Abstract
Introduction
The aim of this study was to describe the complications of ureteroscopy (URS) and to investigate whether performing URS outside normal working hours leads to increased risk for clinically significant complications.
Material and methods
A cohort of 486 consecutive patients treated with URS, with a total of 567 sessions between 2009 and 2015 at Helsingborg/Ängelholm Hospital, Sweden, was analyzed. Outcome was complications within 14 days after URS treatment.
Results
We found no increased risk of complications related to URS performed outside normal working hours. Stone-free rate (SFR) in the distal third of the ureter was 95.2% (315/331), in the middle ureter 92.8% (90/97), in the proximal ureter 84.0% (63/75) and 69.0% (40/58) in renal pelvis. The overall complication rate was 10.6% (n = 60). None of the potential risk factors for complications showed any significance when adjusted for age and gender. We found an inverse relationship between stenting and SFR (p = 0.002). The most common preoperatively cultured bacteria was Escherichia coli. With adequate antibiotics, there was no increased risk of complications. There was an increased risk of complications after URS related to age, but not with gender.
Conclusions
URS in modern setting provides excellent results with adequate SFR and low morbidity. Time of day, the presence of urological specialized operating nurses did not affect the risk of complications and we found no other significant risk factors for complications. Escherichia coli was the most commonly found bacteria in preoperative cultures. The risk of complications increases with age. For patients >65 years old, this should be considered in preoperative counseling.
Keywords: complications, infection, monotherapy, ureteric stone, ureteroscopy, stone
INTRODUCTION
For the past 7,000 years our civilizations have been trying to find a cure to the suffering caused by stones in the urinary tract [1]. We can now treat stones within the urinary tract, and minimize the morbidity and mortality. In Sweden, the incidence of urolithiasis is 1–2% in males and 0.5% in females [2]. The prevalence was over 10% in males and 3% in females. The recurrence of urolithiasis within 10 years has been reported to be 26% in first-time stone formers [3]. The prevalence of urolithiasis in Western countries range from 8-19% in males and from 3–5% in females [4] and the prevalence of urolithiasis is increasing [5].
Studies suggest that ureteroscopy (URS) is as effective as extracorporeal shockwave lithotripsy (ESWL) for treating stones also in proximal parts of the urinary tract [6, 7]. The guidelines of the European Association of Urology (EAU) [8] recommend using either ESWL or URS for stones <2 cm. With the exception of untreated urinary tract infections (UTI) and contraindications for general anesthesia, URS can be safely performed in the majority of patients. The Holmium: YAG laser is effective on all types of stones and is nowadays considered the gold standard for stone disintegration. Preoperative stenting has been shown to increase the success rate of the URS treatment [9]. The usage of postoperative stents in URS can, however, cause irritative lower urinary symptoms [10].
Stone-free rate (SFR) is used to measure outcome and successful treatment. Residual stones ≤4 mm in diameter after treatment have been considered clinically insignificant, and the patient considered stone- free [11]. The complication rates range from 9–25%, after URS [8].
A urine culture is mandatory according the EAU guidelines, and patients with a UTI should receive antibiotic treatment prior to URS [8]. The most common bacteria causing a UTI is Escherichia coli [12]. The complication rates for post-URS UTI range from 2–4%, and the rates of sepsis range from 2–4% [13].
The discussion of whether stone surgery should be done outside normal working hours or not is debated within the urological society. The influence of personnel not specially trained in urological procedures (on- call operating personnel) and whether the surgeon's fatigue may affect outcome and complication rates is debated and sometimes used as an excuse for not preforming stone surgery at night.
The objective of this study is to retrospectively evaluate the outcome of patients treated with URS in the north-western part of the Scania County, Sweden, during the period of 2009 to 2015. Additionally, our goal was to describe the complication's related to URS. Evaluating and understanding the complications may potentially lead to better patient selection and consequently improved safety for patients treated with URS.
MATERIAL AND METHODS
All consecutive patients treated with URS at Helsingborg/Ängelholm Hospital in the north-western part of Scania County, Sweden, during the period 2009–2015, were included. Symptomatic stones >6 mm were considered a treatment indication. Stones <6 mm persisting after one month on X-ray were also considered a treatment indication.
The method used to treat the stone was decided by the urologist in consensus with the patient. Patients with stones >6 mm and located in the lower third part of the ureter were recommended URS. Pre-URS stenting was not used routinely.
A semi-rigid ureteroscope was used when the stone was located in the ureter. A flexible ureteroscope was used in the renal pelvis. Holmium Laser was used for fragmentation.
For the journal search the Swedish surgical codes for nephro-pyelo-lithotomy, urethero-lithotomy, and uretheroscopy were used, also including the diagnoses in the updated Charlson Comorbidity Index and mortality [14] (see Appendix 1).
The data gathered were: sex; age at intervention; size and location of stones according to pre- and postoperative computed tomography (CT) scan; pre- and postoperative use of pigtail stent; preoperative urine culture; type of bacteria; pre-, per-, and postoperative antibiotics; days with antibiotics; days of hospitalization; and if the patient sought medical attention at the emergency department within 14 days of the surgery.
Stone-free status was defined as absence of stones or presence of residuals ≤4 mm, in accordance with the clinic standard, evaluated on postoperative CT, and presented as: no residual stones, residual stones ≤2 mm, and residual stones ≤4 mm. If the urologist during the operation could confirm that all stones and fragment were removed, it was not mandatory to follow-up with a CT. For patients without a follow-up CT, the medical records were re-examined ensuring that the patient had not sought medical attention due to stone events within one year after the treatment. To evaluate if the complication rate could correlate to the personnel performing surgery (on-call personnel/normal operating personnel), if fatigue could be a factor (nights, not between 0800-1700) or if surgery was performed acute or elective could have an effect on complications, data was collected from the surgical procedures. Additionally, flexible and semi-rigid ureteroscopy were compared regarding the complication rates.
