Abstract
Rationale:
Consumption of oral contraceptive pills (OCP) is a known risk factor for cerebral venous sinus thrombosis (CVST) among women. Development of dural arteriovenous fistula (dAVF) afterwards was very uncommon. We present a rare chronic complication of development of dAVF after CVST.
Patient concerns:
A 22-year-old woman suffered headache for a week. She was then admitted into our hospital.
Diagnosis:
Contrast enhanced magnetic resonance venography (MRV) demonstrated the thrombosis of the left transverse-sigmoid sinus the second day.
Interventions:
The intravenous thrombolysis was carried out. As the symptoms improved, the patient was discharged, while the treatment with oral dabigatran continued. However, 3 months after the onset, magnetic resonance imaging (MRI) showed swelling brainstem, and digital subtraction angiography (DSA) confirmed a dAVF. Clipping of the fistula was conducted, and her clinical symptoms improved gradually.
Outcomes:
The patient was transferred to rehabilitation center later, and received follow-up care.
Lessons:
When a patient taking OCP and suffering from a sudden headache, a clinical suspicion of possible CVST should always arise to avoid the onset of dAVF as soon as possible.
Keywords: cerebral venous sinus thrombosis (CVST), dural arteriovenous fistula (dAVF), oral contraceptive pills (OCP)
1. Introduction
Cerebral venous sinus thrombosis (CVST) is a rare form of venous thromboembolism with an estimated annual incidence rate round 3∼7/1,000,000.[1] The incidence rate is higher among women,[2] especially in the Asian area.[3] The risks for CVST include irregular menstruation, pregnancy, trauma, surgery, postpartum state, and hormonal changes in young women, and the patients often suffer non-specific headache.[4,5] In addition, consumption of oral contraceptive pills (OCP) is a known risk factor for CVST among women.[6]
Development of dural arteriovenous fistula (dAVF) after CVST was very uncommon. dAVFs could either be acute or chronic complications.[1] We present a case of chronic development of dAVF after CVST with OCP to raise the awareness of the disease in clinical management.
2. Case report
A 22-year-old woman suffered severe headache for 1 week. She had a history of consuming OCP for more than 2 months. Head computed tomography (CT) scan displayed the left temporal lobar hemorrhage [Fig. 1]. Laboratory tests revealed slightly elevated levels of C-reactive protein (CRP,12.6 mg/L) and D-dimers (2.23 μL/mL), and the cranial magnetic resonance imaging (MRI) displayed a local area of hemorrhagic infarction and edema in the temporal lobe [Fig. 2]. In view of clinical suspicion of CVST, on the second day, contrast enhanced magnetic resonance venography (MRV) and T1 contrast-enhanced image demonstrated the thrombosis of the left transverse-sigmoid sinus and internal jugular vein [Figs. 3 and 4]. The intravenous thrombolysis was conducted with warfarin and heparin. The patient was then discharged as the symptoms improved, and at that time the left transverse-sigmoid sinus was still not apparent, and the left internal jugular vein was small. A month later, follow-up MRI examination showed that her left transverse-sigmoid sinus was still not recanalized, and the left temporal lobe was softened on T2WI [Fig. 5]. Oral dabigatran was taken for continuing treatment. However, 3 months after the onset, the patient had a progressively paroxysmal dizziness, deteriorated nausea and vomiting. After her admission, MRI showed edema within brain stem on T2WI, and displayed obvious enhancement after contrast injection. Edema and mass effect was mild [Figs. 6 and 7], and MR angiography (MRA) was normal. At first, this case was misdiagnosed as demyelination or encephalitis. The clinical symptoms of the patient aggravated rapidly with choking, hoarseness and lip skewing to the left. Digital subtraction angiography (DSA) confirmed a dAVF fed by the left occipital artery and drained into the left sigmoid sinus [Fig. 8]. These characteristics corresponded to the hypointensity in the region of MRI T2. The patient was then transferred to neurosurgery. Subsequently, clipping of the fistula was conducted [Fig. 9]. As the postoperative course such as mental and speaking symptoms improved gradually, the patient was transferred to rehabilitation center. Five months later, the patient's clinical symptoms improved significantly, and MRI examination showed a little old hemorrhage in the brain stem and left cerebellar hemisphere. MRV revealed that her left transverse-sigmoid sinus was smaller compared with the previous images, and the AVF was resolved. This case report was approved by Nanjing Brain Hospital of Nanjing Medical University Research Ethics Board, and informed written consent for publication was obtained from the patient.
