Abstract
We explore the impacts of Malawi’s national unconditional cash transfer program targeting ultra-poor households on youth mental health. Experimental findings show that the program significantly improved mental health outcomes. Among girls in particular, the program reduces indications of depression by about 15 percentage points. We investigate the contribution of different possible pathways to the overall program impact, including education, health, consumption, caregiver’s stress levels and life satisfaction, perceived social support, and participation in hard and unpleasant work. The pathways explain from 46 to 65 percent of the program impact, advancing our understanding of how economic interventions can affect mental health of youth in resource-poor settings. The findings underline that unconditional cash grants, which are used on an increasingly large scale as part of national social protection systems in Sub-Saharan Africa, have the potential to improve youth mental wellbeing and thus may help break the vicious cycle of poverty and poor mental health.
Keywords: Cash transfers, Malawi, Mental health, Poverty, RCT, Youth
1. Introduction
Poverty and mental health are closely related. Poverty can be a cause of poor mental health outcomes, such as stress and depression. Poor mental health, moreover, can lead to impairment and thus poor economic outcomes. This vicious cycle of poverty and poor mental health has been documented, among others, by Patel and Kleinman (2003), Lund et al. (2011), and Haushofer and Fehr (2014). The relationship between poverty and mental health is particularly pertinent during adolescence and early adulthood, when most mental health disorders first arise and may affect broader psychosocial development and transitions to adulthood (Patel et al., 2007). Yet, we know little about the policies and interventions that help to address poor mental health outcomes of young people (Haushofer and Fehr, 2014; Lund et al., 2011; Patel et al., 2007).
In this paper, we examine whether and how Malawi’s scaled-up Social Cash Transfer Program (SCTP) affects youth mental health. The SCTP provides unconditional income support to ultra-poor, labor-constrained households. A cluster-randomized evaluation integrated into the roll-out of the program allows us to rigorously estimate the effects of the program (the evaluation design and wide-ranging effects of the SCTP is also discussed in two reports: CPC, 2016a & 2016b). In our analysis we rely on a short, commonly used screening instrument (the Center for Epidemiological Studies Depression scale, CES-D) to measure program impacts on depressive symptoms among youth aged 13 to 19 at baseline. We examine how impacts differ by gender and explore the pathways through which the SCTP may affect youth mental health.
There are plausible pathways through which programs like the SCTP may improve youth mental health. As outlined also in CPC (2016a), SCTP income support is expected to directly increase poor households’ expenditure on basic consumption goods and services, and may raise their investment in agricultural activities and schooling. These expenditures and investments may in turn improve youths’ mental health by increasing their school participation, improving their physical health, improving their food-security and ‘material wellbeing’, and reducing the need for youth to contribute to household income. They may also indirectly improve youth mental health by reducing stress experienced by caregivers and by improving the households’ social connections with community members and peers. Literature on each of these pathways is discussed in more detail in the Appendix. Program impacts are moderated by the gender of the youth: during early adolescence, depression rates typically increase rapidly for girls, resulting in a gender gap that persists for decades.
Indeed, three recent studies show that programs like the SCTP have the potential to substantively improve youth mental health in developing countries. These studies, alongside the current study are summarized in Table 1. In the Zomba district of Malawi, Baird et al. (2013) examine the effects of an NGO-run cash transfer on mental health among female youth aged 13 to 22. Experimental estimates show that unconditional and conditional cash transfers reduced indications of depression by about 14 and seven percentage points, respectively. Key pathways include better physical health, higher school attendance, personal consumption, and leisure. However, effects dissipated soon after the experiment ended. Higher transfers to the household contingent on girls’ schooling resulted in lower beneficial program effects on depression, suggesting that beneficiary girls experience responsibility for household income as a burden. Moreover, indications of depression changed for girls who lived in the areas randomized into the treatment group, but were not invited to participate in the program. If they lived in a household with another girl benefitting from the program, indications of depression decreased. In contrast, if they did not live in a household with a program beneficiary, indications of depression increased.
Table 1.
Comparison of the characteristics of studies examining the effects of cash transfer programs on youth mental health in Sub-Saharan Africa.
| Kenya | South Africa | Malawi | ||
|---|---|---|---|---|
| Kilburn et al. (2016) | Kilburn et al. (2018a) | Baird et al. (2013) | Present study: | |
| (1) | (2) | (3) | (4) | |
| Program & target population | UCT to poor households with orphan or vulnerable child aged < 18 | CCT to (households with) never-married or pregnant females aged 13–20 attending grades 8–11 | UCT versus CCT to (households with) never-married females aged 13–22 | UCT to ultra-poor, labor constrained households |
| Monthly transfer value | Flat transfer of US$20 per household | US$20 per guardian and US$10 per girl | Experimental variation at the household level (range: US$4–10) and the level of the girl (range: US$l-5) | Varies with household size (range: US$3–7) and composition (US$1 and 2 per primary and secondary school aged child respectively). |
| Transfer value (relative to pre-program consumption) | 20% | 16% | 10% | 18–23% |
| Program implementation period before main measurement | 4 years | 3 years | 1 year | 2 years |
| Mental health instrument | CES-D | CES-D | GHQ-12 | CES-D |
| Age range (years) of interviewed youth (endline) | 15–24 | 16–23 (in school at baseline) | 15–24 | 15–22 |
| Average impact on probability of depressive symptoms (females) | Not significant (mean in control 33%) | Not significant (mean in control 4.4) | UCT (in school at baseline): −14 pps CCT (in school at baseline): −6 pps (mean in control 38%) CCT (out of school at baseline): Not significant (mean in control 46%) |
− 15 pps (mean in control 68%) |
| Average impact on probability of depressive symptoms (males) | − 9 pps (mean in control 40%) | N.A. | N.A. | − 15 pps (mean in control 55%) |
Notes: CES-D=Center for Epidemiological Studies Depression Scale; CCT: conditional cash transfer; GHQ-12=General Health Questionnaire-12; UCT = Unconditional cash transfer; pps=percentage points. Due to exchange rate fluctuations, monthly transfer amounts are approximations. Transfer amounts for the present study reflect the inflation correction described in this paper. The primary impact estimate reported for Baird et al. (2013) was obtained after one year of program implementation, when the program was still in progress. The ages of interviewed youth for Baird et al. (2013) and the present study are approximations, based on ages reported at baseline. The percentage point impacts for Kilburn et al. (2016) represent unadjusted differences, kindly calculated by the authors for the preparation of this table. Kilburn et al. (2018a) report CES-D z-score and scale only, and not depressive symptoms.
Kilburn et al. (2016), show that the scaled-up, unconditional, government-run Cash Transfer for Orphans and Vulnerable Children in Kenya reduced the odds of depressive symptoms by 24 percent among youth aged 15 to 24, however these reductions were concentrated among male and orphan youth. Although the program substantially increased school enrollment, changes in school participation do not appear to explain the improvement in mental wellbeing. Finally, Kilburn et al. (2018a) find that an NGO-run cash transfer conditional on school attendance in South Africa had no average impact on the CES-D scale among female youth aged 13–20 at baseline, yet improved both mental health and hope among girls in the poorest households at baseline. Taken together, these results show promise for similar income support programs to improve youth mental health. However, questions remain concerning the importance of gender, as well as program design and mechanisms underlying impacts.
