Abstract
To attain the Global End Tuberculosis (TB) goals, the treatment of persons with TB requires advancements in coordinated approaches that are low-cost and highly accessible. Treating TB successfully requires prolonged medication regimens with good adherence, which in turn requires patients to be adequately supported. Furthermore, TB care-providers often wish to monitor treatment-taking by patients in order to track the success of their programs and ensure adequate completion of therapies by individuals. The standard-of-care for treatment monitoring in TB programs often includes directly observed therapy (DOT). Video observed therapy (VOT) has emerged as a method to mimic in-person visits or observations, especially in the smartphone era with internet data connections, but remains simply inaccessible to patients in areas where TB is most endemic. Both approaches may be considered more intensive than necessary for many patients, leaving an opportunity for more affordable and acceptable approaches. The rapid increase in mobile phone penetration provides an opportunity to reach patients between clinical visits. Short message services (SMS) are available on almost every mobile phone and are supported by first generation cellular communication networks, thus providing the farthest reach and penetration globally. Evidence from non-TB conditions suggests SMS, used in a variety of ways, may support outpatients for better medication adherence and quality of care but the evidence in TB remains limited. In this paper, we discuss how basic mobile phones and SMS-related services may be used in supporting global care of persons with TB, with a focus on patient-centered approaches.
Keywords: Tuberculosis, Mobile health, Text messaging, Video observed therapy, Patient-centered care, Patient care
1. Introduction
Treating tuberculosis (TB) is important to reduce morbidity and mortality as well as the risk of ongoing transmission, but it can be challenging to support and monitor persons with TB over the full course of treatment [1]. Active TB treatment typically requires a daily administration of a combination of medicines for six months or longer (e.g. 20 months or more for multidrug resistant [MDR] TB) [2].
Poor adherence to TB treatment can have deleterious effects, such as the potential for further TB transmission, relapse, acquired drug resistance, treatment failure, and death [4], [5], [6]. Interventions aimed to improve adherence have traditionally targeted the health system, the social environment, or persons with TB themselves [7], [8], [9] The World Health Organization (WHO) recommends in-person directly observed therapy (DOT) in their guidelines, either at a health facility or at home, for improving TB adherence [10], [11]. However, DOT is often challenging and not feasible to implement in most settings with a high burden of TB; TB programmes often struggle with providing human resources to ensure repeated face-to-face encounters over many months. From the perspective of persons with TB, DOT is incredibly time consuming, can substantially interfere with employment, family commitments, and other daily activities, and may be construed as patronizing and intrusive [12]. Even in settings where DOT is implemented, systematic reviews have shown that DOT is generally not effective in improving patient outcomes when compared to less disruptive or intrusive alternatives [13], [14]. Treatment of latent TB infection (LTBI) is also challenging as recommended LTBI regimens require three to nine months of treatment [2]. Furthermore, both first-line and second-line medications for TB and LTBI can cause adverse reactions, that may negatively impact the persons’ quality-of-life and safety, and lead to treatment interruption [2]. A considerable portion of persons with LTBI, who are by definition asymptomatic, have been shown to be at risk for loss to follow-up at all stages of cascade of care (i.e. initial TB screening to treatment completion) and are particularly likely to miss doses or stop treatment [2], [3].
In recent years, patients and health care providers have benefited from improved access to digital communication technologies. Mobile phone ownership has grown considerably in regions with high TB incidence and burden [1], [15]. The number of mobile phone subscriptions now exceeds the number of people globally, with widespread penetration into low- and middle-income countries (LMIC) including persons of lower socioeconomic status [15], [16]. This widespread penetration of mobile phones bring the potential of overcoming the challenges associated with DOT-based TB care, as mobile phones provide an opportunity to facilitate direct communication between health care providers and persons with TB with its short message service (SMS) and mobile voice call features. SMS, which includes basic text messaging and other app-based messaging features, are the most popular form of communication, followed by mobile calls that allow for voice communication. In addition, with increasing ownership of smart phones there is now capacity to communicate via video in some regions with adequate internet bandwidth.
A holistic approach that integrates digital technologies into various elements of care for persons with TB or LTBI is gaining considerable attention [17], [18]. The increasingly equitable access to mobile phone communications provides a unique opportunity to facilitate direct communication between health care providers and persons with TB. While video communication is not feasible in remote regions with weak or no internet connectivity, cellular SMS can likely reach persons with TB who reside in these areas. These communications may be used to monitor and support persons with TB between clinical visits that would allow for a growing framework in differentiated care, where different care packages with varying intensity can be delivered for patients based on their needs [19].
In this review, we discuss the role of mobile phones in TB care, building on the recently released Handbook for the Use of Digital Technologies to Support Tuberculosis Medication Adherence published by the World Health Organization (WHO) [18]. We will specifically discuss the evidence and opportunities to guide the use of SMS-based communication interventions to support TB care. We emphasize patient-centered approaches that can be integrated into the digital health landscape. Other innovations, such as the use of dose and pill packaging monitors and video observed therapy (VOT), which could be used in isolation or alongside mobile phone communications, are discussed in more depth in articles 4 and 6 of this series. While the current evidence on best digital practices in TB care remains limited, we can borrow from evidence and lessons learned in HIV and other chronic disease care where evidence exists to assess SMS-based interventions in establishing interactive, patient-centered approaches to care [20], [21].
2. Potential for mobile phone communications in global health
Globally, virtually all mobile phones, basic or smart, support text messages. Basic phones with limited applications can support additional functions such as mobile money transfer where available. Feature phones may include a variety of other services, such as multimedia messaging service (MMS), email, internet access, short-range wireless communications (infrared, Bluetooth), business applications, video games, and digital photography. Smartphones with an operating system and cellular network connection offer greater advanced capabilities, such as video messaging.
People across the socioeconomic spectrum utilize cellular communications frequently. For instance, 6 billion SMS are sent daily in the United States, corresponding to a daily average of 36 texts per person [22]. Globally, it is estimated that at least 23 billion SMS are sent and received each day. SMS tends to have higher open rates (that is, the probability of being opened for reading) compared with longer messaging formats such as email [23] and may be preferred to voice calls and video messaging in some circumstances [24], [25]. Although there are many potential approaches for mobile phone-based adherence interventions (Box 1), this review will primarily focus on those that use SMS since this is the most ubiquitous and has been most extensively evaluated in the health context. Health interventions that use conditional mobile money transfer have not been investigated among TB patients, but there is a pilot study on vaccination promotion with promising results [26], [27], [28]. Digital gaming approaches have been piloted to support adherence, but usually require smartphones and have not yet been reported for TB care.
