OBJECTIVES:
Rates of surgery for nonmalignant colorectal polyps are increasing in the United States despite evidence that most polyps can be managed endoscopically. We aimed to determine nationally representative estimates and to identify predictors of in-hospital mortality and morbidity after surgery for nonmalignant colorectal polyps.
METHODS:
Data were analyzed from the National Inpatient Sample for 2005–2014. All discharges for adult patients undergoing surgery for nonmalignant colorectal polyps were identified. Rates of in-hospital mortality and postoperative wound, infectious, urinary, pulmonary, gastrointestinal, or cardiovascular adverse events were calculated. Multivariable logistic regression using survey-weighted data was used to evaluate covariables associated with postoperative mortality and morbidity.
RESULTS:
An estimated 262,843 surgeries for nonmalignant colorectal polyps were analyzed. In-hospital mortality was 0.8% [95% confidence interval: 0.7%–0.9%] and morbidity was 25.3% [95% confidence interval: 24.2%–26.4%]. Postoperative mortality was associated with open surgical technique (vs laparoscopic), older age, black race (vs non-Hispanic white), Medicaid use, and burden of comorbidities. Female sex and private insurance were associated with lower risk. Patients developing a postoperative adverse event had a 106% increase in mean hospital length of stay (10.3 vs 5.0 days; P < 0.0001) and 91% increase in mean hospitalization cost ($77,015.24 vs $40,258.30; P < 0.0001).
DISCUSSION:
Surgery for nonmalignant colorectal polyps is associated with almost 1% mortality and common morbidity. These findings should inform risk vs benefit discussions for clinicians and patients, and although confounding by patient selection cannot be excluded, the risks associated with surgery support consideration of endoscopic resection as a potentially less invasive therapeutic option.
INTRODUCTION
In the United States, more than 6 million screening colonoscopies are performed annually, and the detection and removal of colorectal polyps by endoscopic polypectomy has been associated with reduced long-term risks of colorectal cancer (CRC) incidence and related death (1–3). In approximately 4%–11% of colonoscopies, a large colorectal polyp (>20 mm) will be identified, most of which can be removed endoscopically (4). In expert hands, endoscopic resection of complex colorectal polyps has low complication rates and offers several advantages to surgery; polypectomy typically is an outpatient procedure, avoids abdominal incision, preserves bowel anatomy and function, is associated with fewer adverse events, is less costly, and does not preclude subsequent surgery should it be required (5–8).
Although most polyps can be removed endoscopically, partial colectomies are frequently performed for nonmalignant colorectal polyps in the United States. In an analysis of the National Inpatient Sample (NIS), Peery et al. (9) demonstrated a significant increase in the incidence of surgery for this indication between 2000 and 2014, from 5.9 to 9.4 surgeries per 100,000 adults. By contrast, rates of surgery for malignant CRC decreased during the same period, from 31.5 to 24.7 surgeries per 100,000 adults, whereas rates of colonoscopy performed for screening have remained stable. The reasons underlying the increased rates of surgery for nonmalignant colorectal polyps over time are unclear (10,11).
For patients, the decision to undergo surgery should be informed by an understanding of the risks and benefits associated with the available treatment options. Previous estimates of operative risks for resection of nonmalignant polyps have been primarily derived from case series, with postsurgical mortality estimated to range from 0.5% to 1.6% (12–15). More recently, Peery et al. used the National Surgical Quality Improvement Program (NSQIP) database to evaluate outcomes in 12,732 patients who underwent elective surgery for a nonmalignant colorectal polyp (8). The 30-day mortality rate after surgery was 0.7%, and the risk of a major postoperative adverse event was 14%. Although this study provided estimates from a large, prospectively collected database, these rates may not be generalizable to the US population as the NSQIP disproportionately samples tertiary care academic hospitals and encompasses a quality assurance program that may improve the outcomes (16).
To aid clinicians and patients in making informed treatment choices, we aimed to determine a more precise, nationally representative average estimate of postoperative mortality and morbidity after surgery for nonmalignant colorectal polyps and to identify factors associated with adverse outcomes.
METHODS
Study design and population
We performed a retrospective analysis of data collected from the Healthcare Cost and Utilization Project (HCUP) NIS Database for 2005–2014. The NIS is an all-payer administrative health database that captures information from more than 7 million inpatient admissions at over 1,000 hospitals across the United States annually. Weighted data yield national estimates for more than 35 million hospital admissions (17). Adult patients (≥18 years old) with a diagnosis of a colonic or an anorectal nonmalignant polyp (International Classification of Disease, Ninth Edition, Clinical Modification [ICD-9] CM codes 211.3 or 211.4) who underwent colectomy or proctectomy (17.3–17.39, 45.7–45.79, or 48.4–48.6) were identified. To minimize misclassification by surgical indication, patients with intestinal perforation, inflammatory bowel disease, diverticulitis, or CRC were excluded. Patients who underwent total abdominal colectomy were also excluded, which occurs more commonly in patients with familial adenomatous polyposis syndrome. Surgical procedures were categorized as either open or laparoscopic and by location of resection (left colonic, right colonic, other colonic, or rectal). These administrative codes have been previously used to evaluate temporal trends in surgical rates for nonmalignant colorectal polyps (9).
Outcome definitions
The primary outcome was in-hospital death after surgery. The secondary outcome was incidence of postoperative morbidity, defined as a composite of one or more of the following recorded adverse events: wound-related, infectious, urinary, pulmonary, gastrointestinal, cardiovascular, and intraoperative adverse events. Complete definitions of postoperative morbidity are summarized in Supplemental Table 1 (see Supplementary Digital Content, http://links.lww.com/AJG/B290).
