Abstract
Ten years ago, endoscopic techniques began to prevail in clinical treatment of lumbar disc herniation (LDH), but to date, few studies have reported the clinical efficacy of percutaneous transforaminal endoscopic discectomy (PTED) in treating adolescent LDH. This study aimed to evaluate the surgical outcomes of PTED in treating adolescent patients with LDH.
Between June 2012 and June 2016, retrospective analysis of 43 adolescent patients diagnosed with single-segment LDH at spine surgery at the Second Affiliated Hospital of Anhui Medical University. The patients’ lower limb pain was evaluated using visual analogue scale (VAS) scores and the Oswestry Disability Index (ODI). The VAS is the most commonly-used quantitative method for assessing the degree of pain in clinical practice. The measurement method is to draw a 10 cm horizontal line on a piece of paper, 1 end of which is 0, indicating no pain, while the other end is 10, which means severe pain, and the middle part indicates different degrees of pain. The clinician then asks the patient to make a mark on the line to indicate the degree of pain based on how he or she feels. The ODI is the most widely-used assessment method internationally for lumbar or leg pain at present. The ODI questionnaire is composed of 10 questions, covering pain intensity, independent living, carrying, walking, sitting, standing, sleep, travel, sex, and social life. Every category comprises 6 options, with the highest score for each question being 5 points. Thus the 1st option is worth 0 points, the last option scores 5 points, and higher scores represent more serious dysfunction. Patient satisfaction was evaluated using the modified MacNab score. Clinical outcomes were measured preoperatively, and at 3 days, 6 months, and 12 months postoperatively.
All 43 patients were followed up for 12 to 24 months. The average follow-up time was 18.33 months. The VAS scores and ODI scores at 3 days, 6 months, and 12 months postoperatively were significantly lower than before surgery. The difference was statistically significant (P < .001). The differences in VAS scores and ODI scores at 3 days, 6 months, and 12 months after surgery were also statistically significant (P < .001). According to the modified MacNab criteria, 26 cases were rated excellent, 14 cases were good, and 3 cases were acceptable at the final follow-up, and 93.02% of these patients had excellent outcomes.
The PTED is an effective and safe surgical method for the treatment of adolescent patients with LDH, but high-quality randomized controlled trials are still required to further verify these findings.
Keywords: adolescent, lumbar disc herniation, percutaneous transforaminal endoscopic discectomy
1. Introduction
Lumbar disc herniation (LDH) is a common spinal disease, and trauma is the most important pathogenic factor in adolescents.[1] Most adolescent patients with LDH can be cured by conservative treatment. For adolescent patients for whom conservative treatment is ineffective, traditional fenestration discectomy (FD) is considered an effective surgical treatment strategy. Long-term follow-up, however, showed that there were still some patients with lower limb pain after traditional FD.[2] In the past few decades, with the rapid development of minimally-invasive techniques and endoscopic instruments, percutaneous transforaminal endoscopic discectomy (PTED) has come to be considered as a more effective treatment for adult LDH compared with traditional FD.[3,4] Therefore, the authors conjecture that PTED may also be an effective treatment for adolescent LDH. Besides, there have been few studies on the clinical efficacy of PTED in treating adolescent patients with LDH. Thus, this study was conducted to investigate the efficacy of PTED in treating adolescent LDH.
2. Patients and methods
2.1. Patients
Forty-three adolescent patients who were diagnosed with single-segment LDH between June 2012 and June 2016 in the Department of Spinal Surgery of the Second Affiliated Hospital of Anhui Medical University (China) were involved in this study. All patients had typical lumbar and leg pain or numbness symptoms and positive signs in the straight leg elevation test, and all showed obvious lumbar intervertebral disc herniation by magnetic resonance imaging (MRI). The diagnosis was confirmed when combined with the clinical performance. None of the patients showed any significant improvement in symptoms after at least 3 months of strict conservative treatment. Patients with lumbar infection, tumors, instability, or spondylolisthesis or other lumbar disorders were excluded.
