Abstract
Context: Bladder dysfunction is common in patients with spinal cord injuries. Clean intermittent catheterization is a preferred method of neurogenic bladder management among spinal cord injured patients. Some complications may occur due to the use of clean intermittent catheterization.
Findings: In this report, we presented a case with an unexpected foreign body detected in the bladder of a patient who used to perform clean intermittent catheterization for her neurogenic bladder management, to our knowledge, which has not been reported in the literature so far.
Conclusion/Clinical Relevance: In this case report, we want to emphasis the importance of different kind of foreign bodies remaining in the bladder during clean intermittent catheterization.
Keywords: Bladder management, Clean intermittent catheterization, Foreign body, Neurogenic bladder, Spinal cord injury
Introduction
Spinal cord injury (SCI) is a serious medical condition that causes disability throughout life. Bladder dysfunctions are one of the most common complications seen after SCI, which has the prevalence of 70–84%.1 Clean intermittent catheterization (CIC) is one of the methods used for the management of bladder dysfunctions. CIC is a suitable method for spinal cord injured patients who have adequate hand strength, no obstruction in the urethra, and co-operative features.2 The use of CIC in patients with SCI provides not only appropriate emptying of the bladder but also the continence. In addition, CIC prevents serious lower urinary tract infections and upper urinary tract system damage. However, infection, hematuria, urethral trauma, urethritis, and the remaining of a foreign body are some of the complications of CIC.3 Here, we aimed to draw attention on an unexpected complication of CIC in a patient with spinal cord injury. To our knowledge, foreign body related to its own part of the catheter has never been reported yet.
Case report
A 40-year-old female patient was interned to our service for rehabilitation. She sustained a non-vehicle traffic accident that caused a vertebral fracture and spinal contusion at T11 vertebra level eight months ago. Neurological examination of the patient was done according to the Neurological Classification of Spinal Cord Injury developed by American Spinal Injury Association (ASIA), and her ASIA impairment scale (AIS) level was T10 AIS A. She has undergone an anticholinergic drug (Oxybutynin HCL 10 mg/day) and advised self CIC (6 times a day) due to the detrusor overactivity in the urodynamic study which was performed to the patient at another center before coming to our rehabilitation service. The training of CIC was given to the patient by the rehabilitation nurse. The patient performed the CIC with 20 cm length and 14 Fr thickness self-lubricating hydrophilic catheter for 4-hour intervals. According to the Modified Ashworth Scale, grade 3 spasticity was evaluated in bilateral hip adductor, whereas grades 2 and 3 spasticities were evaluated in bilateral knee extensors, and bilateral ankle plantar flexors, respectively.
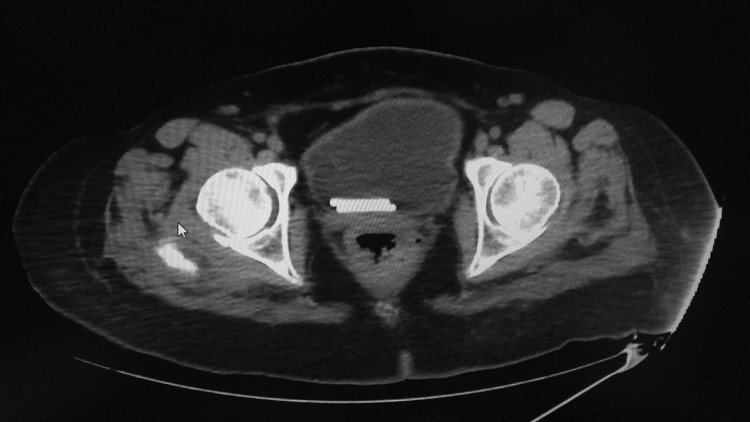
The patient who described a recent increase in spasticity and urinary leakage was requested blood and urine analysis, and there was an elevation in sedimentation rate and C-reactive protein level, whereas 14 leukocytes (Normal values: 0–4) were detected in the urine microscope. For this reason, a urine culture was done, and 105 CFU/ml of Escherichia coli was detected. The patient was undergone antibiotherapy due to the diagnosis of urinary tract infection (UTI). Radiology consultation was requested for urinary tract evaluation, and a linear echogenic appearance with 19 mm size was detected in the bladder with urinary system ultrasonography (USG) by radiologist. Due to the inability to identify foreign objects with USG, the bladder lumen was evaluated by urinary system computed tomography (CT) with the pre-diagnosis of stone in the bladder, and two rod-like foreign body densities were observed in the bladder lumen (Fig. 1). Urology consultation was done for foreign body densities, and two cylindrically shaped and 3.5 cm in length foreign bodies were extracted from the patient’s bladder with cystoscopy by a urologist (Fig. 2). It was found that the extracted foreign bodies were the ‘insertion sleeves’ which were located on the catheter that prevented hand contact during CIC. However, the patient claimed that she was not aware that deterioration of the integrity of the catheter during any CIC that she performed recently. After the removal of foreign bodies from the bladder, the patient showed a decrease in not only urinary leakage but also in spasticity grade by 1 grade. We gave a training to the patient and caregiver about the possibility of such complications.
