Abstract
Purpose: In this cross-sectional study, we examined the distribution of physiotherapists at the health region level across Canada in relation to self-reported physiotherapy use across the provinces and territories. Method: We drew on two data sources: the physiotherapy use question from the 2014 Canadian Community Health Survey and physiotherapists’ primary employment information, obtained from the Canadian Institute of Health Information’s 2015 Physiotherapist Database. We then applied geospatial mapping and Pearson’s correlation analysis to the resulting variables. Results: Physiotherapy use is moderately associated with the distribution of physiotherapists (Pearson’s r92 = 0.581, p < 0.001). The use and distribution variables were converted into three categories using SDs of 0.5 from national means as cut-off values. Cross-classification between the variables revealed that 15.2% of health regions have a high use–high distribution ratio; 18.5% have a low use–low distribution ratio; 4.3% have a high use–low distribution ratio; 2.2% have a low use–high distribution ratio; and 60.0% have medium use–medium distribution ratio. Conclusions: The distribution of physiotherapists and self-reported physiotherapy use varies across health regions, indicating a potential inequality in geographical access. Given that most provinces have a regionalized approach to health human resources and health service delivery, these findings may be helpful to managers and policy-makers and may allow them to make a more granular comparison of intra- and inter-provincial differences and potential gaps.
Key Words: geographic mapping, health resources, health services, spatial analysis
Abstract
Objectif : la présente étude transversale a porté sur la répartition des physiothérapeutes dans les régions sanitaires du Canada par rapport à l’utilisation déclarée des services de physiothérapie dans les provinces et territoires. Méthodologie : les chercheurs ont puisé dans deux sources de données : la question sur l’utilisation des services de physiothérapie de l’Enquête sur la santé dans les collectivités canadiennes de 2014 et les renseignements sur l’emploi primaire des physiothérapeutes tirés de la Base de données sur les physiothérapeutes de l’Institut canadien d’information sur la santé de 2015. Ils ont ensuite appliqué la cartographie géospatiale et l’analyse de corrélation de Pearson aux variables obtenues. Résultats : l’utilisation des services de physiothérapie s’associe modérément à la répartition des physiothérapeutes (r92 de Pearson = 0,581, p < 0,001). Les chercheurs ont converti les variables d’utilisation et de répartition en trois catégories, dont les seuils correspondaient aux écarts-types de ± 0,5 des moyennes nationales. La classification transversale entre les variables a révélé que 15,2 % des régions sanitaires présentaient un ratio forte utilisation/forte répartition, 18,5 %, un ratio faible utilisation/faible répartition; 4,3 %, un ratio forte utilisation/faible répartition, 2,2 % un ratio faible utilisation/forte répartition et 60,0 %, une combinaison de ratios utilisation modérée/répartition modérée. Conclusions : la répartition des physiothérapeutes et l’utilisation déclarée de services de physiothérapie varient selon les régions sanitaires, ce qui est indicateur d’inégalités potentielles à l’égard de l’accessibilité géographique. Puisque la plupart des provinces ont une approche régionale des effectifs en santé et de la prestation des services de santé, ces observations peuvent être utiles pour les gestionnaires et les décideurs, qui peuvent s’en servir pour faire une comparaison plus stricte des différences intraprovinciales et interprovinciales et des lacunes potentielles.