Figure 1.

The head unenhanced CT scanning of a 22-year-old woman showed scattered minor hemorrhages in the left temporal lobe.
Figure 2.
Focal bleeding-infarction and edema on axial T2 magnetic resonance image (MRI).
Figure 3.
The thrombosis of the left transverse-sigmoid sinus on T1WI after contrast injection.
Figure 4.
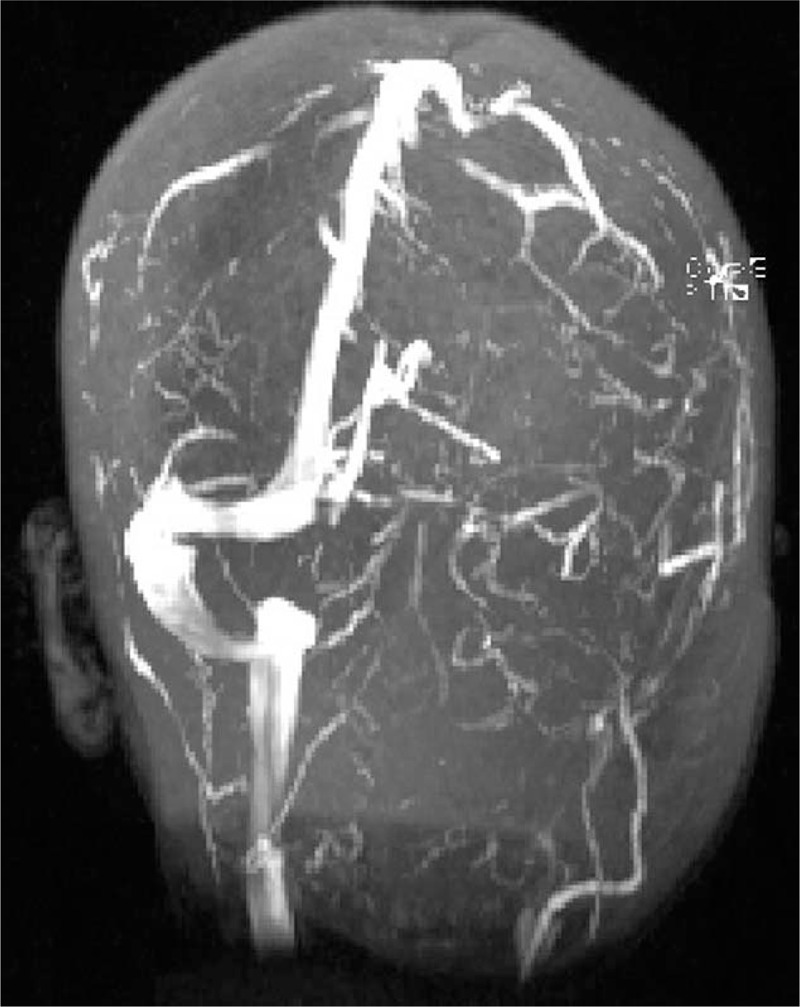
Cerebral magnetic resonance venography (MRV) demonstrated left transverse-sigmoid sinus thrombosed and the left sinus was smaller than the right.
Figure 5.