To grade surgical complications, a modified version of the Clavien-Dindo classification was used (see Appendix 2). The classification can be used in all types of surgery [15].
For patients registered at the emergency department within 14 days, further data were extracted: cause of admission decided by the admitting doctor (infection, bleed, pain, or other); days until readmission; if the patient was readmitted; days of re-hospitalization; if blood and/or urine cultures were taken; type of bacteria; antibiotics given; ICU treatment; respiratory rate; level of consciousness; and if the systolic blood pressure were below 100 mmHg.
Registration of the long-term mortality was made on December 12, 2017, ranging from 3 to 9 years. The mortality was reviewed and registered at fixed intervals following the URS treatment; at 28 days, 90 days, 1 years, 2 years, 3 years, 5 years, and 8 years.
Statistical methods
For correlations between different variables, univariate logistic regression analyses were used. If the analyses were found to be statistically significant, multivariate logistic regression was used comparing the multiple covariates to the same dependent. When the multivariate logistic regression analysis was used, gender and age were included as predefined confounding variables. In case of a small sample (n <10/covariate) no multivariate logistic regression analysis was used. When comparing non-binary variables, the Kruskal-Wallis test was used. The value of p <0.05 was considered statistically significant. The statistical analyses were performed using IBM SPSS for Mac OS v24.0.0.0.
This study was approved by the local ethics committee at Lund University (Dnr 2017/15) and the head of the Department of Urology at Helsingborg Hospital.
RESULTS
Between January 2009 and December 2015, 486 individual patients were treated with URS in a total of 567 sessions. In 60.4% (343/568) the patients could be discharged from the hospital on the same day. If admitted the mean hospitalization time was 2.0 days.
81 (14.3%) patients demanded multiple sessions, whereas 28 (4.9%) of the patients were treated two times, five patients were treated three times, and two patients were treated five times. Twenty patients (3.5%) were re- treated for the same stone within 6 months.
Age, sex, Charlson Comorbidity Index score, diabetic comorbidity, long-term mortality, and the Clavien- Dindo classification score are presented in Table 1. The overall SFR was 90.7% (515/56799 (Table 2). All patients who were readmitted within 14 days (Figure 1) scored ≥1 according to Clavien-Dindo system [15]. Data regarding stone location in the ureter, stone size, and the use of ureteral stents are presented in Table 2.
Table 1.
Patient characteristics and complications
| All patients (n = 567) | Patients not seeking medical within 14 days (n = 507) | Patients seeking medical care within 14 days (n = 60) | ||
|---|---|---|---|---|
| Age, Mean (±SD) | 55.0 (16.3) | 54.8 (16.1) | 56.7 (18.1) | |
| Diabetes | 12.2% (n = 69) | 12.4% (n = 63) | 10.0% (n = 6) | |
| Sex M:F ratio | 2.5:1 | 2.6:1 | 2:1 | |
| Charlson Comorbidity Index |
0 1 2 3 4 6 7 8 |
71.4% (n = 405) 6.2% (n = 35) 15.9% (n = 90) 3.9% (n = 22) 1.6% (n = 9) 0.4% (n = 2) 0.2% (n = 1) 0.5% (n = 3) |
72.0% (n = 365) 5.5% (n = 28) 15.4% (n = 78) 4.1% (n = 21) 1.8% (n = 9) 0.4% (n = 2) 0.2% (n = 1) 0.6% (n = 3) |
66.7% (n = 40) 11.7% (n = 7) 20.0% (n = 12) 1.7% (n = 1) – – – – |
| Mortality | 28-d 90-d 1y 2y 3y 5y 8y |
– 0.2% (n = 1) 0.9% (n = 5) 2.1% (n = 12) 2.8% (n = 16) 4.8% (n = 27) 6.0% (n = 34) |
– – 0.8% (n = 4) 2.0% (n = 10) 2.6% (n = 13) 5.1 % (n = 26) 5.9 % (n = 30) |
1.7% (n = 1) 1.7% (n = 1) 3.3% (n = 2) 5.0% (n = 3) 5.0% (n = 3) 6.7% (n = 4) |
| Clavien-Dindo Classification Score |
0 1 2 3 4 |
79.4% (n = 450) 12.0% (n = 68) 6.5% (n = 37) 1.9% (n = 11) 0.2% (n = 1) |
87.2% (n = 442) 9.9% (n = 50) 2.2% (n = 11) 0.8% (n = 4) – |
13.3% (n = 8) 30.0% (n = 18) 43.3% (n = 26) 11.7% (n = 7) 1.7% (n = 1) |
Table 2.
