Abstract
Background:
Since 2001, San Francisco has experienced a sustained syphilis epidemic that has been nearly exclusively limited to men who have sex with men. We examined the characteristics associated with changes in the syphilis epidemic in San Francisco.
Methods:
All primary and secondary (P&S) syphilis cases reported to the San Francisco Department of Public Health between 2001 and 2011 were examined using joinpoint analysis to identify periods within the broader epidemic. Characteristics of the index cases were compared across the periods using χ2 statistics and t tests.
Results:
Three distinct periods were identified, an acute increase, decline, and then period of resurgence. In the most recent period of resurgence, compared with earlier periods, patients with P&S syphilis were more likely to have a prior syphilis infection, were older, were more likely to meet partners online, and were more likely to have a partner from outside San Francisco.
Conclusions:
In an analysis of 11 years of P&S syphilis data, several factors were associated with declines or resurgences. Innovative prevention measures are needed to reduce syphilis morbidity among men who have sex with men.
BACKGROUND
Between 1999 and 2010, the number of primary and secondary (P&S) syphilis cases reported annually to the San Francisco Department of Public Health rose from 29 to 373, an increase of 1186%.1 A concurrent increase in reported cases was seen in southern California,2,3 and shortly thereafter, similar trends became apparent nationally.4,5 Before 1999, syphilis transmission was largely associated with exchanges of sex for drugs or money and crack cocaine use.6 The rise in syphilis that began in the late 1990s was associated with increased transmission among men who have sex with men (MSM), many of whom were HIV infected and also met their sex partners online.7 As the MSM syphilis epidemic spread across the United States, new and innovative prevention and intervention efforts were needed.
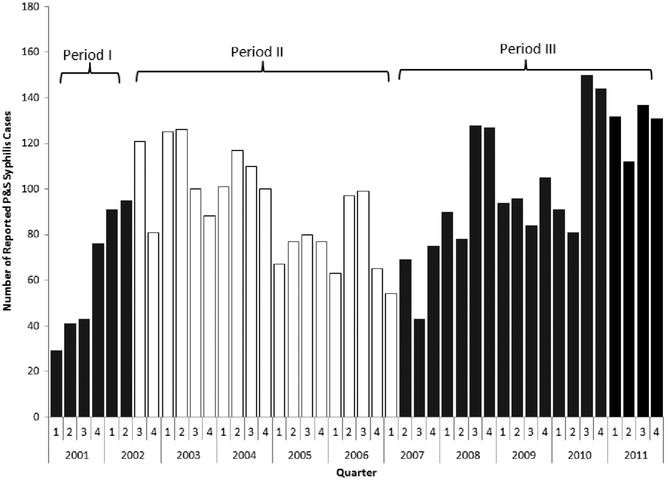
Over the past decade, San Francisco has developed and implemented a number of interventions across many domains in an effort to reduce syphilis morbidity among the city’s MSM population. These efforts include the development of Internet partner notification protocols,8 inSPOT (anonymous online partner notification),9 online syphilis testing (www.stdtest.org),10 and several social marketing campaigns.11,12 Despite these novel programs and declines in syphilis seen between 2003 and 2007 (Fig. 1), reported P&S syphilis began to once again increase later in 2007 and continued to rise through 2011.
Figure 1.
Reported P&S syphilis cases by quarter, San Francisco, 2001–2011.
In their seminal work on sexually transmitted disease (STD) epidemiology, Wasserheit and Aral13 describe how approaches to prevention may differ in distinct epidemic phases. Others have explored the ways in which transmission dynamics may change over the course of these phases, primarily for HIV14,15 An examination of epidemic phases was explored in Baltimore by Cunnigham and colleagues; however, the epidemic examined was almost exclusively among heterosexuals.16 Here we build on the existing foundation of examining epidemic phases and explored the epidemiologic characteristics of P&S syphilis in San Francisco from 2001 to 2011 in an attempt to elucidate what may have precipitated the decline and subsequent resurgence.
