Abstract
Background:
This meta-analysis aimed to explore the overall effect and safety of anterior laparoscopic surgery versus conventional open surgery for patients with colorectal cancer based on eligible randomized controlled trials (RCTs), especially the difference in the postoperative incidence of deep venous thrombosis (DVT).
Methods:
PubMed, Cochrane, and Embase were searched based on keywords to identify eligible studies before February 2018. Only RCTs were eligible. We analyzed the main outcomes using the relative risk (RR) or mean difference (MD) along with 95% confidence interval (95% CI).
Results:
In this meta-analysis, we analyzed a total of 24 studies with 4592 patients in the laparoscopic surgery group and 3865 patients in the open surgery group. The results indicated that compared with the open surgery, laparoscopic surgery significantly decreased estimated blood loss (SMD: −1.14, 95%CI: −1.70 to −0.57), hospital stay (SMD: −1.12, 95%CI: −1.76 to −0.47), postoperative mortality (RR: 0.60, 95%CI: 0.41–0.86) and postoperative complication (RR: 0.83, 95%CI: 0.72–0.95). However, the operative time (WMD: 40.46, 95%CI: 35.94–44.9) was statistically higher in the laparoscopic surgery group than the open surgery group, and there was no significant difference in the incidence of DVT between the 2 groups (RR: 0.96, 95%CI: 0.46–2.02).
Conclusion:
Laparoscopic surgery is superior to open surgery for patients with colorectal cancer. But the 2 surgeries showed no significant difference in the incidence of DVT.
Keywords: colorectal cancer, laparoscopic surgery, meta-analysis, open surgery
1. Introduction
Colorectal cancer is among the top 3 common tumors worldwide,[1,2] and its morbidity has dramatically increased in Asians. Currently, surgery remain the best treatment for colorectal cancer, which includes conventional laparoscopic surgery, hand-assisted laparoscopic surgery, robotic surgery, single-pore laparoscopic surgery, and open surgery.[3,4]
Laparoscopic surgery combines features of the minimally invasive technique and open surgery. Compared with conventional open surgery, laparoscopic surgery has advantages such as smaller incision length, smaller blood loss, and less pain. However, previous studies demonstrated that laparoscopic surgery had some limitations like longer operative time and longer learning curve for surgeons.[6,7] For larger tumors, laparoscopic surgery is less effective due to the lack of tactile feedback and inadequate exposure.[7,8] Up to 2015, the National Comprehensive Cancer Network (NCCN) still did not recommend laparoscopic surgery for colorectal cancer.[9] Deep venous thrombosis (DVT) is one of the most common peripheral vascular diseases, and the post-thrombosis syndrome can influence the daily-life for a long time. Surgery can increase the incidence of DVT. In this study, we explored the influence of open surgery and laparoscopic surgery on the incidence of DVT.
In this meta-analysis, we explored the overall effect and safety of open surgery laparoscopic surgery for patients with colorectal cancer based on qualified RCTs.
2. Methods
2.1. Ethics statement
Ethics approval was waived because this study did not involve any human subjects or animals.
2.2. Literature search
Cochrane library, PubMed, and Embase database were identified for all the qualified studies up to February 2018 on open surgery versus laparoscopic surgery for patients with colorectal cancer. We also searched relevant publications as well as the reference materials. The literature search process was performed by 2 reviewers separately. Any arising disagreement was settled via the help of a third researcher.
2.3. Study selection
Studies should meet the following inclusion criteria: randomized controlled trials; the included patients were diagnosed with colorectal cancer; the test group were treated by laparoscopic surgery, and the control group were treated by open surgery; the outcomes included operative time, blood loss, hospital stay, wound infection, DVT, postoperative mortality, and postoperative complication.
Studies were excluded due to the following criteria: duplicate publications, or shared result; economic analysis, case report, expert comment, theoretical research, meta-analysis, systematic review and conference report; and irrelevant outcomes.
Two investigators identified all studies based on the predefined criteria independently. Any difference was settled by discussion via the aid of a third researcher.
