Abstract
Background
With the development of assisted reproductive technology (ART) and its increasing success rate in the mainland of China, more attention has been paid to the safety of ART. In this study, we explored the associations between conception by ART and pregnancy/perinatal complications, and neonatal outcomes compared with similar outcomes following spontaneous conception.
Methods
This retrospective cohort study of pregnancies over a 3-year period (2013–2015) was performed at Beijing Obstetrics and Gynecology Hospital, Beijing, China. Subjects were divided into two groups: conception by ART (n = 2256) or spontaneous conception (n = 6768). According to different fertilization modes, the ART group was divided into in vitro fertilization (IVF, n = 1873) and intracytoplasmic sperm injection (ICSI, n = 383) subgroups. The ART group was also divided into two different embryo transfer methods; fresh embryo transfer (ET, n = 1583) and frozen embryo transfer (FET, n = 673) subgroups. Pregnancy complications, perinatal complications, and neonatal outcomes of the enrolled subjects were investigated and analyzed by univariate analysis and multivariate logistic regression.
Results
After adjustment for maternal age, gravidity, parity, maternal education, smoking, alcohol consumption, and body mass index (BMI), pregnancies conceived by ART were associated with a significantly increased incidence of gestational diabetes mellitus (GDM; OR 1.88, 95% CI 1.56–2.27), gestational hypertension (OR 2.18, 95% CI 1.83–2.60), and intrahepatic cholestasis of pregnancy (ICP) (OR 2.79, 95% CI 2.15–3.64), compared with spontaneous conception. These associations were similar for the singleton group. In the twin group, only the incidence of ICP was significantly higher than in controls. We found that pregnancies conceived by ART were associated with perinatal complications, including placental abruption (OR 2.14, 95% CI 1.33–3.45), premature rupture of membranes (PROM; OR 1.24, 95% CI 1.06–1.45), postpartum hemorrhage (OR 2.89, 95% CI 2.33–3.59) and polyhydramnios (OR 2.01, 95% CI 1.29–3.16). The singleton group had a similar result with placental abruption, but not with fetal membranes ruptures before labor and polyhydramnios. There were no significant differences in the incidence of these perinatal complications in the twin group. Some neonatal outcomes, including preterm labor (OR 4.29, 95% CI 3.84–4.80) and low birth weight (OR 1.72, 95% CI 1.42–2.08), were more likely to occur with singleton births after ART. However, there were no significant differences for these outcomes from twin pregnancies. Perinatal complications and neonatal outcomes were consistent between the IVF and ICSI subgroups. The FET and ET subgroups showed a similar increase in complications, except for the incidence of placental abruption. After taking into account the effects of parity, birth plurality and maternal age, the ART group still exhibited increased maternal and neonatal complications, although some differences narrowed or disappeared.
Conclusions
This retrospective cohort study demonstrated that patients who underwent ART were at increased risk of several adverse pregnancy outcomes compared with women who conceived spontaneously. These complications may be attributed in part to the relatively high multiple pregnancy rate after ART. Elective single embryo transfer should be promoted in China to reduce the obstetrical risks of ART pregnancy. Singletons of ART pregnancy exhibited increased maternal and neonatal complications as well, suggesting that underlying infertility or other maternal or parental factors may contribute to the adverse outcomes.
Keywords: Reproductive techniques, Assisted; fertilization in vitro; Sperm injections, Intracytoplasmic; Pregnancy complications
Introduction
Since the birth of Louise Brown in 1978, in vitro fertilization (IVF) has become an effective way to treat infertility and has produced millions of babies worldwide. The number of assisted reproductive technology (ART) births per year has increased worldwide, with the total number of IVFs approximately 5 million. IVF accounts for 1.7% to 4% of the total population in developing countries, and 1% of the Chinese population.[1–2] However, ART allows multiple eggs to mature simultaneously via controlled ovarian hyperstimulation, and fertilization and early embryo development are accomplished by in vitro culture and micromanipulation. These techniques interfere with the process of germ cell proliferation, fertilization, development, and differentiation and may have adverse effects on the embryo. More attention has been paid to the safety of ART worldwide.
Several studies have shown that ART increases the incidence of adverse pregnancy outcomes, including preeclampsia, gestational hypertension, placenta previa, gestational diabetes mellitus (GDM), preterm delivery, low birth weight, and birth defects.[3–8] Birth plurality is a post-treatment confounder; a variable that occurs after ART treatment that confounds the causal effect. Many studies have not examined mother's age and other mixed miscellaneous factors.[9–12] Does ART increase adverse pregnancy outcomes? Is the adverse pregnancy outcome due to multiple births or the ART technology itself? At present, opinions vary widely, and no unanimous conclusion can be drawn.
In the present study, we retrospectively investigated ART and natural pregnancies to explore the relationship between ART and adverse maternal and neonatal outcomes in China.
