signaling. Blood. 2013;121:4663–4671. doi: 10.1182/blood-2012-07-441360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Scoville S.D., Nalin A., Chen L.X., Chen L., McConnell K., Casas S.B., Al-Rahman A., Hashi N., Zhang M., Saultz J., et al. The aryl hydrocarbon receptor directly regulates microRNA-29b to inhibit human natural killer cell development and function in acute myeloid leukemia. Cancer Res. 2018;78 doi: 10.1158/1538-7445.AM2018-4729. [DOI] [Google Scholar]
- 130.Zhao H., Su W., Kang Q., Xing Z., Lin X., Wu Z. Natural killer cells inhibit oxaliplatin-resistant colorectal cancer by repressing WBSCR22 via upregulating microRNA-146b-5p. Am. J. Cancer Res. 2018;8:824–834. [PMC free article] [PubMed] [Google Scholar]
- 131.Victor A.R., Weigel C., Scoville S.D., Chan W.K., Chatman K., Nemer M.M., Mao C., Young K.A., Zhang J., Yu J., et al. Epigenetic and Posttranscriptional Regulation of CD16 Expression during Human NK Cell Development. J. Immunol. 2018;200:565–572. doi: 10.4049/jimmunol.1701128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Liu X., Chen Q., Yan J., Wang Y., Zhu C., Chen C., Zhao X., Xu M., Sun Q., Deng R., et al. MiRNA-296-3p-ICAM-1 axis promotes metastasis of prostate cancer by possible enhancing survival of natural killer cell-resistant circulating tumour cells. Cell Death Dis. 2013;4 doi: 10.1038/cddis.2013.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xu D.Q., Han Q.J., Hou Z.H., Zhang C., Zhang J. miR-146a negatively regulates NK cell functions via STAT1 signaling. Cell. Mol. Immunol. 2017;14:712–720. doi: 10.1038/cmi.2015.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mikulak J., Bozzo L., Roberto A., Pontarini E., Tentorio P., Hudspeth K., Lugli E., Mavilio D. Dopamine Inhibits the Effector Functions of Activated NK Cells via the Upregulation of the D5 Receptor. J. Immunol. 2014;193:2792–2800. doi: 10.4049/jimmunol.1401114. [DOI] [PubMed] [Google Scholar]
- 135.Nachmani D., Zimmermann A., Djian E.O., Weisblum Y., Livneh Y., Le V.T.K., Galun E., Horejsi V., Isakov O., Shomron N., et al. MicroRNA Editing Facilitates Immune Elimination of HCMV Infected Cells. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1003963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ni F., Guo C., Sun R., Fu B.Q., Yang Y., Wu L.L., Ren S.T., Tian Z.G., Wei H.M. MicroRNA transcriptomes of distinct human NK cell populations identify miR-362-5p as an essential regulator of NK cell function. Sci. Rep. 2015;5 doi: 10.1038/srep09993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Xie J., Liu M., Li Y., Nie Y., Mi Q., Zhao S. Ovarian tumor-associated microRNA-20a decreases natural killer cell cytotoxicity by downregulating MICA/B expression. Cell. Mol. Immunol. 2014;11:495–502. doi: 10.1038/cmi.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Neviani P., Wise P.M., Murtadha M., Liu C.W., Wu C.H., Jong A.Y., Seeger R.C., Fabbri M. Natural Killer-Derived Exosomal miR-186 Inhibits Neuroblastoma Growth and Immune Escape Mechanisms. Cancer Res. 2019;79:1151–1164. doi: 10.1158/0008-5472.CAN-18-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Min D., Lv X.-B., Wang X., Zhang B., Meng W., Yu F., Hu H. Downregulation of miR-302c and miR-520c by 1,25(OH)2D3 treatment enhances the susceptibility of tumour cells to natural killer cell-mediated cytotoxicity. Br. J. Cancer. 2013;109:723–730. doi: 10.1038/bjc.2013.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Stelma F., van der Ree M.H., Sinnige M.J., Brown A., Swadling L., de Vree J.M.L., Willemse S.B., van der Valk M., Grint P., Neben S., et al. Immune Phenotype and Function of Natural Killer and T Cells in Chronic Hepatitis C Patients Who Received a Single Dose of Anti-MicroRNA-122, RG-101. Hepatology. 2017;66:57–68. doi: 10.1002/hep.29148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gong J., Liu R., Zhuang R., Zhang Y., Fang L., Xu Z., Jin L., Wang T., Song C., Yang K., et al. miR-30c-1* promotes natural killer cell cytotoxicity against human hepatoma cells by targeting the transcription factor HMBOX1. Cancer Sci. 2012;103:645–652. doi: 10.1111/j.1349-7006.2012.02207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Huang Y., Lei Y., Zhang H., Hou L., Zhang M., Dayton A.I. MicroRNA regulation of STAT4 protein expression: Rapid and sensitive modulation of IL-12 signaling in human natural killer cells. Blood. 2011;118:6793–6802. doi: 10.1182/blood-2011-05-356162. [DOI] [PubMed] [Google Scholar]
