Abstract
Objective
To evaluate changes in staff perspectives towards indwelling urinary catheter (IUC) use after implementation of a 1-year quality improvement project.
Design
Repeated cross-sectional survey at baseline (October 2016) and 12-month follow-up (October 2017).
Setting
Seven acute care hospitals in Switzerland.
Participants
The survey was targeted at all nursing and medical staff members working at the participating hospitals at the time of survey distribution. A total of 1579 staff members participated in the baseline survey (T0) (49% response rate) and 1527 participated in the follow-up survey (T1) (47% response rate).
Intervention
A multimodal intervention bundle, consisting of an evidence-based indication list, daily re-evaluation of ongoing catheter need and staff training, was implemented over the course of 9 months.
Main outcome measures
Staff knowledge (15 items), perception of current practices and culture (scale 1–7), self-reported responsibilities (multiple-response question) and determinants of behaviour (scale 1–7) before and after implementation of the intervention bundle.
Results
The mean number of correctly answered knowledge questions increased significantly between the two survey periods (T0: 10.4, T1: 11.0; p<0.001). Self-reported responsibilities with regard to IUC management by nurses and physicians changed only slightly over time. Perception of current practices and culture in regard to safe urinary catheter use increased significantly (T0: 5.3, T1: 5.5; p<0.001). Significant changes were also observed for determinants of behaviour (T0: 5.3, T1: 5.6; p<0.001).
Conclusion
We found small but significant changes in staff perceptions after implementation of an evidence-based intervention bundle. Efforts now need to be targeted at sustaining and reinforcing these changes, so that restrictive use of IUCs becomes an integral part of the hospital culture.
Keywords: patient safety, indwelling urinary catheter, survey, intervention bundle, perception
Strengths and limitations of this study.
The repeated survey design allowed us to assess changes in staff perspectives after implementation of a quality improvement intervention; sustainability of the effects over time, however, could not be evaluated.
By using self-generated identification codes to match respondents in the two surveys, it was possible to evaluate if results obtained at the group level (two cross-sections) represent results at the individual participant level (longitudinal).
No control group was included in the study design.
It is possible that other trends or measures within the hospitals may have affected the outcomes.
Introduction
Although indwelling urinary catheters (IUCs) are commonly used in acute care hospitals, an appropriate medical indication is often missing.1 2 IUCs are associated with urinary tract infections and non-infectious complications such as haematuria and urethral injury. The reduction of IUC use is therefore a key measure to increase patient safety.3–7
Several quality improvement (QI) studies have shown that avoiding inappropriate IUC use prevents urinary catheter harm.8–11 Common to these studies is the implementation of a multimodal intervention bundle focusing on the reduction of unnecessary catheter use, proper insertion techniques and safe catheter maintenance. Successful bundles consist of catheter restriction protocols providing appropriate indications for catheter use and suggesting alternative urine collection methods, evaluation strategies such as reminders and/or stop orders to assess ongoing catheter need and prompt removal of unnecessary catheters, as well as educational interventions to increase awareness among healthcare workers and ensure safe catheter handling.12
In addition to best practices, changes in behaviour and culture—the so-called socioadaptive component—are considered a core element of QI efforts.13 14 The organisational culture, which may be described as ‘the way we do things around here’,15 is known to have a favourable influence on patient safety, although the evidence for a direct causative effect on patient outcome is weak.16 17 Several studies suggest that changes in staff knowledge and attitudes are needed to improve practice in regard to appropriate catheter utilisation and prevention of catheter-associated infections.18–23 However, to our knowledge, only few studies24–26 have reported the effects of a multimodal intervention bundle on staff knowledge and socioadaptive components, such as perceptions and beliefs, but none of them addressed all these factors together.
To promote safe urinary catheter use in Swiss hospitals, a national QI project was developed and conducted by the Swiss Patient Safety Foundation in partnership with Swissnoso, the National Center for Infection Control. The QI project was modelled after other successful QI initiatives in the USA.8 9 The overall project goal was to reduce IUC use and to promote safe catheter insertion and maintenance by implementing an evidence-based intervention bundle in seven Swiss acute care hospitals.
With the present study, we aimed to assess the changes in staff perspectives in the participating hospitals using survey data collected before and after implementation of the intervention bundle. We hypothesised that the intervention bundle may affect staff members differently depending on their tasks, responsibilities and familiarity with catheterisation. We therefore stratified results according to professional group, managerial function (a proxy for hierarchical status and clinical proximity) and frequency of catheter use in order to explore changes within these groups over time. In before/after study designs, data from two (or more) cross-sectional survey waves are commonly analysed at the group level to evaluate short-term effects of an intervention.27–29 However, given the high staff turnover in hospitals and self-selection of participants, it is possible that survey participants are not identical at the different measurement points. Thus, documented changes in staff perspectives between two time points may merely be due to a different composition of participant groups. We therefore used the self-generated identification (ID) code technique30 to anonymously match respondents in the two surveys. This allowed us to compare the effects observed in the overall sample with the effects observed in a subsample of matched participants, for whom we can assume that they had been working at the hospitals for the entire duration of the project.
Methods
Setting
The QI project consisted of two parts, a campaign to raise awareness among healthcare workers and an intervention that was implemented in seven pilot hospitals. For the campaign, recommendations on safe IUC use in acute care hospitals31 were developed and disseminated to all acute care hospitals (including pilot hospitals) in Switzerland after collection of baseline data in the pilot hospitals (November 2016). The intervention focused on the implementation of an evidence-based intervention bundle in seven pilot hospitals over the course of 9 months (February–October 2017). The participating hospitals contractually committed to implement the three main components of the bundle: an evidence-based indication list for urinary catheterisation (online supplementary appendix 1), a process to evaluate and document the continued need for catheterisation on a daily basis, and staff education on proper catheter insertion and maintenance. For the latter, hospitals were required to provide theoretical trainings on safe urinary catheter utilisation and catheter-associated complications to all nursing and medical staff members working on the pilot units. They were also encouraged to offer practical training sessions for catheter insertion. Local project teams received templates for training materials from the programme team, but they were free to design and organise the trainings according to their local structure and processes. In theoretical trainings, information on risk factors for and prevention of catheter-associated complications, correct indications for urinary catheters, and proper catheter insertion techniques was conveyed either by means of presentations at staff events and/or through completion of an e-learning tool. In most hospitals, theoretical trainings were mandatory for nursing and medical staff. In two hospitals, theoretical inputs were immediately followed by practical training sessions for catheter insertion; in four hospitals, practical trainings were offered on separate occasions and attendance was voluntary. One hospital did not offer practical training sessions. No exact data could be elicited in regard to the percentage of staff members from the pilot units that actually completed theoretical and/or practical trainings. Strategies to implement the intervention bundle in pilot hospitals included designated champions, internal newsletters, posters and screen savers with key project messages.
