Abstract
For many patients in India, pharmacies are their first point of contact, where most drugs, including antibiotics, can be purchased over-the-counter (OTC). Recent standardised (simulated) patient studies, covering four Indian cities, provide new insights on how Indian pharmacies manage patients with suspected or known tuberculosis. Correct management of the simulated patients ranged from 13% to 62%, increasing with the certainty of the TB diagnosis. Antibiotics were frequently dispensed OTC to patients, with 16% to 37% receiving such drugs across the cases. On a positive note, these studies showed that no pharmacy dispensed first-line anti-TB drugs. Engagement of pharmacies is important to not only improve TB detection and care, but also limit the abuse of antibiotics.
Tuberculosis (TB) is the world's top infectious disease killer, accounting for an estimated 1.8 million deaths in 2015 [1]. Over a quarter of those deaths were in India, which carries the largest burden of the disease, with worryingly high rates of MDR-TB. Early symptoms of pulmonary TB are common, vague and persistent, leading infected individuals to seek care from a variety of local primary care providers [2]. A study of patient pathways to care in 13 countries showed that nearly 60% of TB patients begin their care seeking in the private or informal sectors, including pharmacies [3].
Pharmacies are highly accessible in India due to their vast numbers (around 800,000 nationally) [4], long opening hours and absence of user fees [5]. For many patients, pharmacies may be their first point of contact, where most drugs, including antibiotics, can be purchased over-the-counter (OTC).
What exactly do pharmacists do when they encounter patients with suspected TB, or confirmed TB? We now have reliable, consistent data from two standardised (simulated) patient studies, across 4 Indian cities, on how Indian pharmacies manage such patients [6], [7]. Standardised patients (SPs), also called mystery clients, are widely considered to be the gold standard when it comes to measurement of actual practice [8], and SPs have been effectively used to assess quality of TB care in India, Kenya and China [9], [10], [11].
Together, the two SP studies of pharmacies in India presented three different presentations of TB to multiple pharmacies (Table 1). Management of the patients was benchmarked against guidelines for pharmacists from the Government of India and the Indian Pharmaceutical Association [12]. Referral to a healthcare provider without selling antibiotics or steroids was deemed ‘correct’ management (Table 1). Correct management that is evidence-based is a core element of quality of care. There are, of course, other elements such as user experience and patient outcomes. But these were not captured in the SP studies.
Table 1.
Specific case presentations of tuberculosis by standardised patients in Satyanarayana et al. [7] and Miller and Goodman [6].
| Satyanarayana et al 2016 (Lancet case 1) | Miller and Goodman 2017 (BMJGH case) | Satyanarayana et al 2016 (Lancet case 2) | |
|---|---|---|---|
| Case presentation (opening statement by the simulated patient) | `I have cough and fever that is not getting better. Please give me some medicine' | `I have had cough and some fever for 3–4 weeks. We have had a relative staying with us who has TB. Can you suggest something?' | `I am having cough for nearly a month now and also have fever.' While showing a positive sputum report to the chemist, the patient continues, ‘I went to the government dispensary and they asked me to get my sputum tested. I have this report. Can you please give me some medicine?’ |
| Definition of ‘correct’ management | Verbal or written referral to a DOTS centre or a health-care provider without dispensing any antibiotics (including anti-tuberculosis drugs and fluoroquinolones) or steroids | Referral to TB clinic or other healthcare provider for sputum examination. No sale of antibiotics (including anti-TB medication) or steroids | Verbal or written referral to a DOTS centre or a health-care provider without dispensing any antibiotics (including anti-tuberculosis drugs and fluoroquinolones) or steroids |
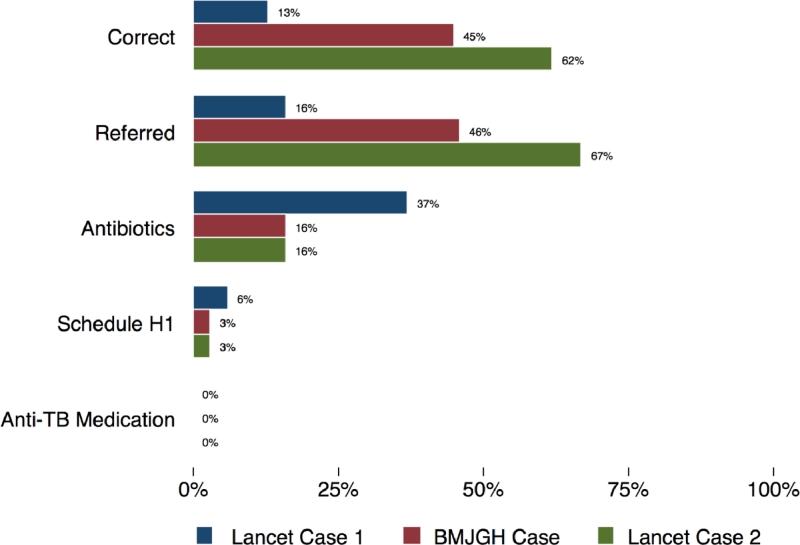
Fig. 1 shows that correct management of the SPs ranged from 13% to 62%, increasing with the certainty of the TB diagnosis. Those presenting with non-specific symptoms of cough and fever, consistent with many differential diagnoses, were correctly managed only in 13% of the SP interactions. However, the suggestion of TB, due to close contact with a relative with TB, increased this figure to 45%. Further still, a confirmed positive sputum test ensured that almost two-thirds of SPs were managed correctly.