Mots-clés : analyse spatiale, cartographie géographique, ressources de santé, services de santé
Faced with an aging population1 and an increase in the prevalence of chronic diseases,2 the Canadian health care system needs to examine whether rehabilitation services are organized and distributed to adequately meet the population’s health needs. Some research has suggested that they are not, particularly when it comes to mobility and pain management.3 Physiotherapists serve an important role in facilitating the restoration of physical function, mobility, reduced pain, and other symptoms, ultimately assisting people with a range of health conditions to return to work, recreation, and other life roles.3–5 Although a growing body of research has examined access to rehabilitation services,6–9 ensuring equitable access to non-physician health care providers, such as physiotherapists, has traditionally received less policy attention than medical services.10 Despite the potential contribution of physiotherapists to the health and well-being of different populations, equitable access to their services can be affected by a range of variables, including geographical barriers.9,11–13
Like many other developed countries, Canada is facing a shortage of health care workers and dealing with the issues of recruiting and retaining health care providers in regions with low population density, particularly rural and remote areas.11,14 However, self-reported use of physiotherapy among the adult population has been increasing (from 8.4% in 2001 to 11.6% in 2014), revealing a growing demand for this service.3 Previous research in Canada has identified significant variations in the distribution of physiotherapists in relation to potential need in Ontario, Quebec, and Saskatchewan.6,8,12 The recently released “Market Profile of Physiotherapists in Canada,” published by the Conference Board of Canada, provides a snapshot of physiotherapist distribution and use at the provincial and terriorial levels across Canada.15 This report concluded that the number of Canadians who have consulted a physiotherapist has steadily increased across Canada; the availability of physiotherapists likely does not satisfy this dramatic rise in demand; and the vast majority of physiotherapists (approximately 90%) work in urban areas, with the result that large gaps in access exist in rural and remote areas.15 It did not, however, examine the relationship of these two variables at the more granular health region level at which health human resources and delivery are typically managed.
Our objective in this study was to analyze the distribution of physiotherapists at the health region level and its association with self-reported physiotherapy use across Canada. By mapping the geographical distribution of physiotherapists in relation to use, we can graphically demonstrate where access to physiotherapy could be optimized. This research is novel in that we examine both physiotherapist distribution and physiotherapy use across health regions and provide a nationwide comparison using geospatial mapping.
Methods
We gathered data from two databases of cross-sectional information, then applied geospatial analysis to map the distribution of physiotherapy use in relation to the availability of physiotherapists across Canadian health regions.
Data on self-reported physiotherapy use
We derived data on self-reported physiotherapy use from Statistics Canada’s confidential microdata files for the Canadian Community Health Survey (CCHS), accessed through the Saskatchewan Research Data Centre.16 Research using Statistics Canada datasets such as the CCHS is exempt from institutional ethics approval. The data were collected from persons aged 12 years or older living in Canadian health regions (approximately 65,000 people). This survey did not include people living on a reserve (or in any other Aboriginal settlement) or full-time members of the Canadian Armed Forces.
Our study focused on the physiotherapy use question (Contacts with Health Professionals Question 18) from the 2014 CCHS Annual Component: “Not counting when you were an overnight patient, in the past 12 months, have you seen, or talked to: a physiotherapist (about your physical, emotional or mental health)?” From the answers to this question, we determined the proportion of the population who self-reported using physiotherapy services in the previous year in their health region.
Data on availability of physiotherapy
We determined the availability of physiotherapy as the number of physiotherapists per 10,000 population at the health region level (i.e., the physiotherapist distribution ratio). The number of physiotherapists by health region was provided by the Canadian Institute for Health Information (CIHI) and was based on its 2015 Physiotherapist Database (which represents the provincial physiotherapy regulators’ submission of 2015 license renewal data to CIHI). CIHI was unable to provide physiotherapist information for the Northwest Territories, Nunavut, and certain health regions for the following reasons: the information is not collected by the data provider on the registration form or a data provider cannot submit the information; no licensing bodies exist to provide data for these territories;17 the information was not provided by the registrant; the data element was not relevant to the registrant’s situation; or the data did not meet CIHI confidentiality regulations (i.e., data with fewer than five data points could not be released). As a result, three health regions were not included in our analysis.
We calculated the physiotherapist distribution ratio for each health region using 2016 census population figures and CIHI’s Physiotherapist Database.18 To align with the CCHS question that asked people to report physiotherapy use not counting as an overnight patient, we included physiotherapists working in community and professional practice settings (as a place of primary employment) in the analysis but excluded physiotherapists working in hospitals and non-clinical settings such as academe and management. Physiotherapy use and physiotherapist distribution ratio data were the variables used in our analysis.