Statistical analysis
The NIS uses a stratified sampling design: to produce national figures, survey weights provided by the HCUP were applied to generate discharge-level estimates. In 2012, the NIS sampling strategy was redesigned. Therefore, revised survey trend weights for 2005–2011 were applied to make estimates comparable with the survey design for 2012–2014. Patient demographics and hospital characteristics are presented using descriptive statistics. Rates of postoperative in-hospital mortality and morbidity were calculated and expressed as proportions and per 1,000 surgeries. Multivariable logistic regression modeling was performed to evaluate predictors of adverse postoperative outcomes. Covariables were chosen a priori, and it included age, sex, race, primary method of payment, Charlson Comorbidity Index (18) (CCI 0, 1, ≥2) (19), open vs laparoscopic surgical technique, hospital type (rural vs urban [>10,000 residents], teaching vs nonteaching; teaching hospitals were defined by having an Accreditation Council for Graduate Medical Education-approved residency program, being a member of the Council of Teaching Hospitals, or having a ratio of interns/residents to beds of ≥0.25), hospital region, and by hospital colectomy volume (<10 colectomies/yr, 10–49 colectomies/yr, and ≥50 colectomies/yr). Effect sizes are expressed as adjusted odds ratios with 95% confidence intervals (CIs). Mean length of stay (LOS) and total hospitalization costs (expressed in US $) were compared between patients with and without postoperative adverse events using an adjusted Wald test. Time trend analyses on mortality and morbidity rates were performed by calculating the annual percent change (APC) using a generalized linear model assuming a Poisson distribution. Joinpoint regression was used to assess for significant inflection points in temporal trends.
All analyses were performed using STATA 14.2 (College Station, TX) and Joinpoint Regression Program 4.6 (Statistical Research and Applications Branch, National Cancer Institute). The Kaiser Foundation Research Institute determined this study to be exempt from continuing review given the use of de-identified data.
RESULTS
Patient demographics
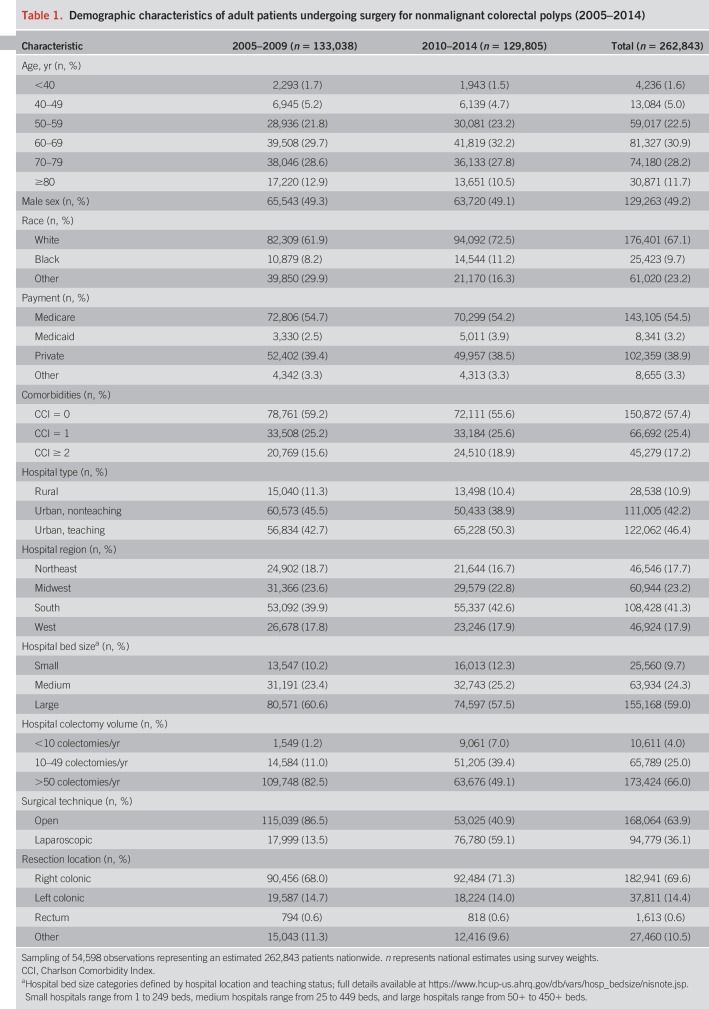
A total of 54,598 discharges for patients undergoing surgery for nonmalignant colorectal polyps were identified, representing an estimated 262,843 discharges nationally between 2005 and 2014. Cohort identification is summarized in Figure 1, and patient baseline demographic characteristics are described in Table 1. Approximately 40% of patients undergoing surgery were older than 70 years, and more than one-third of patients had concurrent comorbidities as defined by the CCI. The incidence of laparoscopic resections increased during the study period from 13.5% in 2005–2009 to 59.1% in 2010–2014.
Figure 1.
