ABSTRACT
Study Design: A prospective, single-arm, pre-postintervention study.
Objective: To determine the preliminary usefulness of providing pain neuroscience education (PNE) on improving pain and movement in patients presenting with non-chronic mechanical low back pain (LBP).
Background: PNE has been shown to be an effective intervention for the treatment of chronic LBP but its usefulness in patients with non-chronic LBP has not been examined.
Methods: A single group cohort pilot study was conducted. Eighty consecutive patients with LBP < 3 months completed a demographics questionnaire, leg and LBP rating (Numeric Pain Rating Scale – NPRS), disability (Oswestry Disability Index), fear-avoidance (Fear-Avoidance Beliefs Questionnaire), pain catastrophizing (Pain Catastrophizing Scale), central sensitization (Central Sensitization Inventory), pain knowledge (Revised Neurophysiology of Pain Questionnaire), risk assessment (Keele STarT Back Screening Tool), active trunk flexion and straight leg raise (SLR). Patients received a 15-minute verbal, one-on-one PNE session, followed by repeat measurement of LBP and leg pain (NPRS), trunk flexion and SLR.
Results: Immediately after intervention, LBP and leg pain improved significantly (p < 0.001), but the mean change did not exceed minimal clinically important difference (MCID) of 2.0. Active trunk flexion significantly improved (p < 0.001), with the mean improvement (4.7 cm) exceeding minimal detectible change (MDC). SLR improved significantly (p = 0.002), but mean change did not exceed MDC.
Conclusions: PNE may be an interesting option in the treatment of patients with non-chronic mechanical LBP. The present pilot study provides the rationale for studying larger groups of patients in controlled studies over longer periods of time.
KEYWORDS: Low back pain, sub-grouping, pain neuroscience education, clinical prediction rules
Introduction
The prevalence of chronic low back pain (LBP) has been reported to be as high as 9.17%, and despite evidence of treatment efficacy, the clinical significance of most interventions remains uncertain [1–5]. Chronic LBP is a heterogeneous condition characterized by persistent and recurrent symptoms that result in various biopsychosocial problems that often require long term management [6]. The transition from acute to chronic or persistent pain is thought to occur through maladaptive neuroplastic mechanisms involving three interrelated processes – peripheral sensitization, central sensitization and descending modulation [7]. An important approach to the prevention of chronic LBP is recognizing appropriate risk factors, and modern clinical guidelines call for the screening of patients with acute LBP into categories of low, medium and high risk for the development of chronic pain and disability [8,9]. It is proposed that patients who score higher on a variety of psychometric tests such as fear-avoidance and pain catastrophizing constitute the high risk group [10–13].
A Physical Therapy (PT) treatment that has emerged in the last 20 years, specifically aiming at patients with these higher risk factors, is pain neuroscience education (PNE) [14,15]. PNE is an educational strategy that focuses on teaching people more about the neurobiological and neurophysiological processes involved in their pain experience [14,16,17]. Current best-evidence regarding musculoskeletal pain provides strong support for PNE to positively influence pain ratings, dysfunction, fear-avoidance, and pain catastrophizing, limitations in movement, pain knowledge and healthcare utilization [17,18]. PNE has shown to positively impact both fear-avoidance and pain catastrophizing, and there is growing evidence that supports the idea that patients with higher fear-avoidance and pain catastrophizing not only do well with PNE, but may in fact be ideal patients for PNE [19,20]. To date, however, PNE has primarily been adopted for patients with chronic pain, especially chronic LBP [17]. This has led to a possible clinical belief that PNE should only be considered for patients with chronic pain [21]. A recent survey was conducted to determine the utilization of PNE by clinicians as well as practice patterns associated with PNE [19]. One specific objective of the study was to determine which patients were thought to respond favorably with PNE. The study did confirm the current belief that PNE is being primarily used for chronic pain, but surprisingly, acute pain was rated second, ahead of high fear-avoidance and pain catastrophizing [19]. The findings of the survey study indicated the need for further investigation into the use of PNE for acute pain states.
Given the evidence that PNE has a positive effect on fear-avoidance and pain catastrophizing, and that both these factors are considered risk factors for the development of chronic LBP, it may be argued that some patients with recent onset LBP may potentially benefit from PNE [22,23]. The present study aimed to explore the feasibility and preliminary efficacy of a clinically applicable PNE intervention delivered to patients with recent onset LBP. Specifically, our purpose was to determine if there would be any immediate change in pain, movement, and/or perceived improvement demonstrated in patients with non-chronic LBP after 15 minutes of PNE. It is proposed that if such a short duration of PNE can result in immediate changes in pain, movement, and/or perceived improvement in such patients, it may provide a window of opportunity for functional improvement and reduce the risks of progression to chronic LBP. While it is beyond the scope of this pilot study, such a proposal would need to be tested with larger data sets and a randomized controlled trial showing improvement in these areas at the sub-acute stage result in a lower rate of progression to chronicity. This may in turn warrant the reconsideration of when PNE interventions might be appropriate or even the development of a clinical prediction rule (CPR) study of PNE for recent onset LBP.
Materials and methods
We conducted a prospective, single-arm, pre-postintervention study with a 15-minute PNE session as the intervention.
Patients
A convenience sample of consecutive patients with non-chronic mechanical LBP presenting to outpatient physical therapy clinics. Mechanical LBP has been defined as arising intrinsically from the spine, intervertebral discs, or surrounding soft tissues [24]. We defined it operationally as symptoms changing (better/worse) with movement, activity or positions. Chronic pain has been defined as pain persisting beyond the normal time of healing and in non-malignant pain, 3 months is considered the most convenient point of division between acute and chronic pain [25].
Inclusion criteria
Patients were aged 18 to 85 years with a history of LBP with or without leg pain less than 3 months, and a willingness to participate.