2.4. Data collection and quality assessment
We extracted data from the included studies. The basic information was regarded as the first part: names of authors, publication year, the Jadad score, sample size, country, gender, and age. The second part was clinical outcomes: operative time, blood loss, hospital stay, wound infection, DVT, postoperative mortality, and postoperative complication. The Jadad score checklist was used to appraise the quality of the included studies. We evaluated all the RCTs from the 5 items: double blinding, detail of access and exit, randomized sequence, statement of randomization, and description of double blinding. Studies with a score <3 represented low-quality and high bias risks, studies with a score >3 indicated high-quality trial. The 2 investigators performed the mentioned process separately. A third investigator resolved differences by discussion.
2.5. Data synthesis and data analysis
We performed data synthesis as well as analysis using STATA 10.0 (Texas). Additionally, I2 tests and Chi-squared test were utilized to determine the heterogeneity of clinical trial results to further decide the model for analyses (the random-effects model or the fixed-effects model). When the I2 test value was >50% and Chi-squared test P-value was <.05, heterogeneity was defined to be high and the random-effects model was utilized. When the I2 test value was less than 50% and Chi-squared test P-value was larger than .05, heterogeneity data were defined to be acceptable and the fixed-effects model was utilized. Mean ± standard deviation and mean difference (MD) were used to express and analyze continuous variables, respectively. Categorical data were presented as percentages and analyzed by relative risk (RR) or odds ratio (OR). DVT, postoperative mortality, and postoperative complication were analyzed by RR and 95%CI. Operative time, blood loss, and hospital stay were analyzed by MD and 95%CI. The primary endpoint of our research is postoperative mortality to evaluate the clinical efficacy of laparoscopic surgery and conventional open surgery. The indicators about operation contain operative time and hospital days. Indexes about adverse events include blood loss, DVT, and postoperative complication.
3. Results
3.1. Study characteristics
Totally, we identified 1347 publications based on index words. After screening abstracts or titles, we excluded 1269 publications, leaving 78 publications for further screening. During full-text screening, a total of 54 publications were excluded due to the following reasons: nonrandomized studies (22), no clinical outcomes (21), and theoretical research or review (11). Finally, in this meta-analysis, 24 studies[10–33] were included with 4592 patients in the laparoscopic surgery group and 3865 patients in the open surgery group. Figure 1 shows the selection process.
Figure 1.
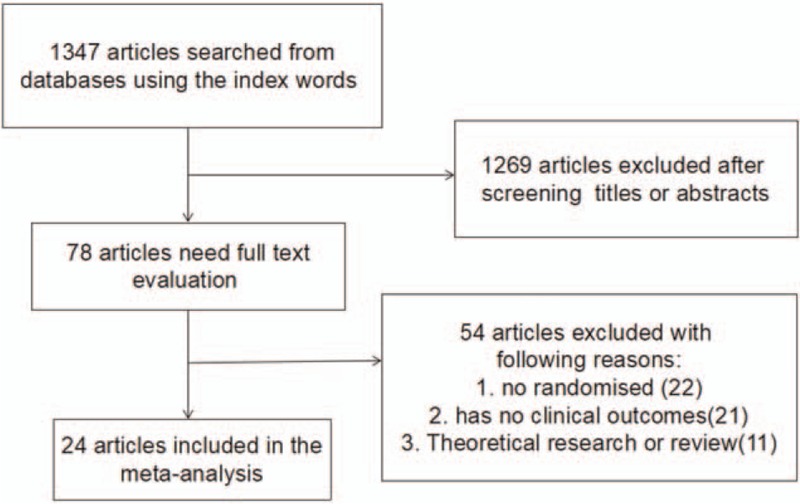
The flow diagram of the literature search and selection process.
Table 1 summarizes the main characteristics of the included studies. The countries or districts of studies included United States, Japan, Germany, China, Hong Kong, Denmark, Singapore, Spain, Italy, Taiwan, Australia, Europe, the Netherlands, France, UK, and Greece. The main Jadad score was 4.54, indicating that the included studies were high quality. The mean age of all the included studies was more than 50 years old.