bmjopen-2018-028740supp001.pdf (84.9KB, pdf)
The hospitals (one small local hospital, four mid-sized regional hospitals and two university hospitals) were recruited to represent different organisational types and geographical regions. Each hospital could decide which wards participated in the project; however, the participation of the emergency department was mandatory. Participating wards included internal medicine, general surgery and neurosurgery, and gynaecology/obstetrics. At each site, interdisciplinary project teams, generally consisting of physicians, nurses and representatives from quality management and the infection prevention unit, were responsible for implementing the intervention bundle in the participating organisational units. To encourage knowledge exchange between the local project teams, two full-day workshops were organised at the beginning and at the end of the intervention phase. The intervention was accompanied by a before/after surveillance and a before/after staff survey. The results of the before/after surveillance, which measured urinary catheter utilisation ratio and catheter-associated complications, will be reported elsewhere. Our publication will focus on the results from the staff surveys and their changes over time.
Study design
To collect data on staff perspectives regarding IUC use, we conducted a written survey during two time periods. The baseline survey (T0) took place in October 2016, 4 months before the participating hospitals started to implement the intervention bundle. The follow-up survey (T1) took place 1 year later in October 2017. At that point, all hospitals had implemented the intervention bundle and had been working with the new processes for 6–8 months. The target population consisted of surgical positioning specialists, nurses (healthcare assistants, registered nurses and nursing managers) and physicians (residents, senior and chief physicians) working on the participating units in one of the seven pilot hospitals at the time of the survey. Staff members not involved in direct patient care, healthcare workers in education and affiliated physicians were excluded.
Questionnaire
The 55-item standardised questionnaire was developed specifically for this study by the authors based on prior survey research conducted during a similar improvement project32 33 and a review of existing surveys reported in the literature18–22 (online supplementary appendix 2). The German version of the questionnaire was pretested among 42 physicians and nurses from three hospitals not participating in the project. Based on their feedback, minor modifications were made to increase validity. The final version was translated into French and Italian by professional translators. Translations were reviewed by four native speakers per language.
The questionnaire consisted of four thematic sections. The first section entailed a 15-item knowledge test on prevalence, risk factors and prevention of catheter-associated complications, as well as appropriate reasons for catheter placement. The second section included 13 items assessing respondents’ perception regarding good practices and cultural factors for safe IUC use within the organisation. Items were rated on a 7-point Likert scale from ‘strongly disagree’ (1) to ‘strongly agree’ (7). Two items were negatively worded and were reverse-coded for data analysis. The content of the first two sections of the questionnaire was in line with the above-mentioned recommendations for safe catheter use.31 The third section examined self-perceived responsibilities in regard to catheter prescription, placement and care by means of one multiple-response question. The fourth section assessed determinants of personal behaviour in regard to the reduction of urinary catheters. Items for this section were developed based on the theory of planned behaviour.34 This theory states that an individual’s intention to perform a behaviour is largely determined by three factors, namely a favourable or unfavourable evaluation of the behaviour (attitudes), the perceived social expectations to perform or not perform the behaviour (subjective norms), and the perceived capability to perform the behaviour (perceived behavioural control).34 35 In our questionnaire, the three constructs (attitudes, subjective norms and perceived behavioural control) were measured with five items each. All 15 items were rated on a 7-point Likert scale from ‘strongly disagree’ (1) to ‘strongly agree’ (7). Two items were negatively worded and were reverse-coded for analysis.
The questionnaire also included a section on demographics and experience with placing urinary catheters. On the first page of the questionnaire, participants were asked to generate an eight-digit code consisting of three elements. To do this, respondents were asked to link the following three elements into a string of letters and numbers: the mother’s initials (maiden name), the father’s initials and the mother’s birth year (for an example see online supplementary appendix 2). These three elements were selected because they do not change over time and refer to personal information usually known by the respondent.30 With this technique, it is possible to clearly identify data from the same subject and, at the same time, ensure anonymity. We used the same questionnaire at both time points. For the follow-up survey, we included four additional questions that specifically referred to the intervention bundle. All other items remained unaltered.
Data collection
Each local project team was required to identify all eligible staff members from the target population, inform and invite them to participate in the survey, and distribute and collect the print version of the questionnaire. In some sites, questionnaires were handed out during shift reports or other staff events; in others they were distributed to internal mail boxes. In one hospital, questionnaires were sent to private home addresses. Participation in the survey was voluntary and anonymous. The returning of the questionnaire was considered informed consent.
Data analysis
Descriptive statistics were calculated for each item. Missing values were excluded from analysis (pairwise exclusion). A large proportion of subjects participating in the baseline survey did not participate in the follow-up survey. Thus, responses to both surveys cannot be assumed to stem from the same sample. Therefore, tests for unpaired samples were used for the main analyses comparing results between time points (see below for analyses of matched individuals). χ2 tests were used to determine differences in sample composition. A ‘knowledge score’ was generated consisting of the number of correctly answered questions out of 15. Cronbach’s alpha was calculated to determine internal consistency of the 13-item perception scale and the 15-item behaviour scale. For both scales mean scale score and 95% CI were computed. Knowledge score and mean scale scores were computed for the overall sample and stratified by professional group (nurses/physicians), managerial function (with/without) and frequency of catheter placement (frequent/infrequent user). Frequent users were defined as healthcare workers placing a catheter a few times a month or more often, and infrequent users as placing a catheter a few times a year or less often. Frequency was determined based on the self-reported frequency of placing a catheter in the current work position. Changes between time points were determined for the overall sample and each subgroup by means of t-tests for independent samples.