The CCHS had collected data on physiotherapy use from 114 provincial health regions. Health regions are provincially defined administrative areas or geographical regions of interest to health authorities that are subject to change over time.19 From these, we excluded 4 with missing physiotherapy use data, physiotherapist distribution ratio, or both. To ensure that the two variables referred to the same geographical area, we merged 3 health regions from Saskatchewan into one combined region and grouped 9 health regions from Nova Scotia into four health management zones. In total, 103 health regions (consisting of combined regions, management zones, regional health authorities) were incorporated into the map.
Geospatial mapping
Using geospatial mapping techniques, we linked the physiotherapy use and physiotherapist distribution ratio variables with Statistics Canada’s Health Regions boundary layer to display the distribution patterns.19 For mapping purposes, we converted both variables to categorical variables by following an SD classification scheme.20 We then divided each variable into the following three categories, using an SD of 0.5 from the national mean value as a cutoff: lower (<−0.5 SD from the mean), moderate (±0.5 SD from the mean), and higher (>0.5 SD from the mean). We subsequently applied a thematic mapping tool available in ArcGIS Desktop software (Version 10.5; ESRI, Redlands, CA) to graphically represent the distribution of physiotherapy use in relation to the physiotherapist distribution ratio. We performed descriptive statistics and correlational analyses using IBM SPSS Statistics (Version 24; IBM Corp., Armonk, NY) to check the data distribution and determine the relationship between the two variables. We used Pearson’s correlation method to empirically explore the association between the two variables.
Results
The average proportion of physiotherapy use by health region was 10.79% (SD = 3.29; range, min–max, 3.13–19.70; skewness = 0.56, n = 103), whereas the average distribution of physiotherapists across health regions was 2.32 physiotherapists per 10,000 people (SD = 1.32; range, min–max, 0.11– 6.60; skewness = 0.95; n = 92). We found a moderately positive correlation between the two variables (Spearman’s ρ = 0.521; p < 0.001; n = 92), which indicates that physiotherapy use is associated with the supply of physiotherapists at the health region level across Canada.
The three categories of each variable revealed the following: for physiotherapy use, lower, <9.15%; moderate, 9.15%–12.44%; and higher, >12.44%; and for physiotherapist distribution ratio, lower, <1.66 physiotherapists per 10,000 population; moderate, 1.66–2.99 physiotherapists per 10,000 population; and higher, >2.99 physiotherapists per 10,000 population. The number of physiotherapists by primary place of employment and physiotherapist distribution ratio is presented in Table 1.
Table 1.
Number of Physiotherapists by Primary Place of Employment by Physiotherapist Distribution Ratio
| Physiotherapist distribution ratio* |
||||
|---|---|---|---|---|
| Primary place of employment | Lower (< 1.66) | Moderate (1.66–2.99) | Higher (> 2.99) | Total |
| Community | 453 | 829 | 714 | 1,996 |
| Professional practice† | 678 | 2,529 | 3,560 | 6,767 |
| Total (included) | 1,131 | 3,358 | 4,274 | 8,763 |
| Not included in the mapping (or analysis) | ||||
| Hospital | 8,127 | |||
| Other | 3,197 | |||
| Missing | 159 | |||
| Total (not included) | 11,483 | |||
Measured as the number of physiotherapists per 10,000 population at the health region level.
Defined by the Canadian Institute for Health Information as a group professional practice, clinic, or solo professional practice or business.
Figure 1 presents a graphical representation of the distribution of physiotherapy use in relation to the physiotherapist distribution ratio by health region (i.e., the spatial distribution of the cross-classification categories between self-reported physiotherapy use and physiotherapist distribution ratio). It shows that, with regard to self-reported physiotherapy use, 27 health regions were in the lower categories; 39, in the moderate categories; and 26, in the higher categories (the sum of each use column in the legend). With regard to the physiotherapist distribution ratio, 36 health regions were in the lower categories; 33, in the moderate categories; and 23, in the higher categories (the sum of each ratio row in the legend).
Figure 1.