Box 1. Ways in which SMS may be used to support treatment adherence.
Examples:
Dosing reminders: Patients receive recurring reminders to take their pills or remind them of their treatment [48].
Motivational messages: Informing or reminding patients that treatment is important to their health [42].
Appointment reminders: Patients receive alerts prior to their upcoming clinical visits [65].
Education: Patients are sent information intended to improve their health literacy [66]
Entertainment: Gaming and other applications intended to make engaging in care and treatment more enjoyable [67]
*Financial incentives: Patients may receive SMS or app-based mobile money transfer to cover healthcare costs or as rewards for treatment milestones [63], [64]
*Insurance: Patient may send and store money via mobile money transfer or products to cover future healthcare costs [63], [64]
Monitoring: Patients may be required to send confirmation of pill taking or other treatment related activities. This can be done via regular mobile phones or special devices that use cellular networks [68], [69].
Support: Patients have access to digital or expert human resources to help them manage their care needs [70]
*Mobile money transfer via basic cell phones using SMS or USSD functionality is available in some countries and have been used for health insurance and health payments (e.g. M-TIBA in Kenya)
2.1. Choosing mobile phone communication interventions
Many health providers use work or personal mobile phones to communicate with patients in formal or informal ways, just as landline telephones were used in the past. In addition to voice communication, mobile phones have allowed for SMS-based communications that patients use frequently, at low-cost. The written nature of text messaging has provided an opportunity for more structured, documented, and targeted interventions to be delivered for patient support and monitoring.
2.1.1. Different SMS-based interventional approaches
There are many different interventional approaches that can be formulated using SMS (Box 1). They can be broadly classified as one-way or two-way communication interventions. One-way communication interventions can take the form of daily treatment or medication dose reminders. This is commonly a recurrent, automated text message sent to remind patients to take their TB medication. Content and frequency of text messages vary, with message frequency ranging from daily to monthly, and content often containing motivational messages intended to inform or remind patients of the importance of adherence. One-way communication has also been utilized in the form of SMS-based reminders to notify persons with TB of an upcoming clinic appointment. Two-way communication interventions, on the other hand, involve interactive messages between health care providers and the patient, directly or via a software application. Two-way messaging has the potential benefit of improving the relationship between persons with TB and their provider, as well as maintaining the engagement of persons with TB in their own care.
2.1.2. Existing evidence for SMS-based interventions
SMS-based interventions have been tested and evaluated for smoking cessation [29], [30], [31], [32], [33], adherence to HIV antiretroviral therapy [34], preventive health care [35], and TB treatment [36], [37], [38]. In these contexts, interactive communication tends to be superior to simple patient reminders [39], [40], [41]. In several studies, regular pill taking reminders alone are often ineffective in the short and long-term, regardless of frequency or motivational content [42]. The effect of pill reminders may provide little additional benefit beyond existing reminder mechanisms (e.g. watch alarms or placing pills in a place that becomes routine to access). Additionally, if people receive one-way messages without an opportunity to respond, they may feel undermined or annoyed with the high frequency of reminders, and may potentially ignore these messages [43]. In contrast, SMS-based clinic appointment reminders have been shown to improve clinic attendance and TB treatment completion and could provide an evidence-based value to TB treatment programmes [44].
Two-way communication interventions have the potential to improve engagement of persons with TB, as shown in persons with HIV [20], [41]. Some interventions allow patients to lead the communication, establishing an open pathway to initiate and direct interactions with health care providers [21]. Voice-based communication interventions certainly allow for two-way, interactive exchange; however, it may be the case that some patients, especially adolescents and youth or people with limited mobile plans, may prefer to exchange communication via SMS, which allows them to respond at convenient times and places, and preserves some privacy. Patients may prefer voice communication with closer relationships [24]. SMS also has the advantage of establishing a written record of healthcare interactions [43]. In summary, the value of interactive (two-way) messaging via mobile phone goes well beyond reminders in offering enhancements in clinical care of patients [21], [45], [46].
2.1.2.1. Existing evidence for SMS interventions for persons with TB
To our knowledge, there are six completed randomized clinical trials that have evaluated the effectiveness of SMS interventions for persons with TB: Mohammed 2016 [42]; Liu 2015 [47]; TB-SMS Cameroon [48,49]; Belknap 2017 [50]; Fang 2017 [51]; and WelTel LTBI [52], [53]. Table 1 summarizes the design of these trials; Table 2 summarizes the intervention approaches that were undertaken for the SMS interventions, and reported effect measures on each trial's primary outcome are summarized in Table 3.
Table 1.
Randomized clinical trials of SMS interventions for TB: Study design.
| Trial ID | Trial registry | Population | Study design | Location | Sample size | SMS intervention | Arm 2 | Arm 3 | Control |
|---|---|---|---|---|---|---|---|---|---|
| Mohammed 2016 [42] | NCT01690754 | Newly diagnosed TB | Individual RCT, open label | Pakistan | 2207 | Two-way SMS reminders | – | – | DOT |
| Liu 2015 [47] | ISRCTN46846388 | Newly diagnosed TB | Cluster RCT | China | 4292 | Two-way SMS reminders | Medication monitor | SMS reminder + medication monitor | Self-administered therapy, family supervision, or DOT |
| TB-SMS Cameroon [48], [49] | PACTR201307000583416 | Active TB | Individual RCT with single blind of health care providers | Cameroon | 279 | One-way SMS reminders | – | – | DOT |
| Belknap 2017 [50] | NCT01582711 | Latent TB | Individual RCT, blinding info NA | US, Spain, Hong Kong, and South Africa | 964 | Weekly SMS reminders + self-administered therapy | Self-administered therapy | – | DOT (monthly) |
| Fang 2017 [51] | – | Active TB | Cluster RCT, blinding info NA | China | 350 | One-way SMS reminders | – | – | DOT |
| WelTel LTBI [53], [75] | NCT01549457 | Latent TB | Individual RCT, open label | Canada | 350 | Two-way SMS check-ins | – | – | Self-administered therapy, |
Table 2.