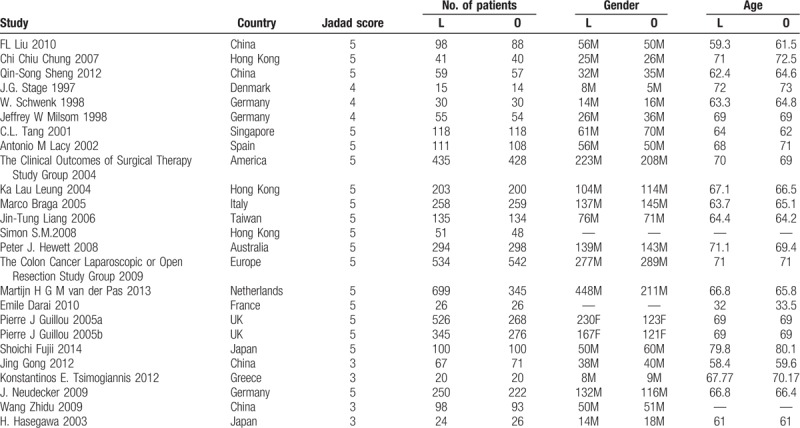
Table 1.
The basic characteristics description of included studies.
3.2. Operative time
Twenty-four studies with 4592 subjects in the laparoscopic surgery group and 3865 subjects in the open surgery group provided data on operative time. Based on the I2 test (I2 = 91.7%) and Chi-squared test (P = .000), we chose the random effects model to analyze operative time due to high variability. The pooled results showed that the laparoscopic surgery group dramatically increased operative time compared with the open surgery group (WMD: 40.46, 95%CI: 35.94–44.98, Fig. 2).
Figure 2.
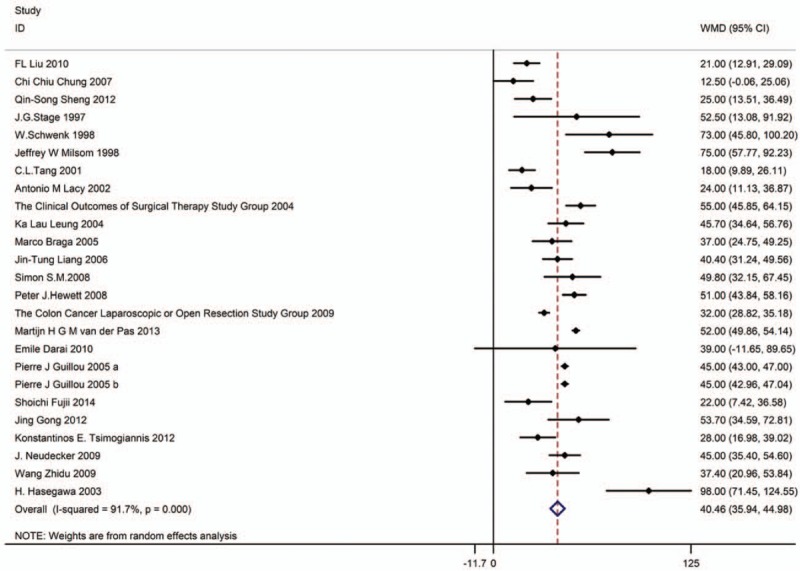
Forest plot showing operative time of laparoscopic surgery versus open surgery.
3.3. Blood loss
Seventeen studies with 2199 subjects in the open surgery group and 2568 subjects in the laparoscopic surgery group reported data on blood loss. Based on the I2 test (I2 = 98.6%) and Chi-squared test (P = .000), the random effects model was adopted to analyze blood loss. The pooled results showed that the laparoscopic surgery group dramatically decreased blood loss compared with the open surgery group (SMD: −1.14, 95%CI: −1.70 to −0.57, Fig. 3).
Figure 3.
