Abstract
Tuberculosis (TB) in Korea remains a serious health problem with an estimated 77 per 100,000 incidence rate for 2016. This makes Korea as the only OECD country with high incidence of TB. The government has increased budgets and strengthened patient management policies since 2011. The management of latent tuberculosis was added to the response with strengthened and extensive contact investigations in the five-year tuberculosis control plan (2013–2017) and implementation was established in 2013. Due to these efforts Korea has achieved an average 5.2% reduction annually in tuberculosis incidence rate between 2011 and 2016. To further expedite the reduction of the TB burden the government has introduced additional measures including mandatory screening of latent tuberculosis infection for community workers in congregate settings including daycare centers for children, kindergarten, and teachers in schools and health care workers in clinics and hospitals to solve the problems identified through contact investigations in 2017.
Providing high quality free diagnosis and treatment of active TB including for multidrug resistant TB combined with active contact investigations is the mainstay of the current programmatic response in Korea. However, the limitation of existing tools for LTBI pose challenge including absence of best mechanism for effective communication with professionals and the public, the need for at least 3 months of treatment and the risk of side effects. Developing effective tools will help to overcome these challenges.
Keywords: Tuberculosis, Latent tuberculosis infection, End TB, Contact investigations, Epidemiology
1. Background
The disease burden of tuberculosis (TB) is high with a TB incidence of 10.4 million in 2016 and 1.7 million deaths and estimated 490,000 developed multidrug-resistant TB (MDR-TB) in the world [1]. The World Health Organization (WHO) announced the END TB Strategy, which aims to end TB by 2035, reaching 90% reduction in TB incidence rate from a projected 100 cases/100,000 in 2015 to 10 cases/100,000 or less by 2035. Since 2000, the current global trend shows −1.5% reduction of incidence rate per year; to achieve the global target in the End TB strategy, the annual reduction rate of incidence should be 10% per year by 2025. To reach the 2035 targets with the incidence of 10 per 100,000 persons, introduction of new tools will be essential including a vaccine, new drugs, and treatment regimens for treatment of active TB disease and latent TB infection (LTBI) and a point of care test [2].
Since the establishment of the national TB control plan in 1955, Korea has implemented a TB control policy centered on public health centers. In addition, the National Tuberculosis Survey was conducted by the Korean National Tuberculosis Association, a non-profit non-governmental organization, over five years from 1965 to 1995. Since the establishment of the Tuberculosis Prevention Act in 1967, the government has enhanced its TB control program. With these efforts, the disease burden of TB decreased significantly. The prevalence of active TB was 5168 per 100,000 population in 1965, but, in 1995, that prevalence decreased to 767 per 100,000 population [3], [4]. From 2000, a web-based TB cases notification system, the Korean National Tuberculosis Surveillance System (KNTSS), replaced the National Tuberculosis Survey for monitoring the disease burden.
Although the TB rate has decreased significantly, Korea has one of the highest TB incidence and mortality rates among the OECD countries. According to the WHO's Global Tuberculosis Report, the incidence of TB was 100 persons per 100,000 population in 2011 [5] and decreased to 77 persons per 100,000 population in 2016. In 2016, the total number of cases reported was 39,245, and the number of new and relapse cases was 36,435 with an incidence rate of 77 persons per 100,000 population. The mortality rate was 5.1 persons per 100,000 population [6]. The WHO's TB incidence rate includes officially reported new and relapse cases as well as an estimate of non-notified TB cases.
Since 2011, Korea has strengthened its TB policy with strong political will and has shown a 5. 2% reduction annually in the incidence of newly reported TB cases from 2011to 2016. Here, we introduce Korea's TB policy including the LTBI control programs, which has intensified since 2013.
In Korea, there are two types of surveillance systems for TB: (1) a web-based TB case notification system and (2) vital registration systems.
-
(1)
The burden of TB is estimated based on the data collected through the Korean National Tuberculosis Surveillance System (KNTSS), a web-based system launched in August of 2000. According to the Tuberculosis Prevention Act, physicians should report to the public health center when they diagnose a TB case or a suspected TB case in private medical facilities or public health centers. The notification data include the patients’ personal information, examination results, treatments, and treatment outcomes. Completeness was evaluated using notifications reported within 365 days of the corresponding insurance claim. The completeness values were 90.0% in 2012, 93.0% in 2013, and 94.0% in 2014 [7].
-
(2)
All deaths must be reported to Statistics Korea within one month of their occurrence. The registered death data include information on age, gender, administrative district of residence, educational level, month of death, occupation, and marital status. Underlying causes of disease are coded in the data according to the International Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Death reporting is operated through the national-level electronic system.
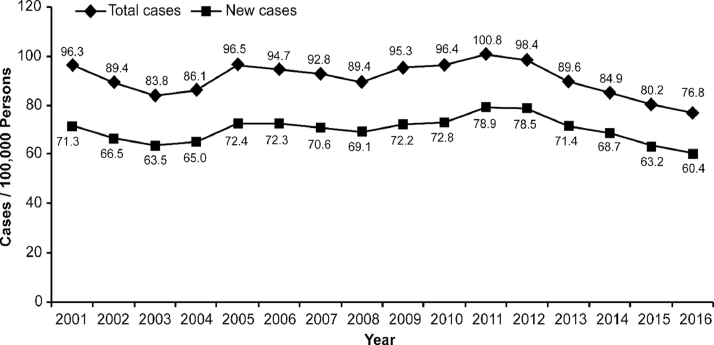
Based on the notification data from the KNTSS, the new TB notification rates from 2001 to 2016 have decreased since 2013. Rates per 100,000 population were 78.9 in 2011, 78.5 in 2012, 71.4 in 2013, 68.7 in 2014, 63.2 in 2015 and 60.4 in 2016 (Fig. 1). They decreased 5. 2% per year during 2011–2016. Age-standardized new TB notification rates per 100,000 population were 72.2 in 2011, 70.2 in 2012, 62.6 in 2013, 58.8 in 2014, 52.6 in 2015, and 48.8 in 2016. The national population in 2005 was used as standard population [8].