METHODS
Epidemiologic Data
All reactive serologic tests for syphilis and clinical diagnoses of syphilis are required to be reported to the local health authority as per California Public Health law. We examined all reported P&S syphilis cases among San Francisco residents from 2001 through 2011. Cases of P&S syphilis reported within 30 days of a prior report for the same individual are considered duplicate case reports, and only the first report was included in the analysis. If cases were reported with an intervening interval greater than 30 days, these were considered separate episodes of P&S syphilis. Although we cannot rule out the possibility of a treatment failure, it is unlikely because all cases were treated with Centers for Disease Control and Prevention–recommended treatment regimens.17 Persons infected with P&S syphilis multiple times during the 11 years of data were included multiple times.
Suspected or confirmed cases of P&S syphilis reported to the San Francisco Department of Health were investigated by trained field staff. These investigations included an interview with the index patient, assurance of appropriate treatment, and elicitation of sexual partners who may have been exposed to syphilis. Data were collected in a standardized electronic interview system. Sociodemographics, substance use, sexual behaviors, and HIV serostatus of the index patients were collected through interviews by field staff. Repeat syphilis was determined through review of any prior reports of early syphilis to San Francisco STD Prevention and Control. HIV status was based on index self-identification. The residential address of the patient was geocoded and assigned to locally defined neighborhood boundary files using MapMarker (Piney Bowes, Troy, NY) and SAS v9.3 (SAS Institute, Cary, NC). Index patients residing in census tracts that corresponded to the Castro neighborhood, where large numbers of gay-identified MSM reside, were coded as Castro residents. Numbers and types of sexual behavior were assessed in the critical period (3 months for primary cases and 6 months for secondary cases) in accordance with standard protocols.18
Data on partners were obtained through the interview of the index and partner service interviews for named partners. Any partners listed with an address outside San Francisco were considered out of jurisdiction (OOJ). We also calculated the average number of partners named per index for each of the 3 periods in these analyses.
In addition, data on P&S syphilis cases from Bay Area counties surrounding San Francisco were obtained from the California Department of Public Health, STD Control Branch. For each of the identified periods, the total number of patients with P&S syphilis reported in the Bay Area, excluding San Francisco, was obtained, as well as the proportion of these reported patients that were initially identified or interviewed in San Francisco. The Bay Area counties examined include Alameda, including the separate jurisdiction of the city of Berkeley, Contra Costa, Marin, Napa, San Mateo, Santa Clara, Solano, and Sonoma counties.
The San Francisco Department of Public Health Laboratory supports syphilis testing in a wide range of sites throughout San Francisco. These include the municipal STD clinic, the gay men’s health center in the Castro neighborhood, several community-based organizations, the San Francisco city jail, several clinics serving adolescents and homeless persons, and the San Francisco Department of Public Health Primary Care clinics. Data on the total number of Venereal Disease Research Laboratory (VDRL) serologic tests conducted by the Public Health Laboratory during the analytic period were also examined to determine if the increases seen in P&S syphilis case reports may be a result of increased access to syphilis screening. Although the Public Health Lab does not perform testing for all providers in San Francisco, their catchment is large and the clinical sites using the Public Health Laboratory have remained largely unchanged since 2000.
This study was considered exempt from human subjects considerations in accordance with the Code of Federal Regulations, Title 45, because these data were deidentified and were undergoing retrospective analysis for public health evaluation and improvement.
Identification of Changes in Reported P&S Syphilis in San Francisco
Epidemic curves by quarter and month were created. To determine inflection points (or points where the epidemic trajectory changes) in the local epidemic, Joinpoint software was used.19 Briefly, joinpoint analysis is based on a Monte Carlo Permutation method that identifies a model with the fewest number of inflection points, or joinpoints. The maximum number of joinpoints is determined a priori, and the software starts with 0 joinpoints and tests whether additional joinpoints (up to the preset maximum) improve model fit. Joinpoint analyses were conducted on the quarterly and monthly P&S syphilis count data with a maximum of 4 joinpoints set a priori. Both analyses produced similar results; only the results of the quarterly P&S count data are presented here. To examine changes in the epidemiologic characteristics of the 3 periods, the characteristics of the index patients, their partners, other Bay Area morbidity, and VDRL testing volume were compared across the 3 periods. Comparisons were evaluated using χ2 statistics for categorical data and t tests for continuous data.