Fig. 1.
Management of 3 different case presentations of tuberculosis by pharmacies in urban India. For definition of ‘correct management’ see Table 1.
Antibiotics were frequently dispensed OTC to patients, with 16%–37% receiving such drugs across the cases. However, three positive findings emerged. First, antibiotic use more than halved when SPs explained they had been in contact with an infected individual or had a confirmed diagnosis, compared to those only presenting symptoms suggestive of TB. Second, the use of restricted Schedule H1 medicines was low in all cities. Third, out of 1533 SP encounters across 4 cities, not a single pharmacy dispensed first-line anti-TB medications without a prescription.
Successful TB control efforts hinge on early diagnosis and appropriate treatment. The results of these recent SP studies are consistent across 4 cities, and show that urban pharmacists do a poor job of asking patients with TB symptoms relevant questions, and referring them for TB testing. These practices likely delay TB diagnosis. However, a pure profit motive whereby pharmacists want to sell drugs to patients at all costs is also a poor explanation of observed behavior. Management varied with the certainty of the diagnosis and pharmacists were willing to forego sales in favor of referring patients with a stronger suggestion of TB. Therefore, training pharmacy staff to recognise the symptoms of TB could improve on the current situation.
In terms of treatment, these studies demonstrate that pharmacists do not give OTC first-line anti-TB drugs and are likely not a major driver of drug resistant TB in the country. The limited use of H1 medicines (a restricted category of medicines, mainly comprising third and fourth generation cephalosporins, carbapenems, newer fluoroquinolones and first- and second-line anti-tuberculosis drugs) also suggests that the introduction of this regulation has had an effect.
Historically, community pharmacists have not been engaged in national policy discussions around TB control. However, recent years have seen some progress in this area culminating in the memorandum of understanding between the Central TB Division and the Indian Pharmaceutical Association, the All India Organisation of Chemists and Druggists, the Pharmacy Council of India and the SEARPharm forum to ``engage pharmacists in RNTCP for TB Care and Control in India''. Over the past decade, there have been projects focused on engaging pharmacists in India [13]. But such public-private mix (PPM) partnerships are yet to reach scale [14]. In the most recent draft of the National Strategic Plan for Tuberculosis Elimination 2017–2025, there are no budgets for engaging retail pharmacists, but mapping of pharmacies and their engagement is surveillance and social mobilization is envisioned [15].
It is widely believed that knowledge may not be sufficient to ensure good pharmacy practice as public health goals may not necessarily align with the financial interests of private sector pharmacists [16], [17]. Our findings suggest that this view needs to be nuanced: pharmacists do deviate from accepted norms when diagnosis is unknown or uncertain. But their behavior improves markedly when diagnoses are more apparent. And their deviations are tightly bound by implicit norms that restrict the use of anti-TB medicines and Schedule H1 antibiotics.
In conclusion, we need to think beyond traditional models that expect pharmacists to be able to recognize who may have TB and passively refer TB patients to the public sector [18]. Pharmacists can be engaged for a variety of TB services across the cascade of care, and private pharmacies have been actively engaged in novel PPM models in India that have dramatically increased private sector TB case notifications in the country and improved quality of TB care in the private sector [19]. In addition, a supportive and effective regulatory environment may be as important to help curb the OTC sale of unnecessary antibiotics, and decrease diagnostic delays for millions of TB patients.
