Opportunity Statement:
Key topics discussed in this article were previously presented at the Center for AIDS Research Social and Behavioral Sciences Network's 12th National Scientific Meeting in August 2018. This article highlights the importance of behavioral and social sciences research (BSSR) in addressing the HIV/AIDS pandemic.
Approach:
NIH has made significant investments in HIV/AIDS-related BSSR. These investments support the development of effective, evidence-based sociobehavioral HIV prevention, treatment, and care strategies.
Discussion:
The implementation and use of evidence-based sociobehavioral approaches in combination with biomedical strategies provide the availability of multiple tools to end the HIV epidemic in the United Sates and the pandemic globally.
Future Directions:
BSSR-related opportunities to mitigate the persistent challenges HIV/AIDS presents include, but are not limited to, further incorporating BSSR into HIV vaccine and cure research; improving interventions that address stigma and the social determinants of health that perpetuate HIV transmission within key populations; and conducting implementation science research that shapes national and international policies impacting HIV prevention, treatment, and care.
Key Words: HIV/AIDS, behavioral, social, sociobehavioral, NIH
BACKGROUND
Dr. Maureen M. Goodenow, the Director of the National Institutes of Health's (NIH) Office of AIDS Research gave the keynote address at the 2018 Center for AIDS Research Social and Behavioral Sciences Research Network (SBSRN) meeting. She discussed NIH's investment in HIV/AIDS-related behavioral and social sciences research (BSSR).1 The Center for AIDS Research SBSRN meeting was an important platform for this discussion in view of the network's long-standing efforts and success in emphasizing, amplifying, and disseminating the role of BSSR in the fight against HIV/AIDS. In addition, the SBSRN has been successful at mentoring new and early career HIV/AIDS-related BSSR investigators. This article links key points discussed during the SBSRN meeting with relevant research endeavors and initiatives.
WHERE WE ARE TODAY
The NIH HIV/AIDS Research Program is comprehensive, spanning the major scientific areas delineated in the FY2019-FY2020 NIH Strategic Plan for HIV and HIV-Related Research.2 BSSR, one of the cross-cutting priorities within the NIH HIV/AIDS Research Program, was supported with $404 million or approximately 13% of the FY2018 NIH HIV/AIDS research investment. This investment supports BSSR-oriented centers, grants, and training awards issued by multiple NIH Institutes, Centers, and Offices.
This JAIDS supplement is published at a critical time in the HIV pandemic. Biomedically-oriented research continues to achieve exceptional advances in the form of antiretroviral medications that are highly effective for HIV prevention and treatment. BSSR provides effective strategies for HIV testing and counseling, behavioral risk reduction, and interventions for treatment adherence and retention that promote sustained viral suppression among people with HIV. Combinations of evidence-based sociobehavioral and biomedical strategies increase confidence that multiple tools to end the pandemic are available and that their use and scale-up can result in real impact. This represents an opportune time to reflect on the role that the behavioral and social sciences will play in this crucial endgame.
One framework that characterizes the vital contributions BSSR provides to the HIV/AIDS field is the Gaist and Stirratt3 BSSR Functional Framework. It conceptualizes BSSR through 4 domains:
Basic BSSR
Basic BSSR, which improves understanding of social and behavioral dynamics in key populations, identifies important intervention opportunities and targets, as well as informs strategies for the delivery of HIV prevention, treatment, sustained viral suppression, and care-related research and services.
Elemental BSSR
Elemental BSSR focuses on the development and testing of behavioral and social interventions that, alone or in combination with other strategies, can directly impact persons at risk of or with HIV across the prevention to cure continuum.
Supportive BSSR
Supportive BSSR aims to strengthen the conduct and outcomes of biomedically-oriented research testing the next generation of HIV prevention, treatment, and cure regimens.
Integrative BSSR
Integrative BSSR advances real-world implementation of proven combination and integrative strategies for HIV prevention, treatment, and cure through the best integrative approaches scaled up for public health and population level impact.
