Abstract
Rationale:
Teratomas are extremely rare in the thyroid gland. A cervical teratoma presenting as a cystic or mixed thyroid lesion can be easily confused with a thyroglossal duct cyst. It is difficult for pediatricians to differentiate between these 2 types of lesions.
Patients concerns:
A 2-year-old girl who presented a growing thyroid mass for 14 months showed a mass in her left thyroid lobe under contrast-enhanced computed tomography (CT).
Diagnosis and interventions:
Ultrasonography found a mass of 5 × 3.5 cm within the left lobe of the thyroid gland, and the sonogram revealed areas with echo-free and mixed-echo patterns. There was no accumulation of technetium-99m pertechnetate on the thyroid scintigraphy (cold thyroid nodule). CT scan showed a mass (5.0 × 3.0 × 2.5 cm in size) that extended from the left thyroid lobe to the anterior mediastinum with no evident enhancement and clear margins that contained calcifications. Complete excision without intraoperative capsule disruption was achieved. Histologically, the thyroid mass was diagnosed as a mature teratoma.
Outcomes:
The postoperative course was uneventful after follow-ups for 2 years, and the patient had no inflammatory signs or evidence of recurrence.
Lessons:
Thyroid teratoma is rare in infants and is usually benign; however, some thyroid teratomas are malignant and inclined to relapse. The authors emphasize that thyroid teratomas in children should be included in the differential diagnosis of cystic lesions located in the head and neck area. Complete resection is essential for good outcomes. In addition, long-term follow-ups are warranted to follow the complications of the malignant or recurrent disease.
Keywords: infant, teratoma, thyroid gland
1. Introduction
Teratomas are rare types of tumors in children that are pathologically defined by the 3 germ cell layer layers: the ectoderm, mesoderm, and endoderm. The most common sites of occurrence in childhood are the sacrococcygeal region, gonads, mediastinum, and pineal region.[1] Head and neck teratomas make up only 0.47% to 6% of all teratomas reported in the literature,[2,3] with exceptionally rare cases found in association with the thyroid gland.
A cervical teratoma presenting as a cystic or mixed thyroid lesion can be easily confused with a thyroglossal duct cyst. Herein, we reported a benign teratoma of the thyroid treated by complete excision in a 2-year-old girl, initially thought to be a thyroid cyst. We present the clinical outcome and diagnostic imaging findings, to highlight this diagnostic challenge.
2. Case report
Ethical approval was obtained from the Ethics Board of the Children's Hospital of Shanghai, Shanghai Jiao Tong University. Informed written consent was obtained from the patient's parents for publication of this case report and accompanying images. Notably, the 2-year-old girl had a cervical mass more than 1 year ago. A left neck mass was identified that gradually increased in size without associated focal or systemic inflammatory manifestations. At the time of admission to our hospital, she was asymptomatic with no dysphagia symptoms, aspiration symptoms, or breathing difficulties.
Physical examination identified a predominantly left-sided cervical mass that crossed the midline. The mass was tough and nontender to palpation, and impressive in size, measuring approximately 5 cm by 3 cm in terms of its transverse anterior-posterior and cephalad-caudal dimensions, respectively. However, the cervical lymph nodes were not affected. There were no discolorations or sinus/fistula openings of the overlying skin.
The results of preliminary laboratory tests, including thyroid function (free triiodothyronine, free thyroxin, thyroglobulin, antithyroid peroxidase antibody and antithyroglobulin antibody), alpha-fetoprotein (AFP), and beta-human chorionic gonadotrophin (βHCG) levels tests were within the reference ranges.
Ultrasonography found a mass of 5 × 3.5 cm within the left lobe of the thyroid gland, and the sonogram revealed areas with echo-free and mixed-echo patterns. There was no accumulation of technetium-99m pertechnetate on the thyroid scintigraphy (cold thyroid nodule). Computed tomography (CT) scan, showed a mass (5.0 × 3.0 × 2.5 cm in size) that extended from the left thyroid lobe to the anterior mediastinum with no evident enhancement and clear margins that contained calcifications (Fig. 1). Additionally, normal morphology of the left thyroid lobe disappeared. The trachea was displaced to the right. Abnormal enlargement of lymph nodes was not observed in the neck.
Figure 1.