Exclusion criteria
Patients were excluded if they: a) were under age 18 (minor); b) complained of LBP with or without leg pain for more than 3 months; c) had undergone lumbar surgery; d) could not read or understand the English language; e) presented with any cognitive deficits from a previous diagnosis (i.e. stroke, traumatic brain injury, etc.) rendering them unsuitable for the educational intervention (PNE), f) declined to participate or g) presented with a medical etiology (red flag) associated with their LBP.
Patient recruitment
Patients were recruited by 7 orthopedic physical therapy residents at St. Ambrose University, working in private practice and hospital outpatient departments.
Therapist training
To standardize delivery of the intervention, all residents attended a 2-day PNE class, which has been shown to increase healthcare provider knowledge of pain and shift their attitudes and beliefs regarding pain [26]. Additionally, all residents had to score ≥ 90% on the rNPQ, in line with previous studies training clinicians for delivery of PNE [27]. Once training was completed, they screened patients, gathered the data and provided the intervention for this study. Institutional Review Board (IRB) approval was obtained at St. Ambrose University. The study was registered as a clinical trial (NCT03722394).
Measurements
Patients eligible for and willing to participate in the study were provided with and asked to sign a written informed consent. Patient demographic data were collected, with no identifiable information being gathered other than the consent. Demographic data gathered included age, gender, duration and location of pain, income level, education level, work status and past history of LBP. Prior to the subjective and physical examination, a set of standardized patient-reported outcome measures were administered in order to provide clarity on any potential subgrouping of patients at higher risk for moving to chronic LBP, as well as measure for any changes post-intervention (Figure 1). The following outcomes tools were administered prior to the subjective examination:
Pain (low back and leg) (numeric pain rating scale – NPRS): LBP and leg pain were measured with the use of a NPRS, as has been used in various studies on LBP and PNE [14,15,28,29]. The minimal clinically important difference (MCID) for the NPRS for non-chronic LBP is reported to be 2.0 [30].
Fear avoidance beliefs (fear avoidance beliefs questionnaire – FABQ): The FABQ is a 16-item questionnaire that was designed to quantify fear and avoidance beliefs in individuals with LBP. The FABQ has two subscales: 1) a 4-item scale to measure fear avoidance beliefs about physical activity (FABP-PA); and 2) a 7-item scale to measure fear-avoidance beliefs about work (FABQ-W). Each item is scored from 0 to 6 with possible scores ranging between 0 and 24 and 0 and 42 for the physical activity and work subscales, respectively, with higher scores representing an increase in fear-avoidance beliefs. The FABQ has demonstrated acceptable levels of reliability and validity in previous LBP studies [31–33]. Presence of avoidance behavior is associated with increased risk of prolonged disability and work loss. It is proposed that FABQ-PA >14 and FABQ-W scores >34 and are associated with a higher likelihood of not returning to work [34,35]. The MCID for the FABQ has been reported as 13.0 [36].
Disability (oswestry disability index – ODI): The ODI is a 10-item questionnaire used to assess different aspects of physical function. Each item is scored from 0 to 5, with higher values representing greater disability. The total score is multiplied by 2 and expressed as a percentage. The ODI has been shown to be a valid and reliable measure of disability related to LBP [37–39]. A change of 5 points (10%) has been proposed as the MCID [40].
Pain catastrophizing (pain catastrophizing scale – PCS): The PCS is a self-report questionnaire that assesses inappropriate coping strategies and catastrophic thinking about pain and injury. The PCS has been used in previous PNE studies for LBP [41,42] and demonstrated strong construct validity, reliability and stability [43]. The PCS utilizes a 13-item, 5-point Likert scale with higher scores indicating elevated levels of catastrophizing. Previous studies utilizing the PCS have shown a median score of 18 in healthy individuals, whereas in patients with pain the PCS is generally higher, with a score over 30 reported as a high level of pain catastrophizing [43]. The minimal detectable change (MDC95) for the PCS is reported to be 9.1 [44].
Central sensitization (central sensitization inventory – CSI): The CSI consist of 25 questions which identifies key symptoms associated with central sensitization syndrome and quantifies the degree of these symptoms [45]. Answers range from never (0 points) and always (4 points) and a score of > 40 points has been reported as indicative of the clinical presence of central sensitization [12,45]. While there is no reported MDC for the CSI, there are 2 studies [46,47] that have found it to be an ‘excellent’ responsive treatment outcome measure [48].
Pain knowledge (revised pain neurophysiology questionnaire – rnpq): The NPQ is based on a current pain science text [49] and was used in a previous study measuring the neurophysiology knowledge of patients and healthcare personnel [50]. The original NPQ is a 19-item questionnaire requesting ‘true’; ‘false’; or ‘not sure’ answers to statements, with higher scores indicating more correct answers. Since the development of the NPQ a statistical analysis of the NPQ has led to the development of an abbreviated revised NPQ (rNPQ) with 12 questions which removed ambiguous questions [51]. The revised 12-question rNPQ was used in this study. No information is available on what constitutes a meaningful shift in NPQ/rNPQ scores, but studies using the NPQ and rNPQ have shown positive changes for patients, healthcare providers and students after PNE with mean increases in NPQ/rNPQ scores of 27% [52].
Risk assessment (keele start back screening tool – keele SBST): The Keele SBST is a 9-item questionnaire that contains questions that are established predictors for disabling LBP. Each item is responded to as ‘“agree”’ or ‘“disagree”’, except the bothersomeness item which uses a Likert scale of ‘“not at all”’ to ‘“extremely”’. The overall score is used to separate into low and medium risk subgroups. The distress subscale is used to separate medium risk subgroup into medium and high risk. It is used to identify potential ‘“at-risk”’ patients for potential long-term chronic problems [53]. These patients need careful assessment and intervention with suitable cognitive and behavioral strategies [9].