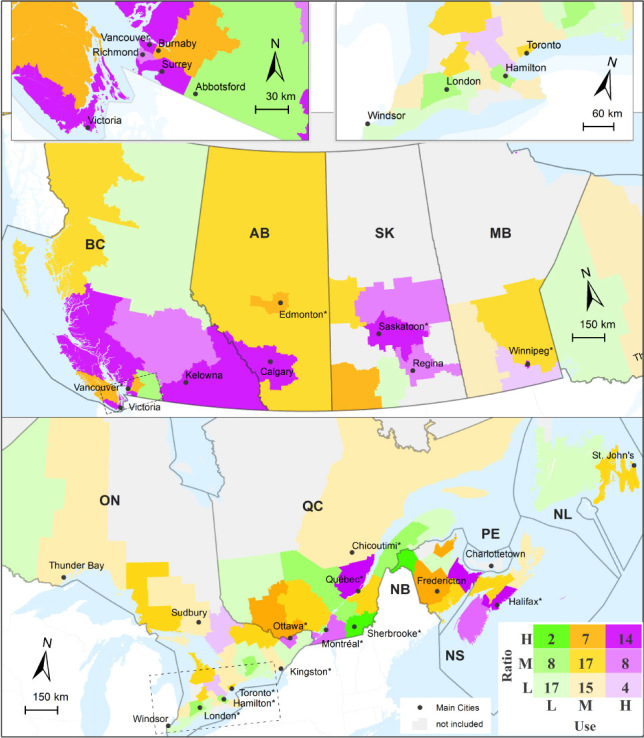
Graphical representation of the distribution of physiotherapy use in relation to the physiotherapist distribution ratio by health region.
As a result of this cross-classification among the categorical variables for which both variables had valid values (i.e., 11 health regions had no ratios), we divided the 92 health regions into nine category combinations. A total of 14 health regions (15.2%) fell into the high use–high distribution ratio combination. A total of 17 health regions (18.5%) fell into the low use–low distribution ratio combination (1 health region in each of New Brunswick and Saskatchewan; 2 each in British Columbia, Newfoundland and Labrador, and Quebec; and 9 in Ontario). High use–low distribution ratio combinations were found in 4 health regions (4.3%; 1 in Manitoba and 3 in Ontario), and low use–high distribution ratio combinations were found in 2 health regions (2.2%; 1 each in New Brunswick and Quebec). We found other combinations with moderate use or distribution in 55 health regions.
Discussion
The purpose of this study was to analyze how closely the distribution of physiotherapists at the health region level matched self-reported physiotherapy use across the Canadian provinces. Using geospatial mapping, we created a cross-classification comparison between self-reported physiotherapy use, reported in the 2014 CCHS data, and the physiotherapist distribution ratio, derived from the 2015 CIHI Physiotherapist Database. We found a moderately positive correlation between use and the distribution ratio, indicating that physiotherapy use is associated with the availability of physiotherapists at the health region level. However, we also found discrepancies between the availability of physiotherapists and physiotherapy use across health regions. Our results agree with a recent Conference Board of Canada report that states that “regional [i.e., provincial] variations exist in publicly funded [physiotherapy] services across the country, contributing to access challenges.”15(p. 6) Our results further support the imbalance in distribution in provincial jurisdictions that has been found in previous research.6,8,12
Comparing health region differences within and between provinces at the health region level can help determine where access to physiotherapy services could be optimized. For example, our research indicates that 18.5% of Canadian health regions have both low use and low distribution. These health regions tend to be in more rural, remote, or northern parts of many provinces (e.g., British Columbia, Saskatchewan, Ontario, Quebec, New Brunswick, Newfoundland and Labrador). In addition to the greater challenges of accessing health care services, rural and remote residents have a higher prevalence of many chronic health conditions, which would likely benefit from physiotherapy services.21–22 To address these access disparities, therefore, these findings may help direct policy- and decision makers in the health system regarding where a need exists to focus on recruiting and retaining physiotherapists in addition to implementing innovative service delivery models.23 A high reported use of physiotherapy services but low physiotherapy distribution may represent a health region in which residents have to travel to another health region to receive services or where they receive services using alternative models, such as telehealth23–25 or distributed practice models (sometimes referred to as “hub and spoke”).