Fig. 1.
(New) TB notification rates, 2001–2016.
*Source: Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis in Korea. 2016.
The number of new TB notification in 2016 was 30,892; among them, 24,696 (79.9%) were pulmonary TB cases, and 6196 (20.1%) were extra-pulmonary TB cases. Among the pulmonary TB cases, 8812 (35.7%) were smear-positive pulmonary cases. Among the 30,892 new TB notification cases, 2405 (7.8%) were reported from the public health centers, and 28,487 (92.2%) were reported from the private medical facilities. Among the cases reported from the private medical facilities, only 756 were reported by clinics, and the other 27,731 cases were reported by general hospitals or hospitals.
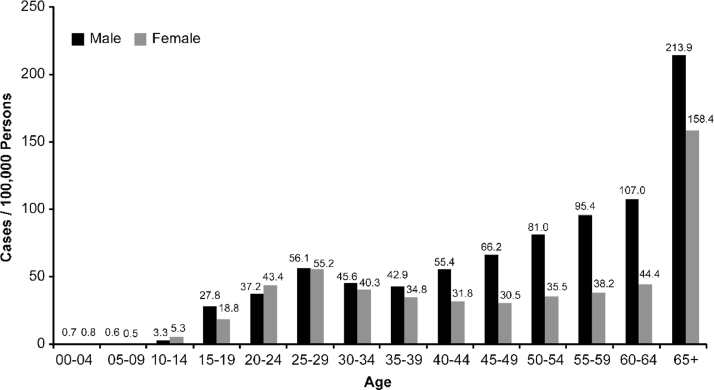
In 2016, the new TB notification rates were 70.0 per 100,000 population in men and 50.9 in women; the male incidence rate was 1.4 times higher than the female rate. The incidence rate increased in the 15–19 age group and peaked in the 25–29 age group, and it increased in those over 50 years old. The incidence rates for men and women over 65 were 213.9 and 158.4 per 100,000 population, respectively (Fig. 2). The peak in the young age group indicates that there might be ongoing transmission at the community level, especially in congregate settings like schools and workplaces.
Fig. 2.
(New) TB notification rates by gender and age, 2016.
*Source: Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis in Korea. 2016.
The numbers of new TB notifications were 39,557 in 2011, 39,545 in 2012, 36,089 in 2013, 34,869 in 2014, 32,181 in 2015, and 30,892 in 2016. Among them, the numbers of reported foreign-born new TB cases were 1007 in 2011, 1227 in 2012, 1420 in 2013, 1566 in 2014, 1589 in 2015, and 2123 in 2016. The proportion of foreign-born cases among new TB notification cases increased from 2.5% in 2011 to 6.9% in 2016, and the number of foreign-born new TB notification cases increased 2.1 times during the period of 2011 to 2016.
Patients with MDR-TB include those who have TB caused by Tubercle bacillus, which is resistant to more than two anti-TB drugs including isoniazid and rifampin. Extensively drug-resistant TB shows resistance to both of isoniazid and rifampin, more than one quinolone, and more than one of 3 injections (capreomycin, kanamycin, and amikacin). The numbers of MDR-TB reports were 975 in 2011, 1212 in 2012, 951 in 2013, 856 in 2014, 787 in 2015, and 852 in 2016. Among them, there were 140 extensively drug-resistant TB cases in 2011, 158 in 2012, 113 in 2013, 63 in 2014, 58 in 2015, and 59 in 2016.
2. The national TB control plan
In 1955, the Korean government announced a five-year TB Control Plan and carried out a BCG vaccination, X-ray screening for the patient detection, and a survey on the status of TB. From 1962, the BCG vaccination campaign, patient registration, and treatment program were performed in public health centers. Since 1963, one TB control staff has been assigned to 182 public health centers nationwide. Since the establishment of the Tuberculosis Prevention Act in 1967, the government has promoted a full-fledged TB control program [3].
Since then, the policy has been focused on the management of TB patients centered on public health centers. Although the number of TB patients treated in the private sector increased after the introduction of the National Health Insurance in 1989, there was lack of systematic management of patients who were treated in the private sector by pursuing TB policies centered on public health centers. In the 1980s, the proportions of patients treated at public health centers and in the private sector were around 75% and 25%, respectively. In 1995, the difference was narrowed to 53% and 47%, respectively. In 2001, the proportions of patients treated at public health centers (41%) and in the private sector (59%) were reversed. In 2008, 79% of patients were treated in the private sector, and only 21% were treated in public health centers. The rate of decline in TB patients slowed since 2000, and the paradigm of TB policy has begun to be reviewed. In 2006, the government announced the “2030 TB Elimination Plan” to combat TB and began to improve the government's TB control policy.
In 2011, the Korean government developed the “New 2020 Plan for Early TB Elimination.” Early detection of TB patients, successful treatment of patients, intensive care for high-risk groups, and boosting public relations were key strategies in that plan. In 2011, the legal basis was strengthened through amendment of the Tuberculosis Prevention Act. The Private-Public Mix cooperation project was implemented to provide comprehensive TB patient management, and the necessary budget was secured in 2011.
The Korea Centers for Disease Control and Prevention (KCDC) organized an international consultation meeting in August of 2011 to discuss the “New 2020 Plan for Early TB Elimination” and to define better strategies to control TB. Leading experts in TB from the WHO and U.S. Centers for Disease Control and Prevention in United States (USCDC) were invited, and Korean experts attended the meeting [9]. Challenges and strengths were reviewed, and action points were recommended during the meeting.
-
✓
The challenges identified were (1) a lack of systematic TB case holding in the private sector and largely unknown outcomes of TB cases treated in the private sector, (2) increasing burden of MDR-TB and a substantial proportion of MDR-TB patients defaulting during treatment, (3) insufficient management of high-risk groups, and (4) lack of infrastructure for a TB management system.