Figure 1.
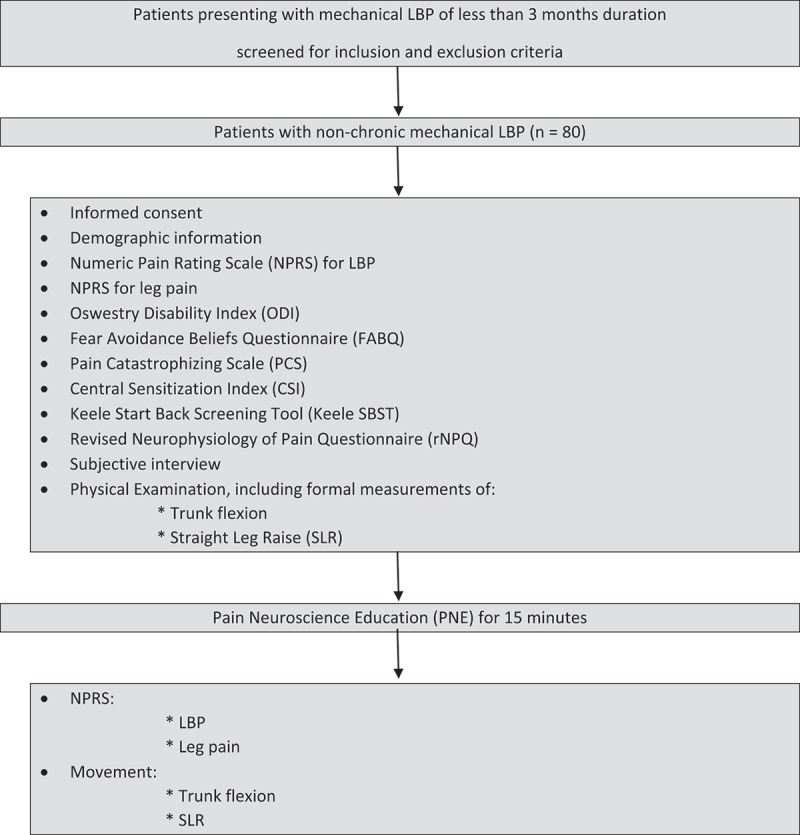
Study flowchart.
Residents were then asked to perform a standardized review of systems, subjective examination, and physical examination consistent with clinical practice guidelines [54]. In order to assess for any potential changes post-intervention, two specific physical tests, common in PNE studies, were assessed before and immediately after the intervention [17,41,42].
Lumbar flexion: Active trunk forward flexion, measured from the longest finger on the dominant hand to the floor [9,41,42]. MDC95 for active trunk forward flexion has been reported as 4.5 cm [55].
Straight leg raise (SLR): SLR was measured with an inclinometer placed on the tibial crest 5 cm distal to the inferior border of the patella on the most affected leg [9,41,42]. SLR for this study kept the ankle in neutral (90 degrees) with no added dorsiflexion or plantar flexion, per previous studies [9,41,42]. MDC for SLR has been reported as a 5.7 degree difference [55].
Upon completion of the intervention, the following were re-measured to determine if there had been any change: LBP (NPRS), leg pain (NPRS), trunk flexion, and SLR. Immediately after intervention, patients were asked if their pain had changed and/or they experienced improvement in movement, and their responses were recorded. Qualitative studies on LBP show these 2 parameters to be important factors in (i) meeting patient needs and (ii) representing successful outcomes [56–58]. MCID was chosen as the primary expression of change, since it represented a positive clinical difference. When MCID was not known for a specific measure, MDC was used as a secondary level of determining a patient’s response to the intervention.
Patients also completed the Global Rating of Change Scale (GROC) to measure perceived outcome following the intervention. The GROC uses a 15-point scale with the following anchors: −7, ‘a very great deal worse’; 0, ‘about the same’; +7, ‘a very great deal better’. It has been reported that scores of +4 and +5 are indicative of moderate changes in patient-perceived status and that scores of +6 and +7 indicate large changes in patient status [59].
Intervention
Following the initial intake forms completion, review of systems, subjective examination and physical examination, the patients received a standardized PNE session [60,61]. The PNE session lasted 15 minutes per patient and was delivered in a one-on-one educational format with a clinician using prepared images, drawings and metaphors [17]. The 15-minute PNE session was utilized to reflect a clinically meaningful intervention in a typical allocated time frame in clinical practice. The content of the PNE is described in detail elsewhere, using a metaphorical alarm system analogy to explain sensitization of the nervous system during a pain experience, which leads to decreased thresholds for movement, emotions and activity, as part of the pain experience [60,61]. The PNE session additionally explained, via the alarm metaphor, how various therapeutic interventions including education and movement (i.e. exercise, manual therapy) can decrease a sensitive alarm system alongside tissue healing phases to result in a recovery from LBP.
Data analysis
This was an exploratory study to investigate the feasibility and possible immediate impact of the intervention on patients with non-chronic LBP. Descriptive statistics such as counts and percentages, frequency distributions, means, standard deviations and confidence intervals were used to describe the demographic variables and patient-reported outcome measures of the patients in the study (Table 1). To compare pre- and post-intervention measures of NPRS for back and leg pain, trunk flexion range, and SLR, paired-samples t-tests were conducted. To assess perceived outcome, we calculated the percentage of patients who reported GROC of +4 or better.
Table 1.