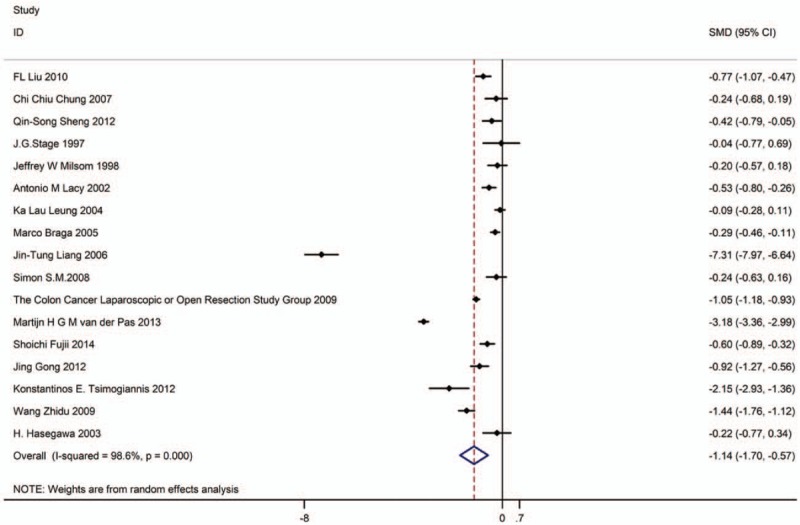
Forest plot showing blood loss that laparoscopic surgery versus open surgery.
3.4. Hospital stay
Thirteen studies with 1567 subjects in the open surgery group and 1948 subjects in the laparoscopic surgery group provided data about on hospital stay. Based on the I2 test (I2 = 98.4%) and Chi-squared test (P = .000), we chose the random effects model to analyze hospital stay. The pooled results showed that the laparoscopic surgery group significantly decreased hospital stay compared with the open surgery group (SMD: −1.12, 95%CI: −1.76 to −0.47, Fig. 4).
Figure 4.
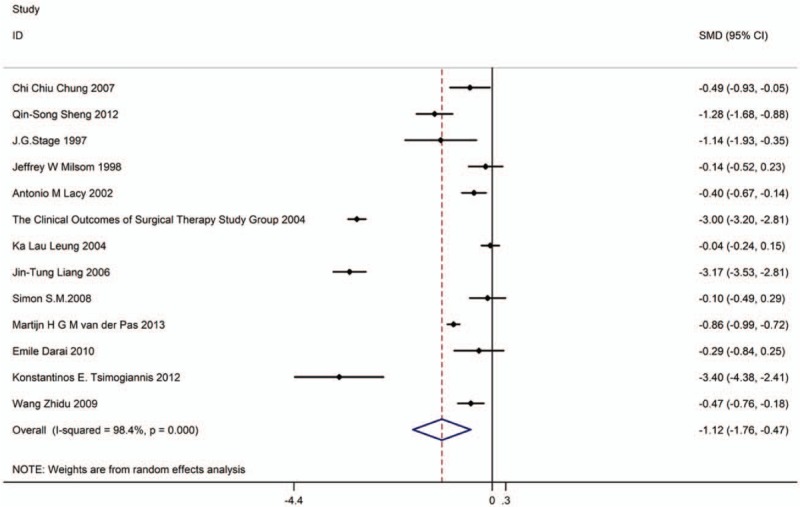
Forest plot showing hospital stay of laparoscopic surgery versus open surgery.
3.5. DVT
Five studies with 1218 patients in the open surgery group and 1577 patients in the laparoscopic surgery group were included. Based on the I2 test (I2 = 0.0%) and Chi-squared test (P = .453), the fixed effects model was used to analyze DVT. The pooled results showed no significant difference in the incidence of DVT between the 2 groups (RR: 0.96, 95%CI: 0.46–2.02, Fig. 5).
Figure 5.