To analyse the subsample of matched participants, self-generated IDs were matched based on the eight-digit code and hospital affiliation. For these subanalyses, cases with identical codes or missing data were dropped. For matched participants, knowledge score and mean scale scores were computed. To determine changes between time points in this subsample of matched participants, we used paired analysis. Changes between time points were determined by means of t-test for paired samples. Mixed analysis of variance was conducted to determine if participation in theoretical and practical training had an effect on knowledge scores over time. In addition, we performed difference-in-difference analyses to compare results for group-level data (cross-sectional data of two unmatched groups) and individual-level data (longitudinal data of matched participants). For each of the main outcomes, we compared the average change over time among matched participants with the average change over time among unmatched participants.
All tests were two-sided and a p value <0.05 was considered statistically significant. Cohen’s d was calculated as a measure of effect size. For paired samples, the formula tc as described in Dunlap et al 36 was used to calculate d. As an orientation for interpreting the importance of the effect, we used the following classification: 0.2=small effect, 0.5=medium effect and 0.8=large effect.37 All analyses were performed with Stata V.14.1.
Patient and public involvement
Patients or the public were not involved in the design or planning of this study.
Results
Response rate and study sample
Out of 3245 invited staff members, 1579 participated in the baseline survey (48.7% response rate), and 1527 out of 3235 invited staff members participated in the follow-up survey (47.2% response rate). The proportion of questionnaires received from each hospital in the total sample was similar in both waves (p=0.39). The characteristics of the study samples at T0 and T1 are provided in table 1. Sample composition differed slightly in regard to age (p=0.03), profession (p=0.04) and work unit between the two time points (p=0.02).
Table 1.
Study sample characteristics
| T0 | T1 | P value* | |
| n=1579 | n=1527 | ||
| Participants per hospital, n (%)† | 0.385 | ||
| Hospital A (approximately 900 beds) | 221 (14.0) | 223 (14.6) | |
| Hospital B (approximately 800 beds) | 154 (9.8) | 170 (11.1) | |
| Hospital C (approximately 500 beds) | 138 (8.7) | 127 (8.3) | |
| Hospital D (approximately 500 beds) | 362 (22.9) | 325 (21.3) | |
| Hospital E (approximately 400 beds) | 347 (22.0) | 342 (22.4) | |
| Hospital F (approximately 300 beds) | 284 (18.0) | 250 (16.4) | |
| Hospital G (approximately 100 beds) | 73 (4.6) | 90 (5.9) | |
| Female, n (%) | 1187 (77.6) | 1191 (79.7) | 0.173 |
| Age in years, mean (SD) | 36.8 (10.5) | 35.9 (10.5) | 0.0255 |
| Profession, n (%) | 0.043 | ||
| Nurse | 1050 (69.1) | 1084 (72.8) | |
| Physician | 350 (23.0) | 288 (19.3) | |
| Other | 120 (7.9) | 117 (7.9) | |
| With managerial function, n (%) | 232 (16.4) | 193 (13.9) | 0.066 |
| Years working in this hospital, n (%) | 0.849 | ||
| <2 | 376 (24.5) | 380 (25.4) | |
| 2 to <5 | 385 (25.0) | 357 (23.9) | |
| 5 to <10 | 264 (17.2) | 271 (18.1) | |
| 10 to <20 | 307 (20.0) | 297 (19.9) | |
| ≥20 | 206 (13.4) | 190 (12.7) | |
| Work unit in the past 3 months, n (%) | 0.020 | ||
| Ward | 906 (58.5) | 963 (63.9) | |
| Emergency department | 248 (16.0) | 190 (12.6) | |
| Intensive care unit | 144 (9.3) | 129 (8.6) | |
| Operating room | 146 (9.4) | 141 (9.4) | |
| Other | 104 (6.7) | 85 (5.6) | |
| Overall experience with catheter placement throughout career, n (%) |
0.300 | ||
| Never | 26 (1.7) | 30 (2.0) | |
| 1–5 times | 169 (11.0) | 171 (11.4) | |
| 6–20 times | 341 (22.2) | 370 (24.6) | |
| >20 times | 1002 (65.2) | 931 (62.0) | |
| Frequency of catheter placement in current position, n (%) | 0.084 | ||
| Frequent user | 690 (44.2) | 618 (41.1) | |
| Infrequent user | 871 (55.8) | 885 (58.9) | |
Due to rounding percentages may not always add up to 100%.
T0: baseline survey; T1: follow-up survey.
Frequent user: places a catheter a few times a month or more often; infrequent user: places a catheter a few times a year or less often.
*P values for changes between the two time periods.
†In the larger hospitals, not all of the departments participated in the project.
Almost all of the 3106 participants in both survey periods generated an eight-digit ID. At baseline, 35 respondents (2.2%) had missing values on each of the three code elements and the sample contained three sets of identical IDs. At follow-up, 51 respondents (3.3%) did not provide an eight-digit ID and two sets of identical IDs were found. For 420 respondents, we were able to successfully match the eight-digit ID code and hospital affiliation. This represents 27.5% of the 1527 potential matches. There were 1118 IDs only present at T0 and 1052 IDs only present at T1.
Knowledge
For the overall study sample, the mean number of correctly answered knowledge items increased significantly between T0 and T1 (p<0.001) (table 2). Subgroup analysis indicates that knowledge scores increased in particular for nurses, staff members without managerial function and staff members frequently placing catheters. Effect sizes for the changes between the time points were small to moderate. Percentages of correct answers for each of the 15 items are provided in online supplementary appendix 3.
Table 2.