Methods
Data collection
This was a retrospective cohort study conducted at Beijing Obstetrics and Gynecology Hospital, Capital Medical University, between January 2013 and December 2015. All ART pregnancies were paired 1:3 with spontaneous pregnancies as the control group during the same time period at Beijing Obstetrics and Gynecology Hospital. The ART and control groups were compared for pregnancy complications, perinatal complications, and neonatal outcomes. Then, we conducted stratification analysis of birth plurality, maternal age, parity and the different types of ART. Only data from live newborns after the 28th week of gestation were included in the analysis. Donor oocytes/sperm or embryo recipients, ovulation induction or women applied preimplantation genetic diagnosis were excluded. Subjects were divided into two groups: conception by ART or spontaneous conception. Then, we conducted stratification analysis of birth plurality, maternal age, parity. According to different fertilization modes, the ART group was divided into IVF and intracytoplasmic sperm injection (ICSI) subgroups. The ART group was also divided into fresh embryo transfer (ET) and frozen embryo transfer (FET) subgroups according to different embryo transfer methods. All data were collected retrospectively from computer databases or telephone interviews.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the Beijing Obstetrics and Gynecology Hospital, Capital Medical University (No. 201592-015). Informed written consent was obtained from all patients in this study. Only data from 28 weeks after live neonatal births were included in the analysis. Methods were carried out in accordance with the approved guidelines.
Statistical analysis
Quantitative data are presented as the mean ± standard deviation (SD). Fisher exact and χ2 tests were performed to test for differences in the proportions of categorical variables between two or more groups. Logistic regression analysis was done to identify possible predictors of pregnancy complications and the association of ART and spontaneous pregnancy. From this analysis, odd ratios (OR) with 95% confidence intervals (CI) were computed for all variables that were significantly associated with pregnancy complications and neonatal defects for ART relative to spontaneous conception. All statistical tests and P values were two-sided, and the limit of statistical significance was P < 0.01. SPSS statistical software (version 21, SPSS Inc., USA) was used for data analysis.
Results
Maternal characteristics of women who conceived by ART or spontaneously
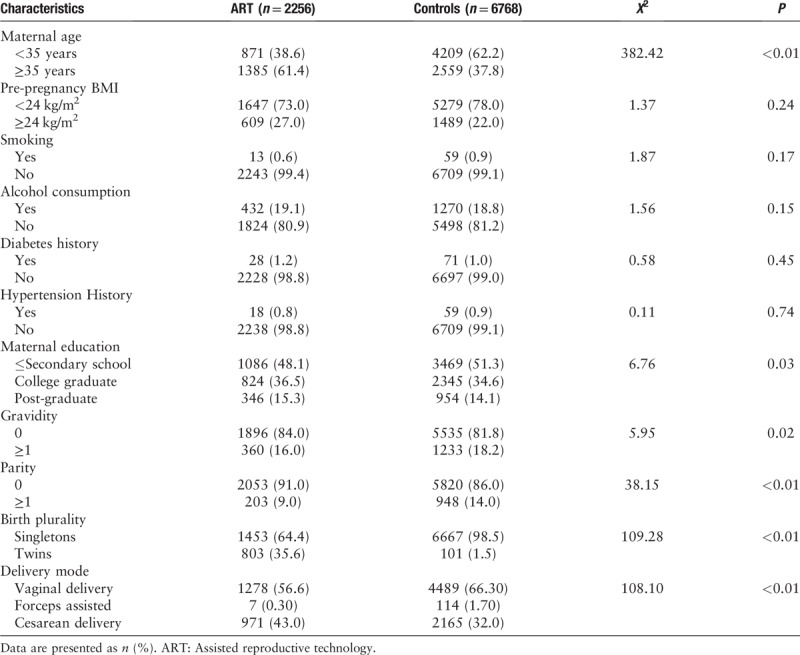
From January 2013 to December 2015, 2256 ART-derived pregnancies and 6768 matched spontaneous pregnancies were enrolled in our study. The ART group consisted of 1453 singleton and 803 twin gestations, while the control group consisted of 6667 singleton and 101 twin gestations. According to different fertilization modes, the ART group was divided into IVF (n = 1873) and ICSI (n = 383) subgroups. The ART group was divided into ET (n = 1583) and FET (n = 673) subgroups by different embryo transfer methods. Table 1 summarizes the maternal characteristics. Women who conceived by ART were older than women who conceived spontaneously. The ART patients tended to be nulliparous. The cesarean section rate was significantly higher in the ART group.
Table 1.
Maternal characteristics among the ART and control groups.
Analysis of pregnancy/perinatal complications and neonatal outcomes in the ART and spontaneous pregnancy groups stratified by birth plurality
Pregnancy complications in the ART and spontaneous pregnant groups are described in Table 2. Regardless of the number of births, women undergoing ART were more likely to develop adverse pregnancy outcomes. Pregnancies after ART were 1.88 times more likely to develop GDM (OR 1.88, 95% CI 1.56–2.27), 2.18 times more likely to develop gestational hypertension (OR 2.18, 95% CI 1.83–2.60), and 2.79 times more likely to develop intrahepatic cholestasis of pregnancy (ICP, OR 2.79, 95% CI 2.15–3.64). Findings were similar in the singleton group. For the twin group, only the incidence of ICP was significantly higher than those in the controls (OR 3.19, 95% CI 2.55–4.00).