2. Research design and setting
2.1. Malawi Social Cash Transfer Program
The Malawi SCTP is implemented by the Ministry of Gender, Children, Disability and Social Welfare, with overall policy coordination on social protection by the Ministry of Finance, Economic Planning and Development. The program started as a pilot in the Michinji district and has since undergone scale-up, currently reaching approximately 330,000 households in all 28 districts. The objectives of the SCTP are to reduce poverty and hunger, and to increase school enrolment rates. Eligibility is determined based on households being: 1) ultra-poor (defined as being unable to meet basic and essential needs, including food), and 2) labor-constrained (defined as having no household members who are ‘fit to work’—i.e., below 19 or above 64, or having a chronic disability or illness—, or if the ratio of unfit to fit exceeds three). A community-based targeting approach is used, where Community Social Support Committees identify households meeting the eligibility criteria. Thereafter, the ultra-poor eligibility criterion is verified using a proxy means test, resulting in within-community coverage of approximately 10 percent.
The transfer is variable based on households’ size and composition, with extra funds for households with primary and secondary school-age children, delivered bimonthly at a local pay point. The transfer was originally equal to approximately 17 percent of median baseline consumption, and was adjusted up to 23 percent of the same in May 2015 (i.e. during the period covered by the experiment discussed in this paper – see timeline below) to account for inflation (CPC 2014; 2016). Although the transfer is unconditional, there is messaging around use of the transfer to encourage beneficiaries to use it to invest in the human capital of children and for household basic needs. Although not a requirement, due to the targeting formula, the majority of transfer recipients are female (83.5 percent within the evaluation sample).
2.2. Study design and data collection
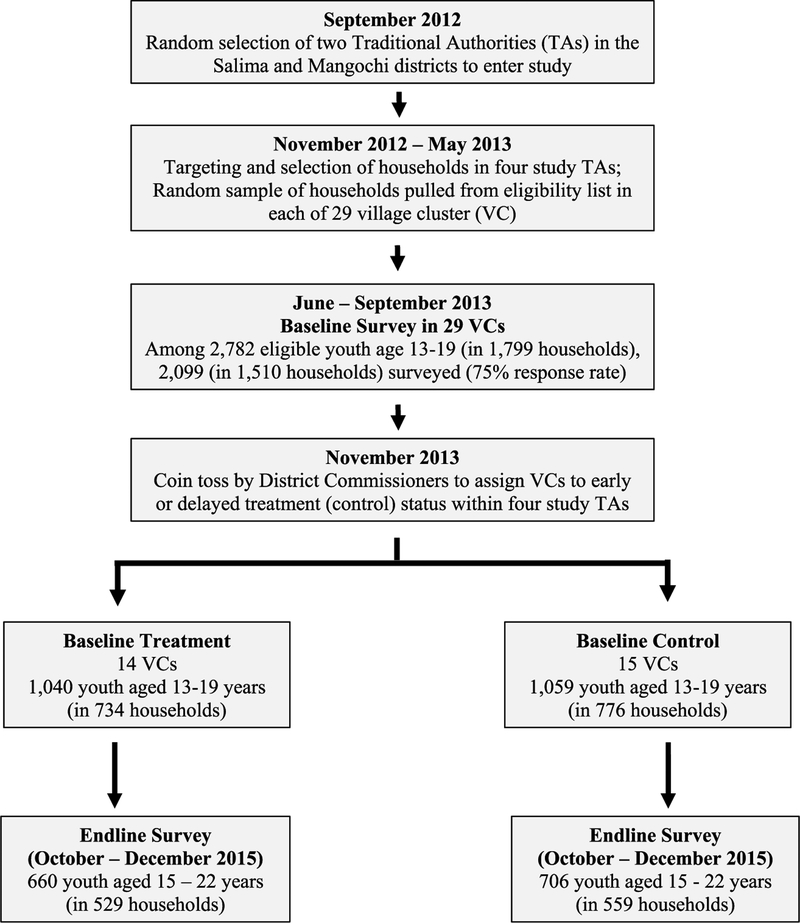
We rely on a cluster-randomized controlled trial (RCT) led by the University of North Carolina in collaboration with the Center for Social Research at the University of Malawi. Fig. 1 describes the treatment assignment and stages of randomization. The RCT was implemented in the districts of Mangochi and Salima, both selected by the Government of Malawi as they were part of scale-up planning. In both districts, two geographical groupings called Traditional Authorities (TAs) were randomly selected into the study (Jalasi and Mbwana Nyambi in Mangochi and Maganga and Ndindi in Salima) in September of 2012. Within these TAs a total of 29 so-called village clusters was randomly selected in the months of June (Salima) and July (Mangochi) of 2013 (Appendix Fig. 1). The number 29 was based on power calculations of under-five child anthropometry, which was deemed to be the key outcome. Selection of TAs and village clusters was carried out during meetings including government representatives and other stakeholders.
Fig. 1.
Study design and sample for baseline to endline longitudinal sample of youth.
Sample represents the longitudinal panel of youth interviewed at baseline and again at endline with non-missing mental health indicators. Approximately 10 youth in the baseline-endline sample were missing any indicators which comprise the CES-D and therefore are dropped from the analysis. In addition, the longitudinal sample at midline is 652 youth (Treatment) 640 youth (Control) for a total panel of 1292 youth (not shown). Approximately 6 youth in the baseline-midline sample were missing any indicators which comprise the CES-D score and therefore are dropped from the analysis.
Data for the baseline survey was collected between July and September 2013. Households were randomly sampled from all households identified as eligible during the targeting process described above (ranging from 66 to 135 households per village cluster) to meet sample size requirements stratified by TA. The total baseline sample consisted of 3531 SCTP-eligible households. The total number of eligible youth aged 13–19 in these households at baseline was 2782. Due to survey logistical constraints, up to three youths aged 13–19 at baseline per household were asked to participate in one-on-one interviews, conducted in private with interviewers of the same sex. In case there were more than three youth in a household, the youngest or the youth with the same sex as the primary enumerator were prioritized. The youth questionnaires contained questions on mental health, social support, sexual activity, among others, which form the basis for the outcome measures analyzed in this paper. After the baseline survey, village clusters were randomly assigned either to treatment (14 village clusters with 1678 households) or comparison (15 village clusters with 1853 households) at a public event.
Two subsequent surveys were conducted on the longitudinal panel of baseline households, again interviewing up to three youth per household. Midline data were collected in November–December 2014 and endline data in October–December 2015, when the baseline youth cohort were approximately 15–22 years old. The analysis mostly focuses on the data collected at endline using the panel of youth interviewed at both baseline and endline, however we provide additional sensitivity analysis on midline impacts to understand the evolution of impacts. At endline, beneficiary households had received approximately 24 months of bi-monthly payments. Interviews were conducted orally in local languages of Chichewa or Chiyao. The household questionnaire targeted the SCTP recipient, who, based on the household demographics is also likely to be the primary caregiver of the youth. For simplicity, we refer to this individual as the caregiver. The Appendix gives additional study design details.