Stone characteristics and use of ureteral stent
| All patients (n = 567) | Patients not seeking medical care within 14 days (n = 507) | Patients seeking medical care within 14 days (n = 60) | ||
|---|---|---|---|---|
| Stone location | Distal Middle Proximal Renal pelvis Bilateral |
58.4% (n = 331) 17.1% (n = 97) 13.2% (n = 75) 10.2% (n = 58) 1.1% (n = 6) |
58.4% (n = 296) 17.9% (n = 91) 13.2% (n = 67) 9.5% (n = 48) 1.0% (n = 5) |
58.3% (n = 35) 10.0% (n = 6) 13.3% (n = 8) 16.7% (n = 10) 1.7% (n = 1) |
| Stone size | ≤2 mm >2≤4 mm >4-≤6 mm >6≤10 mm >10 mm |
1.8%(n = 10) 18.0% (n = 102) 32.3% (n = 183) 40.2% (n = 228) 7.7% (n = 44) |
1.6% (n = 8) 18.1% (n = 92) 33.2% (n = 168) 39.3% (n = 199) 7.9% (n = 40) |
3.3% (n = 2) 16.7% (n = 10) 25.0% (n = 15) 48.3% (n = 29) 6.7 (n = 4) |
| Stone size at follow-up | No residual stones ≤2 mm >2≤4 mm >4-≤6 mm >6≤10 mm >10 mm No follow-up Patient no-show No longer in Scania |
59.8% (n = 339) 3.5% (n = 20) 3.2% (n = 18) 5.8% (n = 33) 2.8%(n = 16) 1.1% (n = 6) 21.7% (n = 123) 1.9% (n = 11) 0.2% (n = 1) |
59.2% (n = 300) 3.4% (n = 17) 2.4% (n = 12) 5.6% (n = 28) 3.0% (n = 15) 1.0% (n = 5) 23.5% (119) 2.0% (n = 10) 0.2% (n = 1) |
65.0% (n = 39) 5.0% (n = 3) 10.0% (n = 6) 8.4% (n = 5) 1.7% (n = 1) 1.7% (n = 1) 6.7% (n = 4) 1.7% (n = 1) – |
| Ureteral stent | Before After |
15.9% (n = 90) 34.4% (n = 195) |
15.8% (n = 80) 34.3% (n = 174) |
16.7% (n = 10) 35.0% (n = 21) |
| SFR | 90.7 (n = 515) | 90.3% (n = 458) | 88.3% (n = 53) |
SFR – stone-free rate
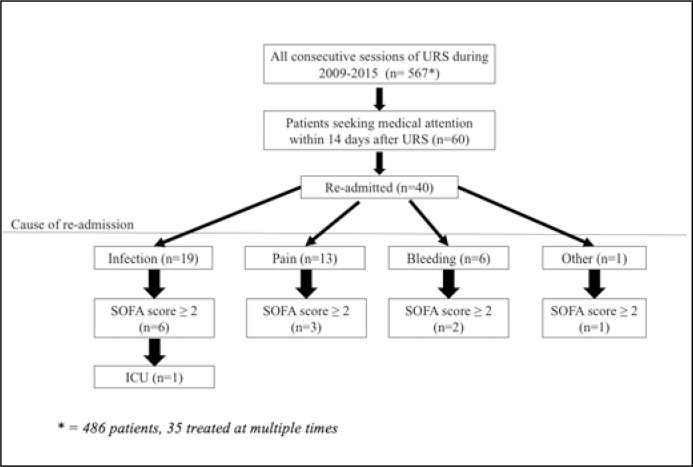
Figure 1.
Flowchart of re-admitted patients, divided into cause of re-admission. The distribution of patients with sequential sepsis-related organ failure assessment (SOFA) score ≥ is also shown.
SFR's determined by preoperative stone location are presented in Table 3a.
Table 3a.
Preoperative stone location in the upper urinary tract and residual stone size
| Distal third of ureter (n = 331) | Middle third of ureter (n = 97) | Proximal third of ureter (n = 75) | Renal pelvis (n = 58) | |
|---|---|---|---|---|
| SFR | 95.2% (n = 315) | 92.8% (n = 90) | 84.0% (n = 63) | 69.0% (n = 40) |
| No residual stones | 66.2% (n = 219) | 62.9% (n = 61) | 50.7% (n = 38) | 34.5% (n = 20) |
| ≤2 mm | 2.7% (n = 9) | 4.2% (n = 4) | 5.3% (n = 4) | 5.1% (n = 3) |
| >2 ≤4 mm | 0.9% (n = 3) | 3.1% (n = 3) | 6.7% (n = 5) | 10.4% (n = 6) |
| >4 ≤6 mm | 2.4% (n = 8) | 5.2% (n = 5) | 8.0% (n = 6) | 19.0% (n = 11) |
| >6 ≤10 mm | 2.1% (n = 7) | 1.0% (n = 1) | 6.7% (n = 5) | 5.1% (n = 3) |
| >10 mm | – | 1.0% (n = 1) | 1.3% (n = 1) | 6.8% (n = 4) |
| No follow-up | 23.6% (n = 78) | 20.6% (n = 20) | 18.7% (n = 14) | 17.2% (n = 10) |
| Patient no-show | 1.8% (n = 6) | 2.1% (n = 2) | 2.7 % (n = 2) | 1.7% (n = 1) |
| No longer in Scania | 0.3% (n = 1) | – | – | – |
SFR – stone-free rate
SFR provided preoperative stone size showed 100 % success rate in stones ≤4 mm (n = 112). SFR for stones >4≤6 mm 96.2 % (176/183), for stones >6≤10 mm 84.6 % (193/228), and for >10 mm 68.2 % (30/44) (Table 3a and 3b).
Table 3b.
Preoperative stone size and stone-free rate
| Preoperativestone size | ≤2 mm (n = 10) | >2≤4 mm (n = 102) | >4≤6 mm (n = 183) | >6≤10 mm (n = 228) | >10 mm (n = 44) |
|---|---|---|---|---|---|
| SFR | 100% (n = 10) | 100% (n = 102) | 96.2% (n = 176) | 84.6% (n = 193) | 68.2% (n = 30) |
SFR – stone-free rate
Of the 20 patients re-treated for the same stone within 6 months, 4 patients (20.0%) had a residual stone size of ≤4 mm (Table 3c). This equaled 10.5 % (4/38) out of all patients with residual stones, considered stone-free.
Table 3c.