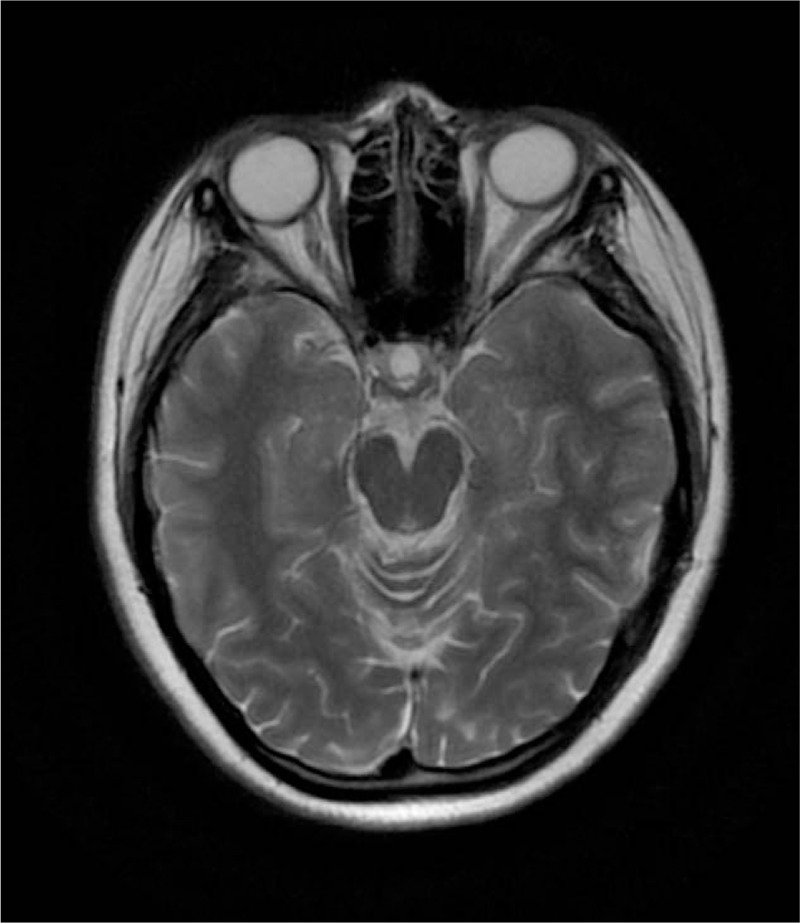
Axial T2 magnetic resonance image (MRI) showed focal subcortical hypointensity in the left temporal lobe a month later.
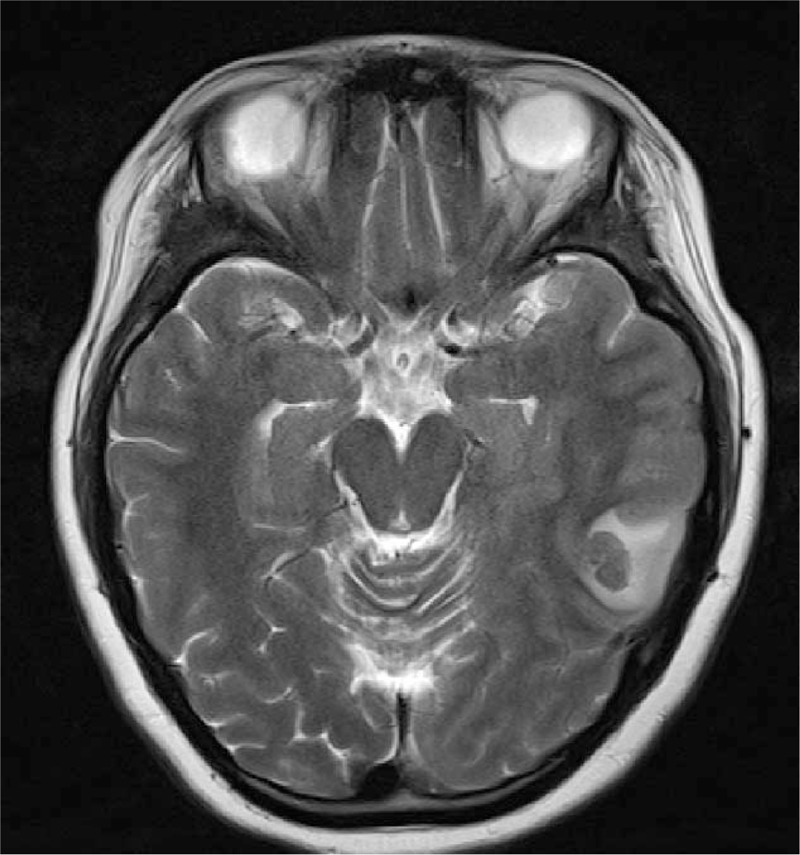
Figure 6.