Findings from the baseline report show that 85 percent and 60 percent of the sample at baseline classified as poor and ultra-poor according to national definitions (in contrast rural poverty in national estimates equals 58 and 28 percent respectively) (CPC 2014). Households have an average dependency ratio of 3, meaning each fit, prime age adult supports three children or elderly. Results from the endline evaluation report show that the SCTP had beneficial midline and end-line impacts on poverty, consumption and food security of the households, economic and productive activities, and children’s school participation, among others (CPC, 2016a). Operational performance of the program was found to be sound, with full payments to beneficiaries occurring regularly, and high levels of knowledge about the program and few corruption or security concerns.
3. Estimation strategy and key indicators
3.1. Mental health indicators
We measured mental health using a 10-item short-form of the longer 20-item CES-D scale. As we describe in more detail in the Appendix, the 10-item CES-D is widely used and has been validated internationally, including in settings such as that studied here. Ten questions were asked on a four-point Likert scale. Over the previous seven days, how often: (i) “did you sleep well?”, (ii) “were you happy?”, (iii) “did you have trouble concentrating?”, (iv) “feel hopeful about the future?”, (v) “feel that everything you did was an effort?“, (vi) “did you feel lonely?“, (vii) “did you feel depressed?”, (viii) “did you feel that you could not get going?”, (ix) “were you bothered by things that don’t usually bother you?”, (x) “did you feel fearful?” We follow previous studies undertaken in Sub-Saharan Africa (SSA) (see Appendix) to transform the responses to the individual CES-D items into two summary indicators. The first consists of the summed scores for all questions normalized by subtracting 10 from the total (thus ranging from 0 to 30), with higher scores reflecting more depressive symptoms. The second consists of a binary outcome variable indicating whether the respondent scored above a validated threshold for depressive symptoms (score ≥ 10). The Cronbach’s alpha, a measure of inter-item reliability, is 0.714 at baseline and 0.786 at endline for the CES-D in the overall sample, indicating a good consistency between indicators (where the rule of thumb is above 0.70).
3.2. Attrition and baseline balance
Table 2 examines youth response rates at baseline, attrition rates from baseline to endline and baseline means for our main outcome variables. We show averages for the treatment and control communities (columns (2) and (3)) and test whether differences between the two groups are statistically significant (below we describe how we calculate the p-values shown in column (4)). The baseline response rate (i.e., the share of eligible youth that was surveyed) equaled 75 percent – a percentage that does not differ between treatment and control in the full sample (i.e., females and males combined) (Panel A) and in the subsamples of females (Panel B) and males (Panel C) separately.
Table 2.
Overall attrition and baseline means by program status of outcomes among panel youth aged 13 to 19, by gender
| N | Treatment average | Control average | P-value of diff. | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Panel A. Full sample | ||||
| Baseline interview response | 2782 | 0.76 | 0.75 | 0.74 |
| Attrition from baseline to endline | 2099 | 0.38 | 0.36 | 0.53 |
| Outcomes CES-D, 0 to 30 | 1366 | 9.76 | 10.10 | 0.25 |
| Depressive symptoms (CES-D ≥ 10) | 1366 | 0.45 | 0.48 | 0.28 |
| Panel B. Female sample | ||||
| Baseline interview response | 1338 | 0.75 | 0.77 | 0.68 |
| Attrition from baseline to endline | 1020 | 0.40 | 0.39 | 0.86 |
| Outcomes CES-D, 0 to 30 | 635 | 10.14 | 9.97 | 0.74 |
| Depressive symptoms (CES-D ≥ 10) | 635 | 0.50 | 0.48 | 0.59 |
| Panel C. Male sample | ||||
| Baseline interview response | 1444 | 0.77 | 0.72 | 0.26 |
| Attrition from baseline to endline | 1079 | 0.36 | 0.33 | 0.39 |
| Outcomes CES-D, 0 to 30 | 731 | 9.43 | 10.25 | 0.06 |
| Depressive symptoms (CES-D ≥ 10) | 731 | 0.41 | 0.49 | 0.03 |
Notes: “Baseline interview response” shows the fraction of eligible youth at baseline actually interviewed at baseline. “Attrition from baseline to endline” shows the attrition among all those interviewed at baseline and re-interviewed at endline. The reported means for each group are computed based on linear regressions that control for Treatment and the traditional authority strata. P-values are reported from Wald tests that the coefficient on Treatment is equal to zero. The reported means for the outcome variables are computed as the average value of each variable for each group based on fully interacted linear regressions that control for a dummy for attriters and traditional authority strata, all interacted with the treatment dummy. P-values are reported from Wald tests that the predicted values (of each listed dependent variable) for Treatment and Control are equal. Robust standard errors adjusted for clustering at the village cluster level in parentheses (total of 29 clusters). All regressions are weighted according to the probability of youth being selected for interview at baseline (except for “Baseline interview response,” where simple household weights are used).
Of the 2099 adolescents who were interviewed at baseline with non-missing CES-D scores, 37 percent were not re-interviewed at endline. As Table 2 shows, there are no significant differences in attrition rates between treatment and control in the full sample, or the subsamples of females and males. The rest of Table 2 investigates our outcome variables—the continuous CES-D scores and the binary indicator for depressive symptoms. In the control group, nearly 50 percent of the female sample was classified as exhibiting depressive symptoms. This share was not significantly different for females in the treatment group. However, there is statistically significant imbalance in the male sub-sample, with 49 percent exhibiting depressive symptoms in the control group against 41 percent in the treatment group.
Additional attrition and balance tests are presented in the Appendix. We show that there are few violations of balance for females in the panel sample, also if we consider a wider range of baseline covariates. We do observe some violations of balance for males, including for the CES-D item on “Most times was bothered by things.” Within the treatment and control group, youth who were not interviewed at baseline are generally similar to youth who were, in terms of characteristics recorded in the baseline household survey administered to the care-giver. Likewise, within the treatment and control group, youth who attrited from baseline to follow-up are similar to those in the panel sample. Based on these results, we conclude that despite a high level of attrition the randomization was in general successful in balancing baseline characteristics across treatment and control among females. The imbalance for boys appears to be due to chance in the randomization process and not due to differential non-response or attrition. This imbalance does not necessarily invalidate our experimental design and the availability of baseline data allow us to correct for the initial imbalance in the empirical analysis.
3.3. Specification
We estimate the intent-to-treat (ITT) effect of the SCTP on youth mental health. In our primary and preferred analysis we rely on analysis of covariance (ANCOVA) estimates that control for the baseline value of the outcome variable. When data are weakly autocorrelated (i.e., with autocorrelation lower than 0.5), the ANCOVA estimator is preferred to differences-in-differences (DD) (McKenzie, 2012), because the latter will over-correct for baseline differences that only weakly predict future outcomes and will be costly in terms of power. In our data, correlations between baseline and endline means of the outcome variables are low (0.07 and 0.04 for CES-D and depressive symptoms, respectively, for the full sample). The correlations are lower for females (0.03 and 0.00, both insignificant) than males (0.11 and 0.08, both significant).