Randomized clinical trials of SMS interventions for TB: SMS approach.
| Trial ID | SMS intervention | Intervention duration [months] | Message Frequency | Motivational message | Message content | Messaging time | Follow-up reminder |
|---|---|---|---|---|---|---|---|
| Mohammed 2016 [42] | Two-way SMS reminders | 6 | Daily | Yes | “Your health is in your hands. Take your medication and remember to respond by SMS or a missed call.” | Reminder sent based on preferred time of patients | If the patient did not respond within two hours, a second reminder was sent. A third and final reminder for the day was sent after two additional hours of non-response. Members of study team phoned participants who did not respond for seven days. |
| Liu 2015 [47] | Two-way SMS reminders | 6 | Daily | No | "Please take the medication on time” | Reminder sent based on preferred time of patients | Up to 3 SMS reminders, patients expected to reply and reminders stop once the patient responds. |
| TB-SMS Cameroon [48], [49] | One-way SMS reminders | 6 | Daily | Yes (every 2 weeks) | "Good morning, it is important to take your drugs against TB every day" "Good morning, taking drugs daily increases your chance of healing" | NR | – |
| Belknap 2017 [50] | Weekly SMS reminders + self-administered therapy | 4 | Weekly | No | NR | NR | – |
| Fang 2017 [51] | One-way SMS reminders | 6 | Daily | No | NR | Morning | Contained TB-related knowledge for establishing healthy life style. |
| WelTel LTBI [53], [75] | Two-way SMS check-ins | 12 | Weekly | No | “How are you?” ”We haven't heard from you, how are you?” | Monday morning | 48 h after initial message. |
Table 3.
Randomized clinical trials of SMS interventions for TB: Reported effect measure on primary outcome.
| Trial ID | Intervention arms vs control | Primary outcome | Arm 1 | Arm 2 | Arm 3 | Control | Secondary outcomes |
|---|---|---|---|---|---|---|---|
| Mohammed 2016 [42] | Arm 1: Two-way SMS reminders Control: DOT | Treatment success - cured (i.e. sputum smear or culture negative in the last month) or treatment completion | 83% | – | – | 83% | Death, transferred out |
| Liu 2015 [47] | Arm 1: Two-way SMS reminders Arm 2: Medication monitor Arm 3: SMS reminder + medication monitor Control: Self-administered therapy or DOT (control) | Poor adherence - at least 20% dose missed | 27.30% | 17.00% | 13.90% | 29.90% | Poor adherence - at least 47% dose missed (7/15 doses) |
| TB-SMS Cameroon [48], [49] | Arm 1: One-way SMS reminders Control: DOT | Negative Microscopy at 5 months | 81% | – | – | 74.6% | Cured (microscopy) at 6 months |
| Belknap 2017 [50] | Arm 1: Weekly SMS reminders + self-administered therapy Arm 2: Self-administered therapy Control: DOT | Treatment completion - 11 or more doses within 16 weeks | 76.4% (95% CI: 71.3 - 80.8) | 74.0% (95% CI: 68.9 - 78.6) | – | 87.2% (95% CI: 83.1 - 90.5%) | Adverse events |
| Fang 2017 [51] | Arm 1: One-way SMS reminders Control: DOT | Treatment completion | 96.3% | – | – | 86.4% | Missed dos, interrupted treatment, reexamination of sputum after 2-, 5- and 6-months of treatment |
| WelTel LTBI [53], [75] | Arm 1: Two-way check-ins Control: Self-administered therapy | Retention at 12 months | 79% (277/349) | – | – | 81% (285/351) | Proportion of scheduled appointments kept and level of engagement, retained in care at 6 months, death |
Mohammed 2016 [42] and Liu 2015 [47] investigated the effectiveness of two-way SMS reminders for newly diagnosed persons with active TB. The trial by Mohammed 2016 [42] was a two-arm, open-label RCT in Pakistan; the trial by Liu 2015 was a cluster RCT conducted in China. Two-way communication modalities were said to be used in these trials; however, they resembled one-way communication modality as persons with TB were just asked to respond to the daily reminders that asked them to take their medication and did not promote further communication (Table 2).
TB-SMS Cameroon [48], [49] and Fang 2017 [51] evaluated the role of daily, one-way SMS reminders in persons with active TB. TB-SMS Cameroon sent a ‘motivational’ message every two weeks that reminded participants of the importance of adherence, whereas the content of the messages was not reported in the trial by Fang 2017 [51].
Belknap 2017 [50] was a multi-national phase 4 non-inferiority trial for persons with LTBI within outpatient TB clinics of US, Spain, Hong Kong, and South Africa. The goal of this trial was to compare the treatment completion by self-administration (i.e. MEMS device) with or without weekly SMS reminders, but other details on the nature of the SMS reminders were not reported in the publication [50]. WelTel LTBI [52], [53], on the other hand, was the only trial that investigated the role of primary interactive two-way SMS check-ins. In that study, no difference was seen in treatment completion between arms, but completion rates were much higher than baseline in both arms. Other potential benefits such as handling of medication side effects and perceived improvements in care received were reported. This trial is discussed more extensively in Box 2 as a case study.
Box 2. Case example: Interactive SMS-based mobile phone support of TB treatment adherence, “Beyond reminders”.
Background: WelTel (www.weltel.org) is a mobile health (mHealth) outreach program and platform service that was initially designed to support HIV treatment adherence in Africa [20]. WelTel expanded its use to other conditions and geographies including TB patient support. It uses mobile phone and SMS to communicate directly with patients in a patient-centered approach [21]. Based on field research with patients and frontline providers to inform preferred messaging content, frequency, and procedures, the system sends weekly text message check-ins to registered patients asking them “How are you?” (or any preferred language). The patient can respond by text either with “OK” or “Not OK” to indicate need for communication with the healthcare provider who can engage in further text messaging, or by voice calling if the patient has limited literacy or the issue is complex. The communications are captured via a web interface that is mobile-device friendly and organized for provider access and work-flows (provider case management). The system records all communications and care plans can be noted. A video component has been integrated for optional use in settings in which smartphone access and sufficient data connections are available. However, the ‘'base of the (economic and digital) pyramid’ approach is maintained by enabling access to the platform by basic cell phones for any user. In addition, WelTel can send the patient clinic appointment reminders via SMS. Provider-side alerts can be shared between different colleagues who care for the patient. Overall, triaging patient-reported issues can help to identify which patients require additional support and when. The program also provides assurances for stable patients who indicate they are doing well and alleviate resources in line with Differentiated Service Models [19], [71].
Implementation approach: With the aim to transform “evidence into action” and expand from grant-funded research into a scalable service for larger impact, WelTel International mHealth Society was formed in 2011 as a non-profit organization to provide services in Africa. In 2013, WelTel Incorporated was founded to further develop the software and digital platform service. Health research funding has been primarily from public sources (i.e. PEPFAR, CDC Foundation, CIHR, NIH, BC Lung Association, the BCCDC Foundation, and Grand Challenges Canada) and sustainable services are done via service contracts with health service providers and health authorities.
