Abstract
Introduction
The aim of this article was to report our experience with laparoscopic and retroperitoneoscopic nephrectomy in patients with xanthogranulomatous (XPG) pyelonephritis.
Material and methods
Between November 2002 and September 2010, 27 patients, with a mean age of 61.1 years (range 43–85), underwent laparoscopic nephrectomy for a unilateral nonfunctioning kidney, because of xanthogranulomatous pyelonephritis. Patient's data was collected retrospectively and included patient age, gender, intraoperative conversion rate, operative time, estimated blood loss, length of hospital stay, perioperative transfusion rate, renal function pre- and postoperatively and postoperative complications.
Results
Laparoscopic nephrectomy was successful in 26 patients. It was transperitoneal in 15 patients, retroperitoneal in 11 patients and in one patient the operation was initiated as retroperitoneal and converted to transperitoneal. One conversion to open surgery was needed. The mean operative time was 193.6 minutes (range 123–340). The mean estimated blood loss was 223.5 ml (range 30–1000). The mean hospital stay was 4.8 days (range 3–12). The transfusion rate was 29.6%. Serum creatinine was 1.3 mg/dl the day before and the day after the operation. Major complications occurred in patients (11.1%).
Conclusions
Laparoscopic nephrectomy should be considered as an initial approach for XGP. The indications for laparoscopic nephrectomy should be extended to these patients.
Keywords: contraindications, laparoscopic nephrectomy, pyelonephritis, renal surgery, xanthogranulomatous pyelonephritis
INTRODUCTION
Since the original report of a successful laparoscopic nephrectomy by Clayman et al. in 1991, laparoscopic nephrectomy has become an alternative to traditional open surgery [1]. In 1993 Gaur and colleagues reported their first retroperitoneoscopic nephrectomy [2]. Laparoscopy is gradually replacing the traditional open approach to remove benign xanthogranulomatous pyelonephritis (XGP) [3]. XGP, a rare form of chronic renal infection, is usually associated with nephrolithiasis, obstructive uropathy, or ongoing urinary tract infection. XGP is a severe, chronic renal-parenchymal infection. Because of the renal and perirenal inflammatory changes that commonly accompany XGP, the laparoscopic approach is difficult. The treatment of choice has been open nephrectomy, which is challenging in itself, given the extent of the disease and and the quite common involvement of the renal hilum and the contiguous structures [4–7].
Laparoscopic approach has been usually contraindicated and not justified in XGP [7]; however, improvements in the skill, instruments, and technique of the laparoscopist have expanded the indications to include XGP in some cases [3, 8, 9]. Herein, we report our experience with laparoscopic and retroperitoneoscopic nephrectomy for XGP.
To our knowledge, this is the largest series to be reported.
MATERIAL AND METHODS
Between November 2002 and September 2010, 27 pa- tients (22 women and 5 men), with a mean age of 61.1 years (range 43–85), underwent laparoscopic nephrectomy for a unilateral nonfunctioning kidney, because of XGP. Patient's data was collected retrospectively. There were 25 patients with nephrolithiasis and recurrent urinary tract infections, while there were two patients with a painful renal mass.
Under general anesthesia, the patient was placed on the operative table in a classic dorsal lithotomy position. The kidney bridge was elevated underneath the last ribs to increase the space between the costal margin and the iliac crest to create a larger retroperitoneal working space. The first incision, 1.5 cm long, was performed under the tip of the 12th rib into the retroperitoneum. Through this incision, the retroperitoneal space was dissected digitally and the peritoneum pushed anteriorly. Creation of the retroperitoneal space was completed by oblong balloon dissection. After insertion of a 10 mm trocar through the incision, a second 10 mm trocar was inserted along the posterior axillary line above the iliac crest. A third and fourth 5 mm trocars were inserted along the anterior axillary line. The camera port was the initial port. The transperitoneal laparoscopic nephrectomy was performed according to the technique described by McDougal and Clayman [10]. We mainly used the 10 mm Endo-Ligasure and sometimes the Harmonic Scalpel for the dissection. The renal vessels were initially dissected, then clipped and divided. Our method was to dissect outside the Gerota fascia. The ureter was dissected, clipped, and divided at a determined level. After the kidney was detached from all its adhesions, it was placed in an Endobag and removed through the first or the second port incision. All kidneys were removed intact by extending the incision 5–6 cm.