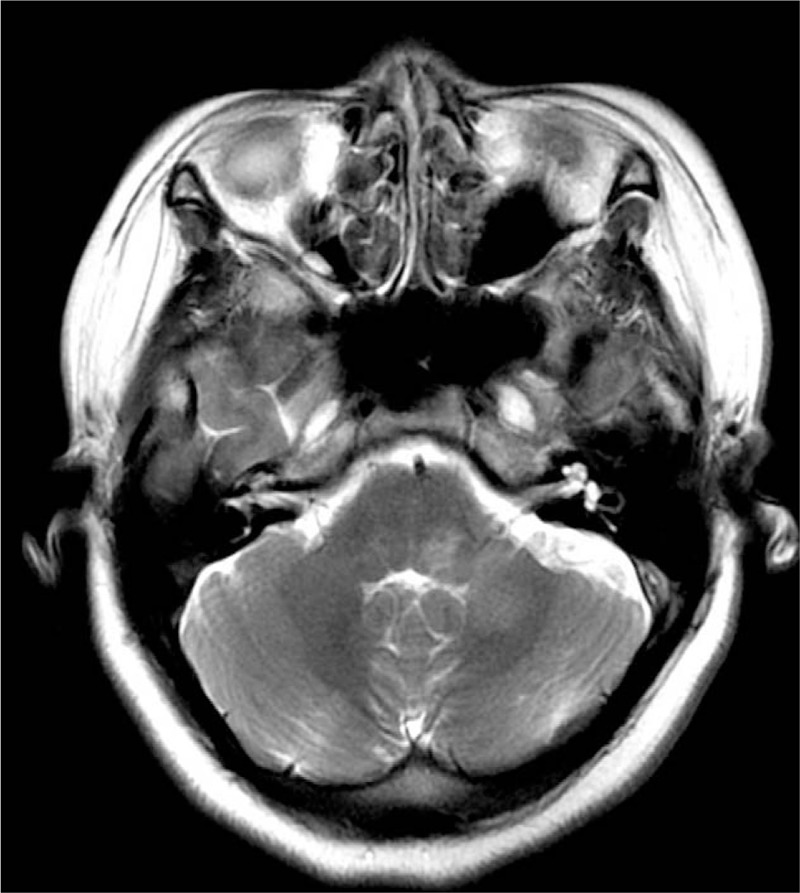
Axial T2 magnetic resonance (MRI) showed focal T2 hypointensity in brain stem and left cerebellar hemisphere 3 months later.
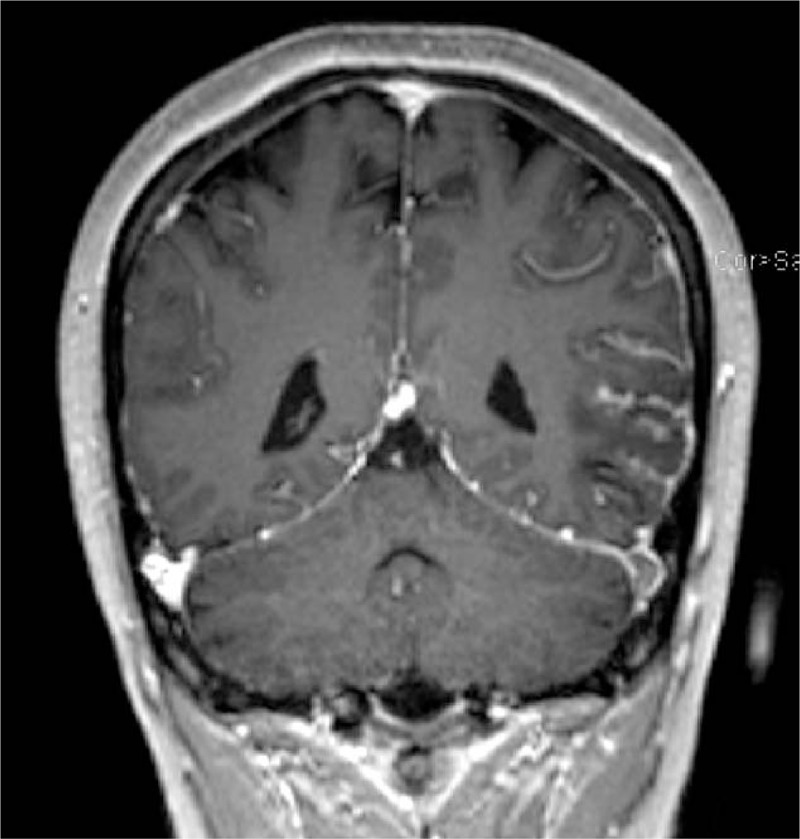
Figure 7.