RESULTS
Between January 1, 2001–June 30, 2002, and December 31, 2011, 4090 cases of P&S syphilis were reported among San Francisco residents. Based on the results of the joinpoint analysis, inflection points were determined and 3 distinct epidemiologic periods were examined. The epidemic in San Francisco is characterized by a period of increasing case reports (period I: January 1, 2011–June 30, 2002) and then a decline in case reports (period II: July 1, 2002–March 31, 2007), followed by a subsequent increase in case reports (period III: April 1, 2007–December 31, 2011).
Comparisons of Initial Increase (Period I) and Subsequent Declines (Period II) in P&S Syphilis Morbidity
A total of 290 and 1380 patients with P&S syphilis were reported in periods I and II, respectively (Table 1). In both periods, approximately one third of these patients were reported in the primary stage and more than 90% were among MSM. No statistically significant differences were seen with respect to race/ethnicity, age, or HIV serostatus between the 2 periods. However, patients with P&S reported in period II were significantly more likely to have had a history of syphilis (P < 0.01). Patients with primary and secondary syphilis were also more likely to be diagnosed in a private care setting in period II compared with period I (P = 0.01). No difference was seen regarding residence in the Castro neighborhood between the 2 periods. Approximately 85% of the reported patients were interviewed in both periods (P = 0.43). Period II also saw a larger proportion of index patients refusing partner services interviews (7.3% vs. 4.0%, P = 0.04); no other differences were seen regarding index interview dispositions between periods I and II. Because substance use data were not consistently collected during the index interview in period I, comparisons were not conducted. However, in period II, the period of decline, patients with P&S were less likely to report meeting partners in bathhouses or sex clubs and were more likely to report meeting partners through the Internet. In both periods, the proportion of patients who had more than 5 critical period partners were similar, as were the proportion of patients who had contact with sex work (as either a client or sex worker). However, in period I, patients with P&S syphilis were more likely to report having a female sex partner during the critical period. Although index patients naming any partners were more likely to have an OOJ partner named in period II, compared with period I, the increase was not statistically significant. The average named partners per index did not differ between periods I and II. However, the proportion of Bay Area morbidity initially identified in San Francisco declined significantly between periods I and II (P = 0.04).
TABLE 1.
Characteristics of Syphilis Cases Among Men who Have Sex With Men, San Francisco 2001–2011
| Periods |
P Values for Period Comparisons |
|||||
|---|---|---|---|---|---|---|
| Patient Characteristics | Period I: January 1, 2001–June 30, 2002, n (%) |
Period II: July 1, 2002–March 31, 2007, n (%) |
Period III: April 1, 2007–December 31, 2011, n (%) |
Period I vs. Period II |
Period II vs. Period III |
Period I vs. Period III |
| Total | 290 (8.9) | 1380 (42.5) | 1574 (48.5) | |||
| Average no. P&S cases per month | 16.1 | 24.2 | 27.6 | |||
| Stage | 0.89 | 0.11 | 0.47 | |||
| Primary | 100 (34.5) | 469 (34.0) | 580 (36.9) | |||
| Secondary | 190 (65.5) | 911 (66.0) | 994 (63.2) | |||
| Repeat cases | <0.01 | <0.01 | <0.01 | |||