Evidence and lessons learned: The TB adaptation was based on RCT evidence that the weekly check-in method improved adherence to antiretroviral therapy (ART) for HIV treatment in Kenya and confirmed in Canada [20], [60]. A pilot study among active TB patients at the BC Center for Disease Control's Provincial TB Clinic in Vancouver, Canada, demonstrated acceptability of the program among TB patients and care providers [52], [53], [72], [73]. In order to address poor completion rates among patients taking treatment for latent TB infection (LTBI) which at the time were estimated at only 60% in BC, an RCT of 358 patients was conducted comparing WelTel supported care to standard care. While there was no significant difference in completion rates (WelTel and SOC arms achieved 79.4% and 81.9% completion) [72], patients enrolled in the WelTel intervention indicated that the primary benefit was feeling ‘better cared for’ (35%) followed by improved management of side effects (32%). To support their claim, there was a higher reporting rate of side effects in the WelTel arm, yet decrease in reported hospital visits in that arm, suggesting side effects may have been managed more proactively. Notably, only 14% of the participants felt the primary benefit to them were the “reminders”, and recent behavioural studies indicate interactive follow-up may be the key factor positive behaviour change [74]. In a recent trial testing WelTel for HIV retention in care, there was a significant improvement in quality of life (QoL) scores in the WelTel arm versus standard care [75]. The economic analysis of WelTel supporting HIV care in Kenya was found to be ‘extremely cost-effective’ by WHO standards below $15 per patient per year in Kenya, and for treatment of LTBI in Canada, a simulation study indicated a 10% improvement in adherence would be cost-effective up to $220 per intervention [52]. Despite emerging evidence, transforming ‘evidence to action’ at scale remains challenging as pathways for scaling digital health services remain less well established than for treatments and diagnostics. Clear or coordinated implementation policies will be required at country and regional levels for digital health services to reach their potential.
Future directions: We will continue assessing inclusion of advancing and emerging technologies while ensuring a ‘bottom of the pyramid’ approach upwards to ensure inclusion of the most vulnerable people and populations, now as well as into the future. In doing so, we will seek to fill evidence gaps to identify best practices for patients and providers and to assist with implementation process. For example, economic analyses of digital health services to support emerging care models such as differentiated care [19], [71] are envisioned which may assist in leveraging large scale policy adoption. By conducting systematic implementation research, we aim to understand the facilitators and barriers to scale in order to share our experiences and data of the TB and other programs [43].
Alt-text: Unlabelled box
Among these six recently completed trials, DOT was the most frequently utilized control. However, the details on how DOT was performed were not frequently reported. Mohammed 2016 [42] and Belknap 2017 [50] reported using in-clinic DOT, and a conventional DOT strategy was reported by TB-SMS Cameroon [48], [49] and Fang 2017 [51]. It is important to recognize that the standard and effectiveness of different DOT strategies varies considerably between regions where these trials were undertaken. Moreover, in the trial by Liu 2015 [47], persons with TB who were assigned to the control group were given a choice of self-administration, treatment supervision by family members, or in-clinic DOT by health care providers, imposing a self-selection bias within the control group. DOT may not be the best control for comparisons of SMS or other digital outreach interventions if improvements in adherence are expected as a primary outcome.
Taken together, these RCTs show that SMS reminders often do not improve treatment adherence and/or clinical outcomes for active TB or LTBI. This may be due to the ways that those programs have significant patient monitoring and support systems in place, or it could be the ways in which SMS was used. For many of these studies, SMS was largely used as a pill reminders, even when used with a two-way intervention. Comparing SMS interventions to in-person DOT for adherence may not be appropriate, as the goals of digital patient centred interventions should focus on other important outcomes such as improved autonomy, perceived quality of care, convenience for patients and providers, cost savings, and availability to support patients between clinical visits. It is plausible that text messages for in-person visits would have an additive effect on adherence where patients are not already seen by more intensive means. For example,– mobile communications such as SMS may stand a higher chance of improving adherence for self-administered therapy (SAT) where contact with the patient was limited between scheduled outpatient visits – a reality common to many global TB programs. Furthermore, differences in the intensity of monitoring and support required for LTBI and active TB may be different, as active TB has more immediate morbidity and mortality risk for the patient and is prone to transmission to others form a public health perspective.
At the health system level, two-way interactive messaging may collect data from provider-patient interactions that could inform emerging practices such as Differentiated Care. Data captured from interactive communications between patients and providers could provide valuable information on health system priorities thereby improving efficiency, acceptability, and overall quality-of-care [54].
2.1.3. Status and country experience
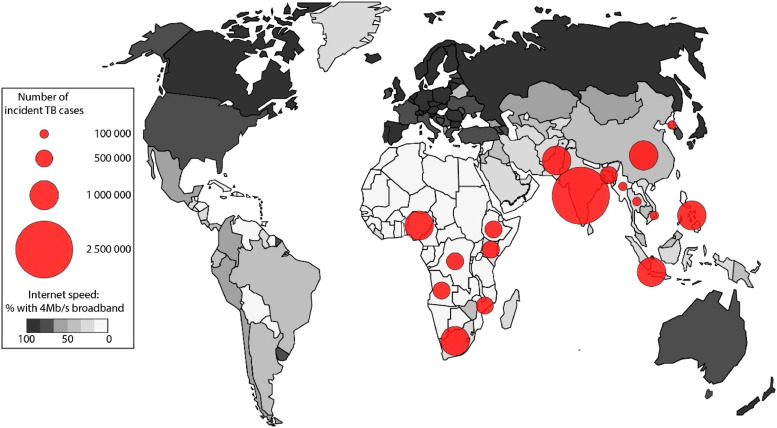
SMS interventions are likely to drive many of the digital health interventions in TB care, in both public and private sectors, after recent demonstration projects in several high- and low-resource settings [18]. However, there are few examples of broad national scale up or countries with a policy advocating for digital health interventions for TB at this time. One such example is in Vietnam, where a pilot was conducted to test a web-and mobile phone-based system for TB treatment adherence in Ba Ria-Vung Tau province in 2013 [55]. The pilot aimed to support patients in self-management and adherence, and to enable health care workers to monitor patient's progress. SMS reminders were found to contribute significantly to patient's receiving their final sputum smear test and to aiding in adherence to medication. The success of the pilot, as well as linkages to the Vietnam TB patient management system and support from the Vietnamese government led the decision from the National Tuberculosis Control Program to scale up the mHealth and digital TB treatment adherence system nationwide. In countries, where the largest burden of disease exists for TB, there is limited access to smartphones, Internet, or network data limiting the utility of VOT (Fig. 1). In fact, SMS may be the only viable digital option that is consistently available in these settings. Adopting patient-centered care using digital health interventions, if used broadly, may also translate into improved outcomes for persons with comorbidities commonly associated with TB, such as HIV infection [20], [21] and diabetes [56], [57].