Another mismatch occurs in health regions in which there is a high proportion of physiotherapists per population but lower physiotherapy use (i.e., two health regions located in Quebec). The reasons for this mismatch are unclear, but they may indicate that residents of those particular health regions travel elsewhere to obtain physiotherapy services or other differences in local physiotherapy service delivery models unique to those regions. In addition, our results show that 14 health regions (8 in British Columbia and 1 each in Alberta, Manitoba, New Brunswick, Nova Scotia, Quebec, and Saskatchewan) fall in the high use–high distribution combination. People living in these health regions tend to have higher socioeconomic status, with universities offering physiotherapy education (5 health regions), or more urban locales (e.g., Vancouver, Calgary, Winnipeg), with high use of physiotherapy services and an abundance of physiotherapists.
However, 55 of the 92 health regions (approximately 60%) have moderate use–moderate distribution combinations. Given the lack of a gold standard for an optimal distribution-to-use ratio, whether these moderate combinations indicate a balance in the supply and use of physiotherapy services is unclear. Health regions with a high use–moderate distribution ratio or a high use–low distribution ratio (8 and 4 health regions, respectively) are, in most cases, located close to high use–high distribution ratio health regions. It may be that in some of the health regions with a high use–moderate or low distribution ratio, residents travel to adjacent health regions in which there are a greater number of physiotherapists.
Equitable access to health care means that services are available wherever and whenever a person needs them. A primary objective of the Canada Health Act is to protect, promote, and restore the physical and mental well-being of residents of Canada and to facilitate reasonable access to health care services without financial or other barriers.26 Under the act, provinces are required to cover medically necessary health services provided in hospitals and those provided by physicians in all settings;26 however, outpatient physiotherapy services provided outside of a hospital are variably funded by provincial governments.6,27–29
Adequate geographical distribution of health human resources and services is a key component of ensuring equitable access to health care.30–31 Realized access is actual use of services, whereas potential access is linked to an individual’s perception of access as well as other contextual and environmental factors, such as geographical distribution of services.32 Our findings highlight variations in the distribution of physiotherapists relative to use across Canadian health regions, suggesting that potential gaps exist in equitable access to care. It is important to note that physiotherapy use data do not directly relate to population health needs because those who need the service may not necessarily be able to access care for a variety of reasons. Access and use are not synonymous because individuals may need to overcome barriers that limit their access to a particular service in order to use it.33 In addition, an individual’s health care needs do not necessarily reflect access to particular services, nor do health care needs consistently correlate with patterns of health care use.34
Several limitations to our study should be considered. As previously stated, CIHI data were not available for two territories and a few health regions for multiple reasons; as a result, we could not perform a comprehensive nationwide analysis. There is also potential variability in how the provincial regulatory boards collected the data before submitting them to CIHI. Because of CIHI’s confidentiality guidelines, we were unable to include 11 health regions or report findings for the two territories.
Our analysis included data from two data sources from different, but temporally close, years (2014 CCHS, 2015 CIHI Physiotherapist Database); thus, we cannot with certainty state that this is a true cross-sectional representation of physiotherapy distribution matched with use across the same time period. However, the use of large data sources over somewhat different but close timeframes is not uncommon in similar types of research6,12 and is the best known option available.
We were also not able to include physiotherapists’ number of work hours; some health regions with reduced use but a higher number of physiotherapists may represent more physiotherapists who are working part time. Approximately 36% of physiotherapists in Canada work part time, with significant variation across the country (ranging from 10.3% in Newfoundland and Labrador to 51.3% in the Yukon);35 therefore, geospatial analysis of all physiotherapists regardless of full-time or part-time status may under-represent actual geospatial access disparities. Further work is needed to fully understand the implications of a part-time workforce for use patterns at various geographical and administrative levels. Also, physiotherapists who were on leave or working in management or academic roles may still have been included, even when they were not providing actual services. We attempted to focus our analysis on those physiotherapists who were more likely to be providing direct patient care by removing those who reported working in a management or academic setting (e.g., university). However, the analysis may still have included some physiotherapists who provide relatively little or no patient care.