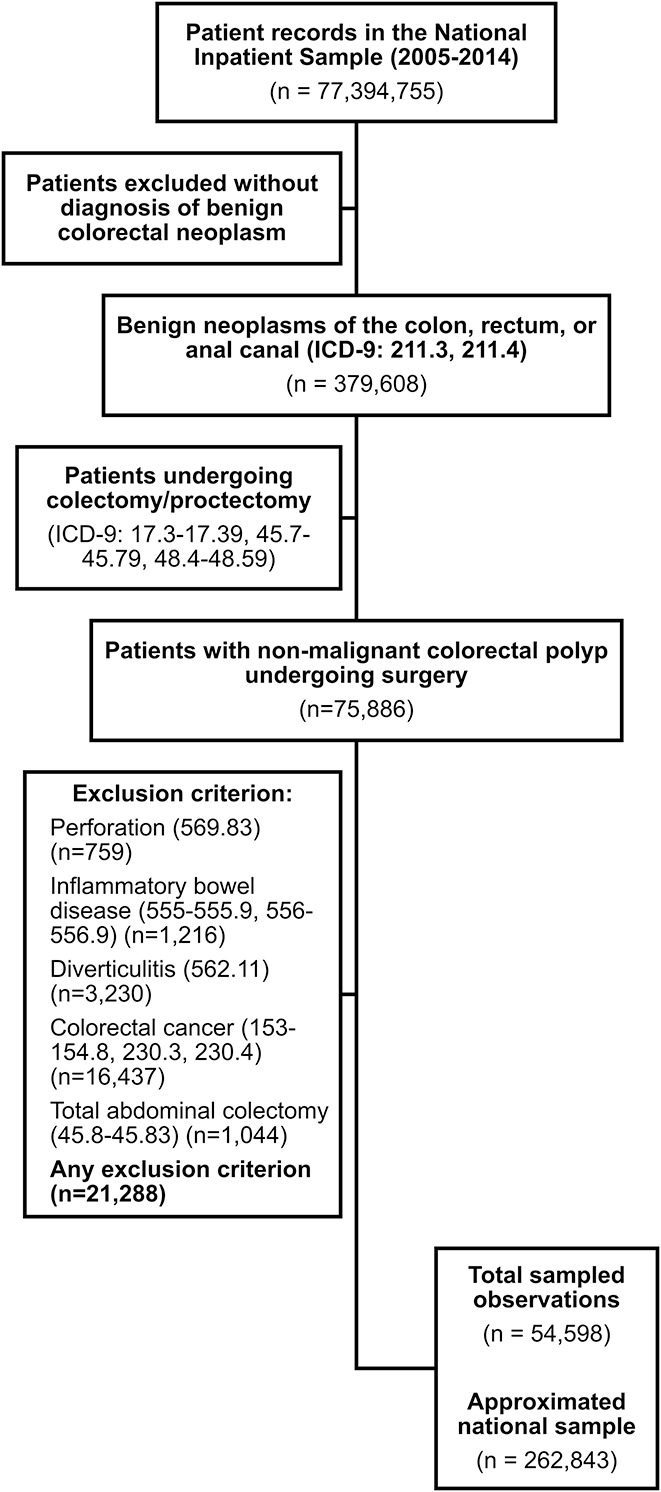
Patient identification flowchart. ICD-9, International Classification of Disease, Ninth Edition.
Table 1.
Demographic characteristics of adult patients undergoing surgery for nonmalignant colorectal polyps (2005–2014)
Rate of in-hospital mortality and morbidity
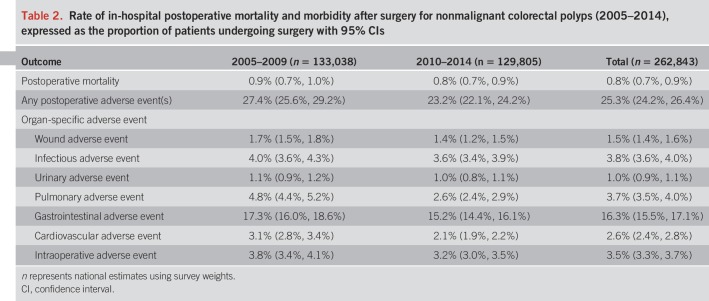
Adjusted rates of in-hospital mortality and morbidity are summarized in Table 2. The overall risk of postoperative in-hospital death was 0.8% [95% CI: 0.7%, 0.9%]. The risk of in-hospital mortality in patients undergoing open surgery was 1.1% [95% CI: 1.0%, 1.2%] compared with 0.4% [95% CI: 0.3%, 0.5%] in patients undergoing laparoscopic surgery. The risk of in-hospital death increased with age: the estimated risk was 0.2% [95% CI: 0.2%, 0.3%] in patients aged 50–59 years, 0.6% [95% CI: 0.4%, 0.7%] in patients aged 60–69 years, 1.0% [95% CI: 0.9%, 1.2%] in patients aged 70–79 years, and 2.5% [95% CI: 2.1%, 2.9%] in patients aged ≥80 years.
Table 2.
Rate of in-hospital postoperative mortality and morbidity after surgery for nonmalignant colorectal polyps (2005–2014), expressed as the proportion of patients undergoing surgery with 95% CIs
A total of 25.3% [95% CI: 24.2%, 26.4%] of patients undergoing surgery experienced an in-hospital postoperative adverse event. The most common postoperative adverse event was gastrointestinal (16.3% [95% CI: 15.5%, 17.1%]). The risk of postoperative morbidity was highest among patients undergoing open surgery (28.6% [95% CI: 27.2%, 30.0%]) than among those undergoing laparoscopic surgery (19.5% [95% CI: 18.4%, 20.6%] and among patients with multiple medical comorbidities (34.9% [95% CI: 33.2%, 36.6%]). Stratified mortality and morbidity rates by age, sex, race, payment, comorbidities, hospital type, hospital region and division, and hospital colectomy volume are summarized in Supplemental Table 2 (see Supplementary Digital Content, http://links.lww.com/AJG/B290).