-
✓
The national TB program in the Republic of Korea has most essential elements in place and appears well structured with the following main strengths. (1) There is a clear and strong political commitment; the budget for TB control tripled recently to 40 million USD per year in 2011. (2) The new 2020 plan sets ambitious and bold goals. (3) A legal framework for TB control is in place. Legislation is largely in place to implement all measures, although, in some cases, the need for enforcement must be addressed. (4) The extension of universal social security coverage to MDR-TB cases will be considered a priority. (5) There is a very high level of technical expertise in-country. (6) Major obstacles and challenges have been analyzed and acknowledged in the new 2020 plan. (7) The new 2020 plan is epidemiologically driven. (8) The new 2020 plan will be promoted with other sectors, including the Ministry of Justice for prisons and other sectors for immigrants and highly susceptible groups.
-
✓
Based on the analysis of challenges and strengths, the following action points were recommended: (1) Expansion of contact investigation and LTBI treatment; (2) Expansion of public-private cooperation projects; (3) Establishment of a TB management system for vulnerable groups including homeless people; (4) Improvement of diagnostic system for early case detection; (5) Research and development for TB management; (6) Private-government development of TB standard guidelines; (7) Support for improving the efficiency of treatment for intractable MDR-TB patients; and (8) Establishment of an integrated TB information system for monitoring and evaluating the TB program, including patient management.
Based on the recommendations, the Ministry of Health and Welfare and KCDC developed the first “Five-Year (2013–2017) Plan for TB Elimination” for the Republic of Korea (hereafter “Five-Year Plan”) in 2013. The plan was established under Article 5 of the Tuberculosis Prevention Act. Under the law, regional governments also must establish their own plan in alignment with the Five-Year Plan at the central level. The Five-Year Plan aimed to achieve an incidence of TB less than 50 per 100,000 people by 2020 (the level was 100 per 100,000 people in 2011) through early detection of TB patients, comprehensive TB patient management, and enhancement of the infrastructure for TB control [10]. The Korean government increased its budget by more than three times in 2011 compared to the previous year. In 2010, the budget for TB control at the central government level was 13 million USD, and it increased to 40 million USD.
2.1. Patient management (Comprehensive TB patient management)
To ensure patient support for treatment adherence including Directly Observed Therapy for general TB and MDR-TB patients, Korea strengthened private–public cooperation and collaboration. The Public– Private Mix (PPM) collaboration pilot project was introduced in 2007. PPM collaboration was expanded from 11 hospitals in 2007 to 128 hospitals in 2016. Through PPM collaboration, trained nurses dispatched to private hospitals are responsible for patient education and monitoring of treatment adherence. Sixty-six percent of new TB patients were treated at PPM collaboration hospitals in 2016.
In 2017, 236 public health officials in 254 public health centers in municipalities and more than 210 nurses at 127 PPM hospitals provide patient counseling and education to increase treatment adherence. Comprehensive management of TB patients such as case studies, administration of medication during the infectious period, management of side effects until the completion of the treatment, and contact examination among family members are implemented in PPM programs. Treatment success rates among smear-positive TB patients increased from 68.0% in 2011 to 88.3% in 2016. The rates were 68.0% in 2011, 79.8% in 2012, 85.1% in 2013, 84.4% in 2014, 83.8% in 2015, and 83.3% in 2016 (Table 1) [11]. This increase in treatment success rate is a result of the PPM program. The reason for the low treatment success rate in 2011 is presumably that treatment compliance was not high since the PPM program was at an early stage of program introduction. The treatment success rate among MDR-TB cases increased from 54.1% in 2014 to 60.0% in 2015 and 64.3 in 2016 (Table 1) [12].
Table 1.
Treatment success rate among smear positive patients (%) (2011–2016).
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|
| Treatment success rate among smear positive patients | 68.0 | 79.8 | 85.1 | 84.4 | 83.8 | 83.3 |
| Treatment success rate among MDR-TB patients | NA | NA | NA | 54.1 | 60.0 | 64.3 |
NA: Not available.
2.2. Abolish financial barriers, prevent out-of-pocket expenditures, especially for MDR-TB
The government has supported patient TB treatment at a cost of around 7.6 million USD per year to abolish financial barriers, prevent out-of-pocket expenditures from 2011. Insurance has covered all medical expenses since July of 2016. To support MDR-TB patients, the government has supported medical expenses and living costs of family members when MDR-TB patients and non-compliant patients have been hospitalized. Annually, 500–600 patients are hospitalized to increase treatment success rates, which cost around 1.5 million USD in 2011.
2.3. Contact investigation
Management of LTBI can prevent TB through the prevention of progression from LTBI to active TB. Contacts of TB patients are at increased risk of developing TB. The WHO recommended that systematic testing and treatment of LTBI should be performed for contacts of TB patients [13]. Diagnosis and treatment of contacts of TB cases has highest priority in the national TB control program since 2013.
Public health officials in 254 municipalities and nurses at 128 PPM hospitals provide counselling and TB and LTBI examination for contacts among family members. The TB and LTBI examination rates for contacts among family members of infectious pulmonary TB patients were 74.5% in 2013, 84.8% in 2014, 95.5% in 2015, and 99.1% in 2016 [12]. The government supports costs of TB and LTBI examination and treatment cost for family members.
The KCDC has organized a TB epidemic investigation team (Korea Tuberculosis Epidemic Investigation Service, KTEIS) since 2013. This TB epidemic investigation team consists of public officials and field investigators who are trained nurses. Twenty-five field investigators across the country support and guide local public health centers conducting contact investigations among congregate settings include schools, healthcare facilities, military or police units, social welfare facilities, correctional facilities, workplaces, and others [14].