Table 2.
Multivariate analysis of maternal and neonatal complications in ART and Controls stratified by birth plurality.
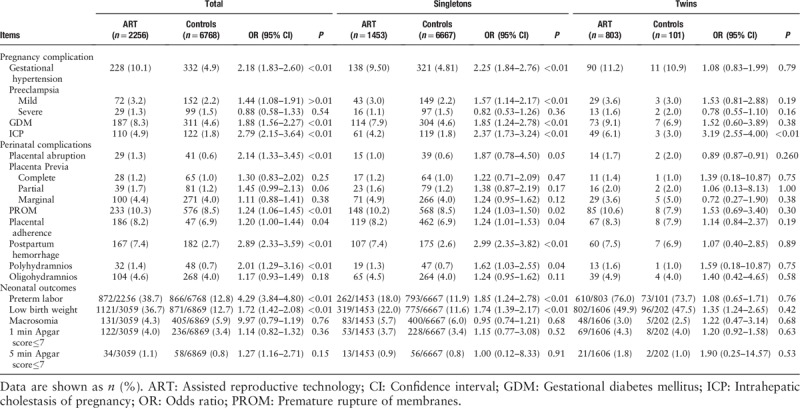
In the ART group, the incidence of most perinatal complications increased significantly [Table 2]. The incidence of placental abruption (OR 2.14, 95% CI 1.33–3.45), fetal premature rupture of membranes (PROM, OR 1.24, 95% CI 1.06–1.45), postpartum hemorrhage (OR 2.89, 95% CI 2.33–3.59) and polyhydramnios (OR 2.01, 95% CI 1.29–3.16), were more likely to occur after ART in all births. The findings were similar in the singleton group, except for PROM and polyhydramnios. There was no significant difference in the incidence of these perinatal complications in the twin group.
The incidences of poor newborn outcomes in the ART and spontaneous pregnancy groups are exhibited in Table 2. Neonatal outcomes included preterm labor, low birth weight, macrosomia, 1-min Apgar ≤ 7, and 5-min Apgar ≤ 7. Some neonatal outcomes, including preterm labor (OR 4.29, 95% CI 3.84–4.80), and low birth weight (OR 1.72, 95% CI 1.42–2.08), were more likely to occur after ART. In the singleton group, preterm labor (OR 1.85, 95% CI 1.24–2.78) and low birth weight (OR 1.74, 95% CI 1.39–2.17) were more likely to occur after ART. However, there was no significant difference in twins.
Analysis of pregnancy/perinatal complications and neonatal outcomes in the ART and spontaneous pregnancy groups stratified by nulliparous and multiparous
There were 2053 nulliparous women in the ART group, and 5820 nulliparous women in the natural conception group. The incidence of nulliparous women in the ART group was significantly higher than that in the natural conception group (91.0% vs. 86.0%). We further studied the incidences of pregnancy, perinatal complications and neonatal outcomes for nulliparous and multiparous women [Table 3]. Nearly all the pregnancy and perinatal complications listed, including gestational hypertension (OR 2.18, 95% CI 1.81–2.62), GDM (OR 1.85, 95% CI 1.60–2.38), ICP (OR 2.87, 95% CI 2.17–3.80), placental abruption (OR 2.43, 95% CI 1.46–4.02), postpartum hemorrhage (OR 3.85, 95% CI 2.27–3.58) and polyhydramnios (OR 2.16, 95% CI 1.39–3.65), were more likely occur after ART in nulliparous women. Gestational hypertension (OR 2.82, 95% CI 1.21–8.72) and complete placenta previa (OR 3.61, 95% CI 1.86–16.87) were significantly increased in multiparous women.
Table 3.
Multivariate analysis of pregnancy outcomes in nulliparous and multiparous groups.
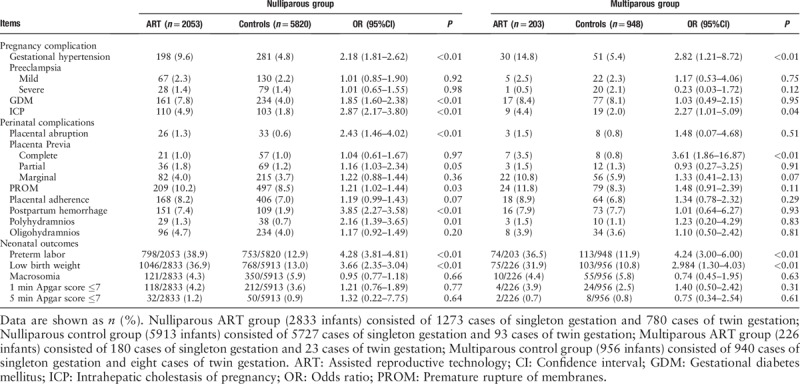
The incidences of poor neonatal outcomes in ART nulliparous and multiparous women are shown in Table 3. For nulliparous women, preterm labor (OR, 4.28, 95% CI 3.81–4.81) and low birth weight (OR, 3.66, 95%CI 2.54–3.04) were significantly different between the two groups. The results were similar between the two groups in multiparous women.
