Abstract
Management of latent tuberculosis infection (LTBI) is one of the globally recommended key strategies to end tuberculosis. However, there is limited experience with translation of global recommendations into action at country levels. We present Ethiopia's experience in implementing LTBI management. Our objective is to share promising practices, existing opportunities and to suggest specific steps required for further scale up of the services. Our report is based on synthesis of data from secondary sources including official routine reports of Ministry of Health, materials presented at review meetings, and findings from supervisory visits to districts and health facilities. Our results suggest that Ethiopia has made significant strides toward strengthening LTBI management in people living with HIV and among under-five-year-old household contacts of TB patients. The use of contact investigation as entry point for LTBI management could be taken as best practice. More effort is needed to further strengthen implementation of LTBI management, and it should be supported through context-specific implementation and operational research activities.
Keywords: Ethiopia, LTBI, Under-five children, INH preventive therapy
Introduction
Latent tuberculosis infection (LTBI) can be defined as a state of persistent immune response to stimulation by Mycobacterium tuberculosis antigens without evidence of clinically manifested active TB, and a third of the world population has LTBI [1]. Of those with LTBI only about 5–10% develop TB disease during their life time [1]. This risk of reactivation can, however, be increased several fold in persons with weak immune status such as in people living with HIV, young children with underdeveloped immune status, and patients undergoing immunosuppressive therapy [1], [2].
Management of reactivation TB has been part of the global recommendations for many years now. PLHIV and under-five children were the two groups recommended to receiving preventive treatment according to the earlier versions of WHO guidelines, and most high burden countries adopted this recommendation [2]. However, uptake of these services has been slow in many countries with only 38% of PLHIV newly enrolled in care having received INH preventive therapy in 2015 (IPT). The coverage of IPT for under-five children among estimated to be eligible is even more disappointing with 7.1% (range- 6.9–7.4%) [2].
Following WHO's 2014 guidelines for management of LTBI, there has been renewed interest to implement LTBI management in low and mid-income settings [1]. However, there is limited experience with implementation of these recommendations at local level. We present Ethiopia's experience in implementing LTBI management. Our objective was to share promising practices, existing opportunities and to suggest specific steps required for further scale up of LTBI management in Ethiopia.
Our report is based on synthesis of data from secondary sources including official routine reports of the Federal Ministry of Health of Ethiopia (FMOH), materials presented at review meetings, and findings from supervisory visits to districts and health facilities. The data source for FMOH reports is the nationally approved health management information system (HMIS). For data not yet fully captured in the HMIS such as contact investigation and IPT in under-five children, we used data reported from pilot projects in partner supported areas.
Country context
Ethiopia is a country which is located in East Africa with a current projected total population of 90.14 million covering a total area of 1.1 million square kilometers [3]. Administratively it is composed of nine regions, two city administrations and 840 districts. The existing health tier system contains three levels of health care system which is classified as the primary, secondary and tertiary level depending on the type and extent of service provided to a given number of population. The national TB program of Ethiopia envisages promoting decentralization of TB and TB/HIV packages into the primary health care context [4].
 |
Ethiopia is among the 30 high TB, TB/HIV and MDR TB burden countries with an estimated incidence and prevalence rate of 207 and 200 per 100,000 populations consecutively [2]. Total all forms of TB cases notified in 2015 is 134,343 with a case detection rate of 62%. The current national HIV prevalence rate is reported to be 1.14%.
Ethiopian national guidelines recommend two group of patients for management of LTBI namely PLHIV and under-five children who are contacts of index TB patients [5]. Management of LTBI in under-five children has been integral part of the national guidelines since 2013. However, this has not been fully implemented. In the next section, successes and challenges in implementing LTBI in these specific group of patients is briefly described.
Data sources
This paper is based on analysis of data from secondary sources including (1) annual TB program performance reports of the Federal Ministry of Health of Ethiopia; (2) proceedings of annual TB program performance meetings; (3) minutes of TB and TB/HIV technical working groups; and (4) performance reports by major TB technical assistance partners. The information was then categorized into the following thematic areas; background and context to LTBI management in Ethiopia; LTBI Management in people living with HIV (PLHIV); and LTBI management in under-five children. The primary results of this thematic analysis was presented at global WHO consultation meeting on the programmatic management of LTBI held between 27-28 April, 2016 in Seoul, Republic of South Korea. http://www.who.int/tb/challenges/consultation_meeting_ltbi/en/. Based on the feedback received at the conference, we further refined the content of the paper through reiterative discussion among the three authors.