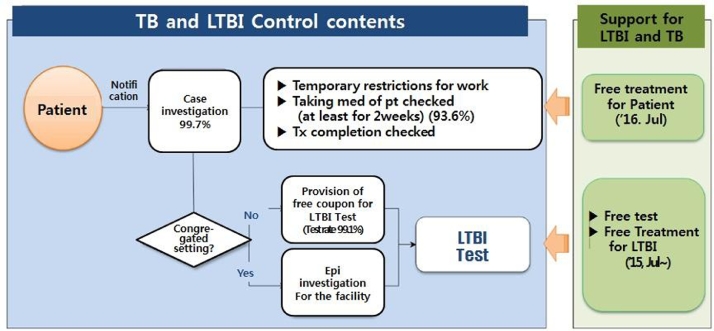
In Korea, TB patients are reported to the Korean National Tuberculosis Surveillance System (KNTSS). When a TB patient is reported to the system, a public health center should check whether the patient belongs to congregate settings. Congregate settings include daycare centers; kindergartens; elementary, middle, and high schools; universities; clinics and hospitals; social welfare facilities; correctional facilities; military or police units; and workplaces. If a patient belonging to congregate settings is considered infectious (sputum acid fast bacilli smear, TB-PCR, or culture positive), contact investigation should be initiated rapidly (Fig. 3). Close contacts are defined as persons who have shared an enclosed environment with an infectious TB patient during the infectious period. Contacts are first evaluated by chest radiography. After the TB screening, close contacts are tested for LTBI by the tuberculin skin test or interferon-gamma release assays (IGRAs). LTBI treatment is recommended to contacts diagnosed with LTBI.
Fig. 3.
Flow chart for TB patient management and contact investigation.
In 2013, a total of 1142 contact investigations in congregate settings were carried out. About 65% of contact investigations were performed in schools in 2013. The number of investigations were 1142 in 2013, 1405 in 2014, 2639 in 2015 and 3502 in 2016 and has increased steadily over the years.
In 2016, a total of 3502 contact investigations in congregate settings were conducted. A total of 146,911 contacts were identified, and 202 secondary TB cases were found. Of 146,911 contacts, 68,686 were tested for LTBI. A total of 12,707 persons (18.5%) were identified as having LTBI. Social welfare facilities including correctional facilities and workplaces showed relatively high LTBI rates of 37.8% and 34.2%, respectively. The number and proportion of investigations in schools decreased from 750 (65.7%) in 2013 to 659 (18.8%) in 2016 (Table 2). Contact investigations in healthcare facilities and workplaces have increased rapidly. The compliance rate for LTBI was analyzed from 2013 to 2014 data; among 14,267 LTBI patients under 35 years old, 10,822 (75.9%) initiated LTBI treatment. Among them, 8985 (83%) completed treatment. The LTBI treatment options were 9 months of isoniazid, a 3-month regimen of isoniazid plus rifampicin, or 4 months rifampicin alone (Table 3).
Table 2.
Results of contact investigation among congregate settings by year (2013–2016).
| Year | 2013 |
2014 |
2015 |
2016 |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of CI | No. of contacts | Contacts with TB disease | Contacts with LTBI (%) | No. of CI | No. of contacts | Contacts with TB disease | Contacts with LTBI (%) | No. of CI | No. of contacts | Contacts with TB disease | Contacts with LTBI (%) | No. of CI | No. of contacts | Contacts with TB disease | Contacts with LTBI (%) | |
| Total | 1142 | 145,486 | 262 | 14,049 | 1405 | 139,562 | 219 | 11,838 | 2639 | 130,838 | 272 | 13,252 | 3502 | 146,911 | 202 | 12,707 |
| (10.8) | (10.9) | (14.5) | (18.5) | |||||||||||||
| Schools | 750 | 123,011 | 192 | 9581 | 758 | 107,795 | 69 | 7652 | 708 | 74,761 | 96 | 4694 | 659 | 74,301 | 58 | 3182 |
| (8.6) | (8.6) | (7.8) | (8.8) | |||||||||||||
| Daycare- center/Kindergarten | 48 | 1961 | 0 | 392 | 37 | 1317 | 0 | 237 | 43 | 2167 | 0 | 228 | 46 | 3179 | 0 | 296 (15.1) |
| (21.0) | (20.1) | (13.5) | ||||||||||||||
| Elementary | 33 | 1628 | 1 | 215 | 44 | 4196 | 2 | 361 | 48 | 2325 | 2 | 278 | 64 | 4160 | 0 | 289 |
| (13.6) | (14.3) | (13.6) | (11.1) | |||||||||||||
| Middle | 89 | 12,624 | 4 | 886 | 85 | 10,329 | 8 | 910 | 62 | 9868 | 35 | 805 | 58 | 7617 | 6 | 608 |
| (7.7) | (9.2) | (9.3) | (9.5) | |||||||||||||
| High | 276 | 77,749 | 104 | 5913 | 245 | 58,043 | 29 | 4175 | 213 | 41,634 | 29 | 2448 | 183 | 43,988 | 38 | 1325 |
| (8.0) | (7.8) | (6.6) | (7.3) | |||||||||||||
| College | 293 | 28,246 | 81 | 2093 | 337 | 33,165 | 30 | 1824 | 329 | 18,390 | 30 | 902 | 295 | 14,799 | 14 | 619 |
| (9.8) | (8.5) | (8.5) | (9.1) | |||||||||||||
| Others | 11 | 803 | 2 | 82 | 10 | 745 | 0 | 145 | 13 | 377 | 0 | 33 | 13 | 558 | 0 | 45 |
| (10.7) | (20.7) | (12.6) | (15.3) | |||||||||||||
| Healthcare facilities | 81 | 3621 | 8 | 938 | 202 | 8827 | 73 | 1370 | 549 | 21,014 | 103 | 3070 | 856 | 29,219 | 83 | 3203 |
| (39.8) | (33.8) | (34.8) | (32.8) | |||||||||||||
| Military/Police unit | 108 | 9029 | 28 | 1045 | 135 | 10,307 | 32 | 1000 | 112 | 6176 | 6 | 565 | 128 | 5379 | 8 | 426 |
| (12.7) | (11.6) | (11.4) | (12.5) | |||||||||||||
| Social welfare/Correctional facilities | 147 | 7971 | 23 | 2072 | 189 | 8906 | 32 | 1225 | 357 | 11,618 | 31 | 1623 | 574 | 15,820 | 30 | 2013 |
| (34.8) | (34.1) | (35.1) | (37.8) | |||||||||||||
| Workplaces | 31 | 1326 | 11 | 329 | 91 | 2889 | 13 | 497 | 845 | 14,942 | 31 | 3034 | 1167 | 19,429 | 22 | 3598 |
| (27.8) | (26.4) | (28.0) | (30.8) | |||||||||||||
| Others | 25 | 528 | 0 | 84 | 30 | 838 | 0 | 94 | 68 | 2327 | 5 | 266 | 118 | 2763 | 1 | 285 |
| (17.2) | (12.1) | (14.2) | (13.0) | |||||||||||||
Table 3.