Descriptive data of the cohort of 80 consecutive patients admitted to the study. Continuous data reported as means ± standard deviation (range) and ordinal data reported as frequencies and percentages.
| Variable | Statistic |
|---|---|
| Age (in years) | 45.2 ± 15.5 (19–81) |
| Females | 49 (61.2%) |
| Duration of symptoms in days | 39.5 ± 30.3 (2–90) |
| Ethnicity | White non-Hispanic 58 (72.5%) African-American 8 (10%) Asian 8 (10%) Hispanic 5 (6.3%) Other 1 (1.3%) |
| Education Level | High School 28 (35%) Graduate 27 (33.8%) Post-Graduate 13 (16.3%) Other 12 (14.9%) |
| Annual Income (per annum) | < $10,000 15 (18.8%) $10,000 – $50,000 27 (33.8%) $50,000 – $100,000 23 (28.8%) > $100,000 14 (17.5%) |
| Currently working (yes) | 60 (75%) |
| Had LBP before (yes) | 58 (72.5%) |
| Family history of back surgery (yes) | 30 (37.5%) |
| NPRS (LBP) | 5.28 ± 2.49 (0–10) |
| NPRS (Leg pain) | 3.06 ± 2.59 (0–9) |
FABQ-PA
|
14.1 ± 6.1 (0–24) 45 (56.3%) |
FABQ-W
|
14.8 ± 12.0 (0–39) 7 (8.75%) |
PCS
|
16.9 ± 12.2 (0–44) 18 (22.5%) |
CSI
|
31.4 ± 13.3 (3–67) 21 (26.25%) |
| rNPQ | 4.4 ± 2.5 (0–11) |
| ODI | 17.1 ± 8.9 (0–42) |
Keele SBST
|
5.2 ± 2.3 (0–9) 60 (75%) |
Keele SBST Sub-score
|
2.5 ± 1.5 (0–5) 23 (28.75%) |
| SLR (degrees) | 52.1 ± 23.01 (0–99) |
| Trunk Flexion (centimeters) | 28.58 ± 17.5 (75–3) |
LBP = Low back pain; NPRS = Numeric Pain Rating Scale; FABQ PA = Fear Avoidance Beliefs Questionnaire – Physical Activity Subscale; FABQ-W = Fear Avoidance Beliefs Questionnaire – Work Subscale; PCS = Pain Catastrophizing Scale; CSI = Central Sensitization Inventory; rNPQ = Revised Neurophysiology of Pain Questionnaire; ODI = Oswestry Disability Index; Keele SBST = Keele STarT Back Screening Tool; SLR = Straight Leg Raise
Finally, we dichotomized the patients into those experiencing ‘success’ or ‘non-success’ following the 15-minute PNE session. For ‘success’, patients had to achieve at least 2 of the following 3 criteria: a) meet or exceed the MCID or MDC for change in the NPRS for back or leg pain; b) meet or exceed the MCID or MDC for change in movement measures (Trunk flexion and SLR); and c) meet or exceed the MDC for the GROC (+3).
Results
Patients
A total of 80 consecutive patients were admitted in this pre- and post-intervention single cohort study. The mean age was 45.2 years (SD = 15.5; Range = 19–81). Mean duration of symptoms was 39.5 days (SD = 30.3; Range = 2–90). Further data describing the cohort can be seen in Table 1.
LBP
Paired samples t-tests revealed a statistically significant difference in pain scores (NPRS) for LBP from pre- to post-intervention (Table 2). Mean difference was 0.79 ± 1.5 (p < 0.001). Although statistically different, the mean change scores for the group did not meet the MCID of 2.0.
Table 2.
Paired samples t-tests for LBP, leg pain, trunk flexion and SLR before and after PNE.
| Paired Differences |
||||||||
|---|---|---|---|---|---|---|---|---|
| 95% Confidence Interval of the Difference |
||||||||
| Mean | Std. Deviation | Std. Error Mean | Lower | Upper | t | df | Sig. (2-tailed) |
|
| NPRS change for LBP (in cm) | .788 | 1.498 | .168 | .454 | 1.121 | 4.701 | 79 | .000* |
| NPRS change for leg pain (in cm) | .556 | 1.336 | .149 | .259 | .854 | 3.724 | 79 | .000* |
| Trunk flexion change (pre-post) in degrees | 4.670 | 9.187 | 1.027 | 2.626 | 6.714 | 4.547 | 79 | .000* |
| SLR change (in degrees | −2.525 | 6.956 | .778 | −4.073 | −.977 | −3.247 | 79 | .002* |
* Significant difference (p < 0.005).
Leg pain
Paired samples t-tests revealed a statistically significant difference in pain scores (NPRS) for leg pain from pre- to post-intervention. Mean difference was 0.56 ± 1.3 (p < 0.001) (Table 2). Although statistically different, the mean change scores for the group did not meet the MCID of 2.0.
Trunk flexion
Paired samples t-tests revealed a statistically significant difference in active trunk flexion range from pre- to post-intervention. Mean difference was 4.7 cm ± 9.2 (p < 0.001), which exceeded the MDC95 for active trunk forward flexion of 4.5 cm.
SLR
Paired samples t-tests revealed a statistically significant difference in SLR from pre- to post-intervention. Mean difference was 2.5° ± 7.0° (p = 0.002). Although statistically different, the mean change in SLR did not meet the MDC of 5.7°.
GROC
While most of the patients (57.5%) rated themselves as ‘a tiny bit better’ or better, i.e. > +1 on the GROC, only 4 reported scores of +4 or better indicating moderate change. Only 16 patients (20%) met or exceeded the MDC of 3 points on the GROC.
Discussion
This pilot study found that an immediate reduction in pain and improvement in trunk flexion movement was observed in patients with non-chronic LBP who were provided a 15-minute PNE session. These improvements, while statistically significant, were not clinically meaningful. However, it should be noted that the intervention was of very short duration and only immediate changes were measured. Given the observed findings, it is possible that PNE may be useful in reducing pain and improving movement in patients with mechanical LBP who have not progressed to chronicity (> 3 months duration).