RESULTS
Laparoscopic nephrectomy was successful in 26 patients. The results and the complications are shown in Table 1 and Table 2. A transperitoneal approach was adapted in 15 patients, retroperitoneal in 11 patients, and in one patient the operation was initiated as retroperitoneal and converted to transperitoneal. Conversion to open surgery was needed in one patient. The mean operative time was 193.6 minutes (range 123–240). The mean estimated blood loss was 223.5 ml (range 30–1000). The mean hospital stay was 4.8 days (range 3–12). Eight patients required transfusion of a single or two units of packed red blood cells, seven of them during the operation and the last some days later due to port site hematoma. Serum creatinine was 1.3 mg/dl the day before and the day after the operation (Table 3). No intraoperative or postoperative gastrointestinal complications developed. Three patients presented with major complications, the first with sepsis, the second with pulmonary edema and the third with retroperitoneal abscess which was drained. Three patients presented with minor complications, port site hernia in one patient, port site hematoma in the second patient, and wound infection in the third patient. In 25 patients a drain was left for 2.7 days (range 2–6).
Table 1.
Results of transperitoneal (TP) and retroperitoneal (RP) laparoscopic nephrectomy for XGP¥
| Range | TP/RP | ||
|---|---|---|---|
| Patients (n) | 27 | ||
| Men/women (n) | 5/22 | – | |
| Mean age (yr) | 61.1 | 43–85 | |
| Retroperitoneal/ transperitoneal (n) | 11/15 | – | |
| Retroperitoneal converted to transperitoneal (n) | 1 | – | |
| Mean operative time (min) | 193.6 | 123–340 | |
| Mean blood loss (ml) | 223.5 | 30–1000 | |
| Mean hospital stay (days) | 4.8 | 3–12 | |
| Conversion to open (%) | 3.7 | – | |
| Wound infection (%) | 3.7 | – | TP |
| Port site hematoma (%) | 3.7 | – | TP |
| Port site incisional hernia (%) | 3.7 | – | RP |
| Sepsis (%) | 3.7 | – | RP |
| Pulmonary edema (%) | 3.7 | – | RP |
| Retroperitoneal abscess (%) | 3.7 | – | TP |
XGP¥ – xanthogranulomatous pyelonephritis
Table 2.
Reported hospital stay (days), blood loss (ml), operative time (min), and conversion rates from laparoscopic to open nephrectomy (%)
| Series | No. | Hospital stay (days) | BL$ (ml) | OT# (min) | CR& (%) | Comments |
|---|---|---|---|---|---|---|
| Khaira et al. [3] | 3 | 4.7 | 1117 | 279 | 33.3 | XGP¥ |
| Bercowsky et al. [7] | 5 | 6 | 260 | 360 | 20 | XGP¥ |
| Hemal et al. [16] | 185 | 3 | 133 | 100 | 9.7 | Benign diseases |
| Rassweiler et al. [19] | 9 | – | – | – | 89 | XGP¥, Renal |
| Tuberculosis | ||||||
| Post traumatic | ||||||
| Renal atrophy | ||||||
| Vanderbrink et al. [20] | 6 | 4.8 | 775 | 301 | 17 | XGP¥ |
| Campanario et al. [21] | 17 | 4.4 | – | 198 | 12.5 | XGP¥ |
| This study | 27 | 4.8 | 223.5 | 193.6 | 3.7 | XGP¥ |
BL$ – blood loss; OT# – operative time; CR& – conversion rate; XGP¥ – xanthogranulomatous pyelonephritis
Table 3.
Serum creatinine and hemoglobin
| No | Pre-op£ | Post-op£ |
|---|---|---|
| 27 | ||
| Hemoglobin g/dl | 13 | 12.5 |
| Creatinine mg/dl | 1.3 | 1.3 |
op£ – operation
DISCUSSION
Since the original report of a successful laparoscopic nephrectomy by Clayman et al. in 1991 [1], laparoscopic nephrectomy has become a routine procedure at specialized centers, with the advantages of less postoperative pain, minimal scars, rapid recovery, and short convalescence. However, there are some technical concerns regarding laparoscopic nephrectomy and its use during nephrectomy for XGP that have not been widely reported [7, 8, 11]. Bercowsky et al. demonstrated that the benefits of laparoscopic nephrectomy do not extend to patients with XGP, and that conventional open surgery is quicker with fewer complications and results in a similar use of analgesics, hospital stay and recovery time [7]. However, surgical situations that only some years ago would have been regarded as contraindications are now accepted as proper indications for the laparoscopic approach because of the rapid improvement in laparoscopic instruments and surgical skill. Nowadays laparoscopic, live donor nephrectomy, which was initially the subject of much debate, has gradually gained wide acceptance because of its minimally invasive nature and acceptable results [12, 13, 14].