LTBI management in PLHIV
In Ethiopia, TB/HIV collaborative activities were initiated in 2002 with establishment of a national coordinating body –the TB/HIV advisory committee (THAC). In 2004, pilot implementation was started in 9 selected sites. Building on the experience of the pilot implementation and as part of the effort to further strengthen the collaborative activities, the National TB/HIV Technical Working Group (TWG) was established in April 2007. The TWG, co-chaired by the TB and HIV programs on a yearly rotation basis started its functions by revising the national implementation guideline in 2008. This was followed by massive capacity building efforts for health workers. Between the year 2007 and 2008, major expansion of ART sites took place i.e. in terms of number, access (geographic coverage). In 2012, TB/HIV collaborative activity guideline got incorporated into comprehensive TBL&TB/HIV guideline. Recommendations from WHO's 2011 guidelines for intensified case find and IPT were incorporated into the training materials [6]. To promote joint TB/HIV programming, to leverage resources for collaborative activities and to put together the planning process between the two programs, joint single TB/HIV concept note was developed in 2014. Xpert MTB/RIF got introduced as the preferred primary screening and diagnostic test for PLHIV for children. In 2014, the national HMIS got revised to include major TB/HIV core indicators. Before that, the national HMIS captured only two TB/HIV indicators (i.e. TB screening among PLHIV& HIV screening among TB patients). To close this gap, the national TB/HIV sentinel surveillance system was introduced in 2010. This surveillance data is used to depict and show the trends in TB/HIV performance of the country according to the core global and national indicators.
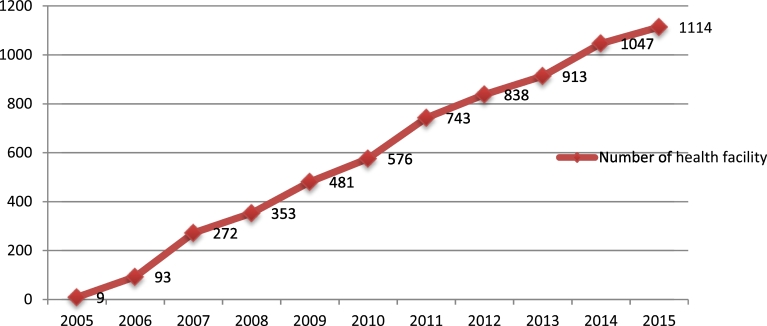
Despite the effort put to improve the uptake of IPT including massive expansion of HIV treatment sites providing IPT (Fig. 1), there was significant decline in the proportion of PLHIV put on IPT. This prompted more in-depth analysis of factors contributing to declining IPT coverage among eligible PLHIV. The main reasons for low provision and uptake of IPT were assessed as part of the national assessment of TB and TB/HIV services. According to the report, 72% of respondents reported INH supply interruption as the main reason while the remaining 28% reported lack of training, fear of acquiring further resistance in individual cases, difficulty of ruling out active TB (especially in children) because of lack of diagnostic capacity, and fear of INH toxicity as reasons for the low uptake of IPT [7].
Fig. 1.
ART sites providing IPT services nationally.
Based on the findings of the national assessment, an accelerated IPT implementation plan was developed and series of sensitization workshops were conducted for health care professionals nationwide which are believed to have contributed to increasing IPT uptake performance in 2015.
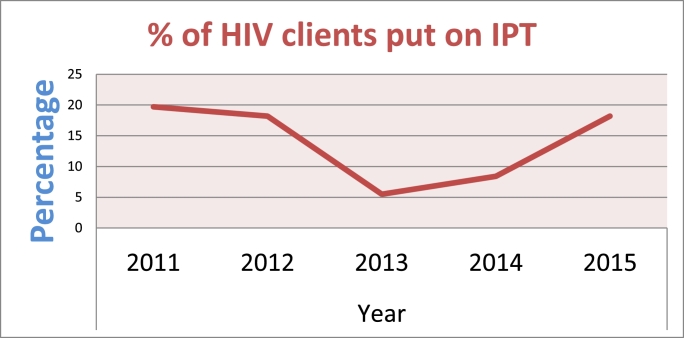
In 2015, the national Isoniazid preventive therapy (IPT) uptake is reported to be 44.4% on HMIS among newly enrolled HIV patients. When compared to the previous years, IPT uptake has shown a remarkable incline as depicted on the annually conducted national sentinel surveillance (Fig. 2).
Fig. 2.
National IPT coverage. National TB/HIV Sentinel Surveillance annual report trend.