LTBI treatment completion rate by treatment regimen (2013–2014).
| Regimens | Number of treatment initiations among LTBI cases | Number of completed LTBI treatments | Treatment completion rate (%) |
|---|---|---|---|
| Total | 10,822 | 8985 | 83.0 |
| Isoniazid and rifampicin 3 months | 3157 | 2791 | 88.4 |
| Rifampicin 4 months | 930 | 820 | 88.2 |
| Isoniazid 9 months | 6735 | 5374 | 79.8 |
3. Strengthened LTBI management program
3.1. Progress of the LTBI management program in summary
Korea's LTBI examination has been conducted since 2004 for HIV-infected persons and contacts of family members under 6 years of age. From 2008, the age of contact examination was extended to under 18 years. A TB epidemic investigation team (KTEIS) was established at the KCDC in 2013 and performed contact investigation among congregate settings proactively at the national level.
It has been revealed through contact investigations since 2013 that the spread of TB in medical institutions, daycare centers, kindergartens, schools, and military units is serious. As the problem became more prominent, efforts to resolve the TB problem more actively were made by the Parliament and the government. In 2017, Korea initiated the “TB-free Korea” program, which includes an LTBI screening program for workers in medical institutions, postnatal care business entities, kindergartens, childcare centers, schools, and welfare facilities and people in correctional facilities, military conscripts, and first-year high school students.
The development process of TB policy in Korea has progressed from 2011 through strengthened management of TB patients, from 2013 through strengthened LTBI management through contact investigations in congregate settings, and from 2017 through implementation of LTBI screening program in congregate settings to solve problems discovered through contact investigations.
3.2. “TB-free Korea” program
In 2016, The Ministry of Health and Welfare announced a “TB-free Korea program” to reinforce the Five-Year (2013–2017) Plan based on the experiences of contact investigations from 2013.
From the contact investigations in congregating settings, additional TB and LTBI cases were identified in daycare centers; kindergartens; elementary, middle, and high schools; universities; clinics and hospitals; social welfare facilities; correctional facilities; and military or police units. TB outbreaks among workers in medical institutions and postpartum care centers became an important social issue. It aroused public awareness and government commitment for the reinforcement of the Five-Year Plan.
The incidence rate by age showed an increase from the age of 15, a small peak at 25–29 years, then a decline, and then an increase after age 50. The incidence of TB increased rapidly at the age of 15, which is the first grade of high school. Newly diagnosed TB patients in 2016 increased considerably around the age of 15 with 4.2 patients per 100,000 people among 10–14-year-olds and 23.5 patients per 100,000 people among 15–19-years-olds. Every year, around 20% of high schools’ experience TB cases and from 2013 to 2015, and half of high schools experienced TB cases. When there are infectious TB cases in high schools, with high contact rates, there is transmission of TB, which results in newly identified TB and LTBI cases. This is presumably due to the effects of pubertal hormones, cumulative exposures, and increased exposure due to increased contact rates among that age group. Contact investigations in congregate settings have defined the spread of infectious TB among young age groups such as schools and military units. Due to the characteristics of the military units, most time is spent in the same space, which is highly contagious and needs to be blocked in advance.
3.2.1. Legislative progress and requirements for LTBI screening
The national congress revised the Tuberculosis Prevention Act to require LTBI examination for employees in high-risk congregate settings effective from August of 2016. According to the amended law, the heads of medical institutions, postnatal care business entities, kindergartens, childcare centers, or schools shall conduct TB and LTBI examinations for the employees.
3.22. LTBI screening program in public settings
On March 24, 2016, the government announced the “TB-free Korea program” at the Prime Ministerial Meeting. The “TB-free Korea program” includes a LTBI screening program for workers in medical institutions, postnatal care business entity, kindergartens, childcare centers, schools, and welfare facilities; for people in correctional facilities; and for military conscripts and first-year high school students.
The existing employees in medical institutions and daycare centers and social workers at welfare facilities who were recruited are being screened under a government-led TB screening program in 2017, and after that, new employees will undergo individual TB and LTBI screening under the responsibility of each director.
In 2017, screenings are being conducted for workers in collective facilities like medical institutions around 120,000, daycare centers around 140,000 who are legally obliged, and social workers at welfare facilities around 118,000. The screening for military conscripts around 340,000, first-year high school students and out-of-school youth are being conducted. Screening for correctional facilities is also being conducted. LTBI tests are being conducted using IGRA.
3.3. LTBI recommendations in clinical settings
The Korean Tuberculosis and Respiratory Society revised the guidelines for TB diagnosis and treatment in 2017 to include recommendations for screening and treatment for LTBI. The recommendations for screening and treatment of LTBI were as follows. For those who have contact history with TB patients, diagnosis and treatment of LTBI is recommended [15].