| No | 271 (93.5) | 1148 (83.2) | 1182 (75.1) | |||
| Yes | 19 (6.6) | 232 (16.8) | 392 (24.9) | |||
| Sex* | 0.14 | 0.26 | 0.03 | |||
| MSM | 262 (90.3) | 1282 (92.9) | 1479 (94.0) | |||
| MSW | 26 (9.0) | 78 (5.7) | 57 (3.6) | |||
| Female | 2 (0.7) | 11 (0.8) | 25 (1.6) | |||
| Transgender | 0 | 8 (0.6) | 11 (0.7) | |||
| Unknown | 0 | 1 (0.1) | 2 (0.1) | |||
| Race/ethnicity | 0.61 | 0.01 | 0.98 | |||
| White | 181 (62.4) | 885 (64.1) | 963 (61.2) | |||
| Hispanic | 54 (18.6) | 243 (17.6) | 279 (17.7) | |||
| Black | 26 (9.0) | 93 (6.7) | 163 (10.4) | |||
| API | 22 (7.6) | 114 (8.3) | 129 (8.2) | |||
| Other | 4 (1.4) | 16 (1.2) | 21 (1.3) | |||
| Unknown | 3 (1.0) | 29 (2.1) | 19 (1.3) | |||
| Age, y | 0.11 | <0.01 | <0.01 | |||
| ≤29 | 38 (13.1) | 208 (15.1) | 251 (16.0) | |||
| 30–39 | 142 (49.0) | 569 (41.2) | 465 (29.5) | |||
| 40–49 | 85 (29.3) | 451 (32.7) | 598 (38.0) | |||
| 50+ | 25 (8.6) | 152 (11.0) | 260 (16.5) | |||
| HIV status† | 0.58 | 0.56 | 0.81 | |||
| Positive | 160 (55.2) | 760 (55.1) | 888 (56.4) | |||
| Negative | 66 (22.8) | 345 (25.0) | 382 (24.3) | |||
| Never tested or data not available | 53 (18.3) | 233 (16.9) | 268 (17.0) | |||
| Unknown on day of syphilis but subsequently tested positive | 11 (3.8) | 42 (3.0) | 36 (2.3) | |||
| Diagnosing provider | ||||||
| STD clinic | 101 (34.8) | 487 (35.3) | 468 (29.5) | 0.89 | 0.01 | 0.10 |
| Gay men’s health center | 0 | 73 (5.3) | 278 (17.7) | — | <0.01 | — |
| HIV care clinic | 13 (4.5) | 61 (4.4) | 96 (6.1) | 1.00 | 0.05 | 0.34 |
| HMO | 10 (3.5) | 116 (8.4) | 69 (4.4) | 0.01 | <0.01 | 0.53 |
| Other | 166 (57.2) | 643 (46.6) | 666 (42.3) | 0.01 | 0.02 | <0.01 |
| Castro neighborhood residence | 54 (18.6) | 300 (21.7) | 293 (18.6) | 0.27 | 0.04 | 1.00 |
| Interviewed patients | 247 (85.2) | 1147 (83.1) | 1321 (83.9) | 0.43 | 0.58 | 0.66 |
| Index patient disposition | ||||||
| OOJ | 0 | 1 (0.1) | 6 (0.4) | — | 1.00 | — |
| Partial interview | 0 | 2 (0.2) | 42 (2.7) | — | <0.01 | — |
| Refused | 11 (4.0) | 100 (7.3) | 94 (6.0) | 0.04 | 0.18 | 0.17 |
| Unable to locate | 30 (10.3) | 122 (8.9) | 138 (8.8) | 0.43 | 0.95 | 0.37 |
| Other | 2 (0.7) | 10 (0.7) | 15 (1.0) | 1.00 | 0.55 | 1.00 |
| Among interviewed index patients | ||||||
| Drug use (last 12 mo) | ||||||
| Poppers | 88 (7.7) | 270 (20.4) | — | <0.01 | — | |
| Meth | 235 (20.5) | 353 (26.7) | — | <0.01 | — | |
| Cocaine | 58 (5.1) | 128 (9.7) | — | <0.01 | — | |
| ED medicine | 34 (3.0) | 266 (20.1) | — | <0.01 | — | |
| IDU | 12 (4.9) | 63 (5.5) | 113 (8.6) | 0.76 | 0.01 | 0.05 |
| Met partners at bathhouse or sex club | 70 (28.3) | 215 (18.7) | 208 (15.8) | 0.01 | 0.05 | <0.01 |
| Met partners on the Internet | 65 (26.3) | 461 (40.2) | 649 (49.1) | <0.01 | <0.01 | <0.01 |
| Sex, critical period | ||||||
| >5 male partners | 110 (44.9) | 454 (40.7) | 504 (40.6) | 0.15 | 0.48 | 0.07 |
| Female partners | 22 (9.0) | 50 (4.5) | 61 (4.9) | 0.01 | 0.77 | 0.01 |
| Sex work | 0 | 5 (0.5) | 7 (0.6) | — | 0.78 | — |
| Dispositions for partners in named time frame | ||||||
| Index named any OOJ partners, among indexes who named at least 1 partner | 67 (45.0) | 380 (53.0) | 435 (55.7) | 0.09 | 0.30 | 0.02 |
| Mean no. named partners per index | 2.21 | 2.3 | 2.8 | 0.70 | 0.01 | 0.08 |
| P&S syphilis morbidity from Bay Area counties (excluding San Francisco) | ||||||
| Reported P&S syphilis | 126 | 751 | 1177 | |||
| Bay Area P&S syphilis initially identified in San Francisco | 20 (15.9) | 71 (9.5) | 130 (11.1) | 0.04 | 0.29 | 0.11 |
Comparison of MSM vs. non-MSM.