LTBI management for <5 yr children
The practice of LTBI management in under 5 child contacts is relatively recent in Ethiopia but encouraging progress has been made over the last five years as shown by recent published reports [8]. Ethiopia used contact investigation among adult patients as the main entry point to IPT for under-five child contacts. Started as project-specific intervention in two regions of Ethiopia [9], [10], contact investigation has now been scaled up to all regions of the country. Also, IPT coverage among under-five children has improved steadily, according to programmatic data reported from nine regions of the country. Accordingly, 2965 of 5742 eligible under-five children identified through contact screening received IPT, making the uptake rate 51.6%.
Despite the progress, several challenges remain to be addressed. The lack of diagnostic capacity and clinical skill makes child TB case ascertainment and ruling out of TB in children very difficult. Now with the introduction of Xpert MTB/RIF technology, sample collection for testing remains to be the major challenge. Due to limited surveillance data among children, estimating the actual burden of latent TB was problematic leading to low forecasting of supply needs for IPT in under-five children. With the accumulation of programmatic experience, the country is now able to make more accurate estimates for IPT needs and the QuanTB tool has been very useful in this regard.
With the country's renewed commitment to strengthen its childhood TB program, as outlined in the national roadmap, there are several opportunities for further strengthening of LTBI management in under-five children. Based on this road map and global guidance, training material for health care workers has been developed and series of sensitizations and CMEs and capacity building activities were conducted on the prevention and control of child TB. Child TB case finding and contact tracing activity also go integrated into the national child survival strategy (IMNCI and ICCM) [11].
Conclusions and way forward
Ethiopia has made significant strides toward strengthening LTBI management in PLHIV and among under-five children. The country's use of contact investigation as entry point for LTBI management could be taken as best practice. Moreover, the national childhood TB roadmap which outlines ways to deliver integrated maternal and child health services together with LTBI is another commendable best practice. The use of accelerated action plans led to noticeable changes in IPT uptake, which other countries can be suggested for replication in other similar settings.
The Ethiopian LTBI management practice, however, requires considerable efforts to further strengthen best practices demonstrated through region-specific projects. The scale up of contact investigation efforts should be supported by FMOH guidelines and standard operating procedures. The relative contribution of contact investigation both as entry point to LTBI management and case finding should be quantified in a more comprehensive manner. Targeting INH need in children and distribution of INH drug nationwide, availability of palatable INH formulations for under five children, lack of global indicators on LTBI management of children, and the place of LTBI management in DR-TB contacts of children are among some of the programmatic challenges. Some of the major priority implementation research questions identified are provision of IPT with ART compared with Pre ART and after ART, clinical management of LTBI treatment interrupters and the place for repeating LTBI treatment after completion.
References
- 1.World Health Organization . World Health Organization; Geneva: 2015. Guidelines for the management of latent TB infection. [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva: 2016. Global tuberculosis report 2016. [Google Scholar]
- 3.Federal Democratic Republic of Ethiopia . Population projection of Ethiopia for all regions at woreda level from 2014-2017. Government of Ethiopia; Addis Ababa, Ethiopia: 2013. Central statistics agency. [Google Scholar]
- 4.Federal Democratic Republic of Ethiopia, National TB program. National TB and TB/HIV strategic plan from 2013-2020. Addis Ababa, Ethiopia, 2013.
- 5.Federal Ministry of Health of Ethiopia . FMOH; Addis Ababa, Ethiopia: 2013. Guidelines for clinical and programmatic management of TB, TB/HIV and leprosy in Ethiopia. [Google Scholar]
- 6.World Health Organization. Guidelines for intensified tuberculosis case finding and isoniazid preventive therapy for people living with HIV in resource- constrained settings WHO 2011.
- 7.Federal Democratic Republic of Ethiopia Ethiopian public health institute. National assessment of TB DOTS and TB/HIV service 2014; Addis Ababa, Ethiopia; 2014. [Google Scholar]
- 8.Tadesse Y., Gebre N., Daba S., Gashu Z., Habte D., Hiruy N., … G., Suarez P. Uptake of isoniazid preventive therapy among under-five children: TB contact investigation as an entry point. PLoS One. 2016;11(5) doi: 10.1371/journal.pone.0155525]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jerene D., Melese M., Kassie Y. The yield of a Tuberculosis house hold contact investigation in two regions of Ethiopia. Int J Tuberc Lung Dis. 2015;19(8):898–903. doi: 10.5588/ijtld.14.0978. [DOI] [PubMed] [Google Scholar]
- 10.Gashu Z., Jerene D., Ensermu M., Habte D., Melese M., Hiruy N., …, Suarez P. The Yield of community-based “retrospective” tuberculosis contact investigation in a high burden setting in Ethiopia. PLoS One. 2016;11(8) doi: 10.1371/journal.pone.0160514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Federal Ministry of Health, National TB Program. National road map for prevention and control of childhood TB in Ethiopia. Addis Ababa, Ethiopia, 2015.