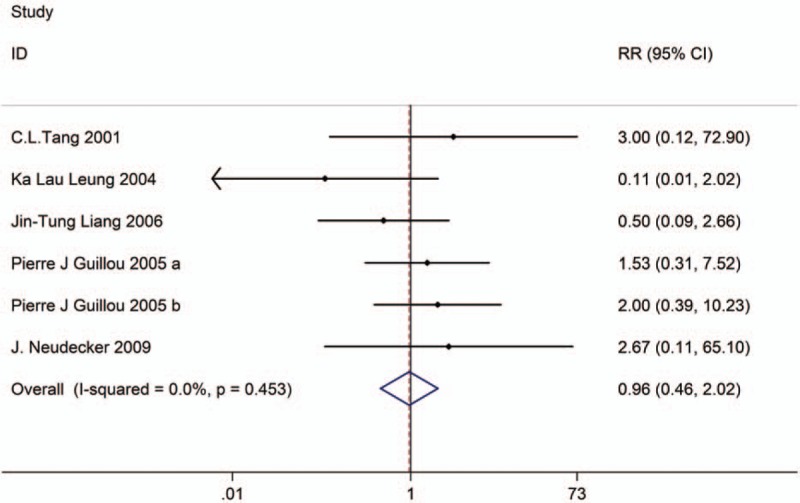
Forest plot showing DVT of laparoscopic surgery versus open surgery. DVT = deep venous thrombosis.
3.6. Postoperative mortality
Nine studies with 2108 patients in the open surgery group and 2470 patients in the laparoscopic surgery group provided data on postoperative mortality. Based on the I2 test (I2 = 0.0%) and Chi-squared test (P = .584), we chose the fixed effects model to analyze postoperative mortality. The pooled results showed that the laparoscopic surgery group significantly decreased postoperative mortality compared with the open surgery group (RR: 0.60, 95%CI: 0.41–0.86, Fig. 6).
Figure 6.
Forest plot showing postoperative complication of laparoscopic surgery versus open surgery.
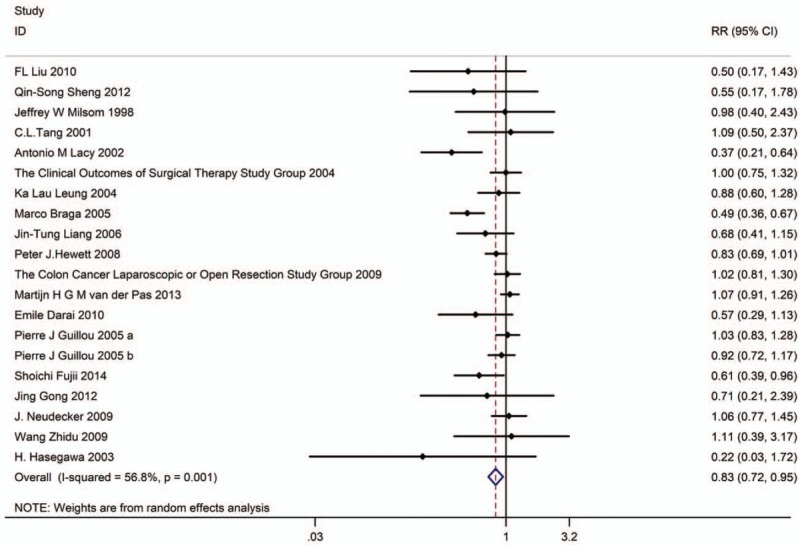
3.7. Postoperative complication
Nineteen studies with 3713 patients in the open surgery group and 4435 patients in the laparoscopic surgery group provided data on postoperative complications. Based on the I2 test (I2 = 56.8%) and Chi-squared test (P = .001), we chose the random effects model to analyze postoperative complications. The pooled results showed that the laparoscopic surgery group significantly decreased the incidence of postoperative complication compared with the open surgery group (RR: 0.83, 95%CI: 0.72–0.95, Fig. 6).
3.8. Quality and bias assessment
According to the inclusion and exclusion criteria, 24 articles were included in this meta-analysis. Quality assessment and potential bias were accessed by funnel plot, Begg's and Mazumdar's rank test, and Egger's test. The funnel plot for log WMD in operative time of the included studies was notably symmetrical, suggesting that there was no significant publication bias (Fig. 7). Moreover, significant symmetry was determined using Begg's and Mazumdar's rank test (Z = 0.72, P = .469). However, Egger's test showed no significant publication bias (P = .276).
Figure 7.