Fig. 1.
2.1.4. Technical considerations of adopting mobile phone communications into TB treatment plans
There are technical considerations of incorporating mobile phone voice- and SMS-based communication interventions into TB patient support plans. Health care providers need to discuss what patients can expect with respect to voice calls and SMS before TB medications are initiated. The discussion needs to cover privacy concerns, along with objectives and procedures that can be followed to handle various situations, such as delayed replies, back-up options if voice or SMS communication fails, and expectations around the time of the day and contact person whom the patient can phone and text for follow-up support.
In the smartphone era, the mode of SMS needs to be established. There are three modes of SMS: 1) Text messages; 2) Short messages through a third-party mobile app; and 3) Short messages through a customized mobile app. Text messaging is a built-in feature of all mobile phones that operates via a mobile subscription network. Third-party messaging mobile apps such as Facebook Messenger, WhatsApp, and Viber that operate via subscription data services or wireless Internet could be used as well. However, the use of third party mobile apps is limited to those who can afford to buy a smartphone and a data plan and live in an area with sufficient broadband (usually 3G or greater) connections.
The use of third-party messaging apps has other disadvantages related to user privacy and data ownership that may not conform to local privacy policies or patient expectations, as many third-party applications hold the right to personal data. Customized apps that allow for SMS communication may help overcome issues of data ownership and privacy, and can be developed specifically for TB care. Other advantages of this approach may include the ability to modify content based on programmatic needs; inclusion of additional features (e.g. clinic visit reminders) on top of basic text messaging system; development of an overall system that can manage all patient message conversations in a single platform, including a summary dashboard for history of patient adherence; and compatibility and interoperability with an electronic medical record (EMR). However, these apps require more advanced phones and data connections with adequate broadband width that may not be consistently available in the countries where highest burden of TB exists. Developing and maintaining customized apps with these features requires substantially more funds and time than using built-in text messaging features.
Choosing a SMS for clinical care involves other logistical matters to be addressed; for instance patients will want to know who is paying for hardware, networks, and communications. Some people may share a phone with others (e.g. family members), in such cases, special attention should be provided to ensure confidentiality. Tailored digital health applications can be bundled into platforms that address many of these issues. One example of an integrated mobile phone-based digital health platform that has been used in TB care is provided in Box 2.
2.1.5. Interactions with other digital technologies
As outlined in Box 1, there are multiple ways in which mobile phone technologies can be approached. The existing research on other digital approaches and technologies, such as MEMS and VOT, is promising and covered in other articles of this series. The digital strategy for TB patient care could add SMS and voice communication to video messaging. Separate devices, such pill monitors (e.g. MEMS) can be paired with mobile phone communications to reach out and support patients. Mobile money transfer, gaming, and stored or transmitted health information could be considered in any number of innovative combinations. Regardless of format, communication approaches that are designed to improve patient-provider relationships and access that enhance patient-centred care should be favoured, as a previous study has shown that pill taking gadgets and memory aids may not yield intended benefits on adherence [58].
3. Potential limitations, considerations and future directions
This review aims to summarize existing evidence on SMS-based communication interventions and contextualize them to help implementers and policy makers to adapt solutions that can work in real world settings. SMS has its strengths and weaknesses, with suitability that can vary between different circumstances and by preferences of the patient and health-care workers. It should be clear that even when utilized on a daily basis, SMS, nor any other form of digital interaction, cannot be expected to entirely replace in-person clinic appointments and various forms of in-person patient support. Instead, these interventions may help patients who are unable to attend in-person clinic visits regularly and flag problems as they arise. Daily pill reminders have not shown increased efficacy when compared with the standard-of-care, and one needs to think beyond automated pill reminders when considering SMS [39].
3.1. Logistics considerations
Two critical logistical factors in determining choice of digital technology for TB programs are smartphone access and broadband internet availability. In areas with the highest TB burden, broadband internet speed may be too slow and unreliable, and persons with TB often cannot afford smartphones, making implementation of nationwide VOT unrealistic in most settings. Currently, SMS is the most accessible, affordable, and scalable digital approach because it can operate without mobile broadband internet coverage. This is likely to continue far into the future in the most resource-limited settings. In regions where reliable (mobile) internet connection, smartphones and tablet computers are widely available, SMS can complement VOT. For example, for persons whose TB treatment is going well, SMS provides a cheaper and less intrusive means for ongoing communication and support, which can always be “escalated” to VOT or more frequent in-person support visits if needed.
3.2. Privacy and security
There are a number of privacy and ethical issues to consider before implementing voice calls, SMS, or other digital technologies into regular TB patient care. Digital technology interventions are premised upon the regular observation of a person's behaviour, which itself raises a number of ethical issues related to how the data is handled [59]. The form and degree of intrusiveness (i.e. intensity) differs between technologies, varying from receiving a daily SMS text message to which a patient may choose to reply, to the video observation or recording of the patients taking their medication.
While there are benefits of recording pill intake and increased opportunities to interact with the patients, there are also potential downsides. Patients may experience the feeling of coercion, loss of control, a sense of being tracked and distrusted, and concerned with confidentiality [18]. There may even be legal issues surrounding adherence and communicable disease treatment in some jurisdictions for which adherence data could play unforeseen roles. Many national and local health jurisdictions have developed strategic plans, standards, and guidelines to help address many of the issues around privacy and security [18]. In addition, these issues should be discussed at length with the patients, who may have very divergent views in terms of external monitoring.
3.3. Directions for future research
Longer-term acceptability has been demonstrated with weekly SMS and phone support of patients undertaking HIV treatment [60], [61] but this has yet to been studied in people with active TB or LTBI. Interactive SMS communication with patients has the potential to triage patient care in real-time, thereby enhancing the quality and efficiency of patient support between in-person clinical and outreach visits [20], [21]. Future investigation with SMS-based strategies may be beneficial; to evaluate how SMS can be channelled in reaching hard-to-reach patients, and to perhaps incorporate and/or integrate with other incentive interventions such as conditional cash transfers. Research evaluations such as pragmatic trial designs should also be explored for patient outcomes apart from adherence, such as completion of diagnostic evaluation. Qualitative or mixed-methods studies are also needed to inform how SMS-based care can improve behaviors and enable adherence. Economic evaluations (i.e. cost-effectiveness analysis and budget-impact analysis) that can assess the value for money and affordability of these mobile interventions will facilitate the decision-making of policymakers interested in adopting these patient-centered care solutions.