Size of residual stones needed to be re-treated within 6 months
| Re-treated patients within 6 months (n = 20) | |
|---|---|
| Size of residual stone ≤2 mm >2 ≤4 mm >4 ≤6 mm >6 ≤10 mm >10 mm |
10.0% (n = 2) 10.0% (n = 2) 30.0% (n = 6) 35.0% (n = 7) 15.0% (n = 3) |
Operating with the on-call OR (operating room) nursing staff or the evening or night staff, we found a SFR of 97.6% (1/41) compared to the SFR of 89% (52/474) during normal working hours; when compensating for age/gender we found no significant difference.
A positive urine culture was found in 15.9% of the patients (90/567). The most common pathogen was Escherichia coli (32/90, 35.6%) and the second most common was Enterococcus faecalis (17/90, 18.9%). A total of 79 patients (13.9%) received preoperative antibiotic treatment, 341 patients (60.1%) received perioperative antibiotics, and 103 patients (18.2 %) received postoperative antibiotics treatment. Of the perioperative antibiotics, aminoglycoside was the most used type (235/341, 69.0%) (Table 4).
Table 4.
Preoperative urine culture and antibiotics treatment
| All patients (n = 567) | Patients not seeking medical care within 14 days (n = 507) | Patients seeking medical care within 14 days (n = 60) | |
|---|---|---|---|
| Positive urine culture E. Coli Enterococcus faecalis Other bacteria |
15.9% (n = 90) 35.6% (n = 32/90) 18.9% (n = 17/90) 45.5% (n = 41/90) |
14.0% (n = 71) 39.4% (n = 28/71) 21.1% (n = 15/71) 39.4% (n = 28/71) |
31.7% (n = 19) 21.1% (n = 4/19) 10.5% (n = 2/19) 68.4% (n = 13/19) |
| Preoperative antibiotics Ciprofloxacin TMP/SMX Other antibiotics |
13.9% (n = 79) 25.3% (n = 20/79) 19.0% (n = 15/79) 55.7% (n = 44/79) |
13.2% (n = 67) 28.4% (n = 19/67) 19.4% (n = 13/67) 52.2% (n = 35/67) |
20.0% (n = 12) 8.3% (n = 1/12) 16.7% (n = 2/12) 75.0% (n = 9/12) |
| Perioperative antibiotics Aminoglycoside Other antibiotics |
60.1% (n = 341) 69.0% (n = 235/341) 31.0% (n = 106/341) |
59.4% (n = 301) 67.4% (n = 203/301) 32.6% (n = 98/301) |
66.7% (n = 40) 80.0% (n = 32/40) 20.0% (n = 8/40) |
| Postoperative antibiotics Ciprofloxacin TMP/SMX Other antibiotics |
18.2% (n = 103) 36.9% (n = 38/103) 34.0% (n = 35/103) 29.1% (n = 30/103) |
17.8% (n = 90) 38.9% (n = 35/90) 34.4% (n = 31/90) 26.7% (n = 24/90) |
21.7% (n = 13) 23.1% (n = 3/13) 30.8% (n = 4/13) 46.1% (n = 6/13) |
| Days of antibiotic treatment, Mean (range) | 2.3 (0–30) | 2.2 (0–30) | 2.8 (0–25) |
TMP/SMX – trimethoprim/sulfamethoxazole; E. Coli – Escherichia coli
Data regarding patients seeking medical attention within 14 days are presented in Table 5. 60 patients (10.6%) sought medical attention within 14 days, of these 40 (7.1%) were readmitted. The causes of readmission were infection (19/60, 31.7%), pain (13/60, 21.7%), bleeding (6/60, 10.0%), and other causes (2/60, 3.3%).
Table 5.
Characteristics of patients with complications
| Patients seeking medical care within 14 days (n = 60) | Patients seeking medical care within 14 days, but not re-admitted (n = 20) | Patients seeking medical care within 14 days, re-admitted (n = 40) | |
|---|---|---|---|
| Age, Mean (±SD) | 56.7 (18.1) | 59.4 (17.6) | 55.4 (18.3) |
| Sex M:F Ratio | 2:1 | 4:1 | 1.5:1 |
| Cause of admission Infection Bleeding Pain Other |
33.3% (n = 20) 13.3% (n = 8) 40.0% (n = 24) 13.3% (n = 8) |
5.0% (n = 1) 10.0% (n = 2) 55.0% (n = 11) 30.0% (n = 6) |
47.5% (n = 19) 15.0% (n = 6) 32.5% (n = 13) 5.0% (n = 2) |
| Days until re-admission, Mean (range) Days of re-hospitalisation, Mean (range) |
4.3 (0–14) 3.1 (0–20) |
3.6 (0–14) – |
4.8 (0–14) 4.6 (1–20) |
| Blood culture drawn | 40.0% (n = 24) | – | 60.0% (n = 24) |
| Urine culture drawn | 63.3% (n = 38) | 40.0% (n = 8) | 75.0% (n = 30) |
| Positive culture Escherichia coli Enterococcus faecalis Other bacteria |
21.7% (n = 13) 38.5% (n = 5/13) 7.7 % (n = 1/13) 53.8% (n = 7/13) |
10.0% (n = 2) 100% (n = 2/2) – – |
27.5% (n = 11) 27.3% (n = 3/11) 9.1% (n = 1/11) 63.6% (n = 7/11) |
| Antibiotics Ciprofloxacin TMP/SMX Aminoglycoside Otherantibiotics |
60.0% (n = 36) 38.9% (n = 14/36) 13.9% (n = 5/26) 30.6% (n = 11/36) 16.7% (n = 6/36) |
30.0% (n = 6) 33.3% (n = 2/6) 16.7% (n = 1/6) 33.3% (n = 2/6) 16.7% (n = 1/6) |
75.0% (n = 30) 40.0% (n = 12/30) 13.3% (n = 4/30) 30.0% (n = 9/30) 16.7% (n = 5/30) |
| ICU | 1.7% (n = 1) | – | 2.5% (n = 1) |
| SOFA score ≥2 | 20% (n = 12) | 5.0% (n = 1) | 27.5% (n = 11) |
TMP/SMX – trimethoprim/sulfamethoxazole
Of the patients admitted, 12 (20.0%) had a SOFA (Sequential sepsis-related organ failure assessment) score ≥2 and one patient was admitted to the ICU [16].