Analysis of pregnancy/perinatal complications and neonatal outcomes in ART and spontaneous pregnancy groups stratified by maternal age
Women who conceived by ART were older than women who conceived spontaneously. The percentage of women ≥35 years old was higher in the ART-conceived group (61.4%) than in the spontaneously pregnant group (37.8%). Therefore, we conducted a maternal age stratification study on the incidences of pregnancy and perinatal complications in ART and control groups [Table 4]. The incidences of gestational hypertension (OR 1.80, 95% CI 1.37–2.39), GDM (OR 1.73, 95% CI 1.64–2.78), ICP (OR 3.03, 95% CI 2.09–4.41), postpartum hemorrhage (OR 2.52, 95% CI 1.83–3.47) were more likely occur after ART when women were younger than 35 years. The risk of gestational hypertension (OR 2.05, 95% CI 1.58–2.68), GDM (OR 1.80, 95% CI 1.37–2.39), ICP (OR 2.65, 95% CI 1.80–3.89), and postpartum hemorrhage (OR 3.37, 95% CI 2.45–4.64) was also markedly increased in advanced age parturient women after ART.
Table 4.
Multivariate analysis of pregnancy outcomes in ART and controls stratified by maternal age.
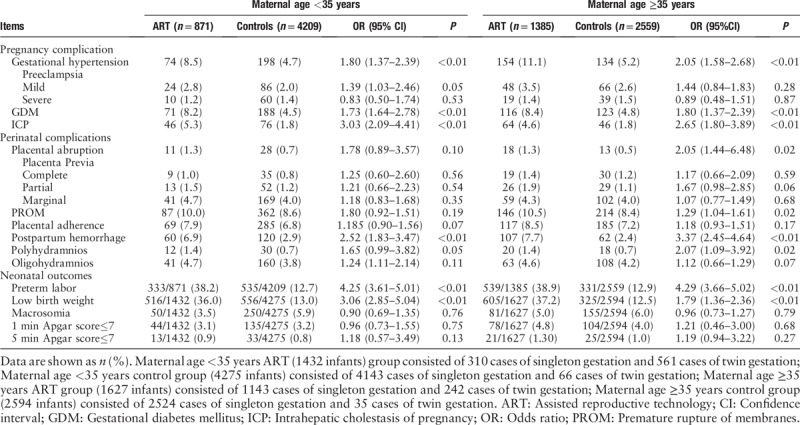
The adverse neonatal outcomes for the ART and control groups according to age stratification are shown in Table 4. Significant increases were observed for preterm labor (OR 4.25, 95% CI 3.61–5.01) and low birth weight (OR, 3.06, 95% CI 2.85–5.04) in the ART group when women were younger than 35 years. For women ≥35 years, the proportions with preterm labor (OR 4.25, 95% CI 3.61–5.01) and low birth weight (OR 3.06, 95% CI 2.85–5.04) were significantly higher for the ART compared with spontaneous group.
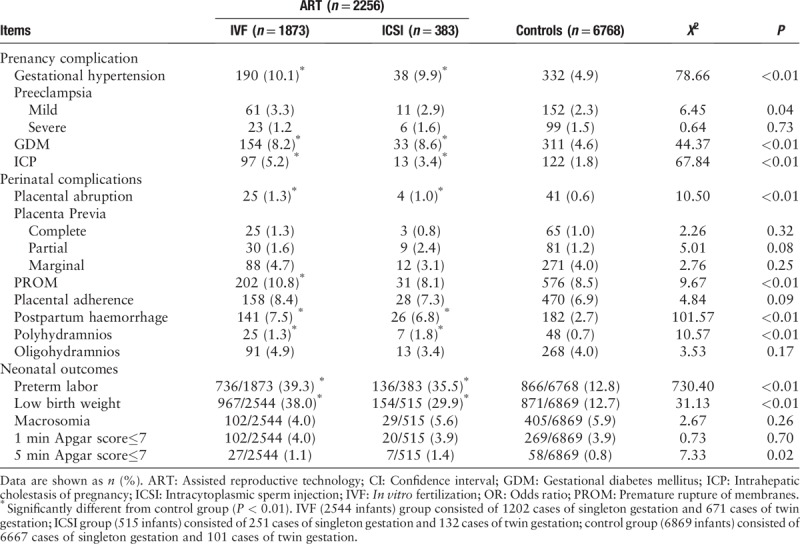
Pregnancy/perinatal complications and neonatal outcomes in IVF, ICSI, and spontaneous pregnancy groups
In addition to stratified analysis of maternal age, parity, and birth plurality, we also compared the incidences of pregnancy and perinatal complications, and neonatal outcomes related to different types of ART, including IVF and ICSI [Table 5]. Patients who underwent IVF were more likely to suffer from gestational hypertension (10.1% vs. 4.9%), GDM (8.2% vs. 4.6%), ICP (5.2% vs. 1.8%), placental abruption (1.3% vs. 0.6%), PROM (10.8% vs. 8.5%), postpartum hemorrhage (7.5% vs. 2.7%), polyhydramnios (1.3% vs. 0.7%), preterm labor (39.3% vs. 12.8%), and low birth weight (38.0% vs. 12.7%), compared with spontaneously conceived pregnancies. ICSI pregnancies showed a higher incidence of gestational hypertension (9.9% vs. 4.9%), GDM (8.6% vs. 4.6%), ICP (3.4% vs. 1.8%), placental abruption (1.0% vs. 0.6%), PROM (8.1% vs. 8.5%), postpartum hemorrhage (6.8% vs. 2.7%), polyhydramnios (1.8% vs. 0.7%), preterm labor (35.5% vs. 12.8%), and low birth weight (29.9% vs. 12.7%) than the control group. Differences became insignificant when comparing the incidence between the IVF and ICSI groups, except for PROM. In the IVF group, 202 women had a pregnancy complicated by PROM (10.8%), compared with 31 women in ICSI group (8.1%, P < 0.001).