Many of the patients in our sample met or exceeded various cut-off scores associated with a higher likelihood of progressing into chronicity [12,34,35,43,45]. More than half of the patients (56.3%) exceeded the FABQ-PA sub-score of 14, and at least a quarter (26.25%) of the patients met or exceeded the CSI cut-off score of 40, indicating a clinical presentation indicative of central sensitization (Table 1). Specific to risk assessment, 75% of the patients scored more than or equal to 4 points on the Keele SBT total score indicating a greater risk for progressing to chronicity (Table 1). If patients in our study are representative of patients with shorter duration (< 90 days) of symptoms of mechanical LBP, then there may be a need to address patient concerns (fear avoidance, central sensitization, etc.) in those considered to be at greater risk for progressing to chronicity. While it was beyond the scope of this pilot study, future studies may shed light on whether PNE might be an appropriate approach for these ‘at risk’ patients.
While the length of the PNE intervention was purposely kept to within 15 minutes to reflect a typical allocated time frame in clinical practice, it may not have been long enough or of sufficient depth to more positively affect the post-intervention measures. Recent systematic reviews of PNE for musculoskeletal pain have shown greater effectiveness when it is combined with a movement-based strategy such as exercise and/or manual therapy [17,18,62]. Future studies on the effectiveness of PNE for patients with non-chronic LBP should therefore include such a movement-based strategy and follow progress for longer time periods. This exploratory study was focused on observing for any immediate changes in pain and trunk flexion movement that may have been attributed to the intervention. If a short, 15-minute PNE session could lead to immediate improvements in pain and trunk flexion movement in patients with LBP, it might be seen as providing a ‘window of opportunity’ for patients to more readily engage in movement-based strategies for their pain.
Using the previously stated parameters for ‘success’, 22 (27.5%) met the criteria for a ‘successful’ intervention. It is remarkable that more than a quarter of the sample experienced ‘success’ after only 15 minutes of PNE, and this may challenge the viewpoint that PNE ‘is only for chronic pain’ [19,21].
In the current literature pertaining to risk assessment for LBP, patients are often classified as low, medium or high risk for moving into chronicity [9,53]. It is argued that patients with low risk will do well with limited treatment and often respond favorably to physical interventions such as manual therapy and exercise, with little need for a cognitive intervention. At the other end of the spectrum, it is proposed that patients with high risk should receive a more biopsychosocial intervention strategy and multidisciplinary care, which has been supported by the literature [63–65]. The findings of this study may provide ideas for future studies which may provide specific data about what to do with the medium risk group [66]. The PNE session used in this study, lasted only 15-minutes, tended to yield positive results and can be administered in clinical practice despite current practical time constraints. Current cognitive and multidisciplinary interventions for higher risk patients are associated with higher expense, waiting lists, lengthy sessions and referral to other specialists [65,67–69]. The authors agree that a certain subset of high-risk patients presenting in PT with recent onset LBP warrant further investigation and management by other skilled professionals, i.e. psychology/psychiatry, but too often patients are merely labeled as medium or high risk and referred on to advanced (outside) treatments. The findings of this study might provide the impetus for research on what might be best to do with medium and potentially even high-risk patients. We hope future studies can examine whether they can and should be treated by PT via a PNE approach, thus strengthening the current push towards PT First [70].
Limitations
The study has several limitations. The study design did not include a control or comparator group and was not randomized therefore the observed changes pre-postintervention may not be attributed solely to the intervention. The immediate follow up does however limit the effect of confounders such as natural history. The population used to recruit patients was predominantly from care seeking individuals presenting to 5 PT clinics in metropolitan Iowa and may not reflect the population from a primary care setting. Not all patient-reported outcome measures were re-evaluated post-intervention. This was because a change in FABQ, ODI, PCS, CSI, rNPQ and Keele SBST were not expected following a 15-minute education session. Another limitation is that the PNE delivered was only 15 minutes, and it could be argued that a lengthier PNE session may have resulted in a more substantial post-intervention shift.
Conclusion
The inclusion of PNE in patients with recent onset LBP is a promising and feasible approach to the management of recent onset LBP. Patients presenting with recent onset LBP and higher levels of risk for chronicity may indeed benefit from PNE in the early stages of management and thus allow for a biopsychosocial PT treatment approach. However, further studies involving larger samples and a comparison group are needed to test this proposal.
Biographies
Adriaan Louw, PT, PhD, CSMT is co-founder and CEO of International Spine and Pain Institute and guest lecturer/adjunct faculty at St. Ambrose University. He has a certificate in spinal manual therapy and has presented at numerous national and international manual therapy, pain science and medical conferences, and has authored and co-authored articles, books and book chapters related to spinal disorders and pain science.
Kevin Farrell, PT, PhD, OCS, FAAOMPT is a professor in the Physical Therapy Department and serves as Chair of the Clinical Residency program in Orthopaedic Physical Therapy at St. Ambrose University. He is a board certified orthopaedic clinical specialist and a Fellow in the American Academy of Orthopaedic Manual Physical Therapists.
Breanna Choffin, PT, DPT, OCS, CMT is staff physical therapist at Vanderbilt University in Nashville, TN. She is graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Brooke Foster, PT, DPT, OCS, CMT is staff physical therapist at Genesis Rehab in Silvis, IL. She is graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Grace Lunde, PT, DPT, OCS, CMT is staff physical therapist at Genesis Rehab in Davenport, IA. She is graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Michelle Snodgrass, PT, DPT, OCS, CMT is staff physical therapist at Rock Valley Physical Therapy in Geneseo, IL. She is graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Robert Sweet, PT, DPT, OCS, CMT is staff physical therapist at Edward Elmhurst Health in Naperville, IL. He is graduate of Southwest Baptist DPT program and the St. Ambrose University residency program. He is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Matthew Weitzel, PT, DPT, OCS, CMT is staff physical therapist at Rock Valley Physical Therapy in Davenport, IA. He is graduate of St. Ambrose University DPT and residency programs. He is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Rebecca Wilder, PT, DPT, OCS, CMT is staff physical therapist at Genesis Rehab in Moline, IL. She is graduate of St. Ambrose University DPT and residency programs. She is a board certified orthopaedic clinical specialist and has a certificate in manual therapy.