We used only physiotherapists’ primary place of employment; therefore, our mapping did not capture those who travel to multiple locations or who provide services to other health regions. This potential for misclassification could alter our results in either direction. We also excluded physiotherapists working in hospital settings so that our analysis would reflect community-based care; however, the results do not capture physiotherapists who provide outpatient services in a hospital setting. Research has shown that outpatient hospital departments may be where the majority of publicly funded physiotherapy is delivered in some provinces.6 Approximately 40% of physiotherapists in Canada report working in a hospital or long-term care facility;36 thus, our analysis did not account for people who did indeed use physiotherapy services in a hospital, either as an inpatient or as both an inpatient and an outpatient.
The question in the 2014 CCHS regarding physiotherapy use asks patients about receiving care from a physiotherapist “not counting [being] an overnight patient.” Thus, people who received care from a physiotherapist as a hospital inpatient or as a resident of a long-term care facility may have responded no to this question. Although the answers help to determine community-based or outpatient physiotherapy use, they do not take into account physiotherapy delivered to inpatients in hospitals or residents of long-term care facilities. Versions of the CCHS earlier than 2011 do not include this wording.
Despite the many challenges inherent in using CIHI and CCHS data sources to investigate physiotherapist distribution relative to use, these are the only known national data sources. Future research investigating the geographical distribution of physiotherapists in a province or smaller geographical unit relative to use may overcome some of the aforementioned challenges by linking these data sources with clinical or administrative data sources (if available).
Conclusion
Our findings of variation in the distribution of physiotherapy providers and self-reported use across Canadian health regions indicate that geographical access to physiotherapy services is unequal. However, using these results to inform practice will depend on the local context and the combination of local factors that drive both ratio and use. Managers play a role in identifying gaps and lobbying policy-makers for resources, but it is beyond the scope of this article to recommend any specific steps that they should take.
Key Messages
What is already known on this topic
Despite the potential contribution of physiotherapists to the health and well-being of different populations, equitable access to physiotherapy is limited; a number of factors may contribute to this situation, including geographical distribution of service provision. Self-reported use of physiotherapy has increased over the past several years; however, whether provision is addressing this increasing demand is unclear.
What this study adds
Our findings of variation in the distribution of physiotherapists and self-reported use across Canadian health regions indicate unequal geographical access to physiotherapy services. Given that most provinces have a regionalized approach to health human resources and health service delivery, understanding how physiotherapy use and distribution are related may be helpful to managers and policy-makers and provide a more detailed comparison of intra- and inter-provincial differences and potential gaps. Comparing differences within and between provinces at the health region level may help to guide where and how access to physiotherapy services can be optimized.
References
- 1. Statistics Canada. Population trends by age and sex, 2016 Census of Population [Internet]. Ottawa: Statistics Canada; 2017. [cited 2018 May 24]. Available from: http://www.statcan.gc.ca/pub/11-627-m/11-627-m2017016-eng.htm. [Google Scholar]
- 2. Roberts KC, Rao DP, Bennett TL, et al. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health Promot Chronic Dis Prev Can: Res Pol Pract. 2015;35(6):87–94. 10.24095/hpcdp.35.6.01. Medline:26302227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martinello N, Bhandari A, Santos J, et al. The role of physiotherapy in Canada: contributing to a stronger health care system. Ottawa: Conference Board of Canada; 2017. [Google Scholar]