Moreover, provision and financing of SMS-based digital health services can either be provided publicly or via public-private partnerships. Opportunities may be created by other services available on mobile phones; an example of this may include mobile banking (mBanking) and mobile money transfer (e.g. M-TIBA and mPESA in Kenya) [62], [63], [64]. Digital technologies can be thought of as complementary interventions.
TB patients could receive dynamic care that is responsive to individualized needs; to monitor and manage their risk of adverse reactions; to adapt when they move or travel to remote locations; to adapt when they experience other events that may disrupt their daily treatment. For example, with SMS, voice and VOT integrated together, an adaptive intervention strategy may be formed and delivered as a holistic, supportive care model. Future investigations should approach digital technologies for TB patient care as multi-stage decision problems and evaluate a sequence of treatment support strategies that can be adapted based on the individual's needs over time.
4. Conclusion
TB is a condition that disproportionately affects the world's poor; accordingly, digital health solutions need to ensure they reach vulnerable and low-income people now and into the future. SMS is the most pervasive digital communication modality, with the potential to improve the quality of care and medication adherence in people with active TB and LTBI. Supporting infrastructure for SMS and voice communications via mobile phones already exists in regions with the highest TB burden and could potentially be the most affordable and timely to implement. Additional research is required to develop implementation strategies that ensure maximal reach, impact, and patient value. The increasing range of technologies available to assist treatment adherence is conducive to the goal of establishing holistic, patient-centered differentiated care models for TB. Digital technologies may perform best when they empower the patient. They are not an end-to-end solution in care, but when used well, they offer unique opportunities to strengthen health systems and improve patient care, moving the global agenda toward the End TB goals.
Conflict of interest
Regarding author Dr. Richard Lester. Dr. Lester is co-founder of a non-profit organization, WelTel mHealth Society, and a private company, WelTel Incorporated. Dr. Richard Lester has financial as well as professional interests in both organizations. None of the other authors have conflicts to declare. You are entitled to ask for more information about this potential for benefit from Dr. Lester. For inquiries, please contact rlester@mail.ubc.ca Funds to WelTel Inc. do not cover any direct research costs. Dr. Lester does not have a financial relationship with the funders of this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. RTL and JCJ are supported by Michael Smith Foundation for Health Research Scholar Awards. RTL is supported by the Canadian Institutes of Health Research Foundation Scheme grant which assisted with time on this work. JJHP is supported by Mitacs Accelerate Program.
Contributor Information
Richard Lester, Email: rlester@mail.ubc.ca.
Jay JH Park, Email: jayhpark1@alumni.ubc.ca.
Lena M. Bolten, Email: lena.bolten@ubc.ca.
Allison Enjetti, Email: allison.enjetti@ubc.ca.
James C. Johnston, Email: james.johnston@bccdc.ca.
Kevin Schwartzman, Email: kevin.schwartzman@mcgill.ca.
Binyam Tilahun, Email: binyam.chakilu@uog.edu.et.
Reference
- 1.World Health Organization; Geneva: 2017. http://www.who.int/tb/publications/global_report/en/ accessed 4 April 2018. [Google Scholar]
- 2.Guidelines for the treatment of drug-susceptible tuberculosis and patient care, 2017 update. Geneva: World Health Organization; 2017 (http://www.who.int/tb/publications/2017/dstb_guidance_2017/en/, accessed 2 April 2018).
- 3.Alsdurf H, Hill PC, Matteelli A, Getahun H, Menzies D. The cascade of care in diagnosis and treatment of latent tuberculosis infection: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(11):1269–1278. doi: 10.1016/S1473-3099(16)30216-X. [DOI] [PubMed] [Google Scholar]
- 4.Pablos-Mendez A, Knirsch CA, Barr RG, Lerner BH, Frieden TR. Nonadherence in tuberculosis treatment: predictors and consequences in New York City. Am J Med. 1997;102(2):164–170. doi: 10.1016/s0002-9343(96)00402-0. [DOI] [PubMed] [Google Scholar]
- 5.Pablos-Mendez A, Sterling TR, Frieden TR. The relationship between delayed or incomplete treatment and all-cause mortality in patients with tuberculosis. JAMA. 1996;276(15):1223–1228. doi: 10.1001/jama.1996.03540150025026. [DOI] [PubMed] [Google Scholar]
- 6.Kliiman K, Altraja A. Predictors and mortality associated with treatment default in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2010;14(4):454–463. [PubMed] [Google Scholar]
- 7.Garner P, Smith H, Munro S, Volmink J. Promoting adherence to tuberculosis treatment. Bull World Health Organ. 2007;85(5):404–406. doi: 10.2471/06.035568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7):e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toczek A, Cox H, du Cros P, Cooke G, Ford N. Strategies for reducing treatment default in drug-resistant tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2013;17(3):299–307. doi: 10.5588/ijtld.12.0537. [DOI] [PubMed] [Google Scholar]
- 10.Uplekar M. The stop TB strategy: building on and enhancing DOTS to meet the TB-related millennium development goals. WHO. 2006 [Google Scholar]
- 11.World Health Organization. The five elements of DOTS. 2007. www.who.int/tb/dots/whatisdots/en/index.html(accessed May 17M 2018ay 17 2018,).
- 12.Zúñiga ML, Collins K, Muñoz F. A qualitative study exploring stakeholder perceptions of video directly observed therapy for monitoring tuberculosis treatment in the US-Mexico border region. J Mob Tech Med. 2016;5(2):12–23. [Google Scholar]
- 13.Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD003343.pub3. CD003343. [DOI] [PubMed] [Google Scholar]
- 14.Karumbi J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database Syst Rev. 2015;(5) doi: 10.1002/14651858.CD003343.pub4. CD003343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GSMA Intelligence. The mobile economy Africa 2016. 2016. https://www.gsma.com/mobileeconomy/africa/(accessed 16 April 2017).
- 16.GSMA Intelligence. The mobile economy 2018. 2018. https://www.gsma.com/mobileeconomy/wp-content/uploads/2018/02/The-Mobile-Economy-Global-2018.pdf(accessed 2 April 2018).