Time trends in postoperative morbidity and mortality
On time trend analysis, the rate of postoperative mortality remained stable (APC: −3.8% [95% CI: −7.5%, +0.1%]; P = 0.08). By contrast, the proportion of patients experiencing a postoperative adverse event decreased significantly (APC: −3.3% [95% CI: −5.1%, −1.5%]; P = 0.002) (Figure 2). On joinpoint regression, a statistically significant change in trend for postoperative morbidity occurred in 2008: before 2008, the rate of postoperative adverse events was stable (APC: +2.7% [95% CI: −3.2%, +8.9%]; P = 0.31). After 2008, the rate of postoperative adverse events decreased significantly (APC: −6.1% [95% CI: −8.2%, −4.0%]; P = 0.001).
Figure 2.
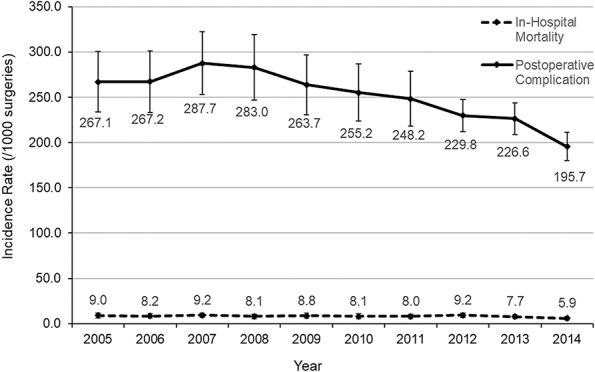
Incidence of in-hospital mortality and postoperative adverse events after surgery for nonmalignant colorectal polyps over time (2005–2014).
Predictors of postoperative mortality and morbidity
Increasing age, male sex, black race, open surgical technique, and the presence of comorbidities increased the risk of postoperative mortality (Table 3). The CCI was the strongest predictor of in-hospital death: patients with ≥2 comorbidities had a 5.6-fold increased risk of postoperative mortality compared with patients without comorbidities. Open surgical technique (compared with laparoscopic surgery) and older age (per decade) were associated with an approximately 2- to 3-fold increased risk of in-hospital death, and female individuals had half the risk of death compared with male individuals. Patients on Medicaid had a 2.6-fold increased risk of in-hospital mortality compared with patients on Medicare.
Table 3.
Factors associated with in-hospital postoperative mortality and morbidity, expressed as aOR with 95% CIs
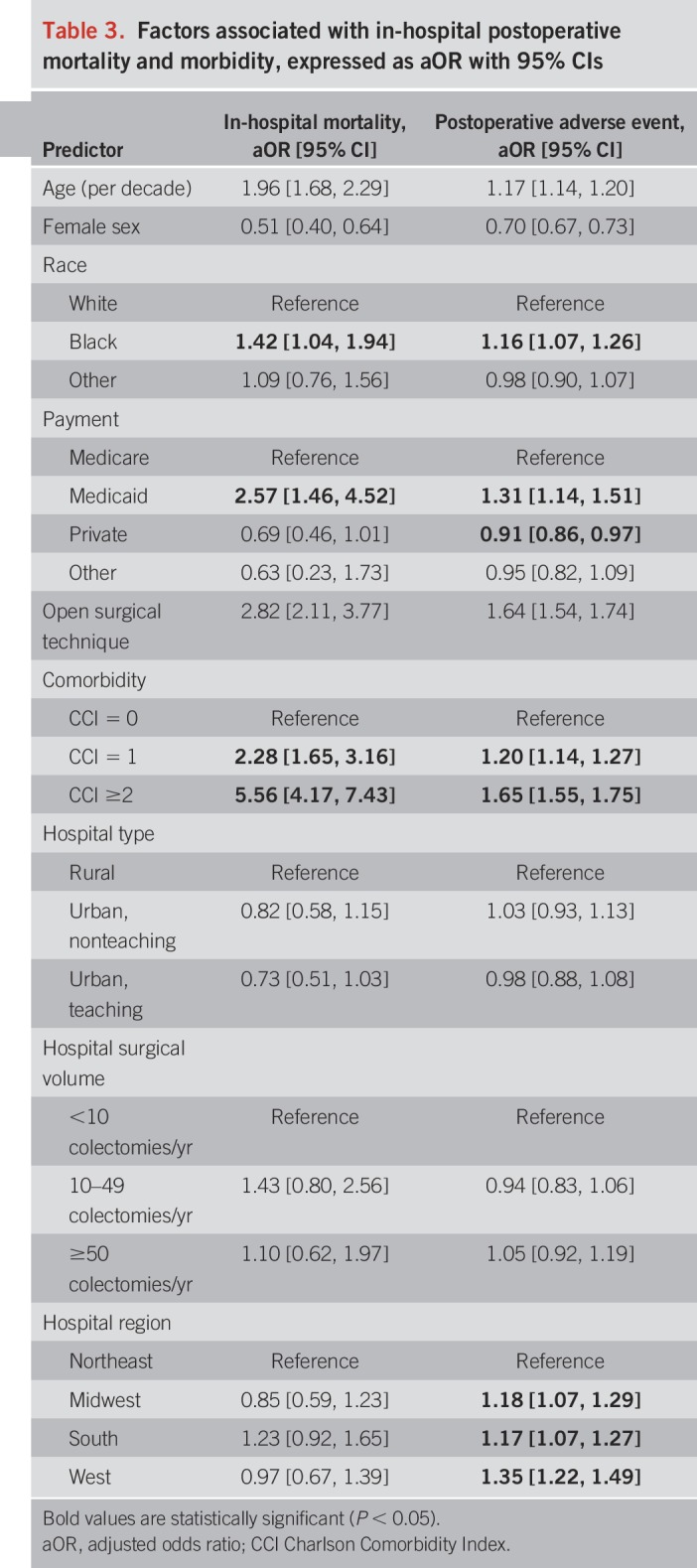
The risk of postoperative morbidity was also associated with increasing age, male sex, black race, open surgical technique, and the presence of comorbidities (Table 3). Patients undergoing laparotomy had a 61% increased risk of postoperative morbidity compared with patients undergoing laparoscopic surgery. Medicaid coverage was associated with a 31% increased risk of postoperative adverse events, whereas private insurance was associated with an 11% reduction in postoperative morbidity compared with Medicare. Regional differences in postoperative morbidity were also observed: when stratified by census division, patients undergoing surgery in New England (22.9% [95% CI: 20.8%, 25.1%]) or Mid-Atlantic (22.5% [95% CI: 21.3%, 23.8%]) states had the lowest risk of postoperative adverse event (see Table 2, Supplementary Digital Content, http://links.lww.com/AJG/B290).