- 4. Saskatchewan Physiotherapy Association. What is physiotherapy. Saskatoon, SK: The Association; 2015. [cited 2015 May 5]. Available from: http://www.saskphysio.org/physiotherapy/what-is-physiotherapy. [Google Scholar]
- 5. Marks D, Comans T, Bisset L, et al. Substitution of doctors with physiotherapists in the management of common musculoskeletal disorders: a systematic review. Physiotherapy. 2017;103(4):341–51. 10.1016/j.physio.2016.11.006. Medline:28801031 [DOI] [PubMed] [Google Scholar]
- 6. Deslauriers S, Raymond MH, Laliberte M, et al. Variations in demand and provision for publicly funded outpatient musculoskeletal physiotherapy services across Quebec, Canada. J Eval Clin Pract. 2017;23(6):1489–97. 10.1111/jep.12838. Medline:29063716 [DOI] [PubMed] [Google Scholar]
- 7. Passalent L, Borsy E, Landry MD, et al. Geographic information systems (GIS): an emerging method to assess demand and provision for rehabilitation services. Disabil Rehabil. 2013;35(20):1740–9. 10.3109/09638288.2012.750690. Medline:23343362 [DOI] [PubMed] [Google Scholar]
- 8. McFadden B, Jones McGrath K, Lowe T, et al. Examining the supply of and demand for physiotherapy in Saskatchewan: the relationship between where physiotherapists work and population health need. Physiother Can. 2016;68(4):335–45. 10.3138/ptc.2015-70. Medline:27904233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bath B, Jakubowski M, Mazzei D, et al. Factors associated with reduced perceived access to physiotherapy services among people with low back disorders. Physiother Can. 2016;68(3):260–6. 10.3138/ptc.2015-50. Medline:27909375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barnes S, Dolan L-A, Gardner B, et al. Equitable access to rehabilitation: realizing potential, promising practices, and policy directions. Toronto: Canadian Working Group on HIV and Rehabilitation and Wellesley Institute; 2012. [Google Scholar]
- 11. Dussault G, Franceschini M. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Hum Resour Health. 2006;4(1):12 10.1186/1478-4491-4-12. Medline:16729892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holyoke P, Verrier MC, Landry MD, et al. The distribution of physiotherapists in Ontario: understanding the market drivers. Physiother Can. 2012;64(4):329–37. 10.3138/ptc.2011-32. Medline:23997387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Adams R, Jones A, Lefmann S, et al. Rationing is a reality in rural physiotherapy: a qualitative exploration of service level decision-making. BMC Health Serv Res. 2015;15(1):121 10.1186/s12913-015-0786-3. Medline:25880469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Watanabe-Galloway S, Madison L, Watkins KL, et al. Recruitment and retention of mental health care providers in rural Nebraska: perceptions of providers and administrators. Rural Remote Health. 2015;15(4):3392 Medline:26567807 [PubMed] [Google Scholar]
- 15. Sutherland G. The market profile of physiotherapists in Canada. Ottawa: Conference Board of Canada; 2017. [Google Scholar]
- 16. Saskatchewan Research Data Centre (SKY-RDC). Data sets available at the SKY-RDC [Internet]. Saskatoon: SKY–RDC; 2014. [cited 2015 Sep 28]. Available from: http://library.usask.ca/sky-rdc/Data.html. [Google Scholar]
- 17. Canadian Institute for Health Information (CIHI). Health workforce database methodology guide for data tables, 2014: medical laboratory technologists, medical radiation technologists, occupational therapists, pharmacists and physiotherapists. Ottawa: CIHI; 2015. [Google Scholar]
- 18. Statistics Canada. Age (in single years) and average age (127) and sex (3) for the population of Canada, provinces and territories, census divisions, census subdivisions and dissemination areas, 2016 census – 100% data [Internet]. Ottawa: Statistics Canada; 2018. [cited 2018 Sep 28]. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=0&GK=0&GRP=1&PID=109525&PRID=0&PTYPE=109445& S=0&SHOWALL=0&SUB=0&Temporal=2016&THEME=115&VID=0& VNAMEE=&VNAMEF=. [Google Scholar]