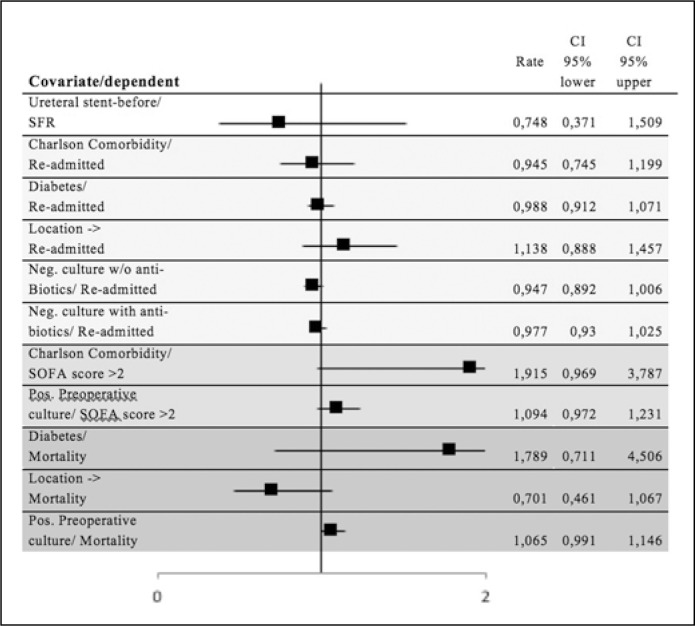
Logistic regression model with SFR, re-admission, SOFA score >2, or mortality as a dependent factor, without statistical significance, are presented in Figure 2 as a forest plot. The univariate logistic regression analyses showing statistical significance are presented in Table 6. Parameters obtaining p ≤0.05 were further investigated in multivariate logistical regression, adding the predefined confounding variables of gender and age. SFR is significantly affected by stone location in the ureter (p <0.001, OR 0.515, CI 95% 0.389–0.682), preoperative stone size (p <0.001, OR 0.728, CI 95% 0.654–0.810), and postoperative ureteral stents (p = 0.009, OR 0.418, CI 95% 0.217–0.804). Using readmission as a dependent, only the Clavien-Dindo classification (p <0.001, OR 8.014, CI 95% 5.220–12.304) was confirmed to be significant. Mortality was not increased if the patient was readmitted within 14 days.
Figure 2.
Forest plot of univariate logistic regression analyses without significant P-value.
Table 6.
Univariate logistical regression analyses showing statistical significance
| P-value | OR | CI 95% | |
|---|---|---|---|
| On call personal to SFR | 0.141 | 0.222 | 0.606–33.378 |
| Not normal working hours to SFR | 0.141 | 0.222 | 0.606–33.378 |
| Stone location in ureter to SFR | <0.001 | 0.482 | 0.376–0.616 |
| Preoperative stone size to SFR | <0.001 | 0.885 | 0.852–0.920 |
| Postoperative ureteral stent to SFR | 0.002 | 0.413 | 0.237–0.721 |
| Clavien-Dindo to re-admission | <0.001 | 7.996 | 5.318–12.022 |
| Positive preoperative urine culture to readmission | 0.001 | 1.100 | 1.041–1.161 |
| Clavien-Dindo to mortality | 0.022 | 1.557 | 1.065–2.278 |
| Charlson Comorbidity index to mortality | <0.001 | 1.869 | 1.506–2.320 |
| SOFA score ≥2 to mortality | 0.023 | 15.667 | 1.460–168.074 |
| Clavien-Dindo to SOFA score ≥2 | 0.003 | 5.426 | 1.788–16.466 |
| Age to SOFA score ≥2 | 0.014 | 1.062 | 1.012–1.115 |
SFR – stone-free rate; SOFA – sequential sepsis-related organ failure assessment
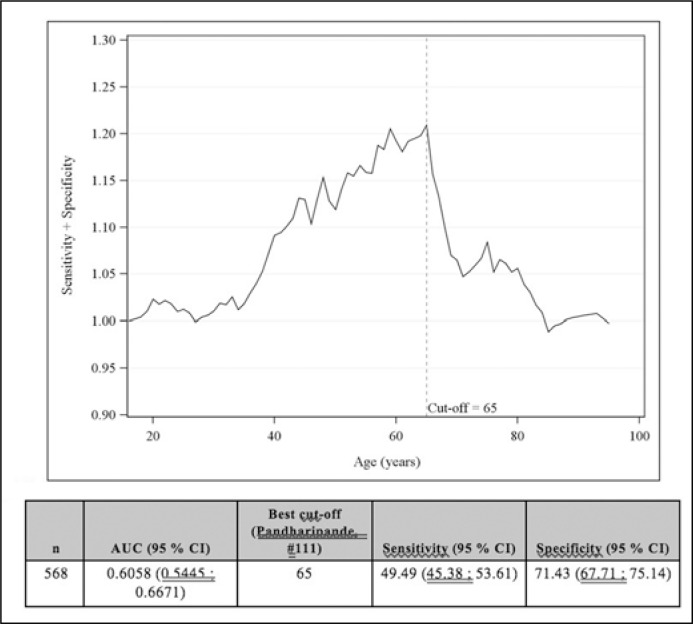
The risk of surgical complications in regard to the time of day (0800–1700 vs. other), ordinary vs. on call personal, acute vs elective surgery and flexible vs semi-rigid ureteroscope, no significant differences were found (Table 7). Age, however, was significant in all groups and the receiver operating characteristic (ROC) curve analysis was performed [16]. Most accurate cut-off point of age, regarding age and the risk of complications, was 65 years (area under curve (AUC) 0.6) (Figure 3).