Impact on hospital LOS and cost
Mean LOS for patients undergoing surgery for a nonmalignant colorectal polyp was 6.3 days (SE: 0.03 days), and mean cost of hospitalization was $49,566.48 (SE: $591.90). In-hospital mortality resulted in a 134% increase in mean LOS (14.6 vs 6.2 days; P < 0.0001) and 234% increase in mean total hospitalization cost ($162,487.20 vs $48,613.18; P < 0.0001). In-hospital morbidity resulted in a 106% increase in mean LOS (10.3 vs 5.0 days; P < 0.0001) and 91% increase in mean total hospitalization cost ($77,015.24 vs $40,258.30; P < 0.0001).
DISCUSSION
Surgical referral for patients with nonmalignant polyps remains a common practice, and the incidence of surgery is rising (9,13,21,22). In this study, we analyzed more than 260,000 surgeries for nonmalignant colorectal polyps in a large US database over a 10-year period. Sampling from all geographic regions in the United States, capturing both small and large surgical volume hospitals, and including patients with all-payer coverage, we determined that nationally, approximately 1 in 4 patients will experience a postoperative adverse event and 1 in 125 patients will die in the hospital after surgery. Furthermore, a complicated postoperative course is associated with intensive resource utilization and the high risk of mortality and morbidity after surgery is notable when a safer endoscopic option exists.
Our primary objective was to determine generalizable, unbiased, national-level estimates of postoperative mortality and morbidity. Hence, we used the NIS to capture a wide breadth of discharges (>35 million weighted discharges annually), drawing from all states participating in the HCUP, representing >97% of the US population. However, because discharge-level rather than patient- or surgeon-level data were collected, the primary limitation of this study is that detailed polyp (histology, morphology, size), colonoscopy (operator, timing, attempted endoscopic resection), and healthcare provider (surgeon experience, gastroenterologist availability) data are not available. These factors may result in selection bias for cohort studies: for example, in areas with minimal access to endoscopic resection, older patients with multiple comorbidities at higher risk for postoperative mortality may still opt to undergo surgery. Alternatively, tertiary care centers may see a higher referral volume of complex cases that are predisposed to greater postoperative risk. Therefore, although we present national-level estimates, regional mortality and morbidity may vary.
We have attempted to mitigate the influence of these factors in several ways. First, although these confounders may be an important source of selection bias in smaller cohorts, their effects on large, population-based, national-level estimates are likely diluted when considering all discharges across all geographic areas. Second, we have included several surrogate measures of these confounders in our analyses, including hospital colectomy volume, teaching hospital status, urban vs rural location, and hospital region. Third, although specific polyp characteristics are important to consider for endoscopic resectability, their impact on colectomy-related outcomes is unclear. It is probable that some polyp features, for example, tubular vs villous vs serrated histology, are unlikely to affect surgical mortality as we have selected nonmalignant, noninvasive polyps.
Previously, Peery et al. (8) reported a 14% risk of at least one major postoperative adverse event, a 7.8% risk of readmission within 30 days, a 3.6% risk of a second major operation, and a 0.7% risk of 30-day mortality using data from the NSQIP database. Although in-hospital mortality rates (0.8%) were similar to those previously reported, we found a substantially higher risk of postoperative morbidity (25% vs 14%). Differences in the risk of postoperative adverse events are likely multifactorial. Research using the NSQIP database may underestimate adverse events due to the quality improvement focus of the program, overrepresentation of academic tertiary care centers, or methodological heterogeneity in adverse event definitions. Although the NSQIP database has advantages for defining preoperative patient comorbidities and prospective collection of postoperative outcomes, the NIS database does not rely on volunteer participation and captures all types of hospitals, payers, and locations. Therefore, our mortality and morbidity estimates are more generalizable, particularly in non-NSQIP participating US institutions. In cohort-based studies, similarly high risks of postoperative adverse events have also been reported at 20%–30%, although these estimates are limited by sample size considerations (14,23).