We specify the ANCOVA model as follows:
| (1) |
Here, Yij1 is the outcome of interest (either the CES-D score or the indicator for depressive symptoms) for youth i from village cluster j observed at endline. Treatmentj is a binary variable taking the value 1 for treatment village clusters (0 otherwise), Yij0 is the outcome of interest at baseline, and Xij0 is a vector of baseline covariates, including youth age dummies (from 14 to 19), single or double orphan status, whether the caregiver is female, whether she/he is literate, household size and, in the full sample of males and females, a dummy for gender. μ is a vector of dummies for TA strata (3 dummies). δ represents the ITT estimator of the program impact.
We examine the robustness of our findings using the following DD specification:
| (2) |
Here, Endlineit is a dummy equal to one if the individual is observed at endline, zero otherwise. The remaining covariates are specified as in equation (1). β1, the coefficient corresponding to the interaction term between TreatmentJ and Endlineit, is the DD ITT estimator, or the effect of being in a treatment village cluster, after correcting for any initial imbalance in the outcome variables and controlling for baseline characteristics.
We estimate (1) and (2) using OLS (i.e. a linear probability model for the binary outcome) and adjust the standard errors for clustering at the village cluster level (the level of randomization). We also correct for the small number of clusters (n = 29) using the wild bootstrap procedure proposed by Cameron et al. (2008) and programmed for Stata by Roodman (2015), showing the p-value corresponding to the coefficient of interest —δ for model (1) and β1 for model (2). Finally, given that 75 percent of the eligible youth were interviewed at baseline (see section 3b), all regressions are weighted according to the probability of youth being selected for interview at baseline.
4. Results
4.1. Basic impacts on mental health
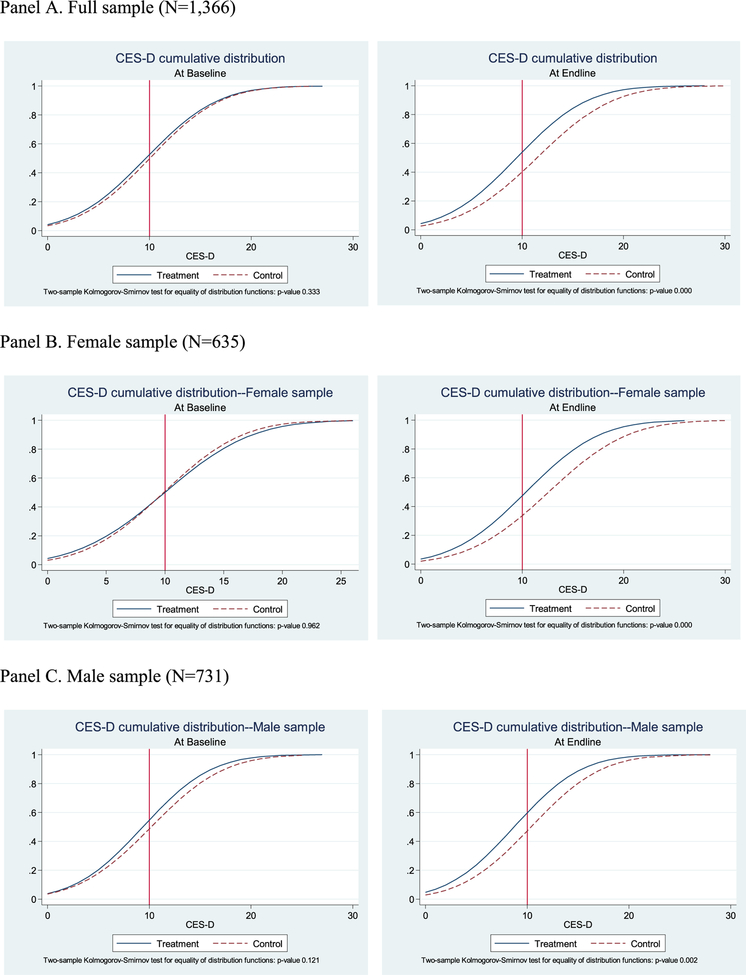
Fig. 2 plots the cumulative distribution functions (CDFs) of the CESD scores by treatment status, separately for baseline (left) and endline (right). The CDFs are drawn for the full sample of panel youth (Panel A), and separately by gender (Panels B and C). The vertical line represents the threshold CES-D score of 10 or above which an individual is classified as exhibiting depressive symptoms or being depressed (see section 4a). The dashed lines represent youths from control villages and the solid line represents youths from treatment villages.
Fig. 2.
Cumulative distribution functions of CES-D by gender and treatment status
Notes: The figures show Gaussian probability curves with the same mean and standard deviation of the empirical CDFs.
At baseline, the CDFs for youth in the treatment and control groups almost overlap, confirming that randomization was generally successful. Indeed, we cannot reject the hypothesis that the two distributions are equal based on a Kolmogorov-Smirnov test (P-value of 0.333). The right-hand graph of Panel A graphically shows a clear impact of the program on the mental health of youth. The proportion of youth with a score below any specific level is higher for the treatment group compared to the control group and we can reject the hypothesis of equality of the two distributions based on the Kolmogorov-Smirnov test with a p-value of 0.000. These findings also confirm that the program impacts do not depend on the choice of a specific threshold of the CES-D score and rather provide evidence of effects on mental health at any given threshold.
The rest of Fig. 2 shows the graphs for females and males separately. Baseline balance is clear for the female sample. There appears to be some initial imbalance for the male sample, although we cannot reject that the distributions are equal for treatment and control (P-value of = 0.121). The endline graphs reveal a large program impact, especially for females. In both cases we can reject the hypothesis of equality of the two distributions based on the Kolmogorov-Smirnov test with a p-values of 0.000 and 0.002 for females and males, respectively. This indicates that visually, early effects were driven by females in the full sample, which we explore in greater detail in subsequent analysis.
We now turn to the regression results. Table 3 presents ITT impacts of the Malawi SCTP on youth mental health indicators estimated based on our preferred ANCOVA (Panel A) and DD (Panel B) specification as a robustness check, for the full sample and separately by gender (full regressions are shown in the Appendix).
Table 3.
Impacts of the Malawi SCTP on CES-D and binary measure of depressive symptoms (ANCOVA and Difference-in-Differences).