Mean number of correct answers provided for 15 knowledge items
| MeanT 0 (95% CI) | nT0 | MeanT1 (95% CI) | nT1 | P value | Effect size | |
| Overall sample | 10.4 (10.3 to 10.5) | 1579 | 11.0 (10.9 to 11.1) | 1527 | <0.001 | 0.29 |
| Professional group | ||||||
| Nurses | 10.2 (10.1 to 10.4) | 1050 | 10.9 (10.8 to 11.0) | 1084 | <0.001 | 0.35 |
| Physicians | 11.1 (11.0 to 11.3) | 350 | 11.4 (11.2 to 11.6) | 288 | 0.047 | 0.16 |
| Managerial function | ||||||
| With | 11.3 (11.1 to 11.5) | 232 | 11.6 (11.4 to 11.9) | 193 | 0.058 | 0.19 |
| Without | 10.3 (10.1 to 10.4) | 1187 | 10.9 (10.8 to 11.0) | 1199 | <0.001 | 0.33 |
| Frequency of catheter placement | ||||||
| Frequent user | 10.0 (9.8 to 10.1) | 690 | 10.7 (10.6 to 10.9) | 618 | <0.001 | 0.40 |
| Infrequent user | 10.8 (10.7 to 10.9) | 871 | 11.2 (11.1 to 11.3) | 885 | <0.001 | 0.22 |
| Matched identification | 10.4 (10.3 to 10.6) | 420 | 11.3 (11.1 to 11.5) | 420 | <0.001 | 0.49 |
| Unmatched identification | 10.5 (10.3 to 10.6) | 1118 | 11.0 (10.9 to 11.1) | 1052 | <0.001 | 0.31 |
T0: baseline survey; T1: follow-up survey.
Frequent user: places a catheter a few times a month or more often; infrequent user: places a catheter a few times a year or less often.
We used the subsample of matched participants to examine the effect of training on the change in knowledge score over time. Among all matched respondents, 102 (25.3%) indicated having participated in both theoretical and practical training; 130 (32.2%) respondents had participated in either theoretical or practical training; and 172 (42.6%) respondents did not participate in any training (missing values n=16). Results from the mixed analysis of variance showed that there was no significant interaction effect between time and training (F 2,401 =1.05, p=0.35). In other words, knowledge scores between participants with practical and/or theoretical training did not change differently over time as compared with participants without training.
Perception of practices and culture
The mean scale score for perception of current practices and culture increased significantly within the overall sample and within all subgroups between the two time points (p<0.001) (table 3). Generally, agreement to the statements was moderate at baseline and strengthened over time. Yet agreement remained moderately strong, with no group reaching a mean scale score above 6 even after implementation of the intervention bundle. The mean scores for each item are provided in online supplementary appendix 4.
Table 3.
Perception: mean scale score
| MeanT0 (95% CI) | nT0 | MeanT1 (95% CI) | nT1 | P value | Effect size | |
| Overall sample | 5.3 (5.3 to 5.3) | 1568 | 5.5 (5.5 to 5.6) | 1521 | <0.001 | 0.31 |
| Professional group | ||||||
| Nurses | 5.4 (5.3 to 5.4) | 1044 | 5.6 (5.6 to 5.7) | 1082 | <0.001 | 0.33 |
| Physicians | 5.1 (5.0 to 5.1) | 347 | 5.3 (5.2 to 5.4) | 286 | <0.001 | 0.29 |
| Managerial function | ||||||
| With | 5.2 (5.1 to 5.3) | 230 | 5.6 (5.5 to 5.7) | 191 | <0.001 | 0.52 |
| Without | 5.3 (5.3 to 5.4) | 1180 | 5.6 (5.5 to 5.6) | 1197 | <0.001 | 0.29 |
| Frequency of catheter placement | ||||||
| Frequent user | 5.2 (5.1 to 5.3) | 690 | 5.4 (5.3 to 5.5) | 618 | <0.001 | 0.22 |
| Infrequent user | 5.4 (5.3 to 5.4) | 861 | 5.7 (5.6 to 5.7) | 880 | <0.001 | 0.37 |
| Matched identification | 5.4 (5.3 to 5.4) | 416 | 5.6 (5.5 to 5.7) | 416 | <0.001 | 0.32 |
| Unmatched identification | 5.3 (5.2 to 5.3) | 1108 | 5.5 (5.5 to 5.6) | 1049 | <0.001 | 0.31 |
Scale consisted of 13 items. Items were answered on a scale from 1 (strongly disagree) to 7 (strongly agree). Cronbach’s alpha for the scale: T0 α=0.79 and T1 α=0.80.
T0: baseline survey; T1: follow-up survey.
Frequent user: places a catheter a few times a month or more often; infrequent user: places a catheter a few times a year or less often.
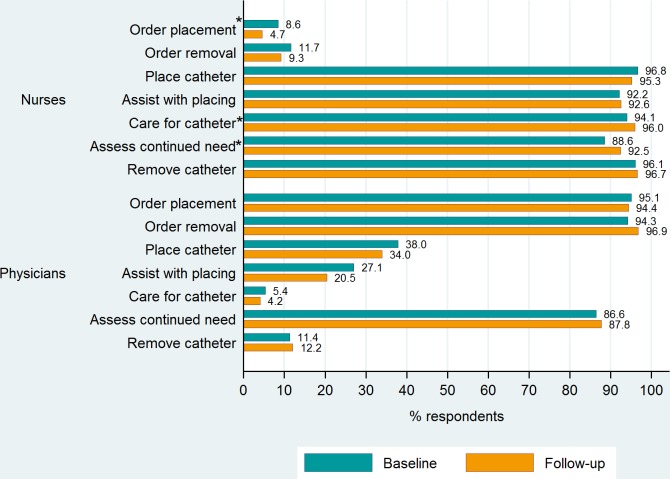
Responsibilities
Self-reported responsibilities concerning IUC management by nurses and physicians changed only slightly over time (figure 1). At baseline and at follow-up, nurses mainly felt responsible for placing, maintaining and removing an IUC. However, at T1, fewer nurses felt responsible for prescribing catheter placement (p<0.001) as compared with T0, and a higher percentage felt responsible for assessing the need for continued catheterisation (p=0.002). Physicians perceived themselves to be mainly responsible for ordering catheter placement and removal at both time points. At T1, fewer of them felt responsible for placing or assisting with placing an IUC as compared with T0, but differences were not statistically significant.