Comparatively, the most common complications associated with endoscopic resection include bleeding and perforation. Intraprocedural and delayed bleeding affect approximately 11% and 6% of polypectomies, respectively (24,25). In meta-analysis, the pooled risk of perforation after large polypectomies is approximately 1.5%, and mortality directly attributable to endoscopy or subsequent surgery after endoscopy is rare (0.08%) (26). Given the lower reported rates of complications associated with endoscopic resection, our study provides additional support for clinical practice recommendations that all polyps should be considered for attempted endoscopic resection before referral for surgery (27,28). Nevertheless, we recognize that there may be circumstances in which surgery is the preferred treatment option for some individual patients. For example, surgery is indicated to manage lesions unsuitable for or after a failed endoscopic resection. Nonlifting lesions and polyps with signs of invasive cancer should undergo surgical resection (5). The absolute incidence of these polyps is low. In meta-analysis, only 8.1% of patients with polyps ≥20 mm (predominantly laterally spreading sessile lesions) required surgery (26). Furthermore, most polyps initially deemed unsuitable for endoscopic resection can be removed when evaluated by an expert endoscopist: Voloyiannis et al. identified that nearly 60% of patients avoided surgical resection when repeat colonoscopy with polypectomy was performed, and similarly, Friedland et al. identified that 71% of lesions referred for surgery were actually amenable to endoscopic resection (29,30).
Surgery may also be required to treat serious adverse events after polypectomy (5). In this respect, there may be differences in referral patterns and case selection for nonmalignant polyps based on whether a gastroenterologist or surgeon performed the index procedure. Surgeons have ready recourse to resection in difficult or complicated cases and in patients harboring a covert cancer, whereas gastroenterologists may be more circumspect regarding lesion evaluation and endoscopic resection. Although these factors are unlikely to significantly impact national-level estimates of postoperative morbidity and mortality, they do highlight that regional differences in practice pattern are observed; correspondingly, we identified geographic disparities in postoperative morbidity. Finally, polypectomy performed in a large center of endoscopic excellence is not available in all jurisdictions: in these cases, patients may choose a local surgical approach rather than remote endoscopic service.
We demonstrated both patient- and system-related differences in the risk of postoperative mortality and morbidity after surgery for a nonmalignant colorectal polyp. Unsurprisingly, elderly patients with advanced comorbidities were at highest risk. In multivariable analysis, male and black patients were more likely to experience adverse outcomes; although this may relate to presentation with more advanced disease compared with female, non-black patients, as is observed with CRC, this requires additional investigation (31,32). Furthermore, although we adjusted for CCI burden on multivariable analysis, residual confounding with respect to comorbidities in male, black patients may persist. Patients on Medicaid and undergoing open laparotomy were also at higher risk for postsurgical adverse events. Given the more than 2-fold increased risk of mortality associated with open surgery, this study provides supporting evidence to exhaust laparoscopic options (33,34). Additionally, although surgery for a nonmalignant polyp may be considered less intensive compared with colectomy for inflammatory or malignant indications, the protective effect seen with laparoscopic surgery suggests that this remains a complex operation that may benefit from centralization of care in expert centers capable of performing minimally invasive procedures (35,36). In our study, a significant decrease in the rate of postoperative adverse events was observed. This is likely multifactorial and may relate to improvements in surgical techniques, decreased invasiveness of surgical procedures, optimized patient selection, national efforts to concentrate select surgical procedures in high-volume centers, surgical quality improvement initiatives, and improved perioperative and postoperative care pathways (37–41).
Importantly, our study highlights the intensive resource utilization associated with a complicated postoperative course after surgery for nonmalignant colorectal polyps. Previous estimates of surgical cost for nonmalignant colorectal polyps range from approximately $16,000 to $19,000 per patient (7,42). These figures underestimate the costs associated with managing postoperative morbidity; in our analysis, patients with a complicated postsurgical course had approximately twice the LOS and the mean total cost of hospitalization exceeded $75,000. In the current era where healthcare expenditures are rising, treatment options that have comparable effectiveness and yet are safer and more cost effective should be considered.
Our study has some important limitations. First, administrative coding errors may introduce a source of misclassification bias. We used codes similar to those used in previous studies to identify surgery for nonmalignant colorectal polyps (9), and postoperative adverse events after colectomy have been validated in an ulcerative colitis population (43). As many jurisdictions in the United States transition to ICD-10 coding, diagnostic, procedural, and postprocedure complication coding should be prospectively validated to ensure accurate case ascertainment. Second, the NIS does not stratify postoperative adverse events by severity (e.g., by the Clavien-Dindo Classification) and does not contain polyp information such as size, histology, and previous attempts at endoscopic resection. Third, postoperative adverse events were presented by body system because ICD-9 administrative coding lacks the granularity to distinguish specific adverse events. Because there are no specific preadmission comorbidity vs postoperative complication diagnostic markers in the NIS, we have used postprocedure ICD-9 codes to maximize the specificity of our outcome definition (see Table 1, Supplementary Digital Content, http://links.lww.com/AJG/B290). This does not allow for more detailed characterization of complications, although it does minimize misclassification bias. Fourth, the level of analysis in the NIS is based on discharges, rather than individual patients limiting the ability to follow patients for adverse events occurring after the index hospitalization or determine their preoperative course with respect to colonoscopy and attempts at endoscopic resection. Finally, the NIS does not capture procedures occurring in ambulatory hospitals and surgical procedures with a same-day discharge. However, it is unlikely that a substantial number of colectomies are performed in ambulatory surgical centers in the United States and also have same-day discharges.