Conflicts of interest
None
Acknowledgements
RM acknowledges the support of the Economic and Social Research Council. MP acknowledges grant funding support from IC-IMPACTS, Grand Challenges Canada, and the Bill & Melinda Gates Foundation. The authors are grateful to Ada Kwan, Ben Daniels, Srinath Satyanarayana and rest of the QuTUB team (Quality of Tuberculosis Care; https://www.qutubproject.org/) for their support.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jctube.2017.11.002.
Appendix. Supplementary materials
References
- 1.World Health Organization . World Health Orgaization; Geneva: 2016. Global tuberculosis report 2016. [Google Scholar]
- 2.Kapoor S.K., Raman A.V., Sachdeva K.S., Satyanarayana S. How did the TB patients reach DOTS services in Delhi? A study of patient treatment seeking behavior. PloS One. 2012;7(8):e42458. doi: 10.1371/journal.pone.0042458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chin D.P., Hanson C.L. Finding the missing tuberculosis patients. J Infect Dis. 2017;216(Suppl 7):S675–S678. doi: 10.1093/infdis/jix368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.IMS consulting group . IMS Consulting Group; New York: 2014. Assessing the growth of pharmacy chains. [Google Scholar]
- 5.Smith F. The quality of private pharmacy services in low and middle-income countries: a systematic review. Pharm World Sci. 2009;31(3):351–361. doi: 10.1007/s11096-009-9294-z. [DOI] [PubMed] [Google Scholar]
- 6.Miller R., Goodman C. Do chain pharmacies perform better than independent pharmacies? Evidence from a standardised patient study of the management of childhood diarrhoea and suspected tuberculosis in urban India. BMJ Global Health. 2017;0 doi: 10.1136/bmjgh-2017-000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satyanarayana S., Kwan A., Daniels B. Use of standardised patients to assess antibiotic dispensing for tuberculosis by pharmacies in urban India: a cross-sectional study. Lancet Infect Dis. 2016;16(11):1261–1268. doi: 10.1016/S1473-3099(16)30215-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cazabon D., Alsdurf H., Satyanarayana S. Quality of tuberculosis care in high burden countries: the urgent need to address gaps in the care cascade. Int J Infect Dis. 2017;56:111–116. doi: 10.1016/j.ijid.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das J., Kwan A., Daniels B. Use of standardised patients to assess quality of tuberculosis care: a pilot, cross-sectional study. Lancet Infect Dis. 2015;15(11):1305–1313. doi: 10.1016/S1473-3099(15)00077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daniels B., Dolinger A., Bedoya G. Use of standardised patients to assess quality of healthcare in Nairobi, Kenya: a pilot, cross-sectional study with international comparisons. BMJ Global Health. 2017;2 doi: 10.1136/bmjgh-2017-000333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sylvia S., Xue H., Zhou C. Tuberculosis detection and the challenges of integrated care in rural China: A cross-sectional standardized patient study. PLoS Med. 2017;14(10) doi: 10.1371/journal.pmed.1002405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Central TB Division MoFW, Government of India and Indian Pharmaceutical Association. Revised National Tuberculosis Control Programme training module for community pharmacists. 2013.
- 13.Lilly MDR-TB Partnership. Creating champions of change. Enrolling community pharmacists in a national tubercuclosis control iniative, 2014.
- 14.Konduri N., Delmotte E., Rutta E. Engagement of the private pharmaceutical sector for TB control: rhetoric or reality? J Pharm Policy Pract. 2017;10(1):6. doi: 10.1186/s40545-016-0093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Central TB Division MoFW, Government of India. National strategic plan for tuberculosis elimination 2017–2025 New Delhi, India 2017.
- 16.Goel P., Ross-Degnan D., Berman P., Soumerai S. Retail pharmacies in developing countries: a behavior and intervention framework. Soc Sci Med. 1996;42(8):1155–1161. doi: 10.1016/0277-9536(95)00388-6. [DOI] [PubMed] [Google Scholar]
- 17.Miller R., Goodman C. Performance of retail pharmacies in low-and middle-income Asian settings: a systematic review. Health Policy Plann. 2016;31(7):940–953. doi: 10.1093/heapol/czw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daftary A., Jha N., Pai M. Enhancing the role of pharmacists in the cascade of tuberculosis care. J Epidemiol Global Health. 2017;7:1–4. doi: 10.1016/j.jegh.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sulis G., Pai M. Missing tuberculosis patients in the private sector: business as usual will not deliver results. Public Health Action. 2017;7(2):80–81. doi: 10.5588/pha.17.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.