| Panel A. Preferred estimates | ANCOVA | |||||
|---|---|---|---|---|---|---|
| CES-D | Depressive symptoms | |||||
| All | female | male | All | female | male | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Treatment | −2.051*** (0.475) |
−2.277*** (0.814) |
−1.828*** (0.457) |
−0.149*** (0.038) |
−0.152** (0.061) |
−0.145*** (0.039) |
| Baseline CES-D | 0.063*** (0.02) |
0.041 (0.038) |
0.090** (0.034) |
|||
| Baseline depressive symptoms | 0.035 (0.021) |
0.008 (0.036) |
0.065* (0.032) |
|||
| Endline mean for control | 11.53 | 12.57 | 10.48 | 0.62 | 0.68 | 0.55 |
| Observations | 1366 | 635 | 731 | 1366 | 635 | 731 |
| P-value wild bootstrap | 0.001 | 0.024 | 0.000 | 0.003 | 0.038 | 0.000 |
| Panel B. Robustness check | Differences-in-Differences | |||||
| CES-D | Depressive symptoms | |||||
| All | Female | male | All | female | male | |
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Treatment*Endline | −1.612** (0.707) |
−2.327* (1.178) |
−0.844 (0.793) |
−0.104 (0.063) |
−0.161 (0.097) |
−0.046 (0.068) |
| Treatment | −0.411 (0.441) |
0.142 (0.667) |
−0.947* (0.517) |
−0.04 (0.042) |
0.022 (0.057) |
−0.097** (0.045) |
| Endline | 1.429*** (0.399) | 2.707*** (0.852) | 0.187 (0.42) | 0.132*** (0.033) | 0.213*** (0.062) | 0.053 (0.043) |
| Endline mean for control | 11.53 | 12.57 | 10.48 | 0.62 | 0.68 | 0.55 |
| Observations | 2732 | 1270 | 1462 | 2732 | 1270 | 1462 |
| P-value wild bootstrap | 0.044 | 0.064 | 0.286 | 0.131 | 0.127 | 0.467 |
Notes: OLS estimates. Robust standard errors adjusted for clustering at the village cluster level in parentheses (total of 29 clusters). ***, ** and * indicate significance at 1%, 5% and 10% level, respectively. The dependent variables in the regressions estimated in panel A are endline values, while in panel B they are the time varying. All regressions include the following controls: baseline youth characteristics (age dummies from 14 to 19, single or double orphan status), baseline household characteristics (whether the caregiver is female, whether she/he is literate, and household size), and dummies for traditional authority strata. The regressions on the full sample of males and females also include a dummy for youth gender. “Treatment” is a dummy = 1 if treated. “P-value wild bootstrap” shows the p-value corresponding to the “Treatment” coefficient in panel A, and the “Treatment*Endline” coefficient in panel B, adjusted for the small number of clusters using the wild bootstrap procedure. All regressions are weighted according to the probability of youth being selected for interview at baseline.
The SCTP has a substantive and statistically significant impact on youth mental health at endline. Based on the ANCOVA and DD specifications, youth in treatment clusters experienced a significant reduction in the CES-D score of about 1.6–2.0 points over the 11.5 point mean for the control group at endline (column (1)). The probability of suffering from depressive symptoms was reduced by about 10–15 percentage points or 17–24 percent (Column (4)). The program had a particularly strong effect on the mental health of females, for whom the CES-D score is about 2.3 points lower at endline compared to a mean of 12.6 for the control group (column (2)). Their probability of exhibiting symptoms of depression is reduced by about 15–16 percentage points (a reduction of about 22 percent, column (5)). Impacts on males depend on the specification. Point estimates based on the ANCOVA model are more pronounced than those based on the DD model (columns (3) and (6)). The ANCOVA suggests the program reduced summed CESD scores by 1.8 points (against a control mean of 10.5) and depressive symptoms by 14.5 percentage points (a reduction of 26 percent). These effects are similar to those for females. The DD point estimates, which correct for baseline imbalance, have the same sign but are smaller and not statistically significant.
Other interesting gender differences emerge from the DD results. There is a significant increase in both the CES-D score and the likelihood of depressive symptoms over time in the control group for females only (see the coefficients for “endline”, columns (2) and (5)). While gender differences in average mental health outcomes among youth aged 13 to 19 in the control group at baseline are small (compare the outcome means in Panel B and C of Table 21, column 3) and insignificant (with a p-value of 0.606 for CES-D and 0.727 for depressive symptoms), these differences increase substantially with youth age. By endline the gap is large, with CES-D scores of females exceeding those of males by approximately 2 points and symptoms of depression exceeding those of boys by 13 percentage points (p-values equal to 0), confirming that gender differences develop rapidly in this age range (Table 3, endline means for control). This pattern is consistent with the psychology literature discussed in the Appendix, which shows that gender differences in depression open up around age 13 and continue to widen during adolescence and after. The results shown in Table 3 indicate that the SCTP had a strong effect on youth mental health capable of offsetting the gender mental health gap by endline.
We carried out several checks to further probe the robustness of our findings, displayed in the Appendix.
4.2. Channels of impact
Given the unequivocal impacts on females, in the following analysis we only present results for the female subsample. Moreover, since we found very low autocorrelations and good baseline balance in this subsample, we show the ANCOVA estimates as our preferred specification. We now explore the possible channels through which the Malawi SCTP affects girls’ mental health outcomes, building on the hypothesized pathways of impact.
4.2.1. Impacts on the pathways
We first examine the ITT impacts of the program on the channels we can measure in our data: youth education, health, and consumption, caregiver wellbeing and distress, social support, and hard and unpleasant work. We constructed 13 relevant pathway variables based on information provided by either caregiver responses to the household questionnaire, or by the youth directly (see Appendix for definitions and baseline balance tests). We regressed these pathway variables on the treatment dummy, the baseline covariates and the TA strata. We rely on cross-sectional regressions at endline, because perceived social support and casual labor questions were only asked at endline. In the Appendix we confirm that the ITT impacts on the other indicators are very similar if estimated with ANCOVA for pathway variables for which we have baseline data.
Table 4 shows that the SCTP had large significant impacts on current school attendance, with females in the treatment group being 12 percentage points more likely to be in school compared to the control group (a 28 percent increase over the mean in the control at endline, column (1)) and having completed 0.7 additional grades (compared to 5.5 grades in the control group, column (2)).
Table 4.
Impacts the Malawi SCTP on potential pathways, females (cross-sectional at endline)
| Education | Health | Consumption | Caregiver | Social support | Casual labor | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Currently enrolled in school | Grade attainment | Poor self-rated health | Illness or injury | AnyHH expenditure on girls’ clothing | AnyHH expenditure on girls’ shoes | Worry about food | Quality of life scale | Perceived stress scale | Number of friends | Number of family contacts | Multi-dimensional scale of perceived social support | Engaged in any casual labor | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | |
| Treatment | 0.122** (0.047) |
0.709* (0.347) |
−0.002 (0.006) |
−0.030 (0.029) |
0.234*** (0.035) |
0.103*** (0.022) |
−0.214*** (0.038) |
0.374*** (0.091) |
−0.312*** (0.079) |
0.257 (0.442) |
−0.229 (0.924) |
0.732*** (0.191) |
−0.118* (0.063) |
| Endline control mean | 0.43 | 5.48 | 0.01 | 0.18 | 0.10 | 0.01 | 0.92 | 2.50 | 3.53 | 4.07 | 7.29 | −0.20 | 0.49 |
| Observations | 635 | 635 | 635 | 635 | 635 | 635 | 635 | 632 | 635 | 635 | 635 | 635 | 635 |
| P-value wild boot. | 0.032 | 0.066 | 0.718 | 0.320 | 0.000 | 0.000 | 0.000 | 0.001 | 0.001 | 0.571 | 0.839 | 0.001 | 0.109 |
Notes: OLS estimates. Robust standard errors clustered at the village cluster level in parentheses (29 clusters). ***, ** and * indicate significance at 1%, 5% and 10% level, respectively. Regressions include the following controls: dummies for traditional authority strata, baseline youth characteristics (age dummies from 14 to 19, single or double orphan status), and baseline household characteristics (whether the caregiver is female, whether she/he is literate, and household size). a, baseline youth characteristics (age dummies from 14ng to the ngle or double orphan status), and baseline household characteristics (whether the cartrap procedure. All regressions are weighted according to the probability of youth being selected for interview at baseline.