- 19. Statistics Canada. Health regions: boundaries and correspondence with census geography (HRP000b11a_e_Oct2013) [Internet]. Ottawa: Statistics Canada; 2013. [cited 2018 June 3]. Available from: http://www5.statcan.gc.ca/olc-cel/olc?ObjId=82-402-X2013002&ObjType=46&lang=en. [Google Scholar]
- 20. Cromley EK, McLafferty SL. GIS and public health. 2nd ed. New York: Guilford Press; 2012. [Google Scholar]
- 21. Pong RW, DesMeules M, Lagacé C.. Rural–urban disparities in health: how does Canada fare and how does Canada compare with Australia? Aust J Rural Health. 2009;17(1):58–64. 10.1111/j.1440-1584.2008.01039.x. Medline:19161503 [DOI] [PubMed] [Google Scholar]
- 22. Bath B, Trask C, McCrosky J, et al. Demographic and health characteristics of rural- and urban-dwelling Canadians with chronic back disorders: a population-based comparison. Spine (Phila Pa 1976). 2014;39(23):1960–8. 10.1097/brs.0000000000000561. Medline:25365711 [DOI] [PubMed] [Google Scholar]
- 23. Lovo Grona S, Bath B, Bustamante L, et al. Case report: using a remote presence robot to improve access to physical therapy for people with chronic back disorders in an underserved community. Physiother Can. 2017;69(1):14–19. 10.3138/ptc.2015-77. Medline:28154440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lovo Grona S, Bath B, Busch A, et al. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2017;24(5):341–55. 10.1177/1357633x17700781. Medline:28403669 [DOI] [PubMed] [Google Scholar]
- 25. Bath B, Lovo Grona S, Milosavljevic S, et al. Advancing interprofessional primary health care services in rural settings for people with chronic low back disorders: protocol of a community-based randomized controlled trial. JMIR Res Protoc. 2016;5(4):e212 10.2196/resprot.5914. Medline:27829573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Canada Health Act. RSC 1985, c C-6 (1985).
- 27. Landry MD, Deber RB, Jaglal S, et al. Assessing the consequences of delisting publicly funded community-based physical therapy on self-reported health in Ontario, Canada: a prospective cohort study. Int J Rehabil Res 2006;29(4):303–7. 10.1097/mrr.0b013e328010badc. Medline:17106346 [DOI] [PubMed] [Google Scholar]
- 28. Gordon M, Waines B, Englehart J, et al. The consequences of delisting publicly funded, community-based physical therapy services in Ontario: a health policy analysis. Physiother Can. 2007;59(1):58–69. 10.3138/ptc.59.1.58. [DOI] [Google Scholar]
- 29. Paul J, Park L, Ryter E, et al. Delisting publicly funded community-based physical therapy services in Ontario, Canada: a 12-month follow-up study of the perceptions of clients and providers. Physiother Theory Pract. 2008;24(5):329–43. 10.1080/09593980802278397. Medline:18821440 [DOI] [PubMed] [Google Scholar]
- 30. Campbell J, Buchan J, Cometto G, et al. Human resources for health and universal health coverage: fostering equity and effective coverage. Bull World Health Organ. 2013;91(11):853–63. 10.2471/blt.13.118729. Medline:24347710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Landry MD, Tepper J, Verrier MC. Moving from “muddling throughˮ to careful planning: physical therapy human resources in Canada. Physiother Can. 2009;61(2):60–2. 10.3138/physio.61.2.60. Medline:20190987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981;19(12):4–27. 10.1097/00005650-198112001-00004. Medline:11643688 [DOI] [PubMed] [Google Scholar]
- 33. Thorpe JM, Thorpe CT, Kennelty KA, et al. Patterns of perceived barriers to medical care in older adults: a latent class analysis. BMC Health Serv Res. 2011;11(1):181 10.1186/1472-6963-11-181. Medline:21812953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70(3):465–72. 10.1016/j.socscimed.2009.10.027. Medline:19914759 [DOI] [PubMed] [Google Scholar]
- 35. Canadian Institute for Health Information (CIHI). Physiotherapists, 2016: Data tables. Ottawa: CIHI; 2016. [Google Scholar]
- 36. CIHI. Physiotherapist workforce, by place of employment and jurisdiction, Canada, 2007 to 2016 Physiotherapists, 2016: data tables. Ottawa: Canadian Institute for Health Information; 2016. [Google Scholar]