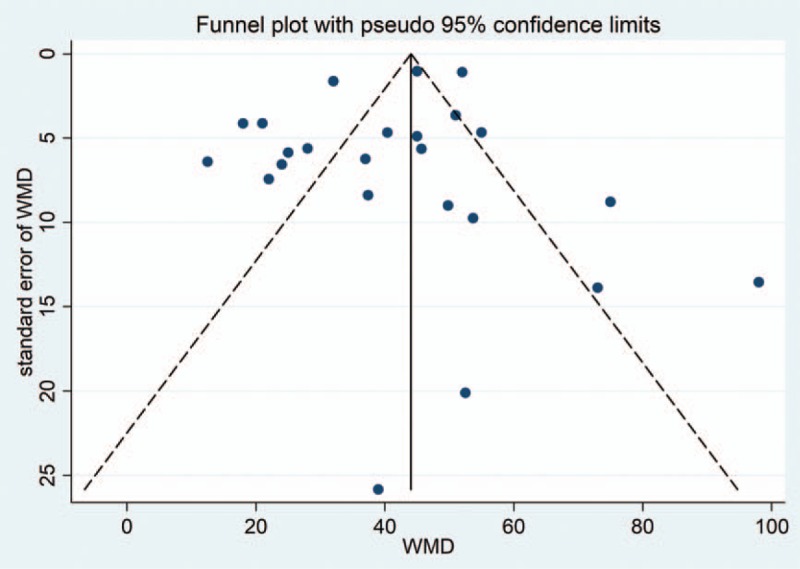
Funnel plot of studies in the meta-analysis.
4. Discussion
Colorectal cancer (including colorectal cancer, rectal cancer, and anal cancer) is a common malignant tumor of the digestive tract. It is the third highest malignant tumor in men and the second highest malignant tumor in women worldwide. Colorectal cancer is the most common malignant tumor following lung cancer and breast cancer, which poses a serious threat to human health. In Western developed countries, the incidence of colorectal cancer tends to be stable or even declining with early intervention in the population. However, the incidence of colorectal cancer in the world is still increasing, especially in Japan, South Korea, China, and some Eastern Europe.
In our results, laparoscopic surgery group cost more operative time, less blood loss and less hospital stay than the open surgery group. The results also showed that the laparoscopic surgery group significantly decreased postoperative mortality compared with the open surgery group. At the same time, laparoscopic surgery group significantly decreased the incidence of postoperative complication compared with the open surgery group. Our study have the similar conclusion with other searches.[34,35] Besides, laparoscopic surgery group significantly decreased the incidence of postoperative complication compared with the open surgery group.
There were some similar meta-analyses of open surgery versus laparoscopic surgery for patients with colorectal cancer. Tong et al[34] summarized 9 clinical trials and supported that laparoscopic surgery appears to be a better alternative therapy for patients with colorectal cancer as compared to the open surgery. Zhang et al[35] summarized fifteen publications which were published between 2007 and 2017, and reported that hand-assisted laparoscopic surgery (HALS) was associated with shorter hospital days, postoperative hospital duration and so on. No difference was observed in the number of lymph nodes harvested, blood transfusion and so on.
However, in ASCOZOG6051 and ALACART studies,[36,37] they reported that laparoscopy in rectal cancer was not as safe as open surgery. This conclusion is different from our research, which is worth further study.
Admittedly, this meta-analysis had several limitations, such as: differences among patients in the mentioned predefined criteria. Patients’ conditions were different in different studies; the surgical techniques in different studies are varied. We used pooled data for further analysis, and individual data were unavailable, which limited for a more comprehensive analysis. Postoperative DVT prophylaxis was not specifically evaluated. The differentiation in types of neoplasms could be analyzed in the future, since the related data was not enough in this article. Nonetheless, the main Jadad score of the included RCTs was more than 3, and no significant publication bias was found among the study, which confirmed our findings.
In conclusion, this systematic review and meta-analysis indeed revealed that laparoscopic surgery has several advantages in decreasing blood loss, hospital stay, postoperative mortality, as well as postoperative complication. Therefore, laparoscopic surgery could be a more effective therapy for patients with colorectal cancer.
Author contributions
Conceptualization: Wei Ye.
Data curation: Wei Ye.
Formal analysis: Zhi-Li Liu.