Figure 1.
The two rod-like foreign body densities in the bladder lumen in computed tomography.
Figure 2.
The foreign bodies extracted from the patient’s bladder.
Discussion
Complications, such as UTIs, scrotal complications (such as epididymitis and epididymo-orchitis), urethral stricture, urethral bleeding, urethral false passage, perineal abscess, and bladder stone, may be seen in patients who perform CIC.3 Bladder stones are common complications in SCI patients. Linsenmeyer et al.4 reported that bladder stones are the second most common urological complications in SCI patients. The incidence of stones in the bladder may be related to the method of bladder drainage. Ord et al.5 reported that the incidence of absolute annual risk of bladder stone in patients with SCI was 4% for those with indwelling urethral or suprapubic catheterization, whereas it was 0.2% in patients using intermittent self-catheterization. In a study, Bartel et al.4 reported that the risk of bladder stone incidence in patients with reflex micturition or using intermittent catheterization was lower than patients using permanent catheters. In the same study, the possibility of bladder stone recurrence was also higher in patients using permanent catheters. Although the risk of intra-bladder stone formation is reduced by CIC, bladder stones should be kept in mind first when foreign bodies detected in the bladder.
There are studies which reported that stone formations formed by hairs entering the bladder.6,7 Pubic hairs may enter into the bladder either by adhering directly to the lubricated catheter, or by overlying the urethral meatus and being pushed into the bladder. The hair in the bladder is an ideal place for crystals to precipitate, which facilitates stone formation, which is manifested by the presence of hair formations within the stones that removed from the bladder.6,7 Many unusual foreign bodies that range from the electric wire, thermometer to glass rods and battery have been reported. In addition, mental disorder, psychosexual disorder and iatrogenic causes have been reported in its etiology.8,9 None of these etiologic factors was present in our patient. In neurogenic bladder patients performing CIC, we did not detect any foreign body report except for stone, pubic hair, and vaginal contraceptive ring.6,9
Chronic persistence of foreign bodies in the bladder causes significant complications. In the literature, recurrent urinary system infections, acute urinary retention, calcification, scrotal gangrene, vesicovaginal fistula, and death from sepsis have been reported.8 Intravesical foreign body-induced bladder calculi may be caused renal failure due to obstruction in the urinary system.10 In the long term, foreign bodies may cause chronic bladder irritation, and this way may induce squamous cell carcinoma. It has been reported that in patients with spinal cord injuries, the use of CIC prevents the bladder cancer comparing to indwelling catheterization.11 However, it should not be forgotten that the CIC fragments which may remain in the bladder can increase the risk of bladder cancer.12
If the CIC fragment remains in the bladder, a possible explanation for this could be that this condition may be caused by the poor quality of the catheter used. A poor quality catheter may break during the CIC application and remain in the urinary system. However, the quality of the catheter used by our patient was approved by the quality standards institution in our country. Based on our observations, this situation was likely to be the result of the carelessness of the patient who performed self CIC. Educating patients about CIC method is very important. In the literature, 11.4% of patients with neurogenic bladder is reported that lack of proper training was an obstacle to CIC method.13,14 We think that proper education of CIC could reduce complications due to catheterization.
Periodic evaluation of the urinary system is recommended because of the frequent occurrence of urinary complications in neurogenic bladder patients.15 In this respect, it is important to perform tests, such as urinalysis, USG which will evaluate the urinary system at certain intervals. However, we should highlight that there is not consensus on the frequency of urine screening that needs to be performed. The European Association of Urology recommends that in high-risk patients, the upper urinary tract should be evaluated by USG at least every six months, and physical examination and urinalysis should be performed every year. At the same time, if there is a significant change in the clinical condition of the patient, it is recommended to carry out further necessary investigations for the urinary system.16 It should not be forgotten that patients with SCI may have systemic complications such as urinary system complications in cases of increased spasticity or urinary leakage.