Figure 1.
Self-reported responsibilities in regard to urinary catheters by profession. *Change between time periods significant at p<0.05.
Determinants of behaviour
The mean score for the scale assessing the determinants of behaviour increased significantly between baseline and follow-up (p<0.001). Positive changes in mean scores were observed for all three constructs (attitudes, subjective norms and perceived behavioural control). They were particularly strong for items assessing perceived social expectations to use catheters restrictively (see online supplementary appendix 5). The positive trends could also be observed for professional group, managerial function and frequency of catheter placement (table 4). Medium effect sizes indicate practical relevance of these changes.
Table 4.
Determinants of behaviour: mean scale score
| MeanT0 (95% CI) | nT0 | MeanT1 (95% CI) | nT1 | P value | Effect size | |
| Overall sample | 5.3 (5.3 to 5.3) | 1539 | 5.6 (5.6 to 5.6) | 1502 | <0.001 | 0.43 |
| Professional group | ||||||
| Nurses | 5.3 (5.2 to 5.3) | 1046 | 5.6 (5.6 to 5.7) | 1083 | <0.001 | 0.56 |
| Physicians | 5.4 (5.3 to 5.5) | 349 | 5.6 (5.5 to 5.6) | 287 | 0.005 | 0.23 |
| Managerial function | ||||||
| With | 5.6 (5.5 to 5.7) | 230 | 5.8 (5.7 to 5.9) | 192 | <0.001 | 0.38 |
| Without | 5.2 (5.2 to 5.3) | 1184 | 5.6 (5.5 to 5.6) | 1198 | <0.001 | 0.50 |
| Frequency of catheter placement | ||||||
| Frequent user | 5.2 (5.2 to 5.3) | 675 | 5.6 (5.5 to 5.6) | 615 | <0.001 | 0.46 |
| Infrequent user | 5.3 (5.3 to 5.4) | 847 | 5.6 (5.6 to 5.7) | 884 | <0.001 | 0.41 |
| Matched identification | 5.3 (5.3 to 5.4) | 405 | 5.7 (5.6 to 5.8) | 405 | <0.001 | 0.58 |
| Unmatched identification | 5.3 (5.3 to 5.3) | 1090 | 5.6 (5.5 to 5.6) | 1038 | <0.001 | 0.37 |
Scale consisted of 15 items. Items were answered on a scale from 1 (strongly disagree) to 7 (strongly agree). Cronbach’s alpha for scale: T0 α=0.72 and T1 α=0.74.
T0: baseline survey; T1: follow-up survey.
Frequent user: places a catheter a few times a month or more often; infrequent user: places a catheter a few times a year or less often.
Difference-in-difference analyses of group-level and individual-level data
Knowledge scores increased slightly more among participants with a matched ID compared with unmatched participants (p=0.047). The mean scale scores for perception of current practices and culture increased for both matched and unmatched participants to a similar extent (p=0.894). The mean scale scores for determinants of behaviour increased slightly more for participants with a matched ID compared with unmatched participants (p=0.033).
Discussion
We observed positive changes in staff knowledge, perceptions and attitudes regarding IUC use following the implementation of a multimodal intervention bundle in seven hospitals. Observed effects were small to moderate, requiring a closer look at the challenges of implementing and evaluating a multifaceted intervention bundle in a large-scale, national programme. We found that in two of the thematic sections—knowledge and determinants of behaviour—the scores for matched participants increased slightly more than for unmatched participants. This seems plausible as the unmatched group includes participants of various levels of programme exposition. It suggests that data analysed at the group level (two unmatched cross-sections) to evaluate short-term effects of an intervention can to some extent, but not fully represent longitudinal effects at the individual participant level.
Knowledge scores increased significantly between baseline and follow-up, indicating that staff members in our pilot hospitals had more factual knowledge about the use and potential harm of urinary catheters after the intervention. Interestingly, however, we could not verify that participation in education and training sessions contributed to knowledge increases. When analysing the results in our subsample of matched participants (ie, individuals for whom we know that they worked in the hospital throughout the entire programme), we found that changes in knowledge scores did not differ between staff members with and without training. The findings indicate that other factors, such as the dissemination of the indication list or the presence of champions, may have contributed to the observed effects in knowledge. Regarding respondents’ perception of current practices and cultural factors within their organisation, we also found a small but significant effect at the end of the intervention. The moderate effect size suggests that staff members indeed perceived positive changes in IUC management and safety climate within their organisation. Factors determining intentions to perform a certain behaviour, namely personal attitudes, perceived behavioural control and subjective norms, changed over the course of the project too. At follow-up, staff members generally expressed higher willingness to contribute to a safe and restrictive use of IUCs. In particular, participants felt higher expectations from their social environment to reduce catheters, suggesting that a change in culture could indeed be initiated.
Even though there was a clear positive trend, the differences between survey periods on all three sections of the questionnaire (knowledge, perception of practices and culture, and determinants of behaviour) were only small to moderate. Recommended practices and socioadaptive components were thus from the perspective of participants, not fully established even after the intervention. These results are not surprising because change in organisational culture is a slow process, requiring endurance and continuous effort that could not be provided within the short time frame of the QI programme. Studies that have collected long-term data on surgical checklist implementation suggest that it takes time for cultural change to develop and for positive effects to fully become evident.38 39 For example, an Australian study that has examined compliance with surgical safety checklist use reports that reduction in mortality rates reached significance only in the period of 2–3 years after implementation.38 In addition, we did not strictly define implementation strategies in order to allow pilot hospitals to adapt the intervention bundle to their local context. Therefore, implementation fidelity could not systematically be assessed. Informal feedback from local project coordinators suggests that it was not always possible to deliver the intervention bundle as intended. For example, even though training sessions were mandatory, not all staff from the target population could eventually be reached.