- 143.Xu H., Cheung I.Y., Guo H.-F., Cheung N.-K.V. MicroRNA miR-29 modulates expression of immunoinhibitory molecule B7-H3: Potential implications for immune based therapy of human solid tumors. Cancer Res. 2009;69:6275–6281. doi: 10.1158/0008-5472.CAN-08-4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mundy-Bosse B.L., Scoville S.D., Chen L., McConnell K., Mao H.C., Ahmed E.H., Zorko N., Harvey S., Cole J., Zhang X., et al. MicroRNA-29b mediates altered innate immune development in acute leukemia. J. Clin. Investig. 2016;126:4404–4416. doi: 10.1172/JCI85413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Feng L., Ma H., Chang L., Zhou X., Wang N., Zhao L., Zuo J., Wang Y., Han J., Wang G. Role of microRNA-141 in colorectal cancer with lymph node metastasis. Exp. Ther. Med. 2016;12:3405–3410. doi: 10.3892/etm.2016.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jasinski-Bergner S., Reches A., Stoehr C., Massa C., Gonschorek E., Huettelmaier S., Braun J., Wach S., Wullich B., Spath V., et al. Identification of novel microRNAs regulating HLA-G expression and investigating their clinical relevance in renal cell carcinoma. Oncotarget. 2016;7:26866–26878. doi: 10.18632/oncotarget.8567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Berchem G., Noman M.Z., Bosseler M., Paggetti J., Baconnais S., Le Cam E., Nanbakhsh A., Moussay E., Mami-Chouaib F., Janji B., et al. Hypoxic tumor-derived microvesicles negatively regulate NK cell function by a mechanism involving TGF- and miR23a transfer. Oncoimmunology. 2016;5 doi: 10.1080/2162402X.2015.1062968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tsukerman P., Stern-Ginossar N., Gur C., Glasner A., Nachmani D., Bauman Y., Yamin R., Vitenshtein A., Stanietsky N., Bar-Mag T., et al. MiR-10b Downregulates the Stress-Induced Cell Surface Molecule MICB, a Critical Ligand for Cancer Cell Recognition by Natural Killer Cells. Cancer Res. 2012;72:5463–5472. doi: 10.1158/0008-5472.CAN-11-2671. [DOI] [PubMed] [Google Scholar]
- 149.Yang H., Lan P., Hou Z., Guan Y., Zhang J., Xu W., Tian Z., Zhang C. Histone deacetylase inhibitor SAHA epigenetically regulates miR-17-92 cluster and MCM7 to upregulate MICA expression in hepatoma. Br. J. Cancer. 2015;112:112–121. doi: 10.1038/bjc.2014.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jiang H., Wang P., Li X., Wang Q., Deng Z.-B., Zhuang X., Mu J., Zhang L., Wang B., Yan J., et al. Restoration of MiR-17/20a in Solid Tumor Cells Enhances the Natural Killer Cell Antitumor Activity by Targeting Mekk2. Cancer Immunol. Res. 2014;2:789–799. doi: 10.1158/2326-6066.CIR-13-0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Su Z., Ye X., Shang L. MiR-506 Promotes Natural Killer Cell Cytotoxicity against Human Hepatocellular Carcinoma Cells by Targeting STAT3. Yonsei Med. J. 2019;60:22–29. doi: 10.3349/ymj.2019.60.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wu J.M., Zhang X.J., Shi K.Q., Chen Y.P., Ren Y.F., Song Y.J., Li G.L., Xue Y.F., Fang Y.X., Deng Z.J., et al. Hepatitis B surface antigen inhibits MICA and MICB expression via induction of cellular miRNAs in hepatocellular carcinoma cells. Carcinogenesis. 2014;35:155–163. doi: 10.1093/carcin/bgt268. [DOI] [PubMed] [Google Scholar]