For who do not have contact history with TB patients, the guideline recommends screening and treatment of LTBI in the following situations grouped for high and medium risk for developing TB (Box 1).
Box 1. LTBI screening recommendations in clinical settings.
High-risk group for developing TB
-
-
people living with HIV, patients preparing for organ or hematologic transplantation
-
-
patients initiating anti-tumor necrosis factor treatment,
-
-
people with spontaneously healed lesions on chest X-ray
-
-
recent convertors within 2 years by either IGRA or Mantoux tuberculin skin test
Medium-risk groups
-
-
Patients with silicosis
-
-
People who are using corticosteroid (15 mg per day, more than one month)
-
-
patients receiving dialysis, people with diabetes, patient with head and neck cancer
-
-
patients with jejunoileal bypass
*Source: Joint Committee for the Revision of Korean Guidelines for Tuberculosis and Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis, third edition. 2017.
In clinical settings, LTBI has not been diagnosed and treated in patients other than HIV-infected patients and patients initiating anti-tumor necrosis factor treatment. In the future, recommending diagnosis and treatment of latent TB should be actively carried out for the high- and medium-risk groups in the guideline.
4. Impacts from strengthened TB control program
With intensified TB patient management and contact investigations, the number of new TB notification cases decreased since 2013 after showing stagnation during 2000–2012. Based on the notification data from the Korean National Tuberculosis Surveillance System, the new TB notification rates from 2001 to 2016 decreased since 2013. Incidence rates of new TB reports per 100,000 population were 78.9 in 2011, 78.5 in 2012, 71.4 in 2013, 68.7 in 2014, 63.2 in 2015, and 60.4 in 2016. Rates decreased 5. 2% from 2011 to 2016 annually [8]. The decrease tendency was prominent in smear-positive pulmonary TB cases; it decreased 5.9% from 2011 to 2016 (Table 4). The percentage of reduction in the new TB notification rate from 2011 to 2016 was 23.4%.
Table 4.
New TB notification cases and rates by type of TB, 2011–2016.
| Year | 2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
% of reduction of new TB notification rate, 2011–2016 | % of annual decrease rate of new TB notification rate, 2011–2016 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Ratea | Case | Rate | Case | Rate | Caser | Rate | Case | Rate | Case | Rate | ||||
| New TB notification | 39,557 | 78.9 | 39,545 | 78.5 | 36,089 | 71.4 | 34,869 | 68.7 | 32,181 | 63.2 | 30,892 | 60.4 | −23.4 | −5.2 | |
| Pulmonary TB | Sub-Total | 30,100 | 60.1 | 31,075 | 61.7 | 28,720 | 56.8 | 27,906 | 55.0 | 25,550 | 50.1 | 24,696 | 48.3 | −19.6 | −4.3 |
| Smear-positive pulmonary TB | 11,714 | 23.4 | 12,137 | 24.1 | 11,100 | 22.0 | 10,446 | 20.6 | 9309 | 18.3 | 8812 | 17.2 | −26.2 | −5.9 | |
| Extrapulmonary TB | 9457 | 18.9 | 8470 | 16.8 | 7369 | 14.6 | 6963 | 13.7 | 6631 | 13.0 | 6196 | 12.1 | −35.8 | −8.5 | |
Rate are per 100,000 population.
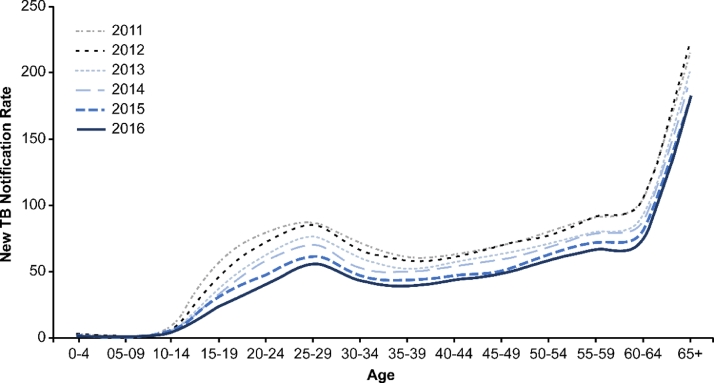
The decrease tendency by age was prominent among the 15–24 age group. The decrease was most significant among 15–19-year-olds (Fig. 4, Table 5). There were 2030 (57.3 people per 100,000) newly reported TB cases among that age group in 2011, and it decreased to 750 (23.5 people per 100,000) in 2016 with almost one-third the level. This has contributed to intensified patient management through the PPM, and the investigation of the contact persons of the collective facilities also played an important role of preventing the development of TB at the individual level and its spread at the community level. This is indirectly demonstrated by the large percentage of decreasing tendency of younger patients who underwent active contact investigations compared to other age groups.
Fig. 4.
New TB notification rates by age group from 2011 to 2016.
Table 5.
New TB notification cases and rates by age, 2011–2016.