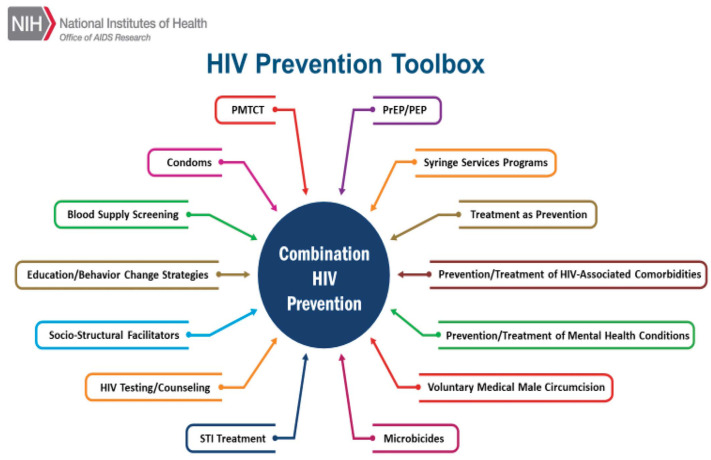
The BSSR Functional Framework provides a platform to emphasize scientific research that integrates multiple, cross-disciplinary approaches essential to continued progress in ending the HIV pandemic. BSSR is an essential component in that integration. For example, Figure 1 illustrates various prevention approaches that have been shown through research to be effective. Utilizing this “toolbox” is critical to advance the study of combination HIV prevention to insure broad and effective uptake, impact, and sustainability. Integrative BSSR approaches continue to fulfill an important role in assessing HIV prevention and care continuum gaps globally.
FIGURE 1.
Combination prevention toolbox for HIV.
The HIV pandemic is often impacted by concurrent conditions, such as depression and other mental health issues; alcohol, opioids, and other substance use disorders; tuberculosis and other infectious diseases, in particular human papillomavirus, hepatitis B, and hepatitis C. Syndemics, an aggregation of 2 or more epidemics or disease clusters in a population, contribute to an increased burden of disease with far-reaching effects and implications. The NIH HIV/AIDS Research Program continually promotes collaborations across Institutes, Centers, and Offices that address the syndemic nature of HIV.
LOOKING FORWARD—CHALLENGES THAT NEED BSSR-BASED SOLUTIONS
The integration of BSS (behavioral and social sciences), implementation science, and health services research to end the pandemic will require new partnerships across federal agencies, as well as with state and nongovernmental partners.
Given where we are and what is needed to eliminate HIV in the United States and globally, there are 8 key, interconnected initiatives:
-
Effectively engage those most at risk of HIV into the prevention continuum
○ This effort entails using BSSR approaches to further engage populations most affected by HIV into services that increase access to pre-exposure prophylaxis (PrEP) and other prevention approaches to decrease the rate of HIV transmission within these groups.4
-
Close the HIV care continuum gaps to achieve domestic and global HIV targets
○ BSSR methodologies are being used to better understand and address sociobehavioral barriers to testing and diagnosing HIV; linking and retaining people with HIV in care; and maintaining medication adherence and viral suppression among people with HIV. Findings from BSS-related research on the HIV care continuum promote meeting domestic and international targets to end the pandemic.
-
Incorporate BSSR into HIV vaccine and cure research
○ HIV vaccine and cure research require consideration of important behavioral and social processes that go beyond the domains of biomedicine. BSSR can serve a critical role in key areas such as study recruitment and retention; HIV medication treatment interruption; and understanding the life contexts of study participants involved in HIV vaccine and cure research.
-
Improve BSSR-informed biomedical product development
○ Trials dedicated to biomedical product research and development should incorporate BSS elements and methodologies into all phases of study designs. The integration of BSSR into research on potential biomedical HIV prevention and treatment products extends beyond assessing products' acceptability and feasibility among study participants.
-
Create tailored HIV interventions for key populations
○ It is evident that a one-size-fits-all approach cannot be used to successfully curtail HIV transmission. Culturally relevant and appropriate prevention and treatment interventions are needed to adequately address the unique needs of key populations disproportionately impacted by HIV/AIDS. BSSR is imperative to understand and eliminate the individual, interpersonal, community, societal, and structural factors that contribute to HIV/AIDS-related health disparities globally.
-
Address stigma and the social determinants that sustain HIV transmission and viral persistence
○ Stigma is a persistent barrier to the effectiveness of HIV prevention and treatment interventions. BSS approaches and strategies are needed to mitigate the barriers to HIV prevention and care associated with the drivers and facilitators of various types of stigma.
-
Improve HIV care and efficiency through differentiated care models
○ Differentiated care models are imperative to efficiently leverage resources for HIV prevention, treatment, and care, especially in resource-limited settings. BSSR and implementation science research (ISR) are critical to assess the HIV/AIDS-related needs of different populations with varying degrees of risk.
-
Conduct ISR at a scale that shapes policies and care guidelines
○ HIV-focused ISR is necessary to fully and effectively translate efficacious interventions into real-world clinical and service delivery settings. Endeavors focused on ending the HIV epidemic in the United States, as well as the pandemic globally, are reliant on the timely application of successful research findings at the population-level, especially in regions with high HIV incidence and prevalence.