Gupta et al. reported their first case with tubercular pyelonephritis in which laparoscopic nephrectomy was attempted and subsequently the procedure was converted to open nephrectomy. Their conclusion was that tuberculous pyelonephritic kidney is a relative contraindication for laparoscopic nephrectomy [15]. Four years later Hemal and Gupta reported on their 185 cases of retroperitoneoscopic nephrectomy and nephroureterectomy for benign nonfunctioning kidneys with various modified techniques for differing etiologies. They concluded that retroperitoneoscopic nephrectomy and nephroureterectomy can be performed safely and successfully with obvious advantages for benign nonfunctioning kidneys regardless of the etiology or pathogenesis including tubercular pyelonephritis [16]. Lee et al. summarized the results of 31 consecutive laparoscopic nephrectomies for renal tuberculosis and compared them with 45 laparoscopic nephrectomies performed for other benign etiologies and concluded that laparoscopic nephrectomy for renal tuberculosis is a safe, effective, and less invasive treatment modality [17]. Hsia and Kapoor presented their technique of laparoscopic nephrectomy in a patient with previous urinary diversion. They demonstrated that in certain circumstances patients with urinary diversions could be offered laparoscopic nephrectomy [18]. Therefore XGP, previously treated by open surgery, can be today treated laparoscopically. In this study we report on 27 laparoscopic transperitoneal and retroperitoneal nephrectomies. The operation has been initiated and terminated laparoscopically with success in 26 patients. Conversion to open surgery was needed in one case only (Table 1). Rassweiler et al. reported an overall conversion rate of 10.3% due to bleeding, bowel injury, and difficult dissection. However, the conversion rate was 89% (8/9) in special situations including, 4 patients with renal tuberculosis, 2 with XGP, and one patient with posttraumatic renal atrophy (Table 2). They suggested that for patients with severe perinephritis due to renal tuberculosis, XGP, and posttraumatic atrophy an open conversion should be considered [19].
We cannot conclude that our patients have minimal fibrosis and therefore it is easier to proceed with the laparoscopic surgery, but we may have a higher threshold for open conversion and laparoscopic instruments such as Endo-Ligasure and Harmonic Scalpel, both widely used nowadays. We believe that high conversion rates which were reported elsewhere should not be a contraindication to the laparoscopic approach.
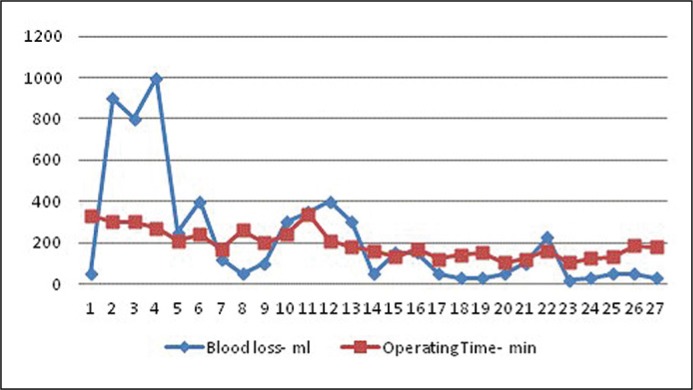
The mean operative time in our study is 193.6 minutes which is higher than that reported by Hemal et al. (100 minutes) [16], but shorter than that reported by Khaira et al. (279 min) and by Vanderbrink et al. (301 minutes) [3, 20]. However, we have noted that our learning curve is steep and the last cases were operated in a much shorter time than the first cases (Figure 1).
Figure 1.
Results of transperitoneal (TP) and retroperitoneal (RP) laparoscopic nephrectomy for xanthogranulomatous pyelonephritis (XGP)¥.