Comparison of HIV positive vs. HIV negative.
ED indicates emergency department; meth, methamphetamines; MSW, men who have sex with women.
Comparisons of Declines (Period II) and Resurgence (Period III) in P&S Syphilis Morbidity
After a period of declining morbidity, P&S syphilis began to increase again in April 2007 (period III). In comparing index patients with P&S in period II and III, no differences were seen regarding the distribution of stage of disease, sex/sexual identity, or HIV serostatus. Patients with P&S syphilis diagnosed in period III were more likely to have had a history of syphilis, were less likely to be white, and were more likely to be older compared with patients with P&S syphilis reported in period II (all P < 0.05). Moreover, patients diagnosed during the resurgence (period III) were also more likely to be diagnosed outside the municipal STD clinic but were less likely to reside in the Castro neighborhood. The proportion of index patients interviewed did not differ between periods II and III. In the period of resurgence, patients with P&S syphilis that were interviewed were more likely to report using poppers, methamphetamines, cocaine, erectile dysfunction medications, and injection drug use (all P < 0.05). Moreover, the proportion of patients who reported meeting sex partners online increased (P < 0.01), whereas the proportion of meeting partners at bathhouses or sex clubs declined (P = 0.05). No differences were seen between periods II and III regarding numbers and types of sex partners. The average named partners per index during the resurgence period increased from 2.3 to 2.8 (P = 0.01); no significant difference was seen in terms of OOJ partners. The proportion of Bay Area P&S syphilis that was initially identified in San Francisco did not differ between periods II and III.
Comparisons of Periods of Increases (Periods I and III) in P&S Syphilis Morbidity
We compared the characteristics of the patients with P&S syphilis diagnosed during the 2 periods of increased morbidity to help elucidate what may have driven the most recent resurgence. No differences were seen in the stage of disease, race/ethnicity, or HIV serostatus when periods I and III were compared. However, the proportion of repeat cases of syphilis increased from 6.6% to 24.9% (P < 0.01) and the proportion of cases among MSM increased from 90.3% to 94.0% (P = 0.03). In addition, patients with P&S syphilis diagnosed in period III were older than those patients diagnosed in period I (P < 0.01). In the later period, a smaller percentage of patients with P&S syphilis were diagnosed outside the 4 most common providers (Table 1) (42.3% vs. 57.2%, P < 0.01), yet no difference was seen in the proportion of patients who resided in the Castro neighborhood. During the resurgence period (period III), a smaller proportion of patients reported meeting sex partners in bathhouses or sex clubs and a larger proportion reported meeting partners online, compared with period I (P < 0.01 for both comparisons). Furthermore, in period III, patients with P&S syphilis were significantly less likely to report any female partners (P = 0.01) and slightly less likely to report more than 5 male partners, although this finding was of borderline significance (P = 0.07). Although the average number of named partner per index was higher in the resurgence period (period III) compared with period I1, the difference was of borderline significance (P = 0.08). No difference was observed in the proportion of patients with syphilis in Bay Area identified in San Francisco; however, the proportion of index patients who had an OOJ partner was significantly higher in period III compared with period I (P = 0.02).