Emilio J. Puentedura, PT, DPT, PhD, OCS, CSMT, FAAOMPT is a professor in the Doctor of Physical Therapy Program at Baylor University. He is a board certified orthopaedic clinical specialist, a Fellow in the American Academy of Orthopaedic Manual Physical Therapists, and has a certificate in spinal manual therapy.
Funding Statement
None to report
Disclosure statement
The authors Adriaan Louw, PT, PhD and Emilio Puentedura. PT, PhD, acknowledge receiving payment for various speaking events (seminars, conferences, etc.) as well as royalties from books, from professionals and patients. None of these conflicts influence the subject matter or materials discussed in this manuscript.
Ethical approval
The study was approved by the Internal Review Board (IRB) at St. Ambrose University, Davenport, IA.
References
- [1].Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012. December 15;380(9859):2163–2196. PubMed PMID: 23245607; PubMed Central PMCID: PMCPMC6350784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Henschke N, Ostelo RW, van Tulder MW, et al. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev. 2010. July 7;(7):CD002014 DOI: 10.1002/14651858.CD002014.pub3 PubMed PMID: 20614428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rubinstein SM, van Middelkoop M, Kuijpers T, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J. 2010. August;19(8):1213–1228. PubMed PMID: 20229280; PubMed Central PMCID: PMCPMC2989199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kuijpers T, van Middelkoop M, Rubinstein SM, et al. A systematic review on the effectiveness of pharmacological interventions for chronic non-specific low-back pain. Eur Spine J. 2011. January;20(1):40–50. PubMed PMID: 20680369; PubMed Central PMCID: PMCPMC3036024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Henschke N, Kuijpers T, Rubinstein SM, et al. Injection therapy and denervation procedures for chronic low-back pain: a systematic review. Eur Spine J. 2010. September;19(9):1425–1449. PubMed PMID: 20424870; PubMed Central PMCID: PMCPMC2989278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hush JM, Refshauge K, Sullivan G, et al. Recovery: what does this mean to patients with low back pain? Arthritis Rheum. 2009. January 15;61(1):124–131. PubMed PMID: 19116958. [DOI] [PubMed] [Google Scholar]
- [7].McGreevy K, Bottros MM, Raja SN.. Preventing chronic pain following acute pain: risk factors, preventive strategies, and their efficacy. Eur J Pain Suppl. 2011;52:365–372. PubMed PMID: 22102847; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Diener I, Kargela M, Louw A. Listening is therapy: patient interviewing from a pain science perspective. Physiother Theory Pract. 2016. July;32(5):356–367.. PubMed PMID: 27351690; eng. [DOI] [PubMed] [Google Scholar]
- [9].Zimney K, Louw A, Puentedura EJ. Use of therapeutic neuroscience education to address psychosocial factors associated with acute low back pain: a case report. Physiother Theory Pract. 2014. April;30(3):202–209. PubMed PMID: 24252071; eng. [DOI] [PubMed] [Google Scholar]
- [10].George DR, Dreibelbis TD, Aumiller B. Google Docs and surveymonkey: lecture-based active learning tools. Med Educ. 2013. May;47(5):518 PubMed PMID: 23574071; eng. [DOI] [PubMed] [Google Scholar]
- [11].Kendall NAS, Linton SJ, Main CJ. Guide to assessing psychosocial yellow flags in acute low back pain: risk factors for long term disability and work loss. Wellington: Accident Rehabilitation & Compensation Insurance Corporation of New Zealand and the National Health Committee; 1997. [Google Scholar]
- [12].Nijs J, Van Houdenhove B, Oostendorp RA. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice [Review]. Man Ther. 2010. April;15(2):135–141. PubMed PMID: 20036180; eng. [DOI] [PubMed] [Google Scholar]
- [13].Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–322. [DOI] [PubMed] [Google Scholar]
- [14].Moseley GL. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4): 297–302. PubMed PMID: 12443524; eng. [DOI] [PubMed] [Google Scholar]
- [15].Moseley GL. Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap. 2003;11(2):88–94. [Google Scholar]
- [16].Meeus M, Nijs J, Van Oosterwijck J, et al. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2010. August;91(8):1153–1159. PubMed PMID: 20684894; Eng. [DOI] [PubMed] [Google Scholar]
- [17].Louw A, Zimney K, Puentedura EJ, et al. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016. July;32(5):332–355. PubMed PMID: 27351541; eng. [DOI] [PubMed] [Google Scholar]
- [18].Louw A, Diener I, Butler DS, et al. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil. 2011. December;92(12):2041–2056. PubMed PMID: 22133255; eng. [DOI] [PubMed] [Google Scholar]
- [19].Louw A, Puentedura EJ, Zimney K, et al. The clinical implementation of pain neuroscience education: A survey study. Physiother Theory Pract. 2017. November;33(11):869–879. PubMed PMID: 28820626. [DOI] [PubMed] [Google Scholar]
- [20].Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017. July;25(3):160–168.. PubMed PMID: 28694679; PubMed Central PMCID: PMC5498797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Louw A, Puentedura EJ, Zimney K, et al. Know pain, know gain? A perspective on pain neuroscience education in physical therapy. J Orthop Sports Phys Ther. 2016. March;46(3):131–134. PubMed PMID: 26928735; eng. [DOI] [PubMed] [Google Scholar]