Table 5.
Chi-squared analysis of pregnancy outcomes in IVF, ICSI, and spontaneous pregnancy groups.
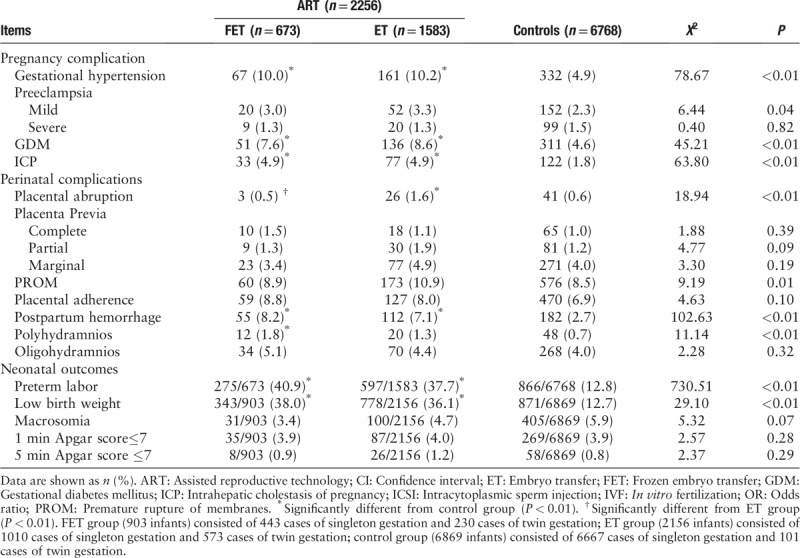
Pregnancy/perinatal complications and neonatal outcomes in fresh, FET and spontaneous pregnancy groups
In considering different ART methods, we also considered different embryo transfer methods. We further studied the incidences of pregnancy/perinatal complications and neonatal outcomes according to different embryo transfer methods, including Fresh and FET [Table 6]. Compared with the control group significantly increased incidences of gestational hypertension (10.0% vs. 4.9%), GDM (7.6% vs. 4.6%), ICP (4.9% vs. 1.8%), PROM (8.9% vs. 8.5%), postpartum hemorrhage (8.2% vs. 2.7%), polyhydramnios (1.8% vs. 0.7%), preterm labor (40.9% vs. 12.8%), and low birth weight (38.0% vs. 12.7%), were observed in both FET subgroup. Fresh subgroup showed a higher incidence of gestational hypertension (10.2% vs. 4.9%), GDM (7.6% vs. 4.6%), ICP (4.9% vs. 1.8%), PROM (10.9% vs. 8.5%), postpartum hemorrhage (7.1% vs. 2.7%), polyhydramnios (1.3% vs. 0.7%), preterm labor (37.7% vs. 12.8%), and low birth weight (36.1% vs. 12.7%) than the control group. It is worth mentioning there is only one insignificant difference between the FET and ET groups. In the FET group, three women had a pregnancy complicated by placental abruption (0.5%), compared with 26 women in ET group (1.6%, P < 0.001).
Table 6.
Chi-squared analysis of pregnancy outcomes in FET, ET, and spontaneous pregnancy groups.