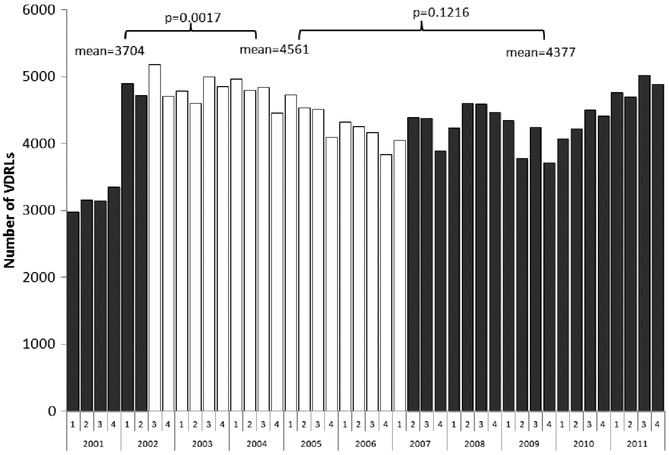
VDRL Testing Conducted by the San Francisco Public Health Laboratory
The quarterly testing volume of VDRLs conducted by the Public Health Laboratory is shown in Figure 2. The average quarterly test volume increased from 3704 in period I to 4561 in period II (P = 0.01). A small decline in quarterly testing volume was seen from periods II to III; however, the difference between these 2 periods was not statistically significant (P = 0.12).
Figure 2.
VDRL testing from San Francisco Public Health Laboratory, 2001–2011.
DISCUSSION
In our analysis of more than a decade of reported P&S syphilis in San Francisco, we identified 3 distinct periods of the modern epidemic. The first period was characterized by a sharp increase in cases; the second period, a gradual decline,; and the third period, a resurgence of cases. Throughout the 11 years of analytic data, the overall characteristics of the populations affected by syphilis have been strikingly consistent —older, mostly white, and MSM, of which approximately 60% are HIV infected. However, we identified changes in how the epidemic crossed jurisdictional boundaries over the period. Our intention was to explore whether changes may have occurred during the 3 periods in an effort to understand what may have facilitated the recent increase and to provide insights into prevention planning and intervention design.
Data on syphilis serologic testing volume suggests that increases seen in case reports are not likely an artifact of improved surveillance. The volume of serologic tests conducted by the San Francisco Public Health Laboratory increased sharply in the beginning of the current epidemic but has remained stable throughout periods II and III. Although the San Francisco Public Health Laboratory does not process specimens for all providers in San Francisco, it has consistently supported the same clinical sites and was the laboratory for serologic testing for approximately 50% of P&S patients diagnosed throughout the analytic period. Thus, although not exhaustive, we would expect that any increase in community-wide screening would be seen in the sentinel data from the Public Health Laboratory. Community-based samples of MSM in San Francisco collected by the STOP AIDS Project from 2003 to 2009 show stable proportions of HIV-uninfected MSM (~50%) and HIV-infected MSM (~70%) who reported being tested for syphilis in prior 6 months (J. Hecht, personal communication; data not shown).
Several factors may have facilitated these increases seen in period III. Over the course of the 11 years we examined, the proportion of patients with syphilis with a prior syphilis infection increased significantly from 6.6% in period I to 24.9% in period III. These data suggest that a small but important core group of men with multiple episodes of syphilis may be sustaining ongoing syphilis transmission. Analyses from several groups have suggested the potential importance of syphilis repeat infections.20-22 Identifying effective approaches to reducing syphilis reinfections may impact sexual networks that facilitate local endemic disease transmission.
Over the analytic period, the clinical site of diagnosis for P&S syphilis cases has shifted slightly. The municipal STD clinic remained the single largest diagnosing site for P&S syphilis. However, the gay men’s health center and HIV care site have been diagnosing an increasingly larger proportion of new syphilis diagnoses. These data highlight the myriad of clinical locations that offer syphilis screening for MSM in San Francisco. Given that the volume of serologic tests for syphilis has remained relatively stable in recent years, it is likely that MSM in San Francisco are seeking services in more diverse settings but are perhaps not seeking services with greater frequency.