- 153.Zhu X.-M., Han T., Wang X.-H., Li Y.-H., Yang H.-G., Luo Y.-N., Yin G.-W., Yao Y.-Q. Overexpression of miR-152 leads to reduced expression of human leukocyte antigen-G and increased natural killer cell mediated cytolysis in JEG-3 cells. Am. J. Obstet. Gynecol. 2010;202:e1–e7. doi: 10.1016/j.ajog.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 154.Regis S., Caliendo F., Dondero A., Casu B., Romano F., LoIacono F., Moretta A., Bottino C., Castriconi R. TGF-β1 Downregulates the Expression of CX3CR1 by Inducing miR-27a-5p in Primary Human NK Cells. Front. Immunol. 2017;8 doi: 10.3389/fimmu.2017.00868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhang J., Han X., Hu X., Jin F., Gao Z., Yin L., Qin J., Yin F., Li C., Wang Y. IDO1 impairs NK cell cytotoxicity by decreasing NKG2D/NKG2DLs via promoting miR-18a. Mol. Immunol. 2018;103:144–155. doi: 10.1016/j.molimm.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 156.Chen E.B., Zhou Z.J., Xiao K., Zhu G.Q., Yang Y., Wang B., Zhou S.L., Chen Q., Yin D., Wang Z., et al. The miR-561-5p/CX3CL1 Signaling Axis Regulates Pulmonary Metastasis in Hepatocellular Carcinoma Involving CX3CR1(+) Natural Killer Cells Infiltration. Theranostics. 2019;9:4779–4794. doi: 10.7150/thno.32543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wong T., Chen S., Zhang M., Chan J.Y., Gao W. Epstein-Barr virus-encoded microRNA BART7 downregulates major histocompatibility complex class I chain-related peptide A and reduces the cytotoxicity of natural killer cells to nasopharyngeal carcinoma. Oncol. Lett. 2018;16:2887–2892. doi: 10.3892/ol.2018.9041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Heinemann A., Zhao F., Pechlivanis S., Eberle J., Steinle A., Diederichs S., Schadendorf D., Paschen A. Tumor suppressive microRNAs miR-34a/c control cancer cell expression of ULBP2, a stress-induced ligand of the natural killer cell receptor NKG2D. Cancer Res. 2012;72:460–471. doi: 10.1158/0008-5472.CAN-11-1977. [DOI] [PubMed] [Google Scholar]
- 159.Dölken L., Krmpotić A., Kothe S., Tuddenham L., Tanguy M., Marcinowski L., Ruzsics Z., Elefant N., Altuvia Y., Margalit H., et al. Cytomegalovirus microRNAs Facilitate Persistent Virus Infection in Salivary Glands. PLoS Pathog. 2010;6 doi: 10.1371/journal.ppat.1001150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Huang Q., Ding J., Gong M., Wei M., Zhao Q., Yang J. Effect of miR-30e regulating NK cell activities on immune tolerance of maternal-fetal interface by targeting PRF1. Biomed. Pharmacother. 2019;109:1478–1487. doi: 10.1016/j.biopha.2018.09.172. [DOI] [PubMed] [Google Scholar]
- 161.De Pelsmaeker S., Romero N., Vitale M., Favoreel H.W. Herpesvirus Evasion of Natural Killer Cells. J. Virol. 2018;92 doi: 10.1128/JVI.02105-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bauman Y., Nachmani D., Vitenshtein A., Tsukerman P., Drayman N., Stern-Ginossar N., Lankry D., Gruda R., Mandelboim O. An Identical miRNA of the Human JC and BK Polyoma Viruses Targets the Stress-Induced Ligand ULBP3 to Escape Immune Elimination. Cell Host Microbe. 2011;9:93–102. doi: 10.1016/j.chom.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 163.Stern-Ginossar N., Elefant N., Zimmermann A., Wolf D.G., Saleh N., Biton M., Horwitz E., Prokocimer Z., Prichard M., Hahn G., et al. Host immune system gene targeting by a viral miRNA. Science. 2007;317:376–381. doi: 10.1126/science.1140956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Nachmani D., Stern-Ginossar N., Sarid R., Mandelboim O. Diverse Herpesvirus MicroRNAs Target the Stress-Induced Immune Ligand MICB to Escape Recognition by Natural Killer Cells. Cell Host Microbe. 2009;5:376–385. doi: 10.1016/j.chom.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 165.Huang W.-T., Lin C.-W. EBV-Encoded miR-BART20-5p and miR-BART8 Inhibit the IFN-γ–STAT1 Pathway Associated with Disease Progression in Nasal NK-Cell Lymphoma. Am. J. Pathol. 2014;184:1185–1197. doi: 10.1016/j.ajpath.2013.12.024. [DOI] [PubMed] [Google Scholar]
- 166.Enk J., Levi A., Weisblum Y., Yamin R., Charpak-Amikam Y., Wolf D.G., Mandelboim O. HSV1 MicroRNA Modulation of GPI Anchoring and Downstream Immune Evasion. Cell Rep. 2016;17:949–956. doi: 10.1016/j.celrep.2016.09.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Piedade D., Azevedo-Pereira J.M. The Role of microRNAs in the Pathogenesis of Herpesvirus Infection. Viruses. 2016;8:156. doi: 10.3390/v8060156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Leong J.W., Sullivan R.P., Fehniger T.A. microRNA management of NK-cell developmental and functional programs. Eur. J. Immunol. 2014;44:2862–2868. doi: 10.1002/eji.201444798. [DOI] [PMC free article] [PubMed] [Google Scholar]