- 17.Meloan M, Iacopino P. Scaling digital health in developing markets: opportunities and recommendations for mobile operators and other stakeholders. London: GSMA. 2017 https://www.gsmaintelligence.com/research/?file=c581aa43bdb7b7d236bb937698c2d6fd&download accessed 2 April 2018. [Google Scholar]
- 18.World Health Organization . 2017. Handbook for the use of digital technologies to support tuberculosis medication adherence. [Google Scholar]
- 19.Pathmanathan I, Pevzner E, Cavanaugh J, Nelson L. Addressing tuberculosis in differentiated care provision for people living with HIV. Bull World Health Org. 2017;95(1):3. doi: 10.2471/BLT.16.187021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lester RT, Ritvo P, Mills EJ. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 21.Lester RT. Ask, don't tell - mobile phones to improve HIV care. N Engl J Med. 2013;369(19):1867–1868. doi: 10.1056/NEJMc1310509. [DOI] [PubMed] [Google Scholar]
- 22.Statistica. Mobile messaging volumes in the U.S. from 2004 to 2014 (in billion messages). https://www.statista.com/statistics/215776/mobile-messaging-volumes-in-the-us/(accessed 21 April 2018).
- 23.SMSGlobal. The impact of SMS on email open rates. https://thehub.smsglobal.com/the-impact-of-sms-on-email-open-rates(accessed 20 April 2018).
- 24.Pew Research Center. For teens, phone calls are reserved for closer relationships. http://www.pewresearch.org/fact-tank/2015/08/17/for-teens-phone-calls-are-reserved-for-closer-relationships/(accessed 01 May 2018).
- 25.Pew Research Center. Americans and text messaging. http://www.pewinternet.org/∼/media//Files/Reports/2011/Americans%20and%20Text%20Messaging.pdf.
- 26.Wakadha H, Chandir S, Were EV. The feasibility of using mobile-phone based SMS reminders and conditional cash transfers to improve timely immunization in rural Kenya. Vaccine. 2013;31(6):987–993. doi: 10.1016/j.vaccine.2012.11.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grantome. Combined phone based video DOT and mobile payments for TB treatment in Cambodia2017. http://grantome.com/grant/NIH/R21-TW010592-01(accessed 23 May 2018).
- 28.URC. Mobile cash helps patients, providers fight TB.2015. http://www.urc-chs.com/news/mobile-cash-helps-patients-providers-fight-tb(accessed 23 May 2018).
- 29.Free C, Hoile E, Robertson S, Knight R. Three controlled trials of interventions to increase recruitment to a randomized controlled trial of mobile phone based smoking cessation support. Clin Trials. 2010;7(3):265–273. doi: 10.1177/1740774510367687. [DOI] [PubMed] [Google Scholar]
- 30.Liao Y, Wu Q, Tang J. The efficacy of mobile phone-based text message interventions ('Happy Quit') for smoking cessation in China. BMC Public Health. 2016;16(1):833. doi: 10.1186/s12889-016-3528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley W, Augustson EM. Mobile phone-based smoking cessation interventions increase long-term quit rates compared with control programmes, but effects of the interventions are heterogeneous. Evid Based Nurs. 2013;16(4):108–109. doi: 10.1136/eb-2012-101204. [DOI] [PubMed] [Google Scholar]
- 32.Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4 doi: 10.1002/14651858.CD006611.pub4. CD006611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ybarra ML, Jiang Y, Free C, Abroms LC, Whittaker R. Participant-level meta-analysis of mobile phone-based interventions for smoking cessation across different countries. Prev Med. 2016;89:90–97. doi: 10.1016/j.ypmed.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2012;(3) doi: 10.1002/14651858.CD009756. CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD007457.pub2. CD007457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ngwatu BK, Nsengiyumva NP, Oxlade O. The impact of digital health technologies on tuberculosis treatment: a systematic review. Eur Respir J. 2018;51(1) doi: 10.1183/13993003.01596-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nglazi MD, Bekker LG, Wood R, Hussey GD, Wiysonge CS. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: a systematic review. BMC Infect Dis. 2013;13:566. doi: 10.1186/1471-2334-13-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nglazi MD, Bekker LG, Wood R, Hussey GD, Wiysonge CS. Mobile phone text messaging for promoting adherence to anti-tuberculosis treatment: a systematic review protocol. Syst Rev. 2013;2:6. doi: 10.1186/2046-4053-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wald DS, Butt S, Bestwick JP. One-way versus two-way text messaging on improving medication adherence: meta-analysis of randomized trials. Am J Med. 2015;128(10):1139. doi: 10.1016/j.amjmed.2015.05.035. e1-5. [DOI] [PubMed] [Google Scholar]
- 40.Mills EJ, Lester R, Thorlund K. Interventions to promote adherence to antiretroviral therapy in Africa: a network meta-analysis. Lancet HIV. 2014;1(3):e104. doi: 10.1016/S2352-3018(14)00003-4. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kanters S, Park JJ, Chan K. Interventions to improve adherence to antiretroviral therapy: a systematic review and network meta-analysis. Lancet HIV. 2017;4(1):e31–e40. doi: 10.1016/S2352-3018(16)30206-5. [DOI] [PubMed] [Google Scholar]
- 42.Mohammed S, Glennerster R, Khan AJ. Impact of a daily SMS medication reminder system on tuberculosis treatment outcomes: a randomized controlled trial. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0162944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bardosh KL, Murray M, Khaemba AM, Smillie K, Lester R. Operationalizing mHealth to improve patient care: a qualitative implementation science evaluation of the WelTel texting intervention in Canada and Kenya. Global Health. 2017;13(1):87. doi: 10.1186/s12992-017-0311-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu Q, Abba K, Alejandria MM, Sinclair D, Balanag VM, Lansang MA. Reminder systems to improve patient adherence to tuberculosis clinic appointments for diagnosis and treatment. Cochrane Database Syst Rev. 2014;(11) doi: 10.1002/14651858.CD006594.pub3. CD006594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chiang N, Guo M, Amico KR, Atkins L, Lester RT. Interactive two-way mHealth interventions for improving medication adherence: an evaluation using the behaviour change wheel framework. JMIR mHealth uHealth. 2018;6(4):e87. doi: 10.2196/mhealth.9187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mills EJ, Lester R, Ford N. Adherence to antiretroviral therapy: supervision or support. Lancet Infect Dis. 2012;12(2):97–98. doi: 10.1016/S1473-3099(11)70354-1. [DOI] [PubMed] [Google Scholar]
- 47.Liu X, Lewis JJ, Zhang H. Effectiveness of electronic reminders to improve medication adherence in tuberculosis patients: a cluster-randomised trial. PLoS Med. 2015;12(9) doi: 10.1371/journal.pmed.1001876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bediang G, Stoll B, Elia N, Abena JL, Geissbuhler A. SMS reminders to improve adherence and cure of tuberculosis patients in Cameroon (TB-SMS Cameroon): a randomised controlled trial. BMC Public Health. 2018;18(1):583. doi: 10.1186/s12889-018-5502-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bediang G, Stoll B, Elia N. SMS reminders to improve the tuberculosis cure rate in developing countries (TB-SMS Cameroon): a protocol of a randomised control study. Trials. 2014;15:35. doi: 10.1186/1745-6215-15-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belknap R, Holland D, Feng PJ. Self-administered versus directly observed once-weekly isoniazid and Rifapentine treatment of latent tuberculosis infection: a randomized trial. Ann Intern Med. 2017;167(10):689–697. doi: 10.7326/M17-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fang XH, Guan SY, Tang L. Effect of short message service on management of pulmonary tuberculosis patients in Anhui Province, China: a prospective, randomized, controlled study. Med Sci Monit. 2017;23:2465–2469. doi: 10.12659/MSM.904957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patel AR, Campbell JR, Sadatsafavi M. Burden of non-adherence to latent tuberculosis infection drug therapy and the potential cost-effectiveness of adherence interventions in Canada: a simulation study. BMJ Open. 2017;7(9) doi: 10.1136/bmjopen-2016-015108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van der Kop ML, Memetovic J, Patel A. The effect of weekly text-message communication on treatment completion among patients with latent tuberculosis infection: study protocol for a randomised controlled trial (WelTel LTBI) BMJ Open. 2014;4(4) doi: 10.1136/bmjopen-2013-004362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Masini E, Hanson C, Ogoro J. Using patient-pathway analysis to inform a differentiated program response to tuberculosis: the case of Kenya. J Infect Dis. 2017;216(suppl_7):S714–SS23. doi: 10.1093/infdis/jix381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.PATH.Using mHealth to combat multidrug-resistant tuberculosis across Vietnam2017. http://www.path.org/publications/files/ID_vietnam_mobile_tb2017_fs.pdf(accessed 23 May 2018).