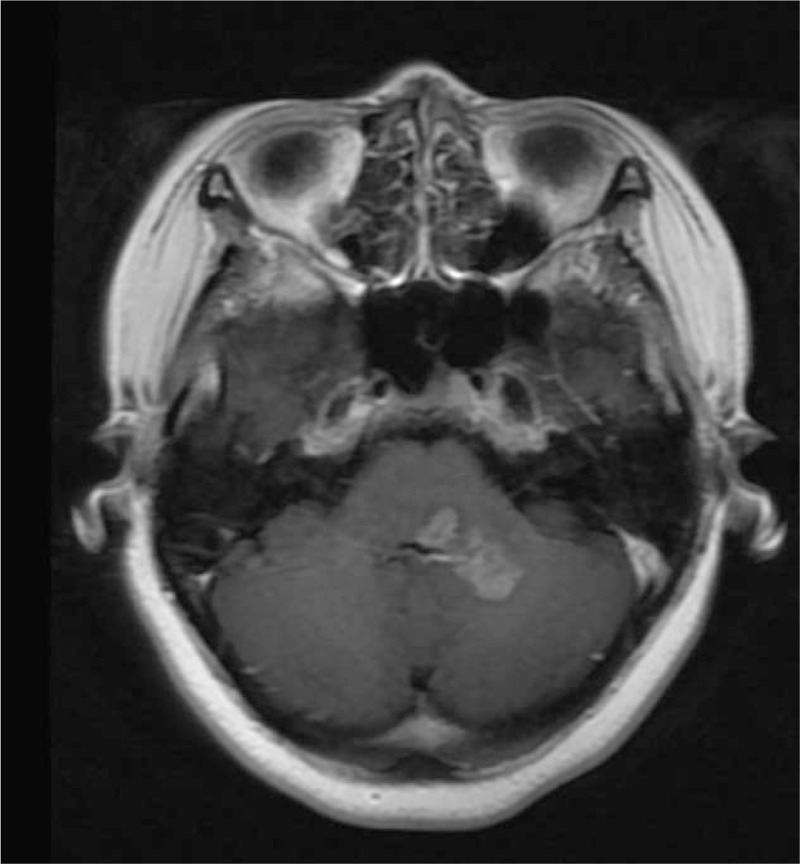
Corresponding contrast-enhanced image of the brain stem and left cerebellar hemisphere.
Figure 8.