The SCTP did not have a significant effect on females’ physical health according to two indicators: overall self-rated poor health and illness or injury in the two weeks prior to the interview (columns 3–4). Our measures of female’s consumption, in contrast, were strongly impacted by the program (columns 5–7). The fraction of households that made any purchase of females’ clothing items (shoes) is more than two (ten) times higher in the treatment group compared to the control. Moreover, there is a significant 19.5 percentage point reduction in the likelihood that the caregiver worried about the household not having enough food. The program had strong and significant beneficial impacts on two scales measuring caregivers’ quality of life (Diener et al., 1985; WHO, 1998) (column (8)) and psychological stress (Cohen et al., 1983) (column (9)). For simplicity, both of these scales are rescaled so that they range from 1 to 5.
While the program did not affect the number of friends and family contacts (columns 10–11), it had a significant beneficial effect on an index measuring the perceived level of support from friends and family (Zimet et al., 1988) (column 12). The Appendix shows the dis-aggregated impacts on individual items of the index, indicating that stronger impacts come from friends, rather than family perceived support. The effect of the SCTP on social support from friends could be the result of a combination of factors, including additional opportunities to nurture contacts with friends by being in school as well as through higher household spending on girls’ clothing and shoes which leads to better opportunities for them to socialize and reduced stigma.
Finally, column 13 of Table 4 shows that girls in the treatment group are about 12 percentage points less likely to be engaged in informal piece work for at least 1 h in the week prior to the endline interview (equivalent to a 24 percent effect, and significant at the 10 percent level). Changes in household members labor supply are documented in more detail in de Hoop et al. (2019).
4.2.2. Impacts on mental health, including endogenous pathways
To assess how much of the total ITT impact on mental health outcomes can be explained by each of the potential channels, we follow the methodology employed in Baird et al. (2013) based on Flores and Flores-Lagunes (2009). To identify a casual mediation effect, the assumption of sequential ignorability must be upheld. There are two parts of sequential ignorability: (1) treatment must be independent of both potential values of outcome and mediating variables and (2) the mediator must be independent of all potential values of the outcome conditioned on the observed treatment and pretreatment covariates (Imani et al., 2010). The first part of sequential ignorability is effectively satisfied with randomization to treatment, but the second part implies that mediators must also be regarded as “as-if” randomized among treatment arms (Keele et al., 2015). To satisfy the second part of this assumption, we control for all pretreatment covariates that may confound the relationship between the mediators and mental health so that the outcome is modeled as a function of the mediator, treatment, and pretreatment covariates including pretreatment levels of each mediator (where baseline variables are available).
We re-estimate the effect of the program on CES-D scores and symptoms of depression including the endline (baseline) values of the pathways (or mediators) as additional regressors. We interpret the coefficient on the treatment indicator as the “net”, or “mediated”, ITT impact after accounting for the effects of the pathways. Caution should be used when interpreting the results as the estimated effect of the mediators and the mediated impact cannot be interpreted as experimentally identified.
Table 5 presents the results with each channel first entered separately (columns (2)–(6) and (9)–(13) for CES-D and depressive symptoms, respectively), and then entered simultaneously (columns (7) and (14)). We only consider the pathways that were significantly affected by the program (i.e. we exclude the health channel, number of friends and family). To make comparisons with the unmediated impact easier, we also report basic impacts on mental health outcomes in columns (1) and (8). The share of the total ITT impact explained by the pathways is shown at the bottom of the table.
Table 5.
ANCOVA estimate of the Malawi SCTP on CES-D and binary measure of depressive symptoms, including endogenous channels (females)
| CES-D | Depressive symptoms | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Basic impacts | Education | Consump-tion | Caregiver | Social support | Casual labor | All channels | Basic impacts | Education | Consump-tion | Caregiver | Social support | Casual labor | All channels | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | |
| Treatment | −2.277*** (0.814) |
−1.958** (0.740) |
−2.080** (0.809) |
−1.913** (0.847) |
−1.681** (0.799) |
−2.117** (0.787) |
−1.219 (0.732) |
−0.152** (0.061) |
−0.129** (0.056) |
−0.118* (0.059) |
−0.119* (0.062) |
−0.116* (0.062) |
−0.143** (0.059) |
−0.053 (0.052) |
| CES-D (baseline) | 0.041 (0.038) |
0.032 (0.036) |
0.039 (0.036) |
0.031 (0.037) |
0.023 (0.041) |
0.031 (0.040) |
0.012 (0.039) |
|||||||
| Depressive symptoms (baseline) | 0.008 (0.036) |
0.004 (0.034) |
0.004 (0.035) |
0.008 (0.036) |
0.000 (0.036) |
0.003 (0.036) |
−0.003 (0.034) |
|||||||
| Currently enrolled (endline) | −1.610** (0.600) | −1.479** (0.639) |
−0.100* (0.052) |
−0.101* (0.057) |
||||||||||
| Grade attainment (endline) | −0.181 (0.145) |
−0.035 (0.149) |
−0.015 (0.012) |
−0.006 (0.011) |
||||||||||
| Any HH exp girls cloths (endline) | −0.587 (0.530) |
−0.203 (0.548) |
−0.089* (0.047) |
−0.081* (0.041) |
||||||||||
| Any HH exp girls shoes (endline) | 0.234 (1.350) |
1.248 (0.986) |
−0.014 (0.087) |
0.043 (0.079) |
||||||||||
| Worry about food (endline) | 0.365 (0.658) |
0.149 (0.566) |
0.055 (0.051) |
0.033 (0.047) |
||||||||||
| Quality of life scale (endline) | 0.049 (0.394) |
0.128 (0.391) |
−0.004 (0.025) |
−0.000 (0.025) |
||||||||||
| Perceived stress scale (endline) | 1.091*** (0.304) |
1.002*** (0.305) |
0.094*** (0.027) |
0.089*** (0.027) |
||||||||||
| Multi-dimensional scale of perceived social support (endline) | −0.809*** (0.120) |
−0.647*** (0.130) |
−0.049*** (0.010) |
−0.036*** (0.009) |
||||||||||
| 1.344** (0.516) |
0.808* (0.466) |
0.071 (0.043) |
0.029 (0.041) |
|||||||||||
| Endline mean in control | 635 | 634 | 635 | 628 | 635 | 635 | 627 | 635 | 634 | 635 | 628 | 635 | 635 | 627 |
| Observations | 0.074 | 0.127 | 0.077 | 0.093 | 0.131 | 0.085 | 0.187 | 0.057 | 0.092 | 0.066 | 0.075 | 0.090 | 0.062 | 0.136 |
| P-value wild bootstrap | 0.024 | 0.030 | 0.034 | 0.061 | 0.068 | 0.026 | 0.155 | 0.038 | 0.054 | 0.084 | 0.089 | 0.099 | 0.041 | 0.367 |
| % impact expl. by channel | 14% | 9% | 16% | 26% | 7% | 46% | 15% | 22% | 22% | 24% | 6% | 65% | ||
Notes: OLS estimates. Robust standard errors clustered at the village cluster level in parentheses (29 clusters). ***, ** and * indicate significance at 1%, 5% and 10% level, respectively. Regressions include baseline values of endogenous channel indicators as well as the following controls: dummies for traditional authority strata, baseline youth characteristics (age dummies from 14 to 19, single or double orphan status), and baseline household characteristics (whether the caregiver is female, whether she/he is literate, and household size). baseline youth characteristics (age dummies from 14 to 19, single or double orphan status), and baseline Allo number of clusters using the wild bootstrap procedure. All regressions are weighted according to the probability of youth being selected for interview at baseline.