To minimize the hemorrhage during dissection it is essential to ligate all the renal vessels initially, however, because of the fibrosis and difficult dissection especially in the first patients the mean blood loss was 223.5 ml. Bercowsky et al. reported a mean blood loss of 260 ml, and Vanderbrink et al. 775 ml [7, 20]. The mean blood loss decreased steeply, the first cases made the major influence on our relatively high mean blood loss. We learned to decrease the bleeding from case to case using advanced devices (Figure 1). Our transfusion rate was 29.6% (8/27) which seems to be high, seven of them during the operation, because of bleeding more than 300 ml, the last patient required transfusion of a single unit of packed red blood cells some days later due to port site hematoma.
The mean hospital stay in our series was 4.8 days, which does not differ widely from other studies (Table 2). Serum creatinine was 1.3 mg/dl the day before and the day after the operation, so there was stable renal function (Table 3). Complications were noted in six patients (22.2%), while three major complications (11.1%) including sepsis, pulmonary edema, and retroperitoneal abscess needed a drainage. Two of the major complications were in patients who were operated in retroperitoneal approach and one in transperitoneal approach (Table 1). Three minor complications including hernia, port site hematoma, and wound infection (Table 1). There were no risk factors in patients who had complications comparing to the other patients in the group.
Campanario-Pérez R. et al. concluded that laparoscopic nephrectomy in XGP is a feasible surgical option although given the nature of XGP, it is associated with complications, which makes it a challenging surgical procedure. They clearly stated that advanced laparoscopic skills and experiences are needed in these cases. The dissemination of the disease is associated with the occurrence of more severe complications and conversion to open procedure [21]. Arvind et al. performed 14 (73.2%) successful laparoscopic nephrectomies in patients with XGP. They converted to open surgery in 5 patients because of non-progression of the procedure in 3 patients, and in 2 patients, conversion was performed on an emergency basis because of bleeding from hilar vessels [22].
As we mentioned in materials and methods, we dissected outside the Gerota fascia in order to reduce the difficulty of the procedure, a technique which was published recently by Ma et al. using laparoscopic nephrectomy in inflammatory renal diseases [23].
CONCLUSIONS
We suggest that laparoscopic nephrectomy should be considered as an initial approach for xanthogranulomatous pyelonephritis (XGP). The indications for laparoscopic nephrectomy should be extended to these patients.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Clayman RV, Kavoussi LR, Soper NJ, et al. Laparoscopic nephrectomy: initial case report. J Urol. 1991;146:278–282. doi: 10.1016/s0022-5347(17)37770-4. [DOI] [PubMed] [Google Scholar]
- 2.Gaur DD, Agarwal DK, Purohit KC. Retroperitoneal laparoscopic nephrectomy: initial case report. J Urol. 1993;149:103–105. doi: 10.1016/s0022-5347(17)36012-3. [DOI] [PubMed] [Google Scholar]
- 3.Khaira HS, Shah RB, Wolf JS. Laparoscopic and open surgical nephrectomy for xanthogranulomatous pyelonephritis. J Endourol. 2005;19:813–817. doi: 10.1089/end.2005.19.813. [DOI] [PubMed] [Google Scholar]
- 4.Chuang CK, Lai MK, Chang PL, et al. Xanthogranulomatous pyelonephritis: experience in 36 cases. J Urol. 1992;147:333–336. doi: 10.1016/s0022-5347(17)37229-4. [DOI] [PubMed] [Google Scholar]
- 5.Eastham J, Ahlering T, Skinner E. Xanthogranulomatous pyelonephritis: clinical findings and surgical considerations. Urology. 1994;43:295–299. doi: 10.1016/0090-4295(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 6.Goodman M, Curry T, Russell T. Xanthogranulomatous pyelonephritis (XGP): a local disease with systemic manifestations. Report of 23 patients and review of the literature. Medicine. 1979;58:171–181. [PubMed] [Google Scholar]