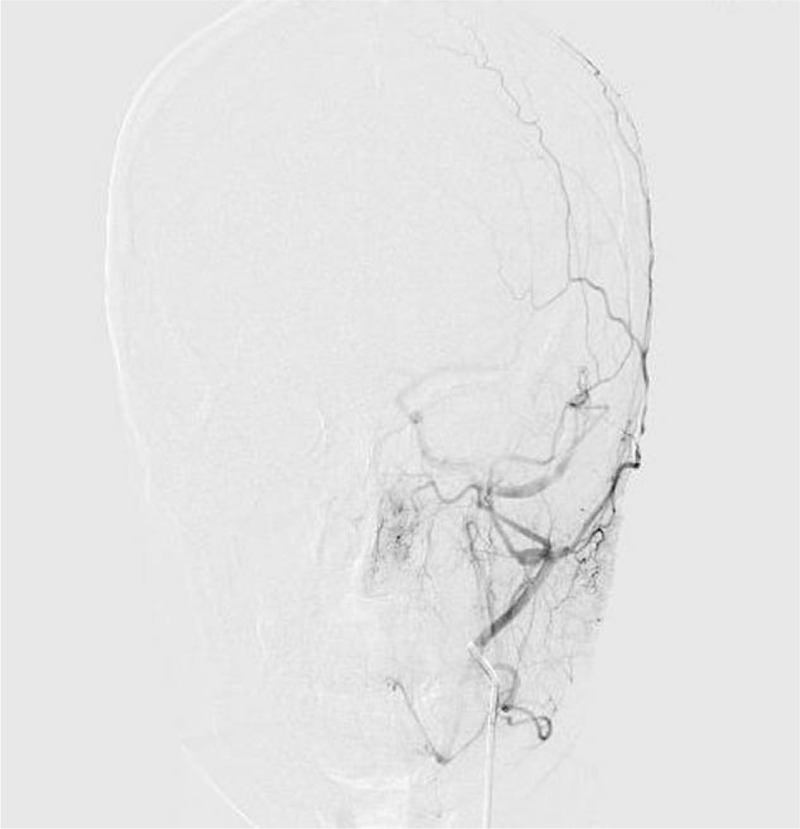
digital subtraction angiography (DSA) confirmed a dural arteriovenous fistula (dAVF) of the left sigmoid sinus supplied by dural branches of the left occipital and right middle meningeal artery.
Figure 9.

Clipping of the fistula was conducted. The left sigmoid sinus was still not patent.
3. Discussion
Cerebral venous thrombosis (CVT) is a rare condition involving both intracranial veins and sinuses. Young age, female gender, oral contraceptives, cancer, trauma, and hereditary coagulopathy can increase the risk for CVST.[1,2,3,4] In the presented case, the patient had a risk factor of taking OPC, and suffered a non-specific headache, which is one of the most frequent symptoms of CVST.[4,5,7] These non-specific clinical symptoms also mimic other neurological disorders, for example, dAVF disguised as CVST.[8] The elevated CPR, D-dimer concentration of laboratory findings were helpful in CVST diagnosis. CT, MRI and MRV features could also help to obtain an early and differential diagnosis. Imaging techniques including susceptibility weighted images (SWI),[9] magnetic resonance black-blood thrombus imaging (MRBTI),[10] diffusion restriction on diffusion weighted image (DWI), a filling defect on unenhanced MRI coronal T2 image and MRV without contrast could detect the thrombus. Although DSA is regarded as the gold standard for diagnosing CVST, contrast-enhanced MRV technology might be the best approach for detecting CVST. In particular, an empty delta sign indicates that a filling defect within a vessel is visible, and the diagnosis of CVST is then easy to make. In our case, filling defect on T2WI, together with the high signal intensity on DWI, empty delta sign on contrast-enhanced images, absence of the transverse-sigmoid sinus on MRV, and history of oral contraceptives led to the diagnosis of CVST.
Complications of CVST could occur in acute or chronic phases, while dAVFs often occur in the chronic stage, but cases in the acute phase have also been reported.[1] Intracranial dAVFs are abnormal direct connections between dural arteries and any portion of the intracranial venous sinuses, meningeal veins, or even cortical veins. These dAVFs may be located anywhere within the intracranial dura, but transverse and cavernous sinus are most commonly seen. Despite the constant investigation about relationships between dAVF and CVST, whether CVST is the cause or result of dAVF remains elusive.[4] In our report, it was obvious that dAVF was developed from CVST. Thus, in the case, venous hypertension might play a major role in the pathogenesis of dAVF formation. In particular, the venous hypertension triggered and aggravated the development of dAVF, which induced the opening of pre-existing physiological shunts between meningeal arterial networks and dural venous sinus.
The edematous lesions in the left temporal lobe of our case was resolved completely on T2WI in the follow-up examinations, and MRV displayed that the left transverse-sigmoid sinus was still not shown a month later. Meanwhile, the patient continued with the treatment of anticoagulant therapy. However, 3 months later, the patient developed dAVF confirmed by DSA. Since the MRA was normal, we previously made a misdiagnosis of demyelination or encephalitis. As the patient had a history of consuming OPC, we should be aware of the possibility of dAVF. The lesson learned in the case was that we should take more active measures to avoid complications in the course of clinical treatment.