| Year | 2011 |
2012a |
2013b |
2014 |
2015 |
2016 |
% of reduction of new TB notification rate, 2011–2016 | % of annual decrease rate of new TB notification rate, 2011–2016 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Ratec | Case | Rate | Case | Rate | Case | Rate | Case | Rate | Case | Rate | |||
| Total | 39,557 | 78.9 | 39,545 | 78.5 | 36,089 | 71.4 | 34,869 | 68.7 | 32,181 | 63.2 | 30,892 | 60.4 | −23.4 | −5.2 |
| 0–4 | 59 | 2.6 | 59 | 2.5 | 40 | 1.7 | 40 | 1.7 | 23 | 1.0 | 17 | 0.8 | −69.2 | −21.0 |
| 5–9 | 38 | 1.6 | 42 | 1.8 | 25 | 1.1 | 21 | 0.9 | 16 | 0.7 | 13 | 0.6 | −62.5 | −17.8 |
| 10–14 | 305 | 9.6 | 199 | 6.5 | 155 | 5.4 | 115 | 4.2 | 128 | 5.0 | 102 | 4.2 | −56.3 | −15.2 |
| 15–19 | 2030 | 57.3 | 1630 | 46.5 | 1281 | 37.2 | 1131 | 33.6 | 1014 | 30.9 | 750 | 23.5 | −59.0 | −16.3 |
| 20–24 | 2496 | 79.0 | 2365 | 72.7 | 2099 | 62.7 | 1988 | 57.9 | 1671 | 47.6 | 1419 | 40.1 | −49.2 | −12.7 |
| 25–29 | 3127 | 86.9 | 2895 | 85.4 | 2465 | 76.4 | 2218 | 70.4 | 1928 | 61.6 | 1760 | 55.7 | −35.9 | −8.5 |
| 30–34 | 2852 | 72.2 | 2659 | 66.3 | 2442 | 60.4 | 2092 | 52.7 | 1794 | 47.3 | 1548 | 43.0 | −40.4 | −9.8 |
| 35–39 | 2620 | 61.3 | 2422 | 58.7 | 2070 | 52.1 | 1935 | 49.9 | 1689 | 43.5 | 1533 | 38.9 | −36.5 | −8.7 |
| 40–44 | 2812 | 62.6 | 2785 | 61.0 | 2608 | 57.2 | 2450 | 54.3 | 2078 | 47.1 | 1863 | 43.8 | −30.0 | −6.9 |
| 45–49 | 2915 | 69.1 | 2907 | 70.1 | 2650 | 63.2 | 2546 | 59.2 | 2211 | 50.6 | 2165 | 48.5 | −29.8 | −6.8 |
| 50–54 | 3,320 | 80.2 | 3,324 | 77.5 | 3,107 | 71.6 | 2,978 | 68.9 | 2,699 | 63.3 | 2,448 | 58.7 | −26.8 | −6.1 |
| 55–59 | 2761 | 91.0 | 2976 | 91.6 | 2758 | 79.9 | 2916 | 79.3 | 2785 | 71.7 | 2719 | 66.7 | −26.7 | −6.0 |
| 60–64 | 2363 | 104.3 | 2452 | 104.8 | 2227 | 91.9 | 2228 | 88.4 | 2207 | 81.3 | 2227 | 75.1 | −28.0 | −6.4 |
| 65+ | 11,859 | 214.6 | 12,798 | 222.2 | 12,157 | 201.6 | 12,211 | 193.9 | 11,938 | 182.2 | 12,328 | 181.8 | −15.3 | −3.3 |
32 cases with age unknown.
5 cases with age unknown.
Rate are per 100,000 population.
5. Challenges for implementation of LTBI program
The TB situation in Korea is very unique. Due to the high incidence of TB and high levels of economic status with sufficient resources, there are insufficient guidelines to develop a latent TB policy suitable for this situation. The WHO LTBI guideline is generally referred to as having low rates of TB and high levels of economic status, primarily in Western countries [16].
The most challenging part is a low perception of LTBI. It is difficult to communicate information on LTBI not only to the public but also to healthcare professionals [17]. Successful implementation of an LTBI policy is urgently required to introduce treatment with fewer side effects in a shorter period of treatment duration. It is a difficult problem to improve adherence to treatment and to manage side effects.
6. Lessons learned
The lessons learned from Korea's TB control policy are as follows.
-
1.
The government's policy will to fight TB is very important. The policy requires support from financial and human resources, which is difficult to secure without the government's political commitment.
-
2.
It is necessary to set clear goals and establish concrete national TB plans to implement. The Korean government has set a clear goal to reduce the incidence of TB from 100 people per 100,000 population in 2011 to 50 per 100,000 people by 2020. In line with this goal, in 2013, the first comprehensive TB control plan was established. This is a five-year plan for the period from 2013 to 2017.
-
3.
In the LTBI policy, contact investigation has the highest priority and gate way to LTBI program [18]. This is because the survey of contact persons in congregate settings can reveal the level of TB in collective facilities as well as the aspect of TB transmission. Through the contact investigations, additional patients other than infectious index patients and LTBI can be detected and treated, thereby contributing to the prevention of transmission of TB.
-
4.
Successful management of LTBI should overcome the economic obstacles by supporting the cost of screening and treatment of LTBI cases [18].
-
5.
A legislative process is needed to effectively settle LTBI policies. Discussions with member of Congress, and the public during the legislative process are crucial for persuading the need for policy and for securing relevant policies and necessary budget for policy implementation
-
6.
To combat TB, it is essential to manage LTBI successfully. To carry out the LTBI policy, research and development should be conducted to develop more accurate diagnosis, treatment regimens with shorter duration and fewer side effects, and policy methods [19].
-
7.
It is very important to communicate effectively with the public and health care professionals continuously. As it is very difficult to communicate information on the concept of LTBI. To overcome this obstacle, in 2017, a nationwide education program for health care workers is being implemented. A treatment network with around 300 hospitals has been organized for the treatment of latent TB cases identified through the LTBI screening program.
7. Conclusion
The successful implementation of Korea's TB control policy is based on the government's political will, increased mobilization of resources including human resources based on clear goals, and well-planned national strategy and policy.
Strengthening the reporting system and patient management program is a very fundamental part. In addition, enhanced contact investigation to detect and treat LTBI have played an important role in accelerating the reduction of TB incidence because it is very effective in preventing the incidence of infectious TB by prevent further community transmission through the preventive treatment to LTBI cases.
Through an active contact investigation from 2013, we found that TB is a serious problem in congregate settings such as schools, daycare centers, and medical institutions. To solve these problems proactively, mandatory TB and LTBI screening for workers in facilities such as medical institutions, postnatal care business entity, kindergartens, childcare centers, and schools has been adopted since 2016, and the TB Free Korea campaign, a screening program for LTBI in high-risk groups, has been implemented since 2017.