Conclusion
In neurogenic bladder patients, fragments related to its own part of the catheter may remain in the bladder during CIC, and a proper education should be given to prevent such complications. It should be kept in mind that when foreign bodies detected in the bladder of patients who perform CIC, it may rarely be catheter fragment.
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest Authors have no conflicts of interest to declare.
ORCID
Alper Mengi http://orcid.org/0000-0003-0898-764X
References
- 1.Lamin E, Newman DK.. Clean intermittent catheterization revisited. Int Urol Nephrol 2016;48:931–9. doi: 10.1007/s11255-016-1236-9 [DOI] [PubMed] [Google Scholar]
- 2.Binard JE, Persky L, Lockhart JL, Kelley B.. Intermittent catheterization the right way! (volume vs. time-directed). J Spinal Cord Med 1996;19:194–6. doi: 10.1080/10790268.1996.11719432 [DOI] [PubMed] [Google Scholar]
- 3.Di Benedetto P. Clean intermittent self-catheterization in neuro-urology. Eur J Phys Rehabil Med 2011;47:651–9. [PubMed] [Google Scholar]
- 4.Bartel P, Krebs J, Wöllner J, Göcking K, Pannek J.. Bladder stones in patients with spinal cord injury: a long-term study. Spinal Cord 2014;52:295–7. doi: 10.1038/sc.2014.1 [DOI] [PubMed] [Google Scholar]
- 5.Ord J, Lunn D, Reynard J.. Bladder management and risk of bladder stone formation in spinal cord injured patients. J Urol 2003;170:1734–7. doi: 10.1097/01.ju.0000091780.59573.fa [DOI] [PubMed] [Google Scholar]
- 6.Joshi M, Mittal N.. Bladder calculi formed over a hair nidus in spinal injury cases. J Spinal Cord Med 2014;37:346–8. doi: 10.1179/2045772313Y.0000000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee HJ, Kim SH.. Characteristic plain radiographic and intravenous urographic findings of bladder calculi formed over a hair nidus: a case report. Korean J Radiol 2001;2:61. doi: 10.3348/kjr.2001.2.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rafique M. Intravesical foreign bodies: review and current management strategies. J Urol 2008;5:223–31. [PubMed] [Google Scholar]
- 9.Ehdaie B, Mason MD, Peters CA, Corbett ST.. Transurethral placement of vaginal contraceptive device in a patient with neurogenic bladder: a case report and review of the literature. J Pediatr Urol 2013;9:e107–10. doi: 10.1016/j.jpurol.2012.11.008 [DOI] [PubMed] [Google Scholar]
- 10.Kamal F, Clark AT, Lavallιe LT, Roberts M, Watterson J.. Intravesical foreign body-induced bladder calculi resulting in obstructive renal failure. Can Urol Assoc J 2008;2:546–8. doi: 10.5489/cuaj.927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.West DA, Cummings JM, Longo WE, Virgo KS, Johnson FE, Parra RO.. Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology 1999;53:292–7. doi: 10.1016/S0090-4295(98)00517-2 [DOI] [PubMed] [Google Scholar]
- 12.Pannek J. Transitional cell carcinoma in patients with spinal cord injury: a high risk malignancy? Urology 2002;59:240–4. doi: 10.1016/S0090-4295(01)01495-9 [DOI] [PubMed] [Google Scholar]
- 13.Bolinger R, Engberg S.. Barriers, complications, adherence, and self-reported quality of life for people using clean intermittent catheterization. J Wound Ostomy Continence Nurs 2013;40:83–9. doi: 10.1097/WON.0b013e3182750117 [DOI] [PubMed] [Google Scholar]
- 14.Le Breton F, Guinet A, Verollet D, Jousse M, Amarenco G.. Therapeutic education and intermittent self-catheterization: recommendations for an educational program and a literature review. Ann Phys Rehabil Med 2012;55:201–12. doi: 10.1016/j.rehab.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 15.Averbeck MA, Madersbacher H.. Follow-up of the neuro-urological patient: a systematic review. BJU Int 2015;115:39–46. doi: 10.1111/bju.13084 [DOI] [PubMed] [Google Scholar]
- 16.Groen J, Pannek J, Diaz DC, Del Popolo G, Gross T, Hamid R, et al. Summary of European Association of Urology (EAU) guidelines on neuro-urology. Eur Urol 2016;69:324–33. doi: 10.1016/j.eururo.2015.07.071 [DOI] [PubMed] [Google Scholar]