- [22].Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007. June;37(6):290–302. PubMed PMID: 17612355; eng. [DOI] [PubMed] [Google Scholar]
- [23].Fritz JM, Lindsay W, Matheson JW, et al. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine (Phila Pa 1976). 2007. December 15;32(26):E793–800. PubMed PMID: 18091473; eng. [DOI] [PubMed] [Google Scholar]
- [24].Will JS, Bury DC, Miller JA. Mechanical low back pain. Am Fam Physician. 2018. October 1;98(7):421–428. PubMed PMID: 30252425. [PubMed] [Google Scholar]
- [25].Von Korff M, Dunn KM. Chronic pain reconsidered. Pain. 2008. August 31;138(2):267–276. PubMed PMID: 18226858; PubMed Central PMCID: PMCPMC2613775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Latimer J, Maher C, Refshauge K. The attitudes and beliefs of physiotherapy studetns to chronic back pain. Clin J Pain. 2004;20:45–50. [DOI] [PubMed] [Google Scholar]
- [27].Louw A, Diener I, Landers MR, et al. Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine (Phila Pa 1976). 2014. August 15;39(18):1449–1457. PubMed PMID: 24875964; eng. [DOI] [PubMed] [Google Scholar]
- [28].Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51(1): 49–52. PubMed PMID: 15748125; eng. [DOI] [PubMed] [Google Scholar]
- [29].Cleland JA, Childs JD, Whitman JM. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008. January;89(1):69–74. PubMed PMID: 18164333; eng. [DOI] [PubMed] [Google Scholar]
- [30].Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005. June 1;30(11):1331–1334. PubMed PMID: 15928561. [DOI] [PubMed] [Google Scholar]
- [31].Cleland JA, Fritz JM, Childs JD. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Am J Phys Med Rehabil. 2008. February;87(2):109–117.. PubMed PMID: 17993982; eng. [DOI] [PubMed] [Google Scholar]
- [32].Grotle M, Vollestad NK, Brox JI. Clinical course and impact of fear-avoidance beliefs in low back pain: prospective cohort study of acute and chronic low back pain: II. Spine (Phila Pa 1976). 2006. April 20;31(9):1038–1046. PubMed PMID: 16641782; eng. [DOI] [PubMed] [Google Scholar]
- [33].Poiraudeau S, Rannou F, Baron G, et al. Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 2006. October;124(3):305–311. PubMed PMID: 16740362; eng. [DOI] [PubMed] [Google Scholar]
- [34].Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002. October;82(10):973–983. PubMed PMID: 12350212; eng. [PubMed] [Google Scholar]
- [35].Burton AK, Waddell G, Tillotson KM, et al. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care [Clinical Trial Randomized Controlled Trial]. Spine (Phila Pa 1976). 1999. December 1;24(23):2484–2491. PubMed PMID: 10626311; eng. [DOI] [PubMed] [Google Scholar]
- [36].George SZ, Fritz JM, McNeil DW. Fear-avoidance beliefs as measured by the fear-avoidance beliefs questionnaire: change in fear-avoidance beliefs questionnaire is predictive of change in self-report of disability and pain intensity for patients with acute low back pain. Clin J Pain. 2006. February;22(2):197–203. PubMed PMID: 16428956; eng. [DOI] [PubMed] [Google Scholar]
- [37].Deyo RA, Battie M, Beurskens AJ, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976). 1998. September 15;23(18):2003–2013. PubMed PMID: 9779535; eng. [DOI] [PubMed] [Google Scholar]
- [38].Fritz JM, Irrgang JJ. A comparison of a modified oswestry low back pain disability questionnaire and the quebec back pain disability scale. Phys Ther. 2001. February;81(2):776–788. PubMed PMID: 11175676; eng. [DOI] [PubMed] [Google Scholar]
- [39].Hakkinen A, Kautiainen H, Jarvenpaa S, et al. Changes in the total oswestry index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007. March;16(3):347–352. PubMed PMID: 16912888; eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Philapa 1976). 2008. January 1;33(1):90–94. PubMed PMID: 18165753. [DOI] [PubMed] [Google Scholar]
- [41].Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–330. PubMed PMID: 15322439; eng Sep-Oct. [DOI] [PubMed] [Google Scholar]
- [42].Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004. February;8(1):39–45. PubMed PMID: 14690673; eng. [DOI] [PubMed] [Google Scholar]
- [43].Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–532. [Google Scholar]
- [44].George SZ, Valencia C, Beneciuk JM. A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. J Orthop Sports Phys Ther. 2010. April;40(4):197–205.. PubMed PMID: 20357418. [DOI] [PubMed] [Google Scholar]
- [45].Mayer TG, Neblett R, Cohen H, et al. The development and psychometric validation of the central sensitization inventory [Research Support, N.I.H., Extramural Validation Studies]. Pain Pract. 2012. April;12(4):276–285. PubMed PMID: 21951710; PubMed Central PMCID: PMC3248986. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Neblett R, Hartzell MM, Williams M, et al. Use of the central sensitization inventory (CSI) as a treatment outcome measure for patients with chronic spinal pain disorder in a functional restoration program. Spine J. 2017. December;17(12):1819–1829. PubMed PMID: 28619687. [DOI] [PubMed] [Google Scholar]
- [47].Choi YH. An examination of the validity of the central sensitization inventory with chronic disabling occupational musculoskeletal disorders. Ann Arbor, MI: ProQuest Information and Learning; 2014. [Google Scholar]