Discussion
In the present retrospective cohort study, we observed the increased risks of perinatal complications and poor neonatal outcomes related to ART, such as GDM, hypertension during pregnancy, ICP, placental abruption, premature rupture of membranes, postpartum hemorrhage, polyhydramnios, premature delivery, and low birth weight. Previous studies have reported that ART has an increased incidence of hypertension during pregnancy, GDM, ICP, postpartum hemorrhage, premature delivery, and low birth weight,[13–16] which is consistent with our present results. The newest ART surveillance in USA reported 23.6% infants conceived with ART were born low birth weight and 29.9% of ART infants were preterm. Several studies have shown that twin pregnancy increased the incidence of adverse pregnancy and birth outcomes.[17–18] However, in our study the twin pregnancy rate in the ART group was over 20 times that in the spontaneous pregnancy group (35.6% vs. 1.5%). Are the adverse maternal and live-birth outcomes of ART in our study due to twin pregnancies? To address this question, we performed further hierarchical analysis by birth plurality. Our study found that the incidence of some adverse pregnancy outcomes in the twin group was higher than that in the singleton group. For example, the incidence of GDM was higher in the twin ART group than in singleton ART group (9.10% vs. 7.69%). The incidence of hypertension during pregnancy in the twin ART group was higher than in singleton ART group (11.2% vs. 9.5%). These findings are consistent with a prospective cohort study by Moini et al.[10] This result suggested that twins are indeed an important factor leading to adverse pregnancy outcomes. Pregnancy, safe delivery, and good maternal and infant outcomes are the goals of successful ART. Single embryo transfer (SET) was first proposed in Sweden in 2003, and is considered the only effective method to avoid multiple pregnancies in ART. SET is on the rise globally, especially in Europe and Japan. In the United States, SET is recommended for patients under 35 years who experienced success with the first or previous ART and have good quality embryos. In China, more doctors are recommending SET for their patients, especially those already with a healthy child. However, ART is typically self-funded in China, and patients seek a higher pregnancy rate and tend to ignore multiple pregnancies and the associated risks. Therefore, the implementation of SET is challenging. As a simple, effective, and easy to implement method, SET can significantly reduce the incidence of multiple pregnancies and maternal/neonatal complications. Actively promoting SET should be standard trend for ART in China.
In our study, the increased risks were found in ART conceived singletons compared with spontaneously conceived singletons: gestational hypertension (2.25-fold), mild preeclampsia (1.57-fold), GDM (1.85-fold), ICP (2.37-fold), postpartum hemorrhage (2.99-fold), preterm labor (1.85-fold), low birth weight (1.74-fold). Although these rates were reduced when analyses were restricted to singletons, significant differences still remained. We conclude that infertility factors in women requiring ART procedures to conceive contribute to adverse obstetric and perinatal outcomes. Ovulatory disorders are a common cause of sterility. These patients may exhibit serious endocrine disorders, such as insulin resistance, and carry high risk factors for obstetrical diseases, such as GDM, and hypertensive disorder complicating pregnancy. Polycystic ovary syndrome is the most common endocrinopathy of infertile women. Kelley et al have suggested that in pregnancy, PCOS women experience increased risk of miscarriage, gestational diabetes, preeclampsia, and extremes of fetal birth weight.[19] Some infertile patients have uterine damage due to uterine cavity operations. These patients more likely to have placental adhesions, placenta previa, postpartum hemorrhage and other perioperative complications after ART conception. A study by suggested that women with one previous induced abortion had higher rates of spontaneous preterm birth (adj. OR, 1.4; 95% CI, 1.0–1.9) and PROM (OR, 2.0; 95% CI, 1.4–3.0).[20] Some ART patients have infertility caused by endometriosis. The uterus of such patients often exhibit adenomyosis, which may lead to a large inflexible uterus and difficult obstetrical delivery, limited fetal growth, premature delivery, low birth weight, and other adverse maternal and infant outcomes. Our conclusions are consistent with some previous studies.[21–22] A meta-analysis revealed that endometriosis is associated with an increased risk of placenta previa in pregnancies achieved through ART (OR 2.96 (95% CI 1.25–7.03). They found that the frequencies of preterm birth and placenta previa were significantly increased in women with endometriosis, and the severity of endometriosis might have an adverse impact on ART pregnancy.[22] A retrospective cohort study in Japan also suggested that some causes of maternal infertility, and not the ART technique, may lead to the risk of poor obstetrics and perioperative outcomes.[23] Although these results should be interpreted with caution because the specificities of the subjects and database vary among studies, it seems that maternal factors associated with infertility may contribute to the adverse outcomes rather than the ART procedures themselves. However, the mechanisms leading to these adverse outcomes in infertile women remain unclear. These issues are worth further studying for elucidation. In future work, we will analyze the pregnancy outcomes of ART patients according to the different causes of sterility to reveal potential underlying mechanisms.
With the rapid development of ART technology, many new technologies have been born. Whether the pregnancy outcomes of different ART technology are different is also a hot topic that people are very concerned about. At present, the relevant research is limited, and the conclusions are inconsistent. In our study, differences became insignificant when comparing the incidence between the IVF and ICSI groups, except for PROM. Andrijasevic et al also found that ICSI was more prone to premature delivery and premature rupture of membranes in patients than IVF.[24] There is only one insignificant difference between the FET and ET groups, which is placental abruption. Our results in part complement a recent publication,[25] which demonstrated that although the increased risk of birth defects associated with IVF was no longer significant after adjustment for parental factors, the risk of birth defects associated with ICSI remained increased after multivariate adjustment. A retrospective study from the Centers for Disease Control and Prevention in the United States from 2007 to 2014 showed that transplantation patterns were closely related to infant birth weight in ART patients. The average birth weight of the FET group was 142 g higher than that of the ET group, and the risk of low birth weight in FET infants was significantly reduced.[26] Noguchi et al suggested that embryo transfer is a risk factor for severe postpartum hemorrhage.[27] The inconsistency of the conclusion may be due to the small sample size of this study. In order to obtain more accurate conclusions, we will further expand the sample size in the next study. According to our study, we suggested that there is no significant difference in pregnancy outcomes between different ART techniques. Clinicians can flexibly adopt various ART techniques according to the actual situation of the patients.