- 56.Kitsiou S, Pare G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pal K, Dack C, Ross J. Digital health interventions for adults with type 2 diabetes: qualitative study of patient perspectives on diabetes self-management education and support. J Med Internet Res. 2018;20(2):e40. doi: 10.2196/jmir.8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Choudhry NK, Krumme AA, Ercole PM. Effect of reminder devices on medication adherence: the REMIND randomized clinical trial. JAMA Intern Med. 2017;177(5):624–631. doi: 10.1001/jamainternmed.2016.9627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.World Health Organization; Geneva: 2017. http://www.who.int/tb/publications/2017/ethics-guidance/en/ accessed 2 April 2018. [Google Scholar]
- 60.King E, Kinvig K, Steif J. Mobile text messaging to improve medication adherence and viral load in a vulnerable canadian population living with human immunodeficiency virus: a repeated measures study. J Med Internet Res. 2017;19(6):e190. doi: 10.2196/jmir.6631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Murray MC, O'Shaughnessy S, Smillie K. Health care providers' perspectives on a weekly text-messaging intervention to engage HIV-positive persons in care (WelTel BC1) AIDS Behav. 2015;19(10):1875–1887. doi: 10.1007/s10461-015-1151-6. [DOI] [PubMed] [Google Scholar]
- 62.TIBU. In: The center for health market innovations. http://healthmarketinnovations.org/program/tibu(accessed 20 April 2018).
- 63.CNN.M-Pesa: Kenya's mobile money success story turns 10. 2017. https://www.cnn.com/2017/02/21/africa/mpesa-10th-anniversary/index.html(accessed 23 May 2018).
- 64.PharmAccess Foundation. "M-TIBA is truly leapfrogging healthcare in Kenya". 2015. https://www.pharmaccess.org/update/m-tiba-is-truly-leapfrogging-healthcare-in-kenya/(accessed 23 May 2018).
- 65.Branson CE, Clemmey P, Mukherjee P. Text message reminders to improve outpatient therapy attendance among adolescents: a pilot study. Psychol Serv. 2013;10(3):298. doi: 10.1037/a0026693. [DOI] [PubMed] [Google Scholar]
- 66.Pena-Robichaux V, Kvedar JC, Watson AJ. Text messages as a reminder aid and educational tool in adults and adolescents with atopic dermatitis: a pilot study. Dermatol Res Pract. 2010;2010 doi: 10.1155/2010/894258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernández-Aranda F, Jiménez-Murcia S, Santamaría JJ. Video games as a complementary therapy tool in mental disorders: PlayMancer, a European multicentre study. J Mental Health. 2012;21(4):364–374. doi: 10.3109/09638237.2012.664302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anhøj J, Møldrup C. Feasibility of collecting diary data from asthma patients through mobile phones and SMS (short message service): response rate analysis and focus group evaluation from a pilot study. J Med Internet Res. 2004;6(4) doi: 10.2196/jmir.6.4.e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11(2):99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Vera MA, Sadatsafavi M, Tsao NW. Empowering pharmacists in asthma management through interactive SMS (EmPhAsIS): study protocol for a randomized controlled trial. Trials. 2014;15(1):488. doi: 10.1186/1745-6215-15-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fund The Global. A toolkit for health facilities: differentiated care for HIV and tuberculosis. Geneva, Switzerland: The Global Fund. 2015 [Google Scholar]
- 72.Johnston JC, van der Kop ML, Smillie K. The effect of text messaging on latent tuberculosis treatment adherence: a randomised controlled trial. Eur Respir J. 2018;51(2) doi: 10.1183/13993003.01488-2017. [DOI] [PubMed] [Google Scholar]
- 73.van der Kop ML, Memetovic J, Smillie K. Use of the WelTel mobile health intervention at a tuberculosis clinic in British Columbia: a pilot study. J Mob Tech Med. 2013;2(3):7–14. [Google Scholar]
- 74.Chiang N, Guo M, Amico KR, Atkins L, Lester RT. Interactive two-way mHealth interventions for improving medication adherence: an evaluation using the behaviour change wheel framework. JMIR mHealth uHealth. 2018;6(4):e87. doi: 10.2196/mhealth.9187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.van der Kop ML, Muhula S, Nagide PI. Effect of an interactive text-messaging service on patient retention during the first year of HIV care in Kenya (WelTel Retain): an open-label, randomised parallel-group study. Lancet Public Health. 2018;3(3):e143–ee52. doi: 10.1016/S2468-2667(17)30239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Government Technology Washington, D.C., enjoys fastest average internet speeds in nation. Rep Says. 2015 http://www.govtech.com/network/Washington-DC-Enjoys-Fastest-Average-Internet-Speeds-in-Nation-Report-Says.html (accessed 21 May 2018) [Google Scholar]