Methodology: Zhi-Li Liu.
Project administration: Rong Zeng.
Validation: Rong Zeng.
Writing – original draft: Xiao-Jun Song, Chang-Wei Liu.
Writing – review & editing: Xiao-Jun Song, Chang-Wei Liu.
Footnotes
Abbreviations: DVT = deep venous thrombosis, NCCN = National Comprehensive Cancer Network.
The authors have no conflicts of interest to disclose.
References
- [1].Fakih MG. Metastatic colorectal cancer: current state and future directions. J Clin Oncol 2015;33:1809–24. [DOI] [PubMed] [Google Scholar]
- [2].Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359–386. [DOI] [PubMed] [Google Scholar]
- [3].Wu QB, Wang M, Hu T, et al. Prognostic role of the lymphocyte-to-monocyte ratio in patients undergoing resection for nonmetastatic rectal cancer. Medicine (Baltimore) 2016;95:e4945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chan DK, Chong CS, Lieske B, et al. Laparoscopic resection for rectal cancer: what is the evidence? Biomed Res Int 2014;2014:347810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sjoerdsma W, Meijer DW, Jansen A, et al. Comparison of efficiencies of three techniques for colon surgery. J Laparoendosc Adv Surg Tech A 2000;10:47–53. [DOI] [PubMed] [Google Scholar]
- [6].Pendlimari R, Holubar SD, Pattan-Arun J, et al. Hand-assisted laparoscopic colon and rectal cancer surgery: feasibility, short-term, and oncological outcomes. Surgery 2010;148:378–85. [DOI] [PubMed] [Google Scholar]
- [7].Yang I, Boushey RP, Marcello PW. Hand-assisted laparoscopic colorectal surgery. Tech Coloproctol 2013;17suppl 1:S23–7. [DOI] [PubMed] [Google Scholar]
- [8].Kang JC, Chung MH, Chao PC, et al. Hand-assisted laparoscopic colectomy vs open colectomy: a prospective randomized study. Surg Endosc 2004;18:577–81. [DOI] [PubMed] [Google Scholar]
- [9].Liu Y, Yao H, Gao G. [Review for the NCCN clinical guideline in oncology of rectal cancer on surgical treatment from 2005 to 2015]. Zhonghua Wai Ke Za Zhi 2015;53:68–71. [PubMed] [Google Scholar]
- [10].Liu FL, Lin JJ, Ye F, et al. Hand-assisted laparoscopic surgery versus the open approach in curative resection of rectal cancer. J Int Med Res 2010;38:916–22. [DOI] [PubMed] [Google Scholar]
- [11].Chung CC, Ng DC, Tsang WW, et al. Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg 2007;246:728–33. [DOI] [PubMed] [Google Scholar]
- [12].Sheng QS, Lin JJ, Chen WB, et al. Hand-assisted laparoscopic versus open right hemicolectomy: short-term outcomes in a single institution from China. Surg Laparosc Endosc Percutan Tech 2012;22:267–71. [DOI] [PubMed] [Google Scholar]
- [13].Stage JG, Schulze S, Moller P, et al. Prospective randomized study of laparoscopic versus open colonic resection for adenocarcinoma. Br J Surg 1997;84:391–6. [PubMed] [Google Scholar]
- [14].Schwenk W, Bohm B, Haase O, et al. Laparoscopic versus conventional colorectal resection: a prospective randomised study of postoperative ileus and early postoperative feeding. Langenbecks Arch Surg 1998;383:49–55. [DOI] [PubMed] [Google Scholar]
- [15].Milsom JW, Bohm B, Hammerhofer KA, et al. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 1998;187:46–54. discussion 54-45. [DOI] [PubMed] [Google Scholar]
- [16].Tang CL, Eu KW, Tai BC, et al. Randomized clinical trial of the effect of open versus laparoscopically assisted colectomy on systemic immunity in patients with colorectal cancer. Br J Surg 2001;88:801–7. [DOI] [PubMed] [Google Scholar]
- [17].Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 2002;359:2224–9. [DOI] [PubMed] [Google Scholar]
- [18].Nelson H, Sargent DJ, Wieand HS, et al. Clinical Outcomes of Surgical Therapy Study G. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–9. [DOI] [PubMed] [Google Scholar]