There are several limitations to our study. First, due to the retrospective study design, data were extracted from the medical record system at a single center. The sample number is still relatively small. For getting a more creditable conclusion, we can consider multi-center, prospective studies, and expand the sample size in order to obtain higher level evidence. Second, since no data were collected on the particular cause of infertility, baseline endocrine level, as well as serum hormone levels during ovarian stimulation; therefore, we cannot analyze how these different factors may affect maternal and neonatal outcomes. The intrauterine insemination (IUI) is a relatively less invasive form of ART. However, the records of IUI outcomes are lacked in our database, and not included in the present study, which would lead to bias. It should be considered in future research plan.
To summarize, women who conceived by ART seem to have an increased risk for adverse obstetric and perinatal outcomes. Multiple pregnancies can partly explain this phenomenon. Elective single embryo transfer should be strongly promoted to reduce the perinatal risks of ART pregnancy. Infertility may contribute to the adverse perinatal outcomes. Further studies about how the cause of sterility affects the pregnancy outcome of ART are deserved.
Funding
This research was supported by a grant from the Capital Health Research and Special Development (No. 2014-1-4091).
Conflict of interest
None.
Footnotes
How to cite this article: Lei LL, Lan YL, Wang SY, Feng W, Zhai ZJ. Perinatal Complications and Live-birth Outcomes following Assisted Reproductive Technology: A Retrospective Cohort Study. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000484
References
- 1.Talaulikar VS, Arulkumaran S. Reproductive outcomes after assisted conception. Obstet Gynecol Surv 2012; 67:566–583.. doi: 10.1097/OGX.0b013e31826a5d4a. [DOI] [PubMed] [Google Scholar]
- 2.Yang X, Li Y, Li C, Zhang W. Current overview of pregnancy complications and live-birth outcome of assisted reproductive technology in mainland China. Fertil Steril 2014; 101:385–391.. doi: 10.1016/j.fertnstert.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Farhi A, Reichman B, Boyko V, Hourvitz A, Ron-El R, Lerner-Geva L. Maternal and neonatal health outcomes following assisted reproduction. Reprod Biomed Online 2013; 26:454–461.. doi: 10.1016/j.rbmo.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Jackson S, Hong C, Wang ET, Alexander C, Gregory KD, Pisarska MD. Pregnancy outcomes in very advanced maternal age pregnancies: the impact of assisted reproductive technology. Fertil steril 2015; 103:76–80.. doi: 10.1016/j.fertnstert.2014.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marino JL, Moore VM, Willson KJ, Rumbold A, Whitrow MJ, Giles LC, et al. Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PloS One 2014; 9:e80398.doi: 10.1371/journal.pone.0080398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malchau SS, Loft A, Henningsen AK, Nyboe Andersen A, Pinborg A. Perinatal outcomes in 6,338 singletons born after intrauterine insemination in Denmark, 2007 to 2012: the influence of ovarian stimulation. Fertil Steril 2014; 102:1110–1116.. e2. doi: 10.1016/j.fertnstert.2014.06.034. [DOI] [PubMed] [Google Scholar]
- 7.Li Z, Wang YA, Ledger W, Sullivan EA. Birthweight percentiles by gestational age for births following assisted reproductive technology in Australia and New Zealand, 2002-2010. Hum Reprod 2014; 29:1787–1800.. doi: 10.1093/humrep/deu120. [DOI] [PubMed] [Google Scholar]
- 8.Qin J, Liu X, Sheng X, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 2016; 105:73–85.. e1-6. doi: 10.1016/j.fertnstert.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Geisler ME, O’Mahony A, Meaney S, Waterstone JJ, O’Donoghue K. Obstetric and perinatal outcomes of twin pregnancies conceived following IVF/ICSI treatment compared with spontaneously conceived twin pregnancies. Eur J Obstet Gynecol Reprod Biol 2014; 181:78–83.. doi: 10.1016/j.ejogrb.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 10.Moini A, Shiva M, Arabipoor A, Hosseini R, Chehrazi M, Sadeghi M. Obstetric and neonatal outcomes of twin pregnancies conceived by assisted reproductive technology compared with twin pregnancies conceived spontaneously: a prospective follow-up study. Eur J Obstet Gynecol Reprod Biol 2012; 165:29–32.. doi: 10.1016/j.ejogrb.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Woo I, Hindoyan R, Landay M, Ho J, Ingles SA, McGinnis LK, et al. Perinatal outcomes after natural conception versus in vitro fertilization (IVF) in gestational surrogates: a model to evaluate IVF treatment versus maternal effects. Fertil Steril 2017; 108:993–998.. doi: 10.1016/j.fertnstert.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Bu Z, Chen ZJ, Huang G, Zhang H, Wu Q, Ma Y, et al. Live birth sex ratio after in vitro fertilization and embryo transfer in China--an analysis of 121,247 babies from 18 centers. PloS One 2014; 9:e113522.doi: 10.1371/journal.pone.0113522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harlev A, Walfisch A, Oran E, Har-Vardi I, Friger M, Lunenfeld E, et al. The effect of fertility treatment on adverse perinatal outcomes in women aged at least 40 years. Int J Gynaecol Obstet 2018; 140:98–104.. doi: 10.1002/ijgo.12345. [DOI] [PubMed] [Google Scholar]