School attendance is associated with better mental health and accounts for about 14–15 percent of the total ITT impact on both outcomes. The consumption channel explains 9 percent of the program impact on CES-D and 22 percent of the impact on the likelihood of depressive symptoms. While none of the three indicators of the consumption channel significantly affect CES-D scores (column 3), the coefficient on any expenditure on girl’s clothing is negative and significant for depressive symptoms. This finding is consistent with qualitative interviews conducted among program participants who described the shame and stigma of poverty that effectively denied the material needs for school participation and limited opportunities for socializing (Rock et al., 2016).
While the caregiver’s life satisfaction measure appears to be irrelevant, the caregiver’s stress levels are strongly and significantly associated with girls’ mental health. The caregiver channel explains 16 (22) percent of the overall program impact on CES-D (depressive symptoms). This finding, suggesting a channel of intergenerational transmission of depressive symptoms, is in accordance with the psychology literature documenting that parental mental health affects children’s—particularly daughters’—mental health.
The social support channel explains the largest share of ITT impact (26 and 24 percent for CES-D and depressive symptoms, respectively). A higher index of perceived social support substantially improves females’ mental health (columns (5) and (11), with coefficients significant at the 1% level). The Appendix shows that three individual items are negatively and significantly associated with CES-D and depression, specifically “can share joys and sorrows with friends”, “can get support from family”, and “family is willing to help me make decisions.”
Finally, involvement in casual (ganyu) labor is significantly associated with CES-D scores, however the fraction of explained program impact is comparatively small (7 percent for CES-D and 6 percent for the binary variable). The combination of potential pathways accounts for 46 and 65 percent of the program impacts on the summed CES-D score and the likelihood of being depressed, respectively. After controlling for the pathways, the “net” treatment effects on the summed CES-D and symptoms of depression are no longer statistically significant.
5. Discussion and conclusions
Mental health is recognized as a critical issue during transitions from adolescence to adulthood. Poor mental health during adolescence can have detrimental effects on psychosocial development and, particularly in resource poor settings, perpetuate poverty. Moreover, mental illness is a leading cause of adolescent death and disability-adjusted life years (DALYs) globally, with the highest burdens in low-income countries (Kassebaum et al., 2017). Further, in 2015, the World Health Organization released “Health for the World’s Adolescents” which indicated that suicide was the number one cause of death for adolescent girls aged 15 to 19 (WHO, 2015). Considering growing youth populations and the potential opportunity to reap a demographic dividend, ensuring that adolescents transition to adulthood in an environment that minimizes mental health concerns appears to be of particularly pressing concern in SSA.
We find that Malawi’s unconditional SCTP reduces depressive symptoms among all youth, but especially among females. We believe that these findings are important for at least two reasons. First, our findings further underline the potential of unconditional cash grants, which are increasingly used as part of national social protection systems in SSA, to improve youth mental wellbeing when implemented at scale. As mentioned in the introduction, our findings are in line with three other studies examining the effects of cash transfers on youth mental health in Kenya, Malawi and South Africa (Baird et al., 2013; Kilburn et al., 2016, 2018a). All three programs resulted in improvements in mental health (Kilburn et al., 2018a only for the poorest households), despite differences in the targeting criteria, program features such as transfer amounts, and length of exposure to the program. We are therefore confident that our findings have an important degree of external validity in development settings. We conclude that in SSA large-scale, unconditional cash transfer programs – which typically aim to reduce household poverty and vulnerability – have the potential to improve youth mental health.
Second, the extensive data on which we rely enable us to shed more light on differential impacts by gender and on the pathways through which poverty and mental health are connected – including the mental wellbeing of caregivers, social support from family members and friends, and participation in hard and unpleasant informal labor – all important issues if we are to break the cycle of poverty and poor mental health. In particular, we confirm the importance of caregiver stress and quality of life and how improvements in caregiver mental wellbeing matter for youth mental health. This finding lends weight to the hypothesis that poor mental health is transmitted intergenerationally, and may negatively affect future generations through adverse family environments. These dynamics may be particularly important in understanding the mechanisms through which economic transfers could have beneficial impacts on youth mental health in fragile settings, including those in refugees and in post-conflict settings.
A critical question for future programming is what design components are essential or important for realizing impacts. While our study does not allow us to answer this question in an experimental way, by comparing findings with similar studies in Table 1, some patterns emerge. First, the impacts of unconditional programs appear to be – on average – stronger than conditional programs, the latter potentially resulting in stress as household income depends on youth compliance with program conditions (Baird et al., 2013). In addition, the relative poverty levels of the target group appear to matter. For example, the only study not finding average impacts (but impacts on girls in poorest households) was from a program which was not poverty-targeted, and rather sampled from girls already attending secondary school (Kilburn et al., 2018a). Although not studied explicitly in this evaluation, it is also possible that sensitization and messaging around program purpose, target recipient (guardian or youth), transfer size, duration and payment regularity may be important in certain settings—the former particularly with respect to managing expectations for participants as well as reducing potential for negative impacts on non-beneficiaries.
There are some limitations to the study worth mentioning. One clear limitation is the baseline imbalance of mental health indicators among males, which may have hampered our ability to detect program effects. However, our analysis controls for this difference, and thus there may be other important reasons why we find gender differences in our results due to strength of the cash transfer to affect gender-specific drivers of poor mental health. In addition, although the CES-D 10 has been widely used in the SSA setting, and validation exercises indicate that there is high reliability, there is a chance that a measure further adapted to the setting or biometric measurements would have yielded different results (Kilburn et al., 2018b). And importantly, as we do not have information on the mental wellbeing of youth in ineligible households, we cannot examine whether their mental health was negatively affected (a pattern documented by Baird et al., 2013 and Haushofer et al., 2015).
Finally, further research is needed to understand program design differences, as well as longer-term program effects. For example, while we now have accumulated evidence on cash transfers in SSA on youth mental health, we know less about the effects of broader social protection instruments, including public works programs or insurance mechanisms. A key issue for future research is understanding the time dynamics surrounding impacts. Although we find that impacts after one year of cash transfers (midline) are approximately 2/3 of the endline total impact, an indication of accumulated impacts over time, further research would help unpack whether effects of sustained delivery of programs over prolonged periods of time compound or dissipate. For example, while shorter-term programs of 12-months have shown significant reductions in depressive symptoms similar in magnitude to our study, these impacts were found to dissipate after the transfers ended (Baird et al., 2013). Yet, despite evidence suggesting impacts could be tied to transfer periods, due to the large number of beneficiaries supported by cash programming, there could be substantial gains on the population level. For example, two recent studies of conditional cash transfer programs in Brazil and Indonesia reduced suicide rates, in the latter case by 7.2–9.4 percent among poor populations (Alves et al., 2018; Christian and Roth, 2016). This suggests that the longer-term population level mental health improvements can be substantive.