- 7.Bercowsky E, Shalhav AL, Portis A, Elbahnasy AM, McDougall EM, Clayman RV. Is the laparoscopic approach justified in patients with xanthogranulomatous pyelonephritis? Urology. 1999;54:437–442. doi: 10.1016/s0090-4295(99)00261-7. [DOI] [PubMed] [Google Scholar]
- 8.Merrot T, Ordorica-Flores R, Steyeart H, Ginier C, Valla JS. Is diffuse xanthogranulomatous pyelonephritis a contraindication to retroperitoneoscopic nephroureterectomy? A case report. Surg Laparosc Endosc. 1998;8:366–369. [PubMed] [Google Scholar]
- 9.Traxer O, Pearle MS. Laparoscopic nephrectomy for benign disease. Review Semin Laparosc Surg. 2000;7:176–184. [PubMed] [Google Scholar]
- 10.McDougall EM, Clayman RV. Laparoscopic nephrectomy for benign disease: comparison of the transperitoneal and retroperitoneal approaches. J Endourol. 1996;10:45–49. doi: 10.1089/end.1996.10.45. [DOI] [PubMed] [Google Scholar]
- 11.Anderson KR. Simple nephrectomy: managing the difficult case: xanthogranulomatous pyelonephritis and autosomal dominant polycystic kidney disease. J. Endourol. 2000;14:799–802. doi: 10.1089/end.2000.14.799. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs SC, Cho E, Dunkin BJ, et al. Laparoscopic live donor nephrectomy: the University of Maryland 3-year experience. J Urol. 2000;164:1494–1499. [PubMed] [Google Scholar]
- 13.Lee BR, Chow GK, Ratner LE, Kavoussi LR. Laparoscopic live donor nephrectomy: outcomes equivalent to open surgery. J Endourol. 2000;14:811–819. doi: 10.1089/end.2000.14.811. [DOI] [PubMed] [Google Scholar]
- 14.Brown SL, Biehl TR, Rawlins MC, Hefty TR. Laparoscopic live donor nephrectomy: a comparison with the conventional open approach. J Urol. 2001;165:766–769. [PubMed] [Google Scholar]
- 15.Gupta NP, Agrawal AK, Sood S. Tubercular pyelonephritic nonfunctioning kidney: another relative contraindication for laparoscopic nephrectomy: a case report. J Laparoendosc. Adv Surg Tech. 1997;7:131–134. doi: 10.1089/lap.1997.7.131. [DOI] [PubMed] [Google Scholar]
- 16.Hemal AK, Gupta NP, Wadhwa SN, Goel A, Kumar R. Retroperitoneoscopic nephrectomy and nephroureterectomy for benign nonfunctioning kidneys: a single-center experience. Urology. 2001;57:644–649. doi: 10.1016/s0090-4295(00)01059-1. [DOI] [PubMed] [Google Scholar]
- 17.Lee KS, Kim HH, Byun SS, Kwak C, Park K, Ahn H. Laparoscopic nephrectomy for tuberculous nonfunctioning kidney: comparison with laparoscopic simple nephrectomy for other diseases. Urology. 2002;60:411–414. doi: 10.1016/s0090-4295(02)01759-4. [DOI] [PubMed] [Google Scholar]
- 18.Hsia I, Kapoor A. Technique of laparoscopic nephrectomy in a patient with previous urinary diversion. Can J Urol. 2003;10:2017–2019. [PubMed] [Google Scholar]
- 19.Rassweiler J, Fornara P, Weber M, et al. Laparoscopic nephrectomy: the experience of the laparoscopy working group of the German Urologic Association. J Urol. 1998;160:18–21. doi: 10.1016/s0022-5347(01)63015-5. [DOI] [PubMed] [Google Scholar]
- 20.Vanderbrink BA, Ost MC, Rastinehad A, et al. Laparoscopic versus open radical nephrectomy for xanthogranulomatous pyelonephritis: Contemporary outcomes analysis. J Endourol. 2007;21:65–70. doi: 10.1089/end.2006.0188. [DOI] [PubMed] [Google Scholar]
- 21.Campanario-Pérez R, Sáiz-Marenco R, Amores-Bermúdez J, et al. Laparoscopic Nephrectomy for the Management of Xanthogranulomatous Pyelonephritis: Still a Challenging Procedure. J Endourol. 2018;32:859–864. doi: 10.1089/end.2018.0467. [DOI] [PubMed] [Google Scholar]
- 22.Arvind NK, Singh O, Ali Q, Gupta SS, Sahay S. Laparoscopic nephrectomy in xanthogranulomatous pyelonephritis: 7-year single surgeon outcome. Urology. 2011;78:797–801. doi: 10.1016/j.urology.2011.05.062. [DOI] [PubMed] [Google Scholar]
- 23.Ma L, Yu Y, Ge G, Li G. Laparoscopic nephrectomy outside gerota fascia and En bloc ligation of the renal hilum for management of inflammatory renal diseases. Int Braz J Urol. 2018;44:280–287. doi: 10.1590/S1677-5538.IBJU.2017.0363. [DOI] [PMC free article] [PubMed] [Google Scholar]