In conclusion, in this analysis of the NIS from 2005 to 2014, we found that the overall nationwide mortality rate after surgical resection for nonmalignant colorectal polyps was 0.8%, with an overall postoperative morbidity rate of 25.3%. These results will inform gastroenterologists, surgeons, and primary care physicians when having risk-benefit discussions on treatment options for nonmalignant colorectal polyps. Given that published data on endoscopic resection of large polyps is likely safer and more cost effective than surgery, patients with advanced nonmalignant polyp(s) should be considered for referral to an expert for potential endoscopic management, with surgery being reserved for patients in whom endoscopic resection is deemed unfeasible or has failed.
CONFLICTS OF INTEREST
Guarantor of the article: Jeffrey K. Lee, MD, MPH, MAS.
Specific author contributions: C.M. and A.T. contributed equally to this work. C.M., A.T., J.K.L.: study concept and design, data analysis, data interpretation, and manuscript drafting and editing for important intellectual content. S.S.: manuscript drafting and editing for important intellectual content. N.F., S.J.H., T.L.J., C.A.M., V.J., D.A.C.: manuscript editing for important intellectual content. All authors approve the final version of this study.
Financial support: C.M. is supported by a Clinician Fellowship from the Canadian Institutes for Health Research, Crohn's and Colitis Canada, and the Canadian Association of Gastroenterology. J.K.L. is supported by a career development grant (K07 CA212057) from the National Cancer Institute and American Gastroenterological Association Research Scholar Award. D.A.C. is supported by a National Cancer Institute grant (UM1 CA222035).
Potential competing interests: C.M., A.T., S.S. have no relevant conflicts of interest. N.F. has received research support and speaker's honoraria from Pentax and Boston Scientific. S.J.H., T.L.J., C.A.M., V.J., D.A.C., J.K.L. have no relevant conflicts of interest.
Study Highlights.
WHAT IS KNOWN
✓ Screening and endoscopic polypectomy reduce the incidence of and mortality from CRC.
✓ Most large or complex colorectal polyps can be safely removed by endoscopic resection.
✓ Although endoscopic resection is the preferred first-line modality of treatment, surgery for nonmalignant colorectal polyps may be required and the rates are increasing in the United States.
WHAT IS NEW HERE
✓ In a 10-year analysis of more than 260,000 surgeries for nonmalignant colorectal polyps using a nationally representative sample (NIS), we determined that 0.8% of patients will die in the hospital. Moreover, 25.3% of patients will experience a postoperative adverse event, which is higher than that previously reported in a large quality assurance surgical cohort.
✓ Surgery-, patient-, and system-related factors that increase the risk of adverse postoperative outcomes include open laparotomy, older age, male sex, burden of comorbidities, black race, Medicaid use, and admission to a rural hospital.
✓ Surgery for nonmalignant colorectal polyps is associated with significant resource use and morbidity. Given published safety and effectiveness data on endoscopic resection of large nonmalignant polyps, patients with such polyps should have an evaluation for the appropriateness of endoscopic resection.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/AJG/B290
REFERENCES
- 1.Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 2013;369:1095–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levin TR, Corley DA, Jensen CD, et al. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology 2018;155:1383–91 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joseph DA, Meester RG, Zauber AG, et al. Colorectal cancer screening: Estimated future colonoscopy need and current volume and capacity. Cancer 2016;122:2479–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heitman SJ, Tate DJ, Bourke MJ. Optimizing resection of large colorectal polyps. Curr Treat Options Gastroenterol 2017;15:213–29. [DOI] [PubMed] [Google Scholar]
- 6.Rao AK, Soetikno R, Raju GS, et al. Large sessile serrated polyps can Be safely and effectively removed by endoscopic mucosal resection. Clin Gastroenterol Hepatol 2016;14:568–74. [DOI] [PubMed] [Google Scholar]
- 7.Law R, Das A, Gregory D, et al. Endoscopic resection is cost-effective compared with laparoscopic resection in the management of complex colon polyps: An economic analysis. Gastrointest Endosc 2016;83:1248–57. [DOI] [PubMed] [Google Scholar]
- 8.Peery AF, Shaheen NJ, Cools KS, et al. Morbidity and mortality after surgery for nonmalignant colorectal polyps. Gastrointest Endosc 2018;87:243–50 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peery AF, Cools KS, Strassle PD, et al. Increasing rates of surgery for patients with nonmalignant colorectal polyps in the United States. Gastroenterology 2018;154:1352–60 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swan MP, Bourke MJ, Alexander S, et al. Large refractory colonic polyps: Is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc 2009;70:1128–36. [DOI] [PubMed] [Google Scholar]
- 11.Holt BA, Bourke MJ. Wide field endoscopic resection for advanced colonic mucosal neoplasia: Current status and future directions. Clin Gastroenterol Hepatol 2012;10:969–79. [DOI] [PubMed] [Google Scholar]
- 12.Ahlenstiel G, Hourigan LF, Brown G, et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc 2014;80:668–76. [DOI] [PubMed] [Google Scholar]
