Abstract
Declining a donor when there is a reasonable possibility that the abnormality on chest imaging could be benign carries the risk of losing out on potentially usable lungs in an already parched landscape of donor organ availability. Cautiously aggressive attitudes to acceptance of borderline donors can help bridge the significant discrepancy that exists between the demand and availability of donor organs. Herein, we present a case highlighting successful bilateral lung transplantation from a relatively imperfect donor.
INTRODUCTION
Across the globe, an increasing number of patients with end stage lung pathology are reaping the benefits of lung transplantation. In 2018, more than 4500 lung transplants were performed worldwide. Despite this, there remains a profound gulf in the demand and availability of potentially usable organs, culminating in significant morbidity and mortality on the lung transplant waitlist. Strategies including ex vivo lung perfusion techniques and utilization of organs from cardiac death donors as well as donors with hepatitis C infection are being investigated to address this void. We present a case of successful transplantation where lungs were procured from a donor with mass lesions at two different visceral locations.
CASE REPORT
A 58-year-old man with idiopathic pulmonary fibrosis listed for lung transplantation received a donor lung offer from a 46 year old non-smoking brain dead female donor. Prior to us receiving the offer, the donor lungs had been rejected by three other centers. The Lung Allocation Score for their three recipients ranged from 51.4 to 89.87. The donor blood gasses revealed excellent oxygenation with a PaO2 of 567 mmHg. Chest radiograph, however, revealed a large calcified mass confirmed on computed tomography (CT) as a 3 cm × 3 cm mass in the left lower lobe of the lung (Fig. 1). CT imaging of the abdomen and pelvis revealed a cystic right ovarian lesion measuring 7.3 cm × 4.2 cm × 4.8 cm. The presence of large pulmonary and ovarian masses created initial doubt and hesitation about the safety of using the lungs for transplantation. Due diligence was exercised and discussions were conducted with multiple team members and radiologists. Radiologic appearance of both (pulmonary and ovarian) masses was deemed to be benign and the lungs were accepted. Ovarian biopsy at procurement confirmed a benign mucinous cystadenoma. Bilateral sequential lung transplantation was performed along with backtable wedge resection of left lower lobe lung mass prior to implantation of the left lung. Grossly, the cut surface of the mass had a chalky white appearance. (Fig. 2) Histopathologic examination revealed the pulmonary mass to be a benign hyalinized necrotizing granuloma. (Fig. 3) Postoperatively, the patient did well with no evidence of primary graft dysfunction. More than 1 year after the transplant, the recipient continues to do well with excellent functional status without any evidence of chronic lung allograft dysfunction.
Figure 1.

CT scan of the chest with calcified nodule in left lower lobe.
Figure 2.

Cut section of left lower lobe nodule.
Figure 3.
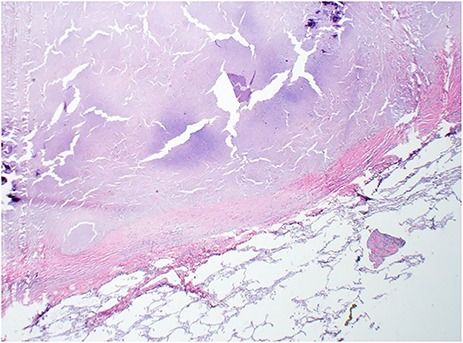
H&E of left lung nodule from wedge resection with hyalinized necrotizing granuloma and surrounding normal lung parenchyma (2×).
DISCUSSION
Despite efforts to maximize donor pool with the use of donation after cardiac death, ex vivo lung perfusion and hepatitis C-infected donors, overall lung procurement rate in the United States remains at a modest 22.2%. This is in sharp contrast to Eurotransplant and Australian regions where the organ utilization rates are much higher at 32.4 and 44%, respectively [1].
A clear chest radiograph is a pivotal component of the traditional definition of an ideal donor [2]. In the era of increasing reliance on CT scans of the chest, incidentally detected pulmonary nodules are relatively common. Even among smokers, the vast majority of nodules identified on CT scan of the chest are benign [3]. Common non-neoplastic lung masses that manifest on chest imaging in otherwise asymptomatic individuals include infectious as well as vasculitic granulomatous lesions. Less common are benign masses emanating from nodular lymphoid hyperplasia, nodular amyloid, IgG4 related sclerosing lesions as well as pulmonary hyalinizing granulomas (PHG), as seen in our donor [4]. Although deemed benign, PHG has been reported to be associated with a systemic disorder in approximately 50% of reported cases. The spectrum of affliction includes mediastinal and retroperitoneal fibrosis, autoimmune disorders and infections as well as tumors—none of which have manifested in our recipient to date [5].
Excluding a potentially usable donor organ based on the presence of a potentially benign pulmonary nodule limits organ utilization in this already parched landscape. This case highlights the significance of complementing the aforementioned innovative strategies with aggressive attitudes to evaluation and acceptance of marginal but potentially transplantable organs. As we strive toward the era of bioartificial organ availability, it remains paramount that we maximize available donor organ use to ameliorate the morbidity and mortality for our waitlisted patients.
REFERENCES
- 1. Paraskeva MA, Levin KC, Westall GP, Snell GI. Lung transplantation in Australia, 1986–2018: more than 30 years in the making. Med J Aust. 2018;208:445–50. [DOI] [PubMed] [Google Scholar]
- 2. Orens JB, Boehler A, de Perrot M, Estenne M, Glanville AR, Keshavjee S, et al. . Pulmonary council, International Society for Heart and Lung Transplantation. A review of lung transplant donor acceptability criteria. J Heart Lung Transplant. 2003;22:1183–200. [DOI] [PubMed] [Google Scholar]
- 3. McWilliams A, Tammemagi MC, Mayo JR, Roberts H, Liu G, Soghrati K, et al. . Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369:910–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borczuk AC. Neoplastic and nonneoplastic benign mass lesions of the lung. Arch Pathol Lab Med. 2012;136:1227–33. [DOI] [PubMed] [Google Scholar]
- 5. Lhote R, Haroche J, Duron L, Girard N, Lafourcade MP, Martin M, et al. . Pulmonary hyalinizing granuloma: a multicenter study of 5 new cases and review of the 135 cases of the literature. Immunol Res. 2017;65:375–85. [DOI] [PubMed] [Google Scholar]