- [19].Leung KL, Kwok SP, Lam SC, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 2004;363:1187–92. [DOI] [PubMed] [Google Scholar]
- [20].Braga M, Vignali A, Zuliani W, et al. Laparoscopic versus open colorectal surgery: cost-benefit analysis in a single-center randomized trial. Ann Surg 2005;242:890–5. discussion 895-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Liang JT, Huang KC, Lai HS, et al. Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: a randomized controlled trial. Ann Surg Oncol 2007;14:109–17. [DOI] [PubMed] [Google Scholar]
- [22].Ng SS, Leung KL, Lee JF, et al. Laparoscopic-assisted versus open abdominoperineal resection for low rectal cancer: a prospective randomized trial. Ann Surg Oncol 2008;15:2418–25. [DOI] [PubMed] [Google Scholar]
- [23].Hewett PJ, Allardyce RA, Bagshaw PF, et al. Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg 2008;248:728–38. [DOI] [PubMed] [Google Scholar]
- [24].Buunen M, Veldkamp R, Hop WC, et al. Colon Cancer Laparoscopic or Open Resection Study G. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 2009;10:44–52. [DOI] [PubMed] [Google Scholar]
- [25].Fujii S, Ishibe A, Ota M, et al. Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 2014;28:466–76. [DOI] [PubMed] [Google Scholar]
- [26].van der Pas MH, Haglind E, Cuesta MA, et al. Group COcLoORIS. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210–8. [DOI] [PubMed] [Google Scholar]
- [27].Gong J, Shi DB, Li XX, et al. Short-term outcomes of laparoscopic total mesorectal excision compared to open surgery. World J Gastroenterol 2012;18:7308–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tsimogiannis KE, Tellis CC, Tselepis AD, et al. Toll-like receptors in the inflammatory response during open and laparoscopic colectomy for colorectal cancer. Surg Endosc 2012;26:330–6. [DOI] [PubMed] [Google Scholar]
- [29].Darai E, Dubernard G, Coutant C, et al. Randomized trial of laparoscopically assisted versus open colorectal resection for endometriosis: morbidity, symptoms, quality of life, and fertility. Ann Surg 2010;251:1018–23. [DOI] [PubMed] [Google Scholar]
- [30].Neudecker J, Klein F, Bittner R, et al. Short-term outcomes from a prospective randomized trial comparing laparoscopic and open surgery for colorectal cancer. Br J Surg 2009;96:1458–67. [DOI] [PubMed] [Google Scholar]
- [31].Wang ZD, Wu ZY, Li Y, et al. Clinical efficacy comparison between laparoscopy and open radical resection for 191 advanced colorectal cancer patients. Zhonghua Wei Chang Wai Ke Za Zhi 2009;12:368–70. [PubMed] [Google Scholar]
- [32].Guillou PJ, Quirke P, Thorpe H, et al. group MCt. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718–26. [DOI] [PubMed] [Google Scholar]
- [33].Hasegawa H, Kabeshima Y, Watanabe M, et al. Randomized controlled trial of laparoscopic versus open colectomy for advanced colorectal cancer. Surg Endosc 2003;17:636–40. [DOI] [PubMed] [Google Scholar]
- [34].Tong G, Zhang G, Liu J, et al. A meta-analysis of short-term outcome of laparoscopic surgery versus conventional open surgery on colorectal carcinoma. Medicine (Baltimore) 2017;96:e8957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Zhang X, Wu Q, Gu C, et al. Hand-assisted laparoscopic surgery versus conventional open surgery in intraoperative and postoperative outcomes for colorectal cancer: An updated systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e7794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Davies L, Gebski V, Hague W, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 2015;314:1356–63. [DOI] [PubMed] [Google Scholar]
- [37].Reibetanz J, Germer CT. Pathological outcomes after laparoscopic and open surgery for rectal cancer: The ALaCaRT multicenter trial. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 2015;87:72. [DOI] [PubMed] [Google Scholar]