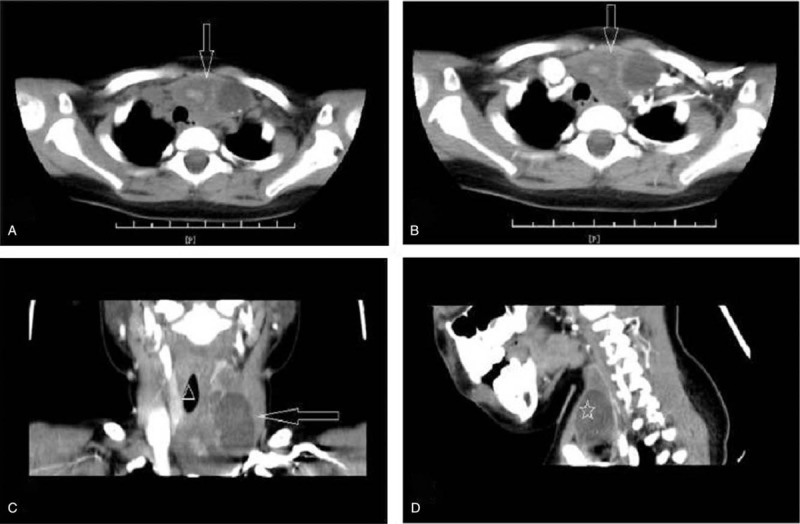
A, CT scan showing a heterogeneous cystic and solid mass (white arrow) within the left thyroid lobe and clear margins that contained calcifications. B, Intravenous contrast-enhanced axial reveals no evident enhancement,(white arrow). C, There are distortion and compression of the airway (white triangle). D, Coronal views. CT = computed tomography.
Complete excision without intraoperative capsule disruption was achieved (Fig. 2). Grossly the tumor consists of both solid and cystic contents. Histopathologic examination revealed cystic compounds in which characteristic mature brain tissue, choroid tissue, thyroid follicles, and smooth muscle components were mixed (Fig. 3). The consensus opinion was that the presence of all 3 germ layers was representative of mature teratoma.
Figure 2.
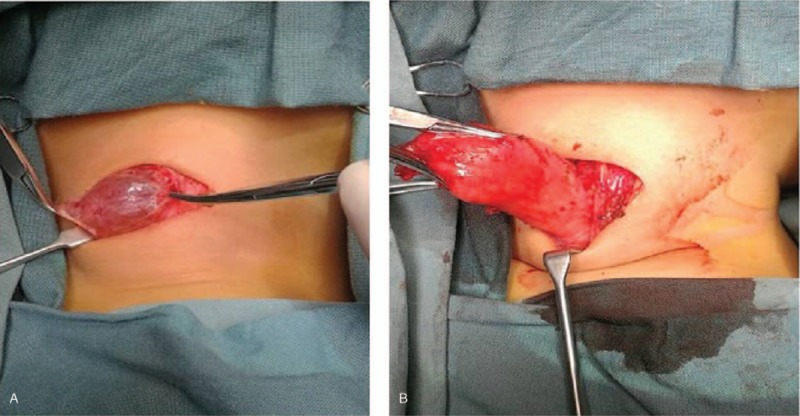
An intraoperative clinical picture demonstrates a well-demarcated tumor surrounded by a thin capsule.
Figure 3.
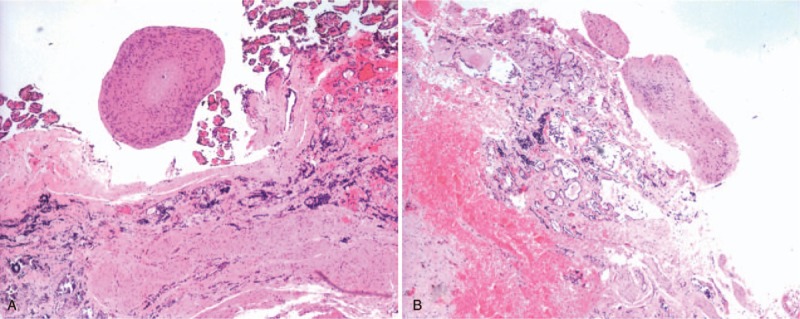
Histopathologic examination revealed cystic compounds in which characteristic mature brain tissue, choroid tissue, thyroid follicles, and smooth muscle components were mixed. (H&E, original magnification×200). H&E = hematoxylin and eosin staining.
The postoperative course was uneventful after follow-ups for 2 years, and the patient had no inflammatory signs or evidence of recurrence. The patient is still attending the outpatient clinic.
