ABSTRACT
Intestinal vaginoplasty, first described in 1904, has more recently become a popular mechanism for gender-affirming surgery in the United States. We present the case of a transgender female patient with retained foreign bodies in her neovagina, which required endoscopic therapy, provide a brief review of the literature, and discuss the potential long-term complications that can arise from a neovagina after intestinal transfer. It is important that gastroenterologists have awareness and recognition of these issues, as surgical reconstruction using intestinal segments for transgender patients becomes more common.
INTRODUCTION
The incidence of gender-affirming surgeries among transgender patients in the United States has increased over the past 2 decades and continues to rise.1 The use of intestinal transfer in vaginal reconstruction using the sigmoid colon provides satisfactory form and function, compared to more traditional methods. Although the long-term complications are still developing, there have been several case reports of diversion colitis and malignancy.2–4 We explore the potential complications of a sigmoid neovagina in a transgender female patient who presented with retained foreign bodies.
CASE REPORT
A 40-year-old transgender female presented to the gastroenterology clinic for foreign bodies in her neovagina. She underwent a sigmoid vaginoplasty 11 years prior in Thailand. She endorsed increasing foul-smelling discharge over the past 6 months, which was unresponsive to antibiotic treatment. She denied purposeful introduction of foreign bodies into her vagina but endorsed high-risk sexual behaviors. She had previously presented to her gynecologist and urologist, who were able to visualize the foreign bodies with a speculum and cystoscopy examination, respectively, but unable to retrieve the foreign bodies, which were beyond the reach of their retrieval devices. In our office, her abdominal and rectal examination was unremarkable.
Manual examination of her neovagina was also unremarkable. Labs revealed a normal complete blood count and basic metabolic panel. Her abdominal and pelvic computed tomography scan without contrast revealed postsurgical changes from her previous sigmoid resection and a neovagina created from the intestinal segment with at least 3 conical-shaped foreign bodies, approximately 12 cm from the orifice (Figure 1). She was taken to the endoscopy unit for retrieval of the foreign bodies. She was placed in lithotomy position; an upper endoscope was introduced through the introitus. We identified 4 foreign bodies embedded in the mucosa, with associated erythema, edema, deep ulcerations, and surrounding inflammatory appearing polyps (Figure 2). The foreign bodies were consistent with plastic caps from lubricant jelly tubes. Each cap was removed in series using rat tooth forceps. The procedure was complicated only by minimal mucosal bleeding, which resolved without intervention. She was hospitalized for 1 day and given a 7-day course of amoxicillin–clavulanic acid, with the resolution of her symptoms.
Figure 1.

Foreign bodies appreciated approximately 15 cm proximal to the introitus, with associated granulation tissue.
Figure 2.
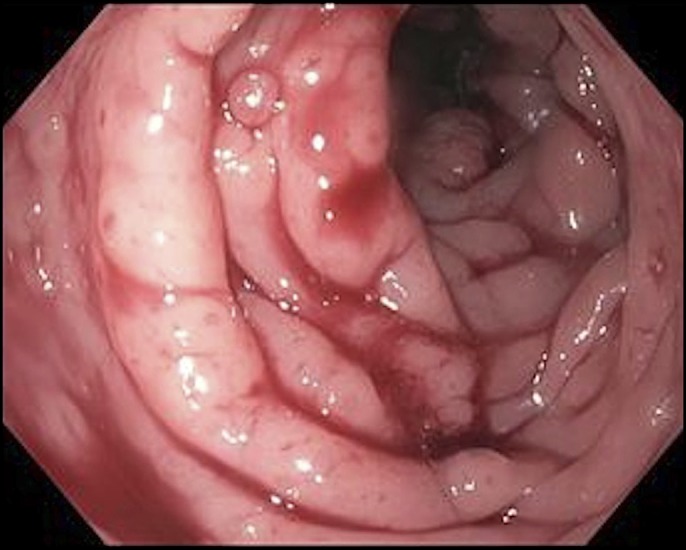
Neovagina constructed of sigmoid colon with inflammatory polyps and ulcerations in the setting of multiple embedded foreign bodies.