4. Conclusion
When taking OCP, a known risk for CVST, women should obey physician prescription. In the case when a patient shows non-specific clinical symptoms of headache and seizures, a clinical suspicion of possible CVST should always arise. MRV and contrast-enhanced MRI were useful for diagnosis and follow-up to avoid the onset of complications such as permanent parenthetical damage, cerebral hemorrhage and dAVF as soon as possible.
Author contributions
Conceptualization: Qingling Huang.
Data curation: Qingling Huang, Xue Chai, Chaoyong Xiao.
Formal analysis: Qingling Huang.
Project administration: Qingling Huang.
Resources: Qingling Huang, Xue Chai, Chaoyong Xiao.
Supervision: Qingling Huang.
Writing – original draft: Qingling Huang, Xuan Cao.
Writing – review & editing: Qingling Huang, Xuan Cao, Xue Chai, Chaoyong Xiao.
Footnotes
Abbreviations: CRP = C-reactive protein, CT = computed tomography, CVST = cerebral venous sinus thrombosis, dAVF = dural arteriovenous fistula, DSA = digital subtraction angiography, DWI = diffusion weighted image, MRA = MR angiography, MRBTI = magnetic resonance black-blood thrombus imaging, MRI = magnetic resonance imaging, MRV = magnetic resonance venography, OCP = oral contraceptive pills, SWI = susceptibility weighted images.
This work was supported by the Health Youth Talents Foundation of Nanjing (Grant No. QRX11115).
This case report was approved by Nanjing Brain Hospital of Nanjing Medical University Research Ethics Board, and informed written consent was obtained from the patient for publication of this case report and accompanying images.
The authors have no conflicts of interests to disclose.
References
- [1]. Chen JG, Li ZX, Zhang DF, et al. Cerebral venous sinus thrombosis complicated with acute development of dural arteriovenous fistula: a case report. J Clin Neurosci 2017;44:225–6. [DOI] [PubMed] [Google Scholar]
- [2]. Das JK, Medhi J, Bhattacharya P, et al. Clinical spectrum of spontaneous carotid-cavernous fistula. Indian J Ophthalmol 2007;55:310–2. [DOI] [PubMed] [Google Scholar]
- [3]. Siddiqui FM, Kamal AK. Incidence and epidemiology of cerebral venous thrombosis. J Pak Med Assoc 2006;56:485–7. [PubMed] [Google Scholar]
- [4]. Gunes HN, Cokal BG, Guler SK, et al. Clinical associations, biological risk factors and outcomes of cerebral venous sinus thrombosis. J Int Med Res 2016;44:1454–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Azin H, Ashjazadeh N. Cerebral venous sinus thrombosis–clinical features, predisposing and prognostic factors. Acta Neurol Taiwan 2008;17:82–7. [PubMed] [Google Scholar]
- [6]. Lidegaard O, Lokkegaard E, Svendsen AL, et al. Hormonal contraception and risk of venous thromboembolism: National follow-up study. BMJ 2009;339:b2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Coutinho JM, Stam J, Canhão P, et al. Cerebral venous thrombosis in the absence of headache. Stroke 2015;46:245–7. [DOI] [PubMed] [Google Scholar]
- [8]. Sun LL, Tang WX, Liu L, et al. Dural arteriovenous fistula disguised as cerebral venous sinus thrombosis. J Zhejiang Univ Sci B 2017;18:733–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Sato T, Terasawa Y, Mitsumura H, et al. Venous stasis and cerebrovascular complications in cerebral venous sinus thrombosis. Eur Neurol 2017;78:154–60. [DOI] [PubMed] [Google Scholar]
- [10]. Yang Q, Duan J, Fan Z, et al. Early detection and quantification of cerebral venous thrombosis by magnetic resonance black-blood thrombus imaging. Stroke 2016;47:404–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