3. Discussion
Teratomas comprise the most common extragonadal germ cell tumors in childhood. Cervical teratomas account for approximately 5% of all teratomas and are reported in approximately 1:20,000 to 1:40,000 live births,[2,3] with a female predominance.[4] Cervical teratomas are divided into thyroid teratomas and extrathyroid teratomas, depending on where they originated.[3] Thyroid teratomas represent <0.1% of all primary thyroid gland neoplasms.[5] Although diagnostic criteria for thyroid teratomas are controversy among researchers, thyroid teratomas must meet at least one of the following criteria: the tumor occupies portions of the thyroid, shows continuity with the gland, or has supposedly replaced the gland.[5,6] In the present case, the lesion met all criteria by occupying part of the left thyroid, being located in direct continuity with the thyroid and having the normal morphology of the left thyroid lobe disappeared. Reports of malignant changes vary between 2.7% and 20%.[7,8] As there was no infiltration into surrounding tissues, or metastasis to lymph nodes, the possibility of a malignant teratoma was ruled out. Asymptomatic gradual enlargement is the most common clinical finding. Rapid enlargement is often associated with secondary infection or hemorrhage.[9] Thyroid teratoma is rare in infants. Although thyroid teratomas are usually benign, they can cause airway compression, depending on the site and size of the mass. In this case, the CT scan displayed that the mass caused a deviation of the airway to the right, but there was no obstructive respiratory distress in the patient.
3.1. Radiology
Ultrasound can be useful in determining the size and consistency of the lesions. Ultrasound often shows well-defined heterogeneous mass, as well as solid and cystic components. In particular, a hypoechoic mass is an important ultrasound finding with a sensitivity of 41%, and specificity of 92%.[10] CT scans are known to be more effective than ultrasound in diagnosing teratomas that occur in the mediastinum or retroperitoneum. Theoretically, distinct imaging features, such as the heterogeneous solid and cystic nature of the mass that sometimes have additional fatty or calcific elements, can help characterize and differentiate teratomas from those entities. In this patient, a CT scan of the neck exhibited a benign tumor containing inhomogeneously little enhancing cystic portions, with a clear margin that extended to the anterior mediastinum and calcification without invasion into lymph nodes or surrounding tissues. MRI typically provides harmless and favorable imaging delineation. The typical appearance is a well-circumscribed complex lesion with both solid and unilocular or multilocular cystic components.[11] If calcification is present, it may be helpful to differentiate these lesions, but the absence of calcifications does not rule out the diagnosis.[12]
3.2. Laboratory tests
AFP is a favorable sign of the therapeutic outcome, but the usefulness of AFP as an initial diagnostic tool is unclear. It has been reported that a persistent or fluctuating AFP level may represent metastatic or recurrent disease and warrants investigation.[13] In our patient, the AFP level was normal at initial diagnosis, and additional monitoring showed that the AFP level was within the reference ranges. Beta-human chorionic gonadotropin monitoring is less reliable and does not appear to add clinical value in addition to AFP monitoring.[14]
3.3. Histopathology
Teratomas are classically defined as germ cell-derivation neoplasms comprised of different tissue components from all 3 germ cell layers. There was an intimate admixture of endodermal (gastrointestinal mucosal inclusions and thyroid follicles), mesodermal (smooth muscle), and ectodermal (squamous epithelium) components in this lesion.[11] Notably, groups of melanocytic cells formed mounds on the cyst wall that stained positive for S100.[14] These findings supported the diagnosis of a cervical teratoma and excluded the other differential considerations.
3.4. Management
This patient was diagnosed with an anterior neck mass in children and subsequently treated with surgical resection, which is widely accepted as the optimal treatment of primary head and neck teratomas.[14] Surgically, the key is to remove all the lesion while preserving the normal structures. In addition, delay in treatment may result in interim lesion growth or infection with subsequent aerodigestive tract impaction.[15] In this patient, the left thyroid was not completely developed, but the patient had normal thyroid function.
3.5. Prognosis
Recurrences of benign thyroid teratomas following complete surgical resection are rare, and the long-term prognosis is excellent.[14,16] Primary thyroid malignant teratoma is rare. According to the few reports available, the overall survival of malignant thyroid teratoma is less than a year.[5,17]
4. Conclusions
Thyroid teratoma is rare in infants and is usually benign; however, some thyroid teratomas are malignant and inclined to relapse. The authors emphasize that thyroid teratomas in children should be included in the differential diagnosis of cystic lesions located in the head and neck area. Complete resection is essential for good outcomes. In the future, long-term follow-up is warranted to follow complications of the malignant or recurrent disease.
Author contributions
Conceptualization: Zhibao Lv.
Data curation: Xiaoling Bai, Jiangbin Liu, Yibo Wu.
Formal analysis: Qingfeng Sheng.
Funding acquisition: Zhibao Lv.
Investigation: Qingfeng Sheng.