3. Methods
3.1. Surgical procedures
The adolescent patients with lumbar disc herniation enrolled into our study were treated by PTED between June 2012 and June 2016. Our study protocol was approved by the ethics committee of the Second Affiliated Hospital of Anhui Medical University. To perform the PTED, the patient was placed in the lateral position. A soft cushion was placed beneath the waist causing it to protrude slightly towards the operative side, in order to increase the height of the operative intervertebral foramen. After the puncture site was marked using C-arm X-ray image intensifier guidance, the operation was performed under local anesthesia with 1% lidocaine, combined with analgesic drugs. The local anesthetic was injected above the iliac crest. When the puncture needle reached the ventral margin of the articular facet of the superior articular process, under guidance with a C-arm X-ray machine, then 2 to 3 mL of 1% lidocaine was locally injected. The puncture needle was removed and a guide wire was inserted. A 7 mm long incision was made along the puncture site and the work channel was gradually expanded. An intervertebral foramen mirror light source, camera and washing fluid were connected. The ligamentum flavum and the upper facet of the lower vertebral body were distinguished. An intervertebral foramen was formed with a circular saw under the microscope. This circular saw was then removed and the work sleeve was inserted. The soft tissue was cleaned using radio frequency coagulation under the microscope. The protruded intervertebral disc was removed with nucleus pliers under the microscope and sent to the pathology department. When the patient's self-feeling symptoms were relieved after decompression, a fiber ring was formed by radio frequency ablation. Hemostasis was performed using an endoscope, then the working sleeve was pulled out and the wound was sutured (Fig. 1).
Figure 1.
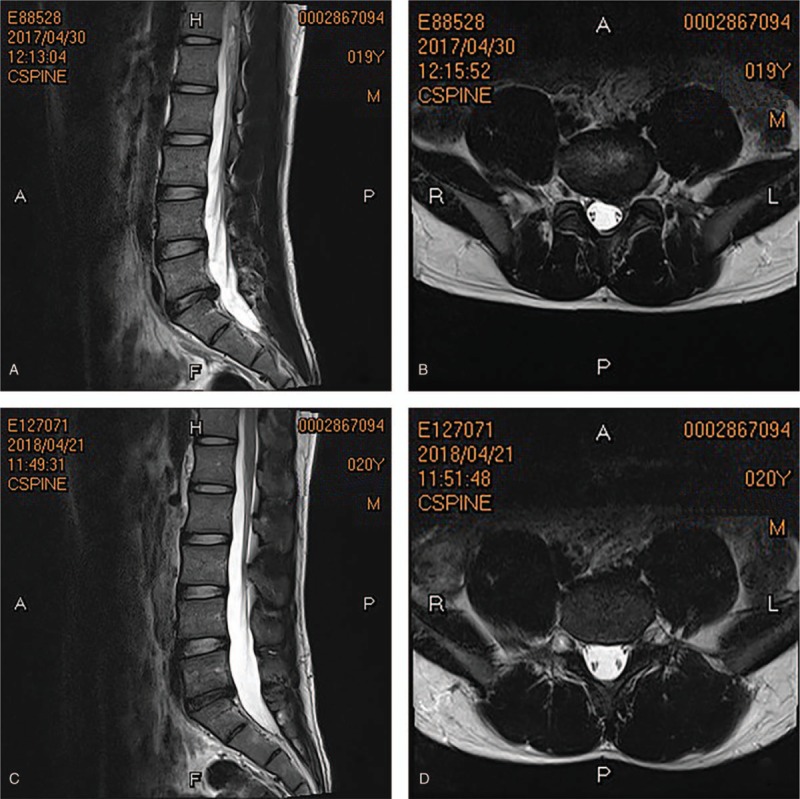
A 19-year-old male patient had a protrusion in the left portion of the L5/S1 intervertebral disc. (A) In the sagittal section, MRI showed an L5/S1 intervertebral disc protrusion on the left. (B) In the cross section, a protrusion could be seen in the left portion of the L5/S1 intervertebral disc, and the nerve roots were compressed. (C) One year after surgery, MRI showed no significant protrusion in the L5/S1 intervertebral disc. (D) One year after surgery, cross-sections showed no significant protrusion in the L5/S1 intervertebral discs, and the nerve roots were not compressed. MRI = magnetic resonance imaging.
3.2. Postoperative care
All patients accepted hormtwos and nutritional neurological drugs after surgery. Each patient was routinely given 5 to 10 mg dexamethasone for 1 to 3 days and 1 tablet each time, 3 times a day mecobalamine for 2 to 3 weeks after surgery. According to each patient's individual recovery, patients were allowed to get out of bed to exercise as appropriate under the protection of the waistline at 6 hours after surgery and to go home at 3 to 4 days after surgery. All patients were suggested to perform back muscle function exercises at 1 week after surgery, wear waist circumference within 1 month after operation, and to avoid strenuous activity within 3 months after operation.
3.3. Efficacy evaluation
Lower limb pain was evaluated using visual analogue scale (VAS) scores and the Oswestry Disability Index (ODI) preoperatively and at 3 days, 6 months, and 12 months postoperatively. The recovery of lumbar function was evaluated using the modified MacNab score at the final follow-up.