To manage LTBI effectively, it is urgently necessary to develop a more accurate diagnosis method and a more effective treatment method. Currently, in situations in which effective treatment is limited, it is necessary to build up the treatment infrastructure to minimize adverse effects of treatment while increasing compliance. It is necessary to actively cooperate with medical staff for latent TB treatment management. In addition, patients should be carefully selected based on the national epidemiological characteristics.
Korea is in the process of establishing a second TB comprehensive management plan for five years from 2018 to 2022. The plan will include establishment of a more systematic approach to vulnerable groups such as elderly people and foreigners in addition to existing patient management, contact investigation, and screening for high-risk groups for TB and LTBI.
In conclusion, to establish and implement a successful TB policy, it is very important and fundamental to set clear goals and define effective strategies with increased political commitment and investment.
The points that other countries can refer to through the evolution process of Korea's TB control policies are as follows.
-
1.
When the health system for TB patient care is changed including the introduction of a national health insurance program, the government should monitor whether the surveillance and TB patient management system captured all the patients including those in the private sector. The PPM collaboration is a very effective management system to increase the treatment success rate of TB patients including those in the private sector. The government should also monitor the financial burden due to TB treatment and care after the change of care system and find ways to abolish financial barriers and prevent out-of-pocket expenditures, especially for MDR-TB.
-
2.
Contact investigation is important to determine the seriousness of TB at the community level including schools, medical institutions, and workplaces. The public should be informed of the problems revealed through contact investigation in a transparent manner, and focus should be on solving problems identified through contact investigation. Then, system improvement measures can be derived according to epidemiological characteristics.
-
3.
Above all, the government's commitment and leadership in TB management are the most important. The government's coordinated policies and actions are needed to maintain partnerships with civil society as well as public and private sectors.
Funding
This study funded by Korea Centers for Disease Control and Prevention.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgments
The authors would like to thank, Kyung-Sook Cho, Kyugwon Hwang, Minkyu Kang, Junwook Kwon, Ki-Suck Jung, Seongchul Lee, Younjae Lee, Ah Young Park, Su Jin Park for technical support and Sung Ryul Jang, GiYeol Heo, Eunyoung Cho for administrative support. Special thanks to Dr Haileyesus Getahun from WHO for comments and Dr Mario Raviglione, Dr Philippe Glaziou, Dr Nobu Nishkiori from WHO, Dr Chiang Chen-Yuan from International Union Against Tuberculosis and Lung Disease (IUATLD), Dr Ken Castro from US CDC, Dr Toru Mori from Japan Anti-Tuberculosis Association (JATA) for wonderful and thoughtful consultancy in the international review meeting, 2011.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jctube.2018.04.006.
Appendix. Supplementary materials
References
- 1.World Health Organization Tuberculosis, fact sheet. 2018. http://www.who.int/mediacentre/factsheets/fs104/en/ Reviewed January 2018.
- 2.World Health Organization. The END TB strategy. 2015.
- 3.Lee YK, Kwon YH, Lee SH, Son HJ, Go UY. Overview of tuberculosis control and prevention policies in Korea. Public health weekly report. KCDC. 2015;8(28):651–656. [Google Scholar]
- 4.Kim HJ. Current status of tuberculosis in Korea. Korean J Med. 2012;82(3):258–262. [Google Scholar]
- 5.World Health Organization. Global tuberculosis report 2012.
- 6.World Health Organization. Global tuberculosis report 2017.
- 7.Kang H-Y, Yoo H, Park W, Go U, Jeong E, Jung K. Tuberculosis notification completeness and timeliness in the Republic of Korea during 2012–2014. Osong Public Health Res Perspect. 2016;7(5):320–326. doi: 10.1016/j.phrp.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis in Korea 2016. http://tbzero.cdc.go.kr/tbzero/board/boardView.do, 2017.
- 9.KCDC. International review meeting on new 2020 plan for TB elimination (Internal document). 2011.
- 10.Ministry of Health and Welfare, KCDC. Five-year (2013–2017) plan for TB elimination for the Republic of Korea. 2013.
- 11.KCDC, Review of TB control program based on the international review meeting in 2011 and way forward of Korea TB control program (Internal document). 2016.
- 12.KCDC, TB programme monitoring report (Internal document). 2016.
- 13.Getahun H, Matteelli A, Abubakar I, Aziz MA, Baddeley A, Barreira D. Management of latent Mycobacterium tuberculosis infection: WHO guidelines for low tuberculosis burden countries. Eur Respir J. 2015;44:1563–1576. doi: 10.1183/13993003.01245-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kwon Y, Kim S, Kim J, Song E, Lee E, Choi Y. Results of tuberculosis contact investigation in congregate settings in Korea, 2013. Osong Public Health Res Perspect. 2014;5(S):S30–S36. doi: 10.1016/j.phrp.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joint Committee for the Revision of Korean . 3rd ed. 2017. Guidelines for tuberculosis and Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis.http://tbzero.cdc.go.kr/tbzero/contents.do [Google Scholar]
- 16.World Health Organization. Guidelines on the management of latent tuberculosis infection. 2015. [PubMed]
- 17.Vries G, Hest R, Bakker M, Erkens C, Hof S, Meijer W. Policy and practice of programmatic management of latent tuberculosis infection in the Netherlands. J Clin Tuberculosis Other Mycobact Dis. 2017;7:40–48. doi: 10.1016/j.jctube.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO, Report of the global consultation on the programmatic management of latent tuberculosis infection. 27–28 April 2016, Seoul, Republic of Korea.
- 19.Matteelli A, Sulis G, Capone S, D'Ambrosio L, Migliori GB, Getahun H. Tuberculosis elimination and the challenge of latent tuberculosis. Prese Med. 2017;46:e13–e21. doi: 10.1016/j.lpm.2017.01.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.