BOLD STEPS FORWARD
The investments in HIV/AIDS-related research across science disciplines have produced effective HIV prevention and treatment medications as well as sociobehavioral and implementation science interventions. PrEP reduces the risk of sexual transmission of HIV by up to 99% when taken daily. Among people who inject drugs, PrEP reduces the risk HIV transmission by at least 74% when taken daily.5 With consistent use of HIV antiretroviral therapy (ART), individuals with HIV who attain an undetectable HIV viral load can live long, healthy lives and have effectively no risk of sexually transmitting HIV to a partner.6 International studies include Population Effects of ART to Reduce HIV Transmission, Sustainable East Africa Research in Community Health, and the Botswana Combination Prevention Project. These studies used BSS approaches within universal HIV testing and treatment models that promote HIV testing and counseling to entire populations; ART to all people with HIV; and, in some instances, PrEP to those at risk of acquiring HIV in these regions.7 These trials aimed to increase access to and uptake of biomedical products, while assessing behavioral, sociocultural, and sociostructural factors, such as how participants' potential experiences with gender inequality, poverty, and other vulnerabilities impact their level of risk and uptake.7
Recognizing the power that HIV prevention and treatment tools can have domestically, the President of the United States during his 2019 State of the Union Address announced a new initiative to end the HIV epidemic in the United States within the next 10 years.8 This initiative, Ending the HIV Epidemic: A Plan for America, is designed to leverage the tools in the geographic areas of the United States that account for more than 50% of new HIV infections annually. The initiative will bring these approaches together with what we have learned to date from BSSR and ISR to achieve its ambitious targets.8
Ending the HIV epidemic in the United States will require expanded cooperation among federal agencies, state health departments, community organizations, and communities throughout the designated areas with the highest incidence rates, as well as delivering the right sociobehavioral approaches at the right time for the right communities. Strategic cooperation and tailored approaches will be needed to successfully bring down the incidence of new HIV infections. For example, the approach in a well-resourced, politically willful, and experienced city like San Francisco will be different than the approach in a small town in the rural South. BSSR and ISR are well positioned to continue to address these dynamics effectively, recognizing that new, coordinated, and nimble interventions are required to effectively meet the needs of those most at risk and/or in need of care and treatment.
IN SUMMARY
To improve the lives of people affected by HIV/AIDS, new and more effective interventions are required that consider the full scope of biomedical, behavioral, and social challenges. NIH continues to invest in areas of research that support the development of an effective HIV vaccine and cure, as well as improve other HIV prevention and treatment interventions. BSSR is an integral and cross-cutting aspect of the HIV/AIDS research agenda. The translation and implementation of evidence-based interventions that use BSS strategies will continue to serve an integral role in ending the HIV pandemic.
ACKNOWLEDGMENTS
The authors acknowledge and thank Judith Auerbach, PhD; Dianne Rausch, PhD; and Amber Wilson, MPH for providing expert perspectives and suggestions to this article.
Footnotes
Topics discussed in this manuscript were presented at the Centers for AIDS Research Social and Behavioral Sciences Research Network's 12th National Scientific Meeting; August 10, 2018; Rockville, MD.
This publication resulted in part from research supported by the Penn Center for AIDS Research (CFAR) (P30 AI 045008 - Ronald Collman, PI), the Penn Mental Health AIDS Research Center (PMHARC) (P30 MH 097488 - Dwight Evans, PI) and the CFAR Social & Behavioral Science Research Network National Scientific Meeting (SBSRN) (R13 HD 074468 - Michael Blank, PI).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Recent Meeting. CFAR Social and Behavioral Sciences Research Network. Perelman School of Medicine University of Pennsylvania; Available at: https://www.med.upenn.edu/sbsrn/. [Google Scholar]
- 2.NIH Strategic Plan for HIV and HIV-Related Research. HIV Policy and Research. NIH Office of AIDS Research; 2018. Available at: https://www.oar.nih.gov/hiv-policy-and-research/strategic-plan. [Google Scholar]
- 3.Gaist P, Stirratt MJ. The roles of behavioral and social science research in the fight against HIV/AIDS: a functional framework. J Acquir Immune Defic Syndr. 2017;75:371–381. [DOI] [PubMed] [Google Scholar]
- 4.McNairy ML, El-Sadr WM. A paradigm shift: focus on the HIV prevention continuum. Clin Infect Dis. 2014;59:S12–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, https://www.cdc.gov/hiv/basics/prep.html, October 17, 2019. [Google Scholar]
- 6.Buchbinder SP. Maximizing the benefits of HIV preexposure prophylaxis. Top Antivir Med. 2018;25:138–142. [PMC free article] [PubMed] [Google Scholar]
- 7.Perriat D, Balzer L, Hayes R, et al. Comparative assessment of five trials of universal HIV testing and treatment in sub‐Saharan Africa. J Int AIDS Soc. 2018;21:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;32:844–845. [DOI] [PubMed] [Google Scholar]