Although few factors differed between the 3 periods examined, a few notable findings deserve discussion. The proportion of patients with P&S syphilis who reported meeting partners in bathhouses or sex clubs declined over time. Men who have sex with men in San Francisco may have changed the locus of sex partner recruitment from physical locations to virtual Internet-based locations. Furthermore, in period III, the proportion of patients who named any sex partners who had at least 1 OOJ partner was significantly higher than that in period I. These data suggest that a significant amount of syphilis may be imported to and exported from San Francisco. Furthermore, data from the surrounding Bay Area counties show that a sizeable amount of Bay Area morbidity is initially identified in San Francisco (although this proportion was relatively stable for 11 years). This analysis highlights the need to think more broadly about regional approaches to syphilis control because the patients we serve may not see jurisdictional boundaries in the same way as local health departments.
Over the course of 11 years we explored, San Francisco Department of Public Health STD Prevention and Control have successfully implemented a number of notable interventions to prevent syphilis. These included the several social marketing campaigns including the Healthy Penis campaign (2002–2003, 2009), online syphilis testing for high-risk MSM (STDtest. org, 2003), an online anonymous partner notification system (inSPOT, 2004), increased community outreach within affected neighborhoods in San Francisco, community-based syphilis testing, and extensive partnering with community clinicians to increase access to syphilis screening, particularly among HIV-infected MSM in care. The overall impact of this collection of interventions on the course of the syphilis epidemic in San Francisco is unknown and is beyond the scope of this analysis. However, it is important to note that over this period, health department–initiated structural and cultural changes including normalizing routine syphilis screening (especially for HIV-infected MSM, outreach to private provider who serve MSM patient populations, and social marketing around syphilis) were occurring among MSM in San Francisco, which may have had an impact of the epidemic trajectory.
A number of additional limitations exist in the analysis presented. First, data are available only on reported syphilis cases; if the case is not investigated, risk behavior data are not available. However, because reactive syphilis serologies are reportable in California and the Public Health laboratory conducts a significant amount of citywide testing, we believe that few cases were missed. In addition, a similar proportion of reported P&S syphilis cases were investigated in each of the 3 periods. Data on the total syphilis testing volume citywide were not available because only reactive serologic tests are required to be reported to the health department. Patients or partners residing outside San Francisco are not interviewed by staff from the San Francisco STD program, which may have resulted in missing sexual partner network connections.
Over the course of 11 years, P&S syphilis has waxed and waned in San Francisco, yet the populations most affected have remained largely stable. Subtle changes were identified in terms of locus of care and Internet use in partner recruitment. However, these changes may have been secular in nature and reflect changes in the larger culture of San Francisco. Our analysis highlights the need for innovative efforts to reduce syphilis morbidity. We identified a handful of factors associated with syphilis resurgence, including repeat infections, greater use of the Internet to recruit sex partners, and sexual partners from outside San Francisco. Efforts that target the small core of repeatedly infected patients with syphilis may have an impact on the overall trajectory of syphilis. Furthermore, the role of HIV-positive serosorting in maintaining endemic STDs also requires further exploration. Unfortunately, data on serosorting practices among the general population of MSM in San Francisco are sparse. In addition, identification of new ways to exploit the Internet, beyond Internet partner notification and social marketing, may be productive because the Internet is a major mechanism for meeting sex partners. A sizable number of both index patients and their known sex partners lived outside the jurisdictional boundaries of San Francisco and may have had an important impact in the local epidemic. Interventions targeted to San Franciscans may have a lessened (or minimal) impact for persons residing out of the county. Hence, identifying ways to approach syphilis prevention and control from a regional perspective may be fruitful, particularly for areas with a large urban center that serves as a hub for employment and recreation surrounded by densely populated suburbs. Activities focused across jurisdictions should be explored. As we move away from the era of syphilis elimination, the identification of truly novel approaches to interrupting syphilis transmission is needed.
Acknowledgments
Supported (in part) by the Comprehensive STD Prevention Projects (1H25PS001354-01), Centers for Disease Control and Prevention.
Footnotes
Conflict of interest: None to report
We thank Rilene Ng, Nicole Olson, and Michael Samuel, California Department of Public Health, for providing data and analysis of Bay Area primary and secondary syphilis case reports; Mark Pandori, San Francisco Public Health Laboratory, for providing data on VDRL testing and Jen Hecht from the STOPAIDS Project for providing data on syphilis testing among men who have sex with men.