- 13.Le Roy F, Manfredi S, Hamonic S, et al. Frequency of and risk factors for the surgical resection of nonmalignant colorectal polyps: A population-based study. Endoscopy 2016;48:263–70. [DOI] [PubMed] [Google Scholar]
- 14.Ikard RW, Snyder RA, Roumie CL. Postoperative morbidity and mortality among Veterans Health Administration patients undergoing surgical resection for large bowel polyps (bowel resection for polyps). Dig Surg 2013;30:394–400. [DOI] [PubMed] [Google Scholar]
- 15.Keswani RN, Law R, Ciolino JD, et al. Adverse events after surgery for nonmalignant colon polyps are common and associated with increased length of stay and costs. Gastrointest Endosc 2016;84:296–303 e1. [DOI] [PubMed] [Google Scholar]
- 16.Alluri RK, Leland H, Heckmann N. Surgical research using national databases. Ann Transl Med 2016;4:393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the national inpatient sample. JAMA 2017;318:2011–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- 19.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–9. [DOI] [PubMed] [Google Scholar]
- 20.Gorgun E, Benlice C, Church JM. Does cancer risk in colonic polyps unsuitable for polypectomy support the need for advanced endoscopic resections?. J Am Coll Surg 2016;223:478–84. [DOI] [PubMed] [Google Scholar]
- 21.Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31–53. [DOI] [PubMed] [Google Scholar]
- 22.Bronzwaer MES, Koens L, Bemelman WA, et al. Volume of surgery for benign colorectal polyps in the last 11 years. Gastrointest Endosc 2018;87:552–61 e1. [DOI] [PubMed] [Google Scholar]
- 23.McNicol L, Story DA, Leslie K, et al. Postoperative complications and mortality in older patients having non-cardiac surgery at three Melbourne teaching hospitals. Med J Aust 2007;186:447–52. [DOI] [PubMed] [Google Scholar]
- 24.Burgess NG, Metz AJ, Williams SJ, et al. Risk factors for intraprocedural and clinically significant delayed bleeding after wide-field endoscopic mucosal resection of large colonic lesions. Clin Gastroenterol Hepatol 2014;12:651–61 e1-3. [DOI] [PubMed] [Google Scholar]
- 25.Ma MX, Bourke MJ. Complications of endoscopic polypectomy, endoscopic mucosal resection and endoscopic submucosal dissection in the colon. Best Pract Res Clin Gastroenterol 2016;30:749–67. [DOI] [PubMed] [Google Scholar]
- 26.Hassan C, Repici A, Sharma P, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: A systematic review and meta-analysis. Gut 2016;65:806–20. [DOI] [PubMed] [Google Scholar]
- 27.Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2017;49:270–97. [DOI] [PubMed] [Google Scholar]
- 28.Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015;47:829–54. [DOI] [PubMed] [Google Scholar]
- 29.Friedland S, Banerjee S, Kochar R, et al. Outcomes of repeat colonoscopy in patients with polyps referred for surgery without biopsy-proven cancer. Gastrointest Endosc 2014;79:101–7. [DOI] [PubMed] [Google Scholar]
- 30.Voloyiannis T, Snyder MJ, Bailey RR, et al. Management of the difficult colon polyp referred for resection: Resect or rescope? Dis Colon Rectum 2008;51:292–5. [DOI] [PubMed] [Google Scholar]
- 31.Williams R, White P, Nieto J, et al. Colorectal cancer in African Americans: An update. Clin Transl Gastroenterol 2016;7:e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen SP, Bent S, Chen YH, et al. Gender as a risk factor for advanced neoplasia and colorectal cancer: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2009;7:676–81 e1–3. [DOI] [PubMed] [Google Scholar]
- 33.Lacy AM, García-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: A randomised trial. Lancet 2002;359:2224–9. [DOI] [PubMed] [Google Scholar]
- 34.Zheng Z, Jemal A, Lin CC, et al. Comparative effectiveness of laparoscopy vs open colectomy among nonmetastatic colon cancer patients: An analysis using the national cancer data base. J Natl Cancer Inst 2015;107:dju491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaplan GG, McCarthy EP, Ayanian JZ, et al. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology 2008;134:680–7. [DOI] [PubMed] [Google Scholar]
- 36.Morris EJ, Taylor EF, Thomas JD, et al. Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut 2011;60:806–13. [DOI] [PubMed] [Google Scholar]
- 37.Fry BT, Smith ME, Thumma JR, et al. Ten-year trends in surgical mortality, complications, and failure to rescue in Medicare beneficiaries. Ann Surg 2019. [Epub ahead of print January 23, 2019.] [DOI] [PubMed] [Google Scholar]
- 38.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 2011;364:2128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fuchshuber PR, Greif W, Tidwell CR, et al. The power of the National Surgical Quality Improvement Program—achieving a zero pneumonia rate in general surgery patients. Perm J 2012;16:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han-Geurts IJ, Hop WC, Kok NF, et al. Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. Br J Surg 2007;94:555–61. [DOI] [PubMed] [Google Scholar]
- 41.Boelens PG, Heesakkers FF, Luyer MD, et al. Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: Prospective, randomized, controlled trial. Ann Surg 2014;259:649–55. [DOI] [PubMed] [Google Scholar]
- 42.Jayanna M, Burgess NG, Singh R, et al. Cost analysis of endoscopic mucosal resection vs surgery for large laterally spreading colorectal lesions. Clin Gastroenterol Hepatol 2016;14:271–8 e1-2. [DOI] [PubMed] [Google Scholar]
- 43.Ma C, Crespin M, Proulx MC, et al. Postoperative complications following colectomy for ulcerative colitis: A validation study. BMC Gastroenterol 2012;12:39. [DOI] [PMC free article] [PubMed] [Google Scholar]