Table 7.
Logistical regression analyses regarding hour of surgery, normal vs. call-time surgery, acute vs. elective surgery and flexible vs. semi-rigid ureteroscope and the risk of complications
| Model | Variable | OR (95% CI) | p-value |
|---|---|---|---|
| Time of day | 08.00–17.00 vs. other time of day | 0.5754 (0.2186; 1.5145) | 0.2630 |
| Age | 1.0230 (1.0085; 1.0377) | 0.0018 | |
| Men vs. women | 1.0781 (0.6562; 1.7713) | 0.7664 | |
| Night / Call | Night / Call vs. daytime | 0.5380 (0.2583; 1.1204) | 0.0977 |
| Age | 1.0224 (1.0080; 1.0371) | 0.0023 | |
| Men vs. women | 1.0870 (0.6612; 1.7868) | 0.7423 | |
| Acute | Acute vs. elective | 0.7539 (0.4400; 1.2919) | 0.3040 |
| Age | 1.0218 (1.0073; 1.0365) | 0.0032 | |
| Men vs. women | 1.0700 (0.6510; 1.7588) | 0.7895 | |
| Flexible | Flexible vs. standard | 1.6526 (0.9386; 2.9095) | 0.0818 |
| Age | 1.0224 (1.0078; 1.0371) | 0.0025 | |
| Men vs. women | 1.1227 (0.6815; 1.8494) | 0.6496 |
Figure 3.
Recevier operating characteristic (ROC) curve describing sensitivity + specificity vs. age for risk of complications and ROC curve.
Charlson Comorbidity index, preoperative stone size, and stone location in the ureter to Clavien-Dindo showed no statistical significant association with postoperative risk for complications (p = 0.227, p = 0.274, p = 0.720, respectively) (Figure 2). A univariate logistical regression analysis was made with diabetes [17] to Clavien-Dindo (dependent) showing no statistical significance (p = 0.717).
DISCUSSION
Regarding the definition of surgical success, there are different ways to report this; however, the older SFR meaning ‘Stone Free Rate’ used when the residual fragments are <4 mm and hence corresponds well to the newer ‘Successful treatment’ having the same definition. The SFR of 90.1% found in this study is comparable to similar studies [6]. Georgescu et al. showed similar results (SFR 90.9%) [18]. Somani et al. reported a SFR of 85.6% in a multi-center worldwide cohort [19]. Ghani & Wolf [20] reviewed multiple studies in order to determine a SFR for URS. Stone-free (no residual stones) was found in 51%, with a cut- off of ≤2 mm, a SFR of 77% was found, and with a cut-off of ≤4 mm a total SFR of 84.5% was found.
Compared to our data (<2 mm/86.9% and <4 mm/83.4%, respectively), the success rate seems to be slightly higher at our center. In a worldwide study including 9681 patients operated with URS, SFR in different parts of the ureter was: 94.2% in the distal third part of the ureter, 89.4% in the middle third part of the ureter, and 84.5% in the proximal third part of the ureter [6]. This is equivalent to our results. As expected, our statistical analysis could confirm that the more distal the stone was, the more probable was a successful stone removal (p <0.001).
The term “clinically insignificant residual stones” remains debated [21]. In an early, prospective study following 160 patients with remaining stone fragments of ≤4 mm after receiving ESWL treatment, about 40% had symptomatic episodes and required intervention [22]. Rebuck et al. [23] evaluated the natural course of post-URS remaining fragments, using a CT-scan to follow fragments ≤4 mm, and showed that 13% of patients with residual fragments ≤4 mm needed to be re-treated. In our study, 10.5% (4/38) of patients with residual fragments ≤4 mm underwent re-URS within 6 months. Treating residual stones ≤4 mm is debatable. There is a significant chance of spontaneously passage, 79.6% passes within 20 weeks according to Jendeberg et al. [24] . If this corresponds to residuals after surgery in the not known. Their data showed the rate of spontaneous passage were 98% in stones >3 mm, 81% in stones 4 mm, 65% in stones 5 mm, 33% in stones 6 mm, and 9% in stones ≥6.5 mm. Our data could show that a significantly higher SFR was reached among smaller stones (p <0.001).
Preoperative ureteral stenting may affect the success rate of the URS. A meta-analysis of nine retrospective studies with a total of 11,239 patients showed a higher SFR if the patient had received a preoperative ureteral stent [25], confirmed in other studies [26]. If the positive effect on SFR by preoperative stenting is due to stone location / stone burden or by stenting itself, remains unclear [9]. Our data show no significant effect of preoperative stenting on SFR (p = 0.417) which also Nabi et al. [10] found. Regarding postoperative stenting we found a negative correlation to SFR (p = 0.002) (independent of age, gender, stone size, and stone location). This might be explained by local clinical practice, stents were used for the most complicated cases having longer operating time.
Correlation between the positive urine culture prior to URS to positive urine culture at readmission showed no significance (p = 0.211). All patients with positive urine culture prior to the treatment received antibiotics pre-, peri-, and/or postoperatively. Our data showed a tendency (p = 0.070) that patients with negative urine culture prior to URS not receiving antibiotics had a higher incidence of positive urine culture at readmission maybe indicating infection as a result of surgery or the effect of bacteria in/on the stone. As expected, a third of the urine cultures show growth of Escherichia coli (35.6%). The increasing resistance in Escherichia coli to antibiotics is alarming [27]. Our study shows a use of ciprofloxacin in approximately 30% of patients, and TMP/SMX in almost 25%. Regardless of its accordance with the EAU - Guidelines on Urolithiasis at the time, this might contribute to increasing resistance in the future.