Another explanation could be high staff turnover rates. Almost all of the respondents generated an eight-digit code. Interestingly, however, only 28% of the IDs provided could be matched between the two surveys. Participants at follow-up were thus, for the most part, not the same individuals as at baseline. This could be a sign for high staff turnover rates during the intervention period. However, it is also possible that unmatched participants had been working at the hospital throughout the intervention, but had been unwilling or unable to participate in the same survey twice. Nevertheless, this finding points to the importance of ensuring that hospitals continuously offer training, education and policy reinforcement. Continued efforts to incorporate recommended practices into routine care even after completion of the actual project phase are needed to move the intervention from a time-limited ‘project’ to a continuous commitment, and ensure that motivation to reduce urinary catheters is kept at a high level.40 41
In our QI programme, a before/after surveillance for catheterisation and catheter-associated complications was conducted in the same time periods as the staff survey. Results show a significant decrease in catheter utilisation rates in all pilot hospitals (A. Schweiger, S. Kuster, J. Maag, et al., unpublished data, manuscript in preparation, 2019). Secondary data analysis would be needed to examine the relationship between catheter utilisation rates and staff perspectives. Some hypotheses can be put forward to explain the observation that while changes in staff perspectives were rather small, we did see a decrease in catheter utilisation. It is possible that even small changes in staff knowledge and perception can have a substantial practical relevance. However, it is also possible that the items in our questionnaire do not adequately measure knowledge and perceptions required to reduce IUC use (content validity). To our knowledge, no other study has assessed the effects of an intervention bundle on staff behaviour with similar measures; therefore, it is not possible to relate our findings to existing research. Wakefield and colleagues15 found that perceptions about the behaviour of professional peers and the personal belief that engaging in a certain behaviour will lead to better safety outcomes are the strongest factors influencing safety behaviour. The authors conclude that interventions too often rely on educational measures in order to change behaviour and argue that using behavioural models to design interventions may be more effective. Our results provide additional support for this argument. We saw the strongest effects in perceived norms to reduce catheter use, suggesting that efforts aimed at changing organisational culture may be particularly effective. We would however argue that staff education and training can offer an important platform to disseminate and reinforce new norms and expectations, especially if they are used by clinical leaders to demonstrate their commitment to the cause and to foster interprofessional collaboration.
Promoting collaboration among nurses and physicians is especially important because urinary catheter management is a strongly interprofessional topic, and roles and responsibilities need to be clear for all of the involved healthcare workers. In a previous study with data from the baseline survey, we analysed how nurses and physicians perceived their respective responsibilities for IUC management.42 We found that physicians mainly felt responsible for prescribing catheter placement and removal, while nurses generally considered themselves responsible for placing, managing and removing them. However, both nurses and physicians felt equally responsible for assessing the need for continued catheterisation. The results from the present study show that, at the end of the intervention, the perceived division of tasks between the two groups remained largely the same. This could either indicate that because of the intervention bundle both groups were encouraged to assume responsibility in this area and interprofessional commitment was strengthened. However, it could also mean that tasks especially in regard to the re-evaluation of the need for a catheter were not clarified over the course of the project.
Limitations
This study has several limitations. We used the theory of planned behaviour to model intention to reduce urinary catheter use. However, it is not possible to know if changes observed in staff perceptions led to a true change in practice. In a future study, staff survey data should be linked with surveillance data at the hospital level to examine if specific changes in staff perceptions are associated with changes in specific clinical outcomes. Direct observations of catheter placements may be considered as another method to gain insight into compliance with protocols for safe catheterisation and changes in clinical practice.43 This method was originally proposed to participating hospitals in our project, but was rejected due to the additional resources required. For practical purposes, we did not include a control group in the study design. The single-group design does therefore not allow any causal inferences about the contribution of the intervention bundle to the observed effects. It is possible that other secular trends or measures within the hospitals may have affected the outcomes. A stepped wedge design could present an alternative to this design. This design randomises participating sites into sequential cohorts. All cohorts eventually implement the intervention, each providing their own control data in the mean time and offering researchers the chance to investigate implementation challenges and make adjustments along the way.44 In addition, conducting focus groups or interviews with staff from each site could have provided a more indepth understanding of staff perceptions after the intervention and the contextual factors that shape the implementation of a complex intervention in a new setting. The before/after study design does not allow us to evaluate sustainability of the intervention over time. A further follow-up survey or a time-series approach could have shed more light on the long-term effects in the hospitals. We chose to administer paper instead of electronic versions of the survey to minimise coverage error because not all staff members in participating hospitals had access to individual email addresses. Furthermore, paper surveys have been shown to generate higher response rates than surveys administered online.45 With this method, we were able to attain reasonable response rates at both survey periods. Since data collection was organised by local project teams, however, we have no information on non-participants. It is possible that only highly motivated staff members participated in the survey, which may result in more positive responses. The two survey samples were comparable with respect to participants per hospital. For some of the sociodemographic characteristics, notably profession and work unit, we found significant differences between the two time periods. We cannot differentiate if this is due to selective non-responses or staff fluctuation. Lastly, it is possible that only high-performing units open to change have been chosen to participate in the intervention project. This may limit generalisability of our findings to other units and hospitals.
Conclusion
Changing staff attitudes, knowledge and behaviour are important prerequisites for an effective reduction of catheter use and catheter-associated complications. We found small but significant changes in staff perceptions after implementation of an evidence-based intervention bundle. The positive trends were present in all subgroups, indicating that regardless of responsibilities and practice of catheter placement, perspectives on urinary catheter use changed over time. Efforts now need to be targeted at reinforcing and sustaining these changes, so that restrictive use of IUCs becomes an integral part of the hospital culture.