Methodology: Xiaoling Bai.
Project administration: Qingfeng Sheng.
Resources: Jiangbin Liu, Yibo Wu.
Software: Xiaoling Bai.
Supervision: Zhibao Lv.
Validation: Xiaoling Bai.
Visualization: Xiaoling Bai.
Writing – original draft: Xiaoling Bai.
Writing – review & editing: Xiaoling Bai, Zhibao Lv.
Footnotes
Abbreviations: AFP = alpha-fetoprotein, CT = computed tomography.
The authors have no conflicts of interest to disclose.
References
- [1].Buckley NJ, Burch WM, Leight GS. Malignant teratoma in the thyroid gland of an adult: a case report and a review of the literature. Surgery 1986;100:932–7. [PubMed] [Google Scholar]
- [2].Dunn CJ, Nguyen DL, Leonard JC. Ultrasound diagnosis of immature cervical teratoma: a case report. Am J Perinatol 1992;9:445–7. [DOI] [PubMed] [Google Scholar]
- [3].Rothschild MA, Catalano P, Urken M, et al. Evaluation and management of congenital cervical teratoma. Case report and review. Arch Otolaryngol Head Neck Surg 1994;120:444–8. [DOI] [PubMed] [Google Scholar]
- [4].Tonni G, De Felice C, Centini G, et al. Cervical and oral teratoma in the fetus: a systematic review of etiology, pathology, diagnosis, treatment and prognosis. Arch Gynecol Obstet 2010;282:355–61. [DOI] [PubMed] [Google Scholar]
- [5].Thompson LD, Rosai J, Heffess CS. Primary thyroid teratomas: a clinicopathologic study of 30 cases. Cancer 2000;88:1149–58. [PubMed] [Google Scholar]
- [6].Kimler SC, Muth WF. Primary malignant teratoma of the thyroid: case report and literature review of cervical teratomas in adults. Cancer 1978;42:311–7. [DOI] [PubMed] [Google Scholar]
- [7].Jordan RB, Gauderer MW. Cervical teratomas: an analysis. Literature review and proposed classification. J Pediatr Surg 1988;23:583–91. [DOI] [PubMed] [Google Scholar]
- [8].Kerner B, Flaum E, Mathews H, et al. Cervical teratoma: prenatal diagnosis and long-term follow-up. Prenat Diagn 1998;18:51–9. [PubMed] [Google Scholar]
- [9].Hartog H, Dikkers FG, Veldhuizen AG, et al. Cervical cystic swelling in an adolescent: unusual association of a cervical mature teratoma with vertebral anomalies and a history of gastric duplication cyst. J Pediatr Surg 2011;46:e15–8. [DOI] [PubMed] [Google Scholar]
- [10].Henrichsen TL, Reading CC. Thyroid ultrasonography. Part 2: nodules. Radiol Clin North Am 2011;49:417–24. v. [DOI] [PubMed] [Google Scholar]
- [11].Wolter NE, Siegele B, Cunningham MJ. Cystic cervical teratoma: a diagnostic and management challenge. Int J Pediatr Otorhinolaryngol 2017;95:97–100. [DOI] [PubMed] [Google Scholar]
- [12].Riedlinger WF, Lack EE, Robson CD, et al. Primary thyroid teratomas in children: a report of 11 cases with a proposal of criteria for their diagnosis. Am J Surg Pathol 2005;29:700–6. [DOI] [PubMed] [Google Scholar]
- [13].Tjalma WA. The value of AFP in congenital cervical teratoma. J Pediatr Surg 2003;38:1846. [DOI] [PubMed] [Google Scholar]
- [14].Alexander VRC, Manjaly JG, Pepper CM, et al. Head and neck teratomas in children—a series of 23 cases at Great Ormond Street Hospital. Int J Pediatr Otorhinolaryngol 2015;79:2008–14. [DOI] [PubMed] [Google Scholar]
- [15].Bhutta MF, Ching HY, Hartley BE. Cervico-thoracic teratoma masquerading as lymphatic malformation. J Laryngol Otol 2006;120:955–8. [DOI] [PubMed] [Google Scholar]
- [16].Brodsky JR, Irace AL, Didas A, et al. Teratoma of the neonatal head and neck: a 41-year experience. Int J Pediatr Otorhinolaryngol 2017;97:66–71. [DOI] [PubMed] [Google Scholar]
- [17].Ueno NT, Amato RJ, Ro JJ, et al. Primary malignant teratoma of the thyroid gland: report and discussion of two cases. Head Neck 1998;20:649–53. [DOI] [PubMed] [Google Scholar]