3.4. Statistical analysis
All results are expressed as mean ± standard deviation (SD). Data were statistically analyzed using statistical software SPSS 24.0. The obtained data were processed by statistical analysis and evaluated using T test. P < .05 was considered statistically significant.
4. Results
The operation was successfully completed in all 43 patients. All patients were followed up after surgery and complete clinical data were available. The average follow-up was 18.33 ± 3.24 months after surgery. No related complications occurred and there was no recurrence of LDH within 12 months after surgery. Of the 43 patients, 24 were males and 19 were females. Their ages ranged from 15 to 21 years old, with an average of 18.02 ± 1.67 years old. The average body height was 1.64 ± 0.06 m and the average body weight was 59.62 ± 6.63 kg. The lesions were located at L4/5 in 20 patients and at L5/S1 in 23 patients (Table 1). The VAS scores for lower limb pain were 6.98 ± 0.86 before surgery, 2.07 ± 0.77 at postoperative 3 days, 1.14 ± 0.74 at 6 months postoperatively, and 0.74 ± 0.69 at 12 months postoperatively (Fig. 2). The ODI scores for lower limb pain were 41.21 ± 2.68, 20.02 ± 2.97, 8.70 ± 2.67, and 2.91 ± 2.29 before surgery and at 3 days, 6 months, and 12 months postoperatively, respectively (Fig. 3). The differences in VAS scores and in ODI scores before and after surgery were statistically significant (P < .001). Furthermore, differences in VAS scores and in ODI scores at 3 days, 6 months, and 12 months after surgery were statistically significant (P < .001). The differences in VAS scores and in ODI scores between 6 months after surgery and 12 months after surgery were also statistically significant (P < .001). According to the modified MacNab criteria, the clinical efficacy was excellent in 26 patients, good in 14 patients, and acceptable in 3 patients at the final follow-up. According to the modified MacNab criteria, patients in whom the efficacy were both excellent and good accounted for 93.02%.
Table 1.
Pre-operative clinical data of all the patients.
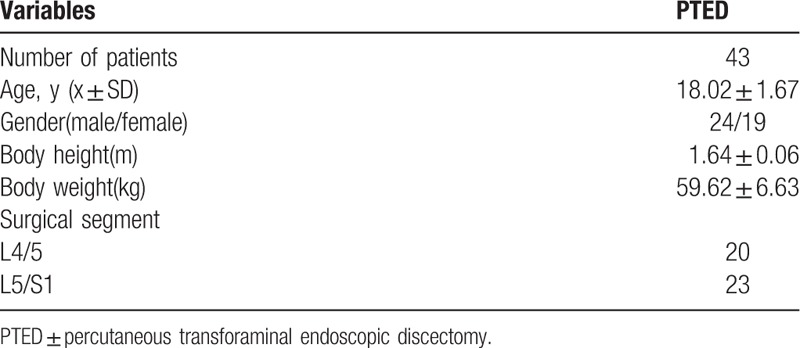
Figure 2.
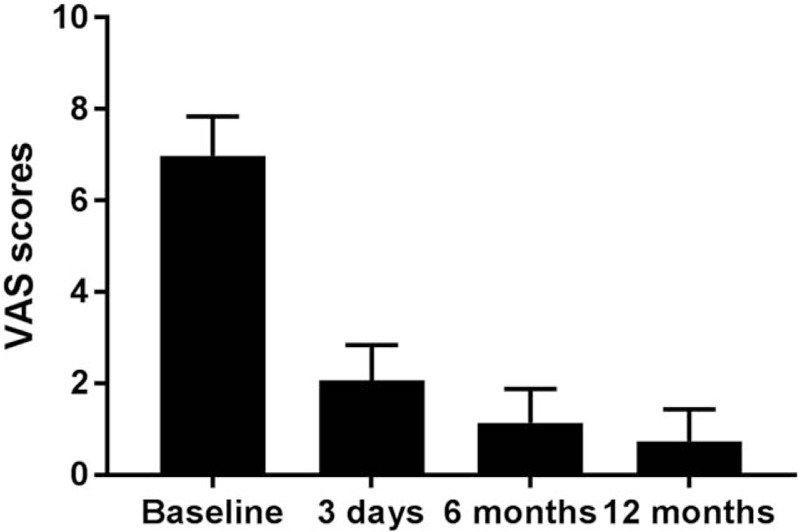
The VAS scores of lower limb pain at different time-points ① = Baseline, ② = 3 days, ③ = 6 months, ④ = 12 months, ① compared with ②③④, P < .01; ② compared with ③, P < .01; ② compared with ④, P < .01; ③ compared with ④, P < .01; baseline pre-operative outcome. VAS = visual analogue scale.