- [48].Scerbo T, Colasurdo J, Dunn S, et al. Measurement properties of the central sensitization inventory: a systematic review. Pain Pract. 2018. April;18(4):544–554. PubMed PMID: 28851012. [DOI] [PubMed] [Google Scholar]
- [49].Wall PD, Melzack R. Textbook of pain. 5th ed. London: Elsevier; 2005. [Google Scholar]
- [50].Moseley GL. Unravelling the barriers to reconceptualisation of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. 2003;4(4):184–189. [DOI] [PubMed] [Google Scholar]
- [51].Catley MJ, O’Connell NE, Moseley GL. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties [Randomized Controlled Trial]. J Pain. 2013. August;14(8):818–827. PubMed PMID: 23651882; eng. [DOI] [PubMed] [Google Scholar]
- [52].Louw A, Puentedura E, Schmidt S, et al. Pain neuroscience education: teaching people about pain. 2nd Minneapolis, MN: OPTP; 2018. [Google Scholar]
- [53].Hill JC, Vohora K, Dunn KM, et al. Comparing the STarT back screening tool’s subgroup allocation of individual patients with that of independent clinical experts [Comparative Study Research Support, Non-U.S. Gov’t]. Clin J Pain. 2010;26(9):783–787. PubMed PMID: 20842014; eng Nov-Dec. [DOI] [PubMed] [Google Scholar]
- [54].Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2019. March 2 DOI: 10.1136/bjsports-2018-099878 PubMed PMID: 30826805. [DOI] [PubMed] [Google Scholar]
- [55].Ekedahl H, Jonsson B, Frobell RB. Fingertip-to-floor test and straight leg raising test: validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch Phys Med Rehabil. 2012. December;93(12):2210–2215. PubMed PMID: 22555005; eng. [DOI] [PubMed] [Google Scholar]
- [56].Verbeek J, Sengers MJ, Riemens L, et al. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine (Phila Pa 1976). 2004. October 15;29(20):2309–2318. PubMed PMID: 15480147; eng. [DOI] [PubMed] [Google Scholar]
- [57].Hopayian K, Notley C. A systematic review of low back pain and sciatica patients’ expectations and experiences of health care [Research Support, Non-U.S. Gov’t Review]. Spine J. 2014. August 1;14(8):1769–1780. PubMed PMID: 24787355; eng. [DOI] [PubMed] [Google Scholar]
- [58].McRae M, Hancock MJ. Adults attending private physiotherapy practices seek diagnosis, pain relief, improved function, education and prevention: a survey. J Physiother. 2017. October;63(4):250–256. PubMed PMID: 28967562. [DOI] [PubMed] [Google Scholar]
- [59].Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989. December;10(4):407–415. PubMed PMID: 2691207. [DOI] [PubMed] [Google Scholar]
- [60].Louw A, Butler DS, Diener I, et al. Development of a preoperative neuroscience educational program for patients with lumbar radiculopathy [Comparative Study Review]. Am J Phys Med Rehabil. 2013. May;92(5):446–452. PubMed PMID: 23478459; eng. [DOI] [PubMed] [Google Scholar]
- [61].Louw A, Zimney K, O’Hotto C, et al. The clinical application of teaching people about pain. Physiother Theory Pract. 2016. July;32(5):385–395. PubMed PMID: 27351903; eng. [DOI] [PubMed] [Google Scholar]
- [62].Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain: systematic review and meta-analysis. Man Ther. 2011. December;16(6):544–549. PubMed PMID: 21705261. [DOI] [PubMed] [Google Scholar]
- [63].Karjalainen K, Malmivaara A, van Tulder M et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults [Review]. Cochrane Database Syst Rev. 2000. (3):CD002194 DOI: 10.1002/14651858.CD002194 PubMed PMID: 10908529; eng. [DOI] [PubMed] [Google Scholar]
- [64].Karjalainen K, Malmivaara A, van Tulder M et al.Multidisciplinary biopsychosocial rehabilitation for subacute low back pain among working age adults [Review]. Cochrane Database Syst Rev. 2003. (2):CD002193 DOI: 10.1002/14651858.CD002193 PubMed PMID: 12804427; eng. [DOI] [PubMed] [Google Scholar]
- [65].Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2014. September 2;(9):CD000963 DOI: 10.1002/14651858.CD000963.pub3 PubMed PMID: 25180773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Linton SJ, Shaw WS. Impact of psychological factors in the experience of pain. Phys Ther. 2011. May;91(5):700–711. PubMed PMID: 21451097. [DOI] [PubMed] [Google Scholar]
- [67].Choiniere M, Dion D, Peng P, et al. The Canadian STOP-PAIN project - Part 1: who are the patients on the waitlists of multidisciplinary pain treatment facilities? [Multicenter Study Research Support, Non-U.S. Gov’t]. Can J Anaesth. 2010. June;57(6):539–548. PubMed PMID: 20393821; eng. [DOI] [PubMed] [Google Scholar]
- [68].Guerriere DN, Choiniere M, Dion D, et al. The Canadian STOP-PAIN project - Part 2: what is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? [Research Support, Non-U.S. Gov’t]. Can J Anaesth. 2010. June;57(6):549–558. PubMed PMID: 20414821; eng. [DOI] [PubMed] [Google Scholar]
- [69].Castel LD, Freburger JK, Holmes GM, et al. Spine and pain clinics serving North Carolina patients with back and neck pain: what do they do, and are they multidisciplinary? [Research Support, N.I.H., Extramural Research Support, U.S. Gov’t, P.H.S.]. Spine (Phila Pa 1976). 2009. March 15;34(6):615–622. PubMed PMID: 19282742; PubMed Central PMCID: PMC2757449. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].BuildPT.com GetPT1st 2019. 2019. March 31 Available from: http://getpt1st.com/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- BuildPT.com GetPT1st 2019. 2019. March 31 Available from: http://getpt1st.com/