It is noteworthy that of patients being re-admitted, 11 had positive urine and/or blood culture, and all SOFA score ≥2. URS treatment itself may entail a risk of impacting creatinine levels [28], maybe giving all our patients a SOFA score of 1. Study limitations with retrospective data, trying to classify the qSOFA/SOFA score requires lots of work and patients rarely are classified according to this algorithm which could lead to inaccuracy.
Perez et al. [6] showed an intraoperative complication rate of 3.8–7.7%, and a postoperatively complication rate of 2.4–4.6% depending on stone location, including bleeding, infection, pain, and others. This can be compared to a complication rate of around 6% in ESWL, and approximately 10% in PCNL [8]. Our data show a re-admission rate/complication rate of 7.1/10.7%.
We show no increased risk for postoperative complications in patients with comorbidities classified with the Charlson Comorbidity index (p = 0.720), nor in patients with diabetes (p = 0.717). According to our findings there were no correlation between an increased risk of complications and stone location (p = 0.227) or stone size (0.274). This study does not show an increased risk for complications when surgery is performed with on-call personal or if it is performed acute and the time (day/night) does not seem to matter. The possibility of selection bias regarding this group and a tendency to only do uncomplicated stones outside normal working hours could be one explanation. Another could be that on-call surgery was performed only by senior consultants. Since the numbers are small, larger studies are needed. Studies have indicated that the risk of complications does not increase with age [29]. In our study the risk of complications seems to increase with age and the ROC curve analysis indicates that a possible cut off at 65 years might be recommended.
As in other retrospective cohort studies, we have had to rely on the documenting doctor/nurse for all retrospective data. Some of our findings are based on small numbers and errors in documentation might lead to shifts in our data analyses.
CONCLUSIONS
According to our findings performing ureteroscopy outside ‘office hours’ does not increase the complication rate. Outcome of URS treatment in the north-western part of Scania County, Sweden, seems to be in parity with previous studies.
We conclude that there are a few complications to modern URS treatment and that stone-free rate (SFR) is high. URS seems to be a safe and effective method for treating ureteral stones regardless of location, but should preferably be used for stones in the lower part of the ureter. In this study, we found no significant risk factors for complications. E. coli is the most common bacteria in preoperative cultures. The risk of complications increases with age and for patients older than 65 years another modality than URS could be considered.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Acknowledgments
ACKNOWLEDGMENTS
We like to thank the staff at the Department of Urology, Helsingborg and Ängelholms hospital for helping with patient registration.
Appendix 1
Updated Charlson Comorbidity Index (Quan, 2011 #71). Used to predict long-term mortality among patients with chronic disease(s). The updated score of the Index was used, validated to modern treatment of these disease(s).
| Variable | Updated Charlson Score |
|---|---|
| Charlson comorbidity | |
| Myocardial infarction | 0 |
| Congestive heart failure | 2 |
| Peripheral vascular disease | 0 |
| Cerebrovascular disease | 0 |
| Dementia | 2 |
| Chronic pulmonary disease | 1 |
| Rheumatologic disease | 1 |
| Peptic ulcer disease | 0 |
| Mild liver disease | 2 |
| Diabetes without chronic complications | 0 |
| Diabetes with chronic complications | 1 |
| Hemiplegia or paraplegia | 2 |
| Renal disease | 1 |
| Any malignancy, including leukaemia /lymphoma | 2 |
| Moderate or severe liver disease | 4 |
| Metastatic solid tumour | 6 |
| AIDS/HIV | 4 |
| Maximum comorbidity score | 24 |
AIDS – acquired immunodeficiency syndrome; HIV – human immunodeficiency virus
The following comorbid conditions were mutually exclusive: diabetes with chronic complications and diabetes without chronic complications; mild liver disease and moderate or severe liver disease; and any malignancy and metastatic solid tumour.
Appendix 2
The Clavien-Dindo Classification, used to classify surgical complications [40].
| Grade I | Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions. Allowed therapeutic regimens are: drugs as antiemetics, antipyretics, analgetics, diuretics and electrolytes and physiotherapy. This grade also includes wound infections opened at the bedside. |
| Grade II | Requiring pharmacological treatment with drugs other than such allowed for grade I complications. Blood transfusions and total parenteral nutrition are also included. |
| Grade III | Requiring surgical, endoscopic or radiological intervention. |
| Grade IV | Life-threatening complication (including CNS complications) requiring IC/ICU-management. |
| Grade V | Death of a patient. |
FUNDING
This work was supported by Gorthon foundation, Lions foundation, Percy Falk foundation and ALF Region Skåne.