Figure 3.
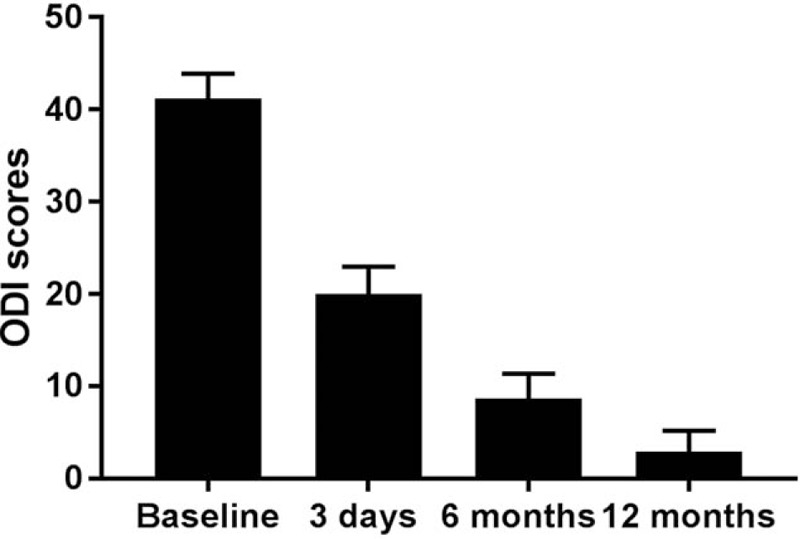
The ODI scores of lower limb pain at different time-points ① = Baseline, ② = 3 days, ③ = 6 months, ④ = 12 months, ① compared with ②③④, P < .01; ② compared with ③, P < .01; ② compared with ④, P < .01; ③ compared with ④, P < .01; baseline pre-operative outcome. ODI = Oswestry Disability Index.
5. Discussion
The most important finding of the study is that PTED is an effective and safe surgical method for the treatment of adolescent LDH. The prevalence of LDH has gradually increased in adolescents, reaching between 1 to 5%.[5] The main pathogenesis includes degeneration, genetic and developmental malformation and, especially, trauma.[6] These factors can lead to pain in a lower limb, which will seriously affect the patient's quality of life. Surgical treatment plays a crucial role in the treatment of LDH in adolescent patients who do not respond to conservative treatment.[7,8,9] With the maturation of the traditional FD, orthopedists have shifted their attention to the minimally-invasive technique which has the advantages of small surgical trauma and fast recovery after surgery.[10–12] In 1975, Hijikata et al[13] reported the use of percutaneous lumbar discectomy in the treatment of adult LDH. In 1997, Perez-Cruet et al[14] reported for the 1st time that LDH could be treated with micro-endoscopic discectomy. These 2 studies showed that minimally-invasive techniques had a definite effect on treatments of LDH and had many advantages compared with traditional FD. However, few publications reported the efficacy of PTED in the treatment of adolescent patients with LDH. Therefore, we conducted this study to evaluate the efficacy of PTED in the treatment of adolescent LDH. Our results suggest that this surgical procedure is an effective and safe way of treating adolescent patients with LDH.
The advantages of PTED are as follows: First, because the patient can be operated on under local anesthesia, doctors can communicate with patients at any time to avoid nerve damage. Second, muscle tissue is not extensively stripped, so patients recover faster after surgery. Third, the range of the surgical field is extended through the use of endoscopic techniques to effectively prevent endorhachis and nerve root injury, which greatly reduces the risk during the operation. Fourth, because the cone is not cut off and the joint is not damaged, postoperative lumbar instability is prevented.[15] Fifth, there is no significant interference with intraspinal tissue during the operation, thus avoiding significant bleeding in the spinal canal and preventing postoperative scar adhesion.
There are several limitations to this study. Firstly, this is a retrospective analysis rather than a prospective controlled study. Thus, high-quality randomized controlled trials will be required to further verify the efficacy of PTED. Secondly, the sample of patients was relatively small, which could affect the results of this study, and a larger sample size will be necessary to confirm the results. Finally, even though our results show that PTED is an effective surgical method for treating patients with adolescent LDH, studies comparing minimally-invasive surgery and open surgery should be carried out to verify the ideal surgical method for patients with adolescent LDH.