Supplementary Material
Acknowledgements
The authors wish to recognize the contributions of several parties, without which this study would not have been possible. Our appreciation goes to the Government of Malawi for their supportive engagement with the evaluation team, and for their time and intellectual contributions, specifically Dr. Mary Shawa, Dr. Esmie Kainja, Mr. Laurent Kansinjiro, Mr. Charles Chabuka and Mr. Gideon Kachingwe of the Ministry of Gender, Children, Disabilities and Social Welfare, Mr. Harry Mwamlima of the Ministry of Finance, Economic Planning and Development, as well as the District Commissioner’s Offices of Salima and Mangochi. We would also like to acknowledge Chantal Elmont of Ayala Consulting, who continually supported the evaluation team by providing vital information on the implementation of the SCTP. Many thanks to the research team CSR for their exceptional work. We thank the European Union, the German Government through KfW, Irish Aid, FAO, the International Initiative for Impact Evaluation (3ie), the UK Department for International Development and UNICEF Malawi for their financial contributions and stakeholder support for the study.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2019.01.037.
References
- Alves FJO, Machado DB, Barreto ML, 2018. Effect of the Brazilian Cash Transfer Programme on Suicide Rates: a Longitudinal Analysis of the Brazilian Municipalities. Social Psychiatry and Psychiatric Epidemiology (in press). [DOI] [PubMed] [Google Scholar]
- Baird S, de Hoop J, Özler B, 2013. Income shocks and adolescent mental health. J. Hum. Resour 48 (2), 370–403. [Google Scholar]
- Cameron AC, Gelbach JB, Miller DL, 2008. Bootstrap-based improvements for inference with clustered errors. Rev. Econ. Stat 90 (3) 414–27. [Google Scholar]
- Carolina Population Center (CPC), 2014. Malawi social cash transfer Programme baseline evaluation report CPC: University of North Carolina at Chapel Hill (UNC). https://transfer.cpc.unc.edu/wp-content/uploads/2015/09/Malawi-SCTP-Baseline-Report.pdf. [Google Scholar]
- Carolina Population Center (CPC), 2016a. Malawi social cash transfer Programme endline impact evaluation report CPC: University of North Carolina at Chapel Hill (UNC). https://transfer.cpc.unc.edu/wp-content/uploads/2015/09/Malawi-SCTP-Endline-Report_Final.pdf. [Google Scholar]
- Carolina Population Center (CPC), 2016b. Impact of the Malawi social cash transfer Programme on household resilience CPC: University of North Carolina at Chapel Hill (UNC). https://transfer.cpc.unc.edu/wp-content/uploads/2015/09/Malawi-Endline-Resilience-Aug-2016.pdf. [Google Scholar]
- Christian C, Roth C, 2016. Can Cash Transfers Prevent Suicides? Experimental Evidence from Indonisia. Working Paper
- Cohen S, Kamarck T, Mermelstein R, 1983. A global measure of perceived stress. J. Health Soc. Behav 24 (4), 385–396. [PubMed] [Google Scholar]
- de Hoop J, Groppo V, Handa S, 2019. Cash Transfers, Microentrepreneurial Activity, and Child Work: Evidence from Malawi and Zambia. World Bank Econ. Rev (in press) [DOI] [PMC free article] [PubMed]
- Diener ED, Emmons RA, Larsen RJ, Griffin S, 1985. The satisfaction with life scale. J. Pers. Assess 49 (1), 71–75. [DOI] [PubMed] [Google Scholar]
- Flores CA, Flores-Lagunes A, 2009. Identification and Estimation of Causal Mechanisms and Net Effects of a Treatment under Unconfoundedness. IZA Discussion Papers 4237 Institute for the Study of Labor (IZA). [Google Scholar]
- Haushofer J, Fehr E, 2014. On the psychology of poverty. Science 344, 862–867. [DOI] [PubMed] [Google Scholar]
- Haushofer J, Reisinger J, Shapiro J, 2015. Your Gain Is My Pain: Negative Psychological Externalities of Cash Transfers. Working Paper
- Imani K, Keele L, Tingley D, 2010. A general approach to casual mediation analysis. Psychol. Methods 15 (4), 309. [DOI] [PubMed] [Google Scholar]
- Kassebaum N, Kyu HH, Zoeckler L, et al. , 2017. Child and adolescent health from 1990 to 2015: findings from the global burden of diseases, injuries and risk factors 2015 study. JAMA Pediatrics 171, 573–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keele L, Tingley D, Yamamoto T, 2015. Identifying mechanisms behind policy interventions via causal mediation analysis. J. Pol. Anal. Manag 34 (4), 937–963. [Google Scholar]
- Kilburn K, Thirumurthy H, Halpern CT, Pettifor A, Handa S, 2016. Effects of a large-scale unconditional cash transfer program on mental health outcomes of young people in Kenya. J. Adolesc. Health 58 (2), 223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilburn K, Hughes JP, MacPhail C, Wagner RG, Gomez-Olive FX, Kahn K, Pettifor A, 2018a. Cash transfers, young women’s economic well-being and HIV Risk: evidence from HPTN 068. AIDS. Behav (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilburn K, Prencipe L, Hjelm L, Peterman A, Handa S, Palermo T, 2018b. Examination of performance of the center for epidemiological studies depression scale short form 10 among African youth in poor, rural households. BMC Psychiatry 18 (201). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, Knapp M, Patel V, 2011. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet 378, 1502–1514. [DOI] [PubMed] [Google Scholar]
- McKenzie D, 2012. Beyond baseline and follow-up: the case for more T in experiments. J. Dev. Econ 99, 210–221. [Google Scholar]
- Patel V, Flisher AJ, Hetrick S, McGorry P, 2007. Mental health of young people: a global public-health challenge. Lancet 369, 1302–1313. [DOI] [PubMed] [Google Scholar]
- Patel V, Kleinman A, 2003. Poverty and common mental health disorders in developing countries. Bull. World Health Organ 81 (8), 609–615. [PMC free article] [PubMed] [Google Scholar]
- Rock A, Barrington C, Abdoulayi S, Tsoka M, Mvula P, Handa S, 2016. Social networks, social participation, and health among youth living in extreme poverty in rural Malawi. Soc. Sci. Med 170, 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roodman D, 2015. BOOTTEST: Stata module to provide fast execution of the wild bootstrap with null imposed https://ideas.repec.org/c/boc/bocode/s458121.html.
- World Health Organization (WHO) (WHOQOL Group), 1998. The World health organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc. Sci. Med 46 (12), 1569–1585. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO), 2015. Health for the World’s Adolescents, a Second Chance in the Second Decade World Health Organization, Geneva. http://apps.who.int/adolescent/second-decade/, Accessed date: July 2017. [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, Farley GK, 1988. The multidimensional scale of perceived social support. J. Pers. Assess 52 (1), 30–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.