References
References
- 1.Lyu J, Wu R. A brief history of recognition on urolithiasis before medieval period. Zhonghua Yi Shi Za Zhi. 2014;44:36–39. [PubMed] [Google Scholar]
- 2.Ljunghall S. Incidence and natural history of renal stone disease and its relationship to calcium metabolism. Eur Urol. 1978;4:424–430. doi: 10.1159/000474013. [DOI] [PubMed] [Google Scholar]
- 3.Ahlstrand C, Tiselius HG. Recurrences during a 10-year follow-up after first renal stone episode. Urol Res. 1990;18:397–399. doi: 10.1007/BF00297372. [DOI] [PubMed] [Google Scholar]
- 4.Trinchieri A. Epidemiology of urolithiasis: an update. Clin Cases Miner Bone Metab. 2008;5:101–106. [PMC free article] [PubMed] [Google Scholar]
- 5.Hesse A, Brandle E, Wilbert D, Köhrmann KU, Alken P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol. 2003;44:709–713. doi: 10.1016/s0302-2838(03)00415-9. [DOI] [PubMed] [Google Scholar]
- 6.Perez Castro E, Osther PJ, Jinga V, et al. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol. 2014;66:102–109. doi: 10.1016/j.eururo.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Drake T, Grivas N, Dabestani S, et al. What are the Benefits and Harms of Ureteroscopy Compared with Shock-wave Lithotripsy in the Treatment of Upper Ureteral Stones? A Systematic Review. Eur Urol. 2017;72:772–786. doi: 10.1016/j.eururo.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Turk C, Petrik A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 9.Rubenstein RA, Zhao LC, Loeb S, Shore DM, Nadler RB. Prestenting improves ureteroscopic stone-free rates. J Endourol. 2007;21:1277–1280. doi: 10.1089/end.2007.9888. [DOI] [PubMed] [Google Scholar]
- 10.Nabi G, Cook J, N'Dow J, McClinton S. Outcomes of stenting after uncomplicated ureteroscopy: systematic review and meta-analysis. BMJ. 2007;334:572. doi: 10.1136/bmj.39119.595081.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lingeman JE, Newman D, Mertz JH, et al. Extracorporeal shock wave lithotripsy: the Methodist Hospital of Indiana experience. J Urol. 1986;135:1134–1137. doi: 10.1016/s0022-5347(17)46016-2. [DOI] [PubMed] [Google Scholar]
- 12.Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014;28:1–13. doi: 10.1016/j.idc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Preminger GM, Tiselius HG, Assimos DG, et al. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007;52:1610–1631. doi: 10.1016/j.eururo.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenschein U, Budde-Schwartzman B. Ultrasound coronary angioplasty: state of the art and new clinical aspects. Herz. 1997;22:308–317. doi: 10.1007/BF03044281. [DOI] [PubMed] [Google Scholar]
- 17.Bai J, Lin J, Zhuang H, Guo D, Yang X, Duan M. Changes in plasma cholesterol level and risk factors of death in patients with sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2016;28:164–168. doi: 10.3760/cma.j.issn.2095-4352.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Georgescu D, Multescu R, Geavlete B, Geavlete P. Intraoperative complications after 8150 semirigid ureteroscopies for ureteral lithiasis: risk analysis and management. Chirurgia (Bucur) 2014;109:369–374. [PubMed] [Google Scholar]
- 19.Somani BK, Giusti G, Sun Y, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the Clinical Research Office of Endourological Society URS Global study. World J Urol. 2017;35:675–681. doi: 10.1007/s00345-016-1909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghani KR, Wolf JS., Jr What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Rev Urol. 2015;12:363. doi: 10.1038/nrurol.2015.133. [DOI] [PubMed] [Google Scholar]
- 21.Deters LA, Jumper CM, Steinberg PL, Pais VM., Jr Evaluating the definition of ‘stone free status’ in contemporary urologic literature. Clin Nephrol. 2011;76:354–357. doi: 10.5414/cn106787. [DOI] [PubMed] [Google Scholar]
- 22.Streem SB, Yost A, Mascha E. Clinical implications of clinically insignificant store fragments after extracorporeal shock wave lithotripsy. J Urol. 1996;155:1186–1190. [PubMed] [Google Scholar]
- 23.Rebuck DA, Macejko A, Bhalani V, Ramos P, Nadler RB. The natural history of renal stone fragments following ureteroscopy. Urology. 2011;77:564–568. doi: 10.1016/j.urology.2010.06.056. [DOI] [PubMed] [Google Scholar]
- 24.Jendeberg J, Geijer H, Alshamari M, Cierzniak B, Lidén M. Size matters: The width and location of a ureteral stone accurately predict the chance of spontaneous passage. Eur Radiol. 2017;27:4775–4785. doi: 10.1007/s00330-017-4852-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang Y, Tang Y, Bai Y, Wang X, Feng D, Han P. Preoperative double-J stent placement can improve the stone-free rate for patients undergoing ureteroscopic lithotripsy: a systematic review and meta-analysis. Urolithiasis. 2018;46:493–499. doi: 10.1007/s00240-017-1012-z. [DOI] [PubMed] [Google Scholar]
- 26.Assimos D, Crisci A, Culkin D, et al. Preoperative JJ stent placement in ureteric and renal stone treatment: results from the Clinical Research Office of Endourological Society (CROES) ureteroscopy (URS) Global Study. BJU Int. 2016;117:648–654. doi: 10.1111/bju.13250. [DOI] [PubMed] [Google Scholar]
- 27.Folkhälsomyndigheten Escherichia coli. Resistensläge [Internet] 2017. [cited 2017 2017-12-05]. Available from: https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaser-och-visualisering/sjukdomsstatistik/escherichia-coli/?t=county.
- 28.Benli E, Ayyildiz SN, Cirrik S, Noyan T, Ayyildiz A, Cirakoglu A. Early term effect of ureterorenoscopy (URS) on the Kidney: research measuring NGAL, KIM-1, FABP and CYS C levels in urine. Int Braz J Urol. 2017;43:887–895. doi: 10.1590/S1677-5538.IBJU.2016.0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daels FP, Gaizauskas A, Rioja J, et al. Age-related prevalence of diabetes mellitus, cardiovascular disease and anticoagulation therapy use in a urolithiasis population and their effect on outcomes: the Clinical Research Office of the Endourological Society Ureteroscopy Global Study. World J Urol. 2015;33:859–864. doi: 10.1007/s00345-014-1382-6. [DOI] [PubMed] [Google Scholar]