Supplementary Material
Footnotes
Collaborators: Adriana Degiorgi (Ente Ospedaliero Cantonale, Lugano Civico), Thomas Bregenzer (Spital Lachen), Stefan P Kuster (University and University Hospital Zurich), Marianne Laguardia (Inselspital Universitätsspital Bern), Isabelle Montavon-Blondet (Hôpital neuchâtelois), Jasmin Perret (Kantonsspital Winterthur), Vineeta Bansal (Kantonsspital Winterthur), Anja Waltenspül (Luzerner Kantonsspital) and Sonja Bertschy (Luzerner Kantonsspital).
Contributors: AN, SZ, JM, AS and DLBS contributed to the design of the study and the survey instrument. SPK and GJ contributed to data collection. AN and DLBS analysed the data. AN and SZ drafted the manuscript. JM, AS, SPK, GJ and DLBS critically revised the manuscript for important intellectual content. All authors approved the manuscript.
Funding: This work was supported by a grant from the Swiss Federal Office of Public Health (no 15.011083).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Approval for the study was obtained from the Lead Ethics Committee of the Canton of Bern, Switzerland (no 2016–00682).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Contributor Information
on behalf of the progress! Safe urinary catheterization collaboration group:
Adriana Degiorgi, Thomas Bregenzer, Stefan P Kuster, Marianne Laguardia, Isabelle Montavon Blondet, Jasmin Perret, Vineeta Bansal, Anja Waltenspül, and Sonja Bertschy
Collaborators: on behalf of the progress! Safe urinary catheterization collaboration group
References
- 1. Jansen IAV, Hopmans TEM, Wille JC, et al. Appropriate use of indwelling urethra catheters in hospitalized patients: results of a multicentre prevalence study. BMC Urol 2012;12:2–7. 10.1186/1471-2490-12-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Munasinghe RL, Yazdani H, Siddique M, et al. Appropriateness of use of indwelling urinary catheters in patients admitted to the medical service. Infect Control Hosp Epidemiol 2001;22:647–9. 10.1086/501837 [DOI] [PubMed] [Google Scholar]
- 3. Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control 2000;28:68–75. 10.1016/S0196-6553(00)90015-4 [DOI] [PubMed] [Google Scholar]
- 4. Nicolle LE. Catheter associated urinary tract infections. Antimicrob Resist Infect Control 2014;3:1–8. 10.1186/2047-2994-3-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hollingsworth JM, Rogers MAM, Krein SL, et al. Determining the noninfectious complications of indwelling urethral catheters: a systematic review and meta-analysis. Ann Intern Med 2013;159:401–10. 10.7326/0003-4819-159-6-201309170-00006 [DOI] [PubMed] [Google Scholar]
- 6. Lo E, Nicolle L, Classen D, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol 2008;29(Suppl 1):S41–50. 10.1086/591066 [DOI] [PubMed] [Google Scholar]
- 7. Gould CV, Umscheid CA, Agarwal RK, et al. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol 2010;31:319–26. 10.1086/651091 [DOI] [PubMed] [Google Scholar]
- 8. Saint S, Olmsted RN, Fakih MG, et al. Translating health care-associated urinary tract infection prevention research into practice via the bladder bundle. Jt Comm J Qual Patient Saf 2009;35:449–55. 10.1016/S1553-7250(09)35062-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fakih MG, George C, Edson BS, et al. Implementing a national program to reduce catheter-associated urinary tract infection: a quality improvement collaboration of state Hospital associations, academic medical centers, professional societies, and governmental agencies. Infect Control Hosp Epidemiol 2013;34:1048–54. 10.1086/673149 [DOI] [PubMed] [Google Scholar]
- 10. Janzen J, Buurman BM, Spanjaard L, et al. Reduction of unnecessary use of indwelling urinary catheters. BMJ Qual Saf 2013;22:984–8. 10.1136/bmjqs-2013-001908 [DOI] [PubMed] [Google Scholar]
- 11. Saint S, Greene MT, Krein SL, et al. A program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med 2016;374:2111–9. 10.1056/NEJMoa1504906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meddings J, Rogers MAM, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277–89. 10.1136/bmjqs-2012-001774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Saint S, Howell JD, Krein SL. Implementation science: how to jump‐start infection prevention. Infect Control Hosp Epidemiol 2010;31(Suppl 1):S14–17. 10.1086/655991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Weaver SJ, Lubomksi LH, Wilson RF, et al. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:369–74. 10.7326/0003-4819-158-5-201303051-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wakefield JG, McLaws M-L, Whitby M, et al. Patient safety culture: factors that influence clinician involvement in patient safety behaviours. BMJ Qual Saf 2010;19:585–91. 10.1136/qshc.2008.030700 [DOI] [PubMed] [Google Scholar]
- 16. Meddings J, Reichert H, Greene MT, et al. Evaluation of the association between hospital survey on patient safety culture (HSOPS) measures and catheter-associated infections: results of two national Collaboratives. BMJ Qual Saf 2017;26:226–35. 10.1136/bmjqs-2015-005012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Smith SN, Greene MT, Mody L, et al. Evaluation of the association between nursing home survey on patient safety culture (NHSOPS) measures and catheter-associated urinary tract infections: results of a national collaborative. BMJ Qual Saf 2018;27:464–73. 10.1136/bmjqs-2017-006610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Paras ML, Shenoy ES, Hsu HE, et al. Housestaff knowledge related to urinary catheter use and catheter-associated urinary tract infections. Infect Control Hosp Epidemiol 2015;36:1355–7. 10.1017/ice.2015.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jain M, Dogra V, Mishra B, et al. Knowledge and attitude of doctors and nurses regarding indication for catheterization and prevention of catheter-associated urinary tract infection in a tertiary care hospital. Indian J Crit Care Med 2015;19:76–81. 10.4103/0972-5229.151014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Viswanathan K, Rosen T, Mulcare MR, et al. Emergency department placement and management of indwelling urinary catheters in older adults: knowledge, attitudes, and practice. J Emerg Nurs 2015;41:414–22. 10.1016/j.jen.2015.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Drekonja DM, Kuskowski MA, Johnson JR. Foley catheter practices and knowledge among Minnesota physicians. Am J Infect Control 2010;38:694–700. 10.1016/j.ajic.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 22. Drekonja DM, Kuskowski MA, Johnson JR. Internet survey of Foley catheter practices and knowledge among Minnesota nurses. Am J Infect Control 2010;38:31–7. 10.1016/j.ajic.2009.05.005 [DOI] [PubMed] [Google Scholar]