REFERENCES
- 1.STD Control Section. San Francisco Sexually Transmitted Disease Annual Summary, 2010. San Francisco, CA: San Francisco Department of Public Health; 2011. [Google Scholar]
- 2.CDC. Outbreak of syphilis among men who have sex with men—Southern California, 2000. MMWR Morb Mortal Wkly Rep 2001; 50:117–120. [PubMed] [Google Scholar]
- 3.Klausner JD, Wolf W, Fischer-Ponce L, et al. Tracing a syphilis outbreak through cyberspace. JAMA 2000; 284:447–449. [DOI] [PubMed] [Google Scholar]
- 4.Primary and secondary syphilis among men who have sex with men—New York City, 2001. MMWR Morb Mortal Wkly Rep 2002; 51:853–856. [PubMed] [Google Scholar]
- 5.CDC. Primary and secondary syphilis–United States, 2002. MMWR Morb Mortal Wkly Rep 2003; 52:1117–1120. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. The National Plan to Eliminate Syphilis. Atlanta, GA: US Department of Health and Human Services, 2006. [Google Scholar]
- 7.Heffelfinger JD, Swint EB, Berman SM, et al. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health 2007; 97:1076–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klausner JD, Levine DK, Kent CK. Internet-based site-specific interventions for syphilis prevention among gay and bisexual men. AIDS Care 2004; 16:964–970. [DOI] [PubMed] [Google Scholar]
- 9.Levine D, Woodruff AJ, Mocello AR, et al. inSPOT: The first online STD partner notification system using electronic postcards. PLoS Med 2008; 5:e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine DK, Scott KC, Klausner JD Online syphilis testing–confidential and convenient. Sex Transm Dis 2005; 32:139–141. [DOI] [PubMed] [Google Scholar]
- 11.Ahrens K, Kent C, Montoya J, et al. Healthy penis: San Francisco’s social marketing campaign to increase syphilis testing among gay and bisexual men. PLoS Med 2006; 3:e474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stephens SC, Bernstein KT, McCright JE, et al. Dogs are talking: San Francisco’s social marketing campaign to increase syphilis screening. Sex Transm Dis 2010; 37:173–176. [DOI] [PubMed] [Google Scholar]
- 13.Wasserheit JN, Aral SO. The dynamic topology of sexually transmitted disease epidemics: Implications for prevention strategies. J Infect Dis 1996; 2(174 suppl):S201–S213. [DOI] [PubMed] [Google Scholar]
- 14.Potterat JJ, Phillips-Plummer L, Muth SQ, et al. Risk network structure in the early epidemic phase of HIV transmission in Colorado Springs. Sex Transm Infect 2002; 1(78 suppl):i159–i163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Potterat JJ, Muth SQ, Rothenberg RB, et al. Sexual network structure as an indicator of epidemic phase. Sex Transm Infect 2002; 1(78 suppl):i152–i158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cunningham SD, Michaud JM, Johnson SM, et al. Phase-specific network differences associated with the syphilis epidemic in Baltimore city, 1996–2000. Sex Transm Dis 2004; 31:611–615. [DOI] [PubMed] [Google Scholar]
- 17.Workowski KA, Berman S. Sexually transmitted disease treatment guidelines, 2010. MMWR Morb Mortal Wkly Rep 2010; 59:1–110.20075837 [Google Scholar]
- 18.Centers for Disease Control and Prevention. Sexually Transmitted Diseases Surveillance, 2010. Atlanta, GA: Department of Health and Human Services, 2011. [Google Scholar]
- 19.Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19:335–351. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SE, Chew Ng RA, Katz KA, et al. Repeat syphilis among men who have sex with men in California, 2002–2006: Implications for syphilis elimination efforts. Am J Public Health 2012; 102:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marcus JL, Katz KA, Bernstein KT, et al. Syphilis testing behavior following diagnosis with early syphilis among men who have sex with men—San Francisco, 2005–2008. Sex Transm Dis 2011; 38:24–29. [DOI] [PubMed] [Google Scholar]
- 22.Hotton AL, Gratzer B, Pohl D, et al. Factors associated with repeat syphilis testing at a large urban LGBT health clinic: Chicago, IL 2002–2008. Sex Transm Dis 2011; 38:205–209. [DOI] [PubMed] [Google Scholar]