DISCUSSION
Several methods of vaginal reconstruction have been developed for the treatment of vaginal agenesis and, more recently, for gender-affirming surgery. Intestinal vaginoplasty was first described by Baldwin in 1904 but has recently increased in popularity for gender-affirming surgery because it offers several advantages over other methods including traditional inversion vaginoplasty with penile scrotal flaps.5 The functional, aesthetic, and surgical advantages include improved sensation, natural lubrication, superior blood supply, increased luminal width and depth, and an appearance that closely matches vaginal mucosa.6 Although any intestinal segment can be used for this technique, the sigmoid colon has been identified as the optimal bowel segment for this purpose, as it produces less copious secretions, creates a more natural vaginal depth, and results in lower rates of vaginal stenosis.7
Although immediate postoperative care is provided by the surgeon, long-term health care and health maintenance in transgender patients undergoing this surgery remain a challenge. In review of the literature, health maintenance with the primary care physician following gender-affirming surgery emphasizes cancer screening of reproductive organs accounting for the presence of gender-affirming hormones and procedures.8 This includes routine screening for breast, cervical, ovarian, endometrial, and prostate cancer and human papillomavirus and hepatitis B virus vaccinations for at-risk groups. However, patients with intestinal neovaginas represent a unique group who may need additional surveillance of the ectopic colonic tissue, which is at risk for complications.
Transplanted intestinal tissue can develop diversion colitis and chronic inflammatory changes.3 Chronic inflammation may be due to bacterial infection or changes in bacterial flora. Hiroi et al also suggested that frequent sexual intercourse may create microinjury and inflammation to the mucosa.9 The question of whether chemical stimulation from semen and urine can be carcinogenic has also been raised.4 There has been at least one report of ulcerative colitis in the neovagina.10 Human papillomavirus–linked squamous cell carcinoma has also been reported in the neovagina.11 There have been 3 reports to date of colonic neoplasia forming in the neovagina.4,9 These cases raise the question of whether these patients should undergo routine screening of the transplanted colon tissue and whether this tissue is at increased risk of malignancy, given the risk of chronic inflammation. There are currently no formal screening guidelines for this group of patients.
DISCLOSURES
Author contributions: K. Leroy, A. Long, and P. Wong contributed equally to the manuscript. K. Leroy is the article guarantor.
Financial disclosure: none to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;153(7):609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Özkan Ö, Özkan Ö, Çinpolat A, et al. Vaginal reconstruction with the modified rectosigmoid colon: Surgical technique, long-term results and sexual outcomes. J Plast Surg Hand Surg. 2018;52(4):210–6. [DOI] [PubMed] [Google Scholar]
- 3.Van Der Sluis WB, Buncamper ME, Bouman M-B, et al. Symptomatic HPV-related neovaginal lesions in transgender women: Case series and review of literature. Sex Transm Infect. 2016;92(7):499–501. [DOI] [PubMed] [Google Scholar]
- 4.Kita Y, Mori S, Baba K, et al. Mucinous adenocarcinoma emerging in sigmoid colon neovagina 40 years after its creation: A case report. World J Surg Oncol. 2015;13(1):213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldwin JF. The formation of an artificial vagina by intestinal transplantation. Ann Surg. 1904;40(3):398–403. [PMC free article] [PubMed] [Google Scholar]
- 6.Aminsharifi A, Afsar F, Jafari M, Tourchi A. Removal of an entrapped large metallic dilator from the sigmoid neovagina in a male-to-female transsexual using a laparoscopic approach. Int J Surg Case Rep. 2012;3(7):266–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salgado CJ, Nugent A, Kuhn J, Janette M, Bahna H. Primary sigmoid vaginoplasty in transwomen: Technique and outcomes. Biomed Res Int. 2018;2018:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitlock BL, Duda ES, Elson MJ, et al. Primary care in transgender persons. Endocrinol Metab Clin North Am. 2019;48(2):377–90. [DOI] [PubMed] [Google Scholar]
- 9.Hiroi H, Yasugi T, Matsumoto K, et al. Mucinous adenocarcinoma arising in a neovagina using the sigmoid colon thirty years after operation: A case report. J Surg Oncol. 2001;77(1):61–4. [DOI] [PubMed] [Google Scholar]
- 10.Malka D, Anquetil C, Ruszniewski P. Ulcerative colitis in a sigmoid neovagina. N Engl J Med. 2000;343(5):369. [DOI] [PubMed] [Google Scholar]
- 11.Bollo J, Balla A, Luppi CR, Martinez C, Quaresima S, Targarona EM. HPV-related squamous cell carcinoma in a neovagina after male-to-female gender confirmation surgery. Int J STD AIDS. 2017;29(3):306–8. [DOI] [PubMed] [Google Scholar]