- 23. Mizerek E, Wolf L. To Foley or not to Foley: emergency nurses’ perceptions of clinical decision making in the use of urinary catheters in the emergency department. J Emerg Nurs 2015;41:329–34. 10.1016/j.jen.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 24. Marigliano A, Barbadoro P, Pennacchietti L, et al. Active training and surveillance: 2 good friends to reduce urinary catheterization rate. Am J Infect Control 2012;40:692–5. 10.1016/j.ajic.2012.01.021 [DOI] [PubMed] [Google Scholar]
- 25. Gray D, Nussle R, Cruz A, et al. Effects of a catheter-associated urinary tract infection prevention campaign on infection rate, catheter utilization, and health care workers’ perspective at a community safety net Hospital. Am J Infect Control 2016;44:115–6. 10.1016/j.ajic.2015.08.011 [DOI] [PubMed] [Google Scholar]
- 26. Fakih MG, Rey JE, Pena ME, et al. Sustained reductions in urinary catheter use over 5 years: bedside nurses view themselves responsible for evaluation of catheter necessity. Am J Infect Control 2013;41:236–9. 10.1016/j.ajic.2012.04.328 [DOI] [PubMed] [Google Scholar]
- 27. Riad-Allen L, Dermody SS, Herman Y, et al. Becoming tobacco-free: changes in staff and patient attitudes and incident reports in a large academic mental health and addictions Hospital. Am J Addict 2017;26:183–91. 10.1111/ajad.12513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mitchell BG, White N, Farrington A, et al. Changes in knowledge and attitudes of hospital environmental services staff: the researching effective approaches to cleaning in hospitals (reach) study. Am J Infect Control 2018;46:980–5. 10.1016/j.ajic.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 29. Laur CV, Keller HH, Curtis L, et al. Comparing hospital staff nutrition knowledge, attitudes, and practices before and 1 year after improving nutrition care: results from the More-2-Eat implementation project. JPEN J Parenter Enteral Nutr 2017;99 10.1177/0148607117718493 [DOI] [PubMed] [Google Scholar]
- 30. Yurek LA, Vasey J, Sullivan Havens D. The use of self-generated identification codes in longitudinal research. Eval Rev 2008;32:435–52. 10.1177/0193841X08316676 [DOI] [PubMed] [Google Scholar]
- 31. Züllig S, Mascherek A. Sicherheit bei Blasenkathetern. Empfehlungen Im Rahmen des nationalen Pilotprogramms progress! Sicherheit bei Blasenkathetern. Zürich: Stiftung für Patientensicherheit, 2016. [Google Scholar]
- 32. Mascherek AC, Schwappach DL, Bezzola P. Frequency of use and knowledge of the WHO-surgical checklist in Swiss hospitals: a cross-sectional online survey. Patient Saf Surg 2013;7:36–7. 10.1186/1754-9493-7-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mascherek AC, Gehring K, Bezzola P, et al. Using the theory of planned behaviour to model antecedents of surgical checklist use: a cross-sectional study. BMC Health Serv Res 2015;15:462 10.1186/s12913-015-1122-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 35. Ajzen I, Manstead ASR. Changing health-related behaviours: an approach based on the theory of planned behaviour : Hewstone M, Schut H, de Wit J, The scope of social psychology: theory and applications. New York: Psychology Press, 2007: 43–63. [Google Scholar]
- 36. Dunlap WP, Cortina JM, Vaslow JB, et al. Meta-Analysis of experiments with matched groups or repeated measures designs. Psychol Methods 1996;1:170–7. 10.1037/1082-989X.1.2.170 [DOI] [Google Scholar]
- 37. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 2013;4:1–12. 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. de Jager E, Gunnarsson R, Ho Y-H. Implementation of the world Health organization surgical safety checklist correlates with reduced surgical mortality and length of hospital admission in a high-income country. World J Surg 2019;43:117–24. 10.1007/s00268-018-4703-x [DOI] [PubMed] [Google Scholar]
- 39. Berry WR, Edmondson L, Gibbons LR, et al. Scaling safety: the South Carolina surgical safety checklist experience. Health Aff 2018;37:1779–86. 10.1377/hlthaff.2018.0717 [DOI] [PubMed] [Google Scholar]
- 40. Dixon-Woods M, Martin GP. Does quality improvement improve quality? Future Hosp J 2016;3:191–4. 10.7861/futurehosp.3-3-191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Böhmer AB, Kindermann P, Schwanke U, et al. Long-term effects of a perioperative safety checklist from the viewpoint of personnel. Acta Anaesthesiol Scand 2013;57:150–7. 10.1111/aas.12020 [DOI] [PubMed] [Google Scholar]
- 42. Niederhauser A, Züllig S, Marschall J, et al. Nurses' and physicians' perceptions of indwelling urinary catheter practices and culture in their institutions. J Patient Saf 2018. doi: 10.1097/PTS.0000000000000502. [Epub ahead of print: 29 May 2018]. [DOI] [PubMed] [Google Scholar]
- 43. Galiczewski JM, Shurpin KM. An intervention to improve the catheter associated urinary tract infection rate in a medical intensive care unit: direct observation of catheter insertion procedure. Intensive Crit Care Nurs 2017;40:26–34. 10.1016/j.iccn.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 44. Burke RE, Shojania KG. Rigorous evaluations of evolving interventions: can we have our cake and eat it too? BMJ Qual Saf 2018;27:254–7. 10.1136/bmjqs-2017-007554 [DOI] [PubMed] [Google Scholar]
- 45. Dykema J, Jones NR, Piché T, et al. Surveying clinicians by web: current issues in design and administration. Eval Health Prof 2013;36:352–81. 10.1177/0163278713496630 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-028740supp001.pdf (84.9KB, pdf)