- 14.Wennberg AL, Opdahl S, Bergh C, Aaris Henningsen AK, Gissler M, Romundstad LB, et al. Effect of maternal age on maternal and neonatal outcomes after assisted reproductive technology. Fertil Steril 2016; 106:1142–1149.. e1114. doi: 10.1016/j.fertnstert.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 15.Martin AS, Chang J, Zhang Y, Kawwass JF, Boulet SL, McKane P, et al. Perinatal outcomes among singletons after assisted reproductive technology with single-embryo or double-embryo transfer versus no assisted reproductive technology. Fertil steril 2017; 107:954–960.. doi: 10.1016/j.fertnstert.2017.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qin JB, Wang H, Sheng X, Xie Q, Gao S. Assisted reproductive technology and risk of adverse obstetric outcomes in dichorionic twin pregnancies: a systematic review and meta-analysis. Fertil Steril 2016; 105:1180–1192.. doi: 10.1016/j.fertnstert.2015.12.131. [DOI] [PubMed] [Google Scholar]
- 17.Luke B, Gopal D, Cabral H, Stern JE, Diop H. Adverse pregnancy, birth, and infant outcomes in twins: effects of maternal fertility status and infant gender combinations; the Massachusetts Outcomes Study of Assisted Reproductive Technology. Am J Obstet Gynecol 2017; 217:330.e331-330.e315. doi: 10.1016/j.ajog.2017.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shan D, Hu Y, Qiu P, Mathew BS, Chen Y, Li S, et al. Intrahepatic cholestasis of pregnancy in women with twin pregnancy. Twin Res Hum Genet 2016; 19:697–707.. doi:10.1017/thg.2016.74. [DOI] [PubMed] [Google Scholar]
- 19.Kelley AS, Smith YR, Padmanabhan V. A narrative review of placental contribution to adverse pregnancy outcomes in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2019; doi: 10.1210/jc.2019-00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Makhlouf MA, Clifton RG, Roberts JM, Myatt L, Hauth JC, Leveno KJ, et al. Adverse pregnancy outcomes among women with prior spontaneous or induced abortions. Am J Perinatal 2014; 31:765–772.. doi: 10.1055/s-0033-1358771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fujii T, Wada-Hiraike O, Nagamatsu T, Harada M, Hirata T, Koga K. Assisted reproductive technology pregnancy complications are significantly associated with endometriosis severity before conception: a retrospective cohort study. Reprod Biol Endocrinol 2016; 14:73.doi: 10.1186/s12958-016-0209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gasparri ML, Nirgianakis K, Taghavi K, Papadia A, Mueller MD. Placenta previa and placental abruption after assisted reproductive technology in patients with endometriosis: a systematic review and meta-analysis. Arch Gynecol Obstet 2018; 298:27–34.. doi: 10.1007/s00404-018-4765-x. [DOI] [PubMed] [Google Scholar]
- 23.Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril 2012; 98:922–928.. doi: 10.1016/j.fertnstert.2012.05.049. [DOI] [PubMed] [Google Scholar]
- 24.Andrijasevic S, Dotlic J, Aksam S, Micic J, Terzic M. Impact of conception method on twin pregnancy course and outcome. Geburtshilfe Frauenheilkunde 2014; 74:933–939.. doi: 10.1055/s-0034-1383148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yin L, Hang F, Gu LJ, Xu B, Ma D, Zhu GJ. Analysis of birth defects among children 3 years after conception through assisted reproductive technology in China. Birth Defects Res Part A Clin Mol Teratol 2013; 97:744–749.. doi: 10.1002/bdra.23116. [DOI] [PubMed] [Google Scholar]
- 26.Litzky JF, Boulet SL, Esfandiari N, Zhang Y, Kissin DM, Theiler RN, et al. Effect of frozen/thawed embryo transfer on birthweight, macrosomia, and low birthweight rates in US singleton infants. Am J Obstet Gynecol 2018; 218:433.e431–433.e410.. doi: 10.1016/j.ajog.2017.12.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noguchi S, Murakoshi T, Konno H, Matsushita M, Matsumoto M. Embryo transfer is a risk factor for severe postpartum hemorrhage and blood transfusion requirement. J Matern Fetal Neonatal Med 2019; 32:1–4.. doi: 10.1080/14767058.2017.1394288. [DOI] [PubMed] [Google Scholar]