6. Conclusion
According to our results, ODI and VAS scores improved significantly after PTED. Based on our findings, PTED is an effective and safe surgical method in treating adolescent patients with LDH. Further prospective studies are required to confirm our results.
Acknowledgments
We would like to thank all the participants in the studies.
Author contributions
Conceptualization: Lei Chen.
Data curation: Ziyu Li, Dasheng Tian.
Formal analysis: Wei Liu, Qingning Li, Ziyu Li.
Methodology: Qingning Li, Juehua Jing.
Resources: Lei Chen, Dasheng Tian.
Software: Wei Liu, Qingning Li, Ziyu Li, Lei Chen.
Supervision: Dasheng Tian, Juehua Jing.
Validation: Lei Chen.
Writing – original draft: Wei Liu.
Writing – review & editing: Wei Liu, Juehua Jing.
Footnotes
Abbreviations: FD = fenestration discectomy, LDH = lumbar disc herniation, ODI = Oswestry Disability Index, PTED = percutaneous transforaminal endoscopic discectomy, VAS = visual analogue scale.
Wei Liu and Qingning Li contributed equally to this work.
This work was supported by the National Natural Science Foundation of China (81671204).
The authors have no conflicts of interest to disclose.
References
- [1].Ozgen S, Konya D, Toktas OZ, et al. Lumbar disc herniation in adolescence. Pediatr Neurosurg 2007;43:77–81. [DOI] [PubMed] [Google Scholar]
- [2].Wang H, Cheng J, Xiao H, et al. Adolescent lumbar disc herniation: experience from a large minimally invasive treatment centre for lumbar degenerative disease in Chongqing, China. Clin Neurol Neurosurg 2013;115:1415–9. [DOI] [PubMed] [Google Scholar]
- [3].Ahn Y, Lee SH, Lee JH, et al. Transforaminal percutaneous endoscopic lumbar discectomy for upper lumbar disc herniation: clinical outcome, prognostic factors, and technical consideration. Acta Neurochir (Wien) 2009;151:199–206. [DOI] [PubMed] [Google Scholar]
- [4].Jang JS, An SH, Lee SH. Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech 2006;19:338–43. [DOI] [PubMed] [Google Scholar]
- [5].Smorgick Y, Floman Y, Millgram MA, et al. Mid- to long-term outcome of disc excision in adolescent disc herniation. Spine J 2006;6:380–4. [DOI] [PubMed] [Google Scholar]
- [6].Benifla M, Melamed I, Barrelly R, et al. Unilateral partial hemilaminectomy for disc removal in a 1-year-old child. J Neurosurg Pediatr 2008;2:133–5. [DOI] [PubMed] [Google Scholar]
- [7].Kurth AA, Rau S, Wang C, et al. Treatment of lumbar disc herniation in the second decade of life. Eur Spine J 1996;5:220–4. [DOI] [PubMed] [Google Scholar]
- [8].Fakouri B, Nnadi C, Boszczyk B, et al. When is the appropriate time for surgical intervention of the herniated lumbar disc in the adolescent? J Clin Neurosci 2009;16:1153–6. [DOI] [PubMed] [Google Scholar]
- [9].Youn-Soo K, Il-Jung P, Kee-Won R, et al. Surgical excision of the lumbar disc herniation in elementary school age. Asian Spine J 2009;3:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Li X, Hu Z, Cui J, et al. Percutaneous endoscopic lumbar discectomy for recurrent lumbar disc herniation. Int J Surg 2016;27:8–16. [DOI] [PubMed] [Google Scholar]
- [11].Kim HS, Yudoyono F, Paudel B, et al. Analysis of clinical results of three different routes of percutaneous endoscopic transforaminal lumbar discectomy for lumbar herniated disk. World Neurosurg 2017;103:442–8. [DOI] [PubMed] [Google Scholar]
- [12].Kim CH, Chung CK, Choi Y, et al. The selection of open or percutaneous endoscopic lumbar discectomy according to an age cut-off point: nationwide cohort study. Spine 2015;40:E1063–70. [DOI] [PubMed] [Google Scholar]
- [13].Hijikata S, Yamagishi M, Nakayma T. Percutaneous discectomy: a new treatment method for lumbar disc herniation. J Tokyo Den Hosp 1975;5:39–41. [Google Scholar]
- [14].Perezcruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery 2002;51:129–36. [PubMed] [Google Scholar]
- [15].Ahn Y, Lee SH, Park WM, et al. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:326–32. [DOI] [PubMed] [Google Scholar]


