Abstract
An increasingly important concern for clinicians who care for patients with cancers is their psychological problems and quality of life. The present study examined the efficacy of supportive group psychotherapy (SGP) on anxiety, depression and overall quality of life in patients with lung cancer undergoing gamma knife surgery (GKS).
160 patients with lung cancer undergoing GKS were randomly divided into SGP group (n = 82) and care as usual (CAU) group (n = 78). Patients in SGP group received 90 minutes’ group psychotherapy intervention once a week for 8 weeks, while patients in CAU group received usual care. Outcome measures were administered before and after the intervention and at 3-months follow-up. The primary outcome measures were the 14-item Hospital Anxiety and Depression Scale (HADS) and the secondary outcome measures were the 30-item European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30).
Demographic characteristics between SGP and CAU groups showed no difference in sex, age, course of disease, years of education, marital status and profession. Psychological characteristics evaluated by HADS revealed that levels of both depression and anxiety in SGP group were significantly improved compared with that in CAU group at the end of the treatment and the improvement remained at the 3-months follow-up. In addition, EORTC QLQ-C30 demonstrated that functional scales including emotion, cognition and society in SGP group were significantly higher than that in CAU group at the end of the treatment and maintained till 3-months follow-up. EORTC QLQ-C30 also showed that symptom scales including fatigue, nausea/vomiting, pain, syspnea, insomnia, loss of appetite and financial problems in the former group were significantly lower than that in the latter group and maintained till 3-months follow-up. Furthermore, compared with that in SGP group before treatment, these variables in both HADS and EORTC QLQ-C30 showed obvious improvement in the same group after treatment and at the 3-months follow-up.
The results suggested that SGP can alleviate anxiety and depression in patients with lung cancer following GKS and improve the overall quality of life.
Keywords: anxiety, depression, gamma knife surgery, lung cancer survivors, supportive group psychotherapy
1. Introduction
Patients with cancer frequently suffer from psychological problems such as depression and anxiety.[1] These problems has been associated with reduced quality of life, greater mortality, decreased adherence to anticancer therapies, worse satisfaction with care and increased healthcare costs.[2,3]
Lung cancer is one of the most malignant cancers, responsible for 17.6% of total cancer-related deaths. Despite recent advances in treatment, lung cancer has a poor survival rate with only 15% of overall 5-year survival rate, even in well developed countries.[4,5] Similar to other cancer patients, patients with lung cancer also have psychological problems including depression and anxiety. Patients with lung cancer are commonly older adults living in the deprived areas and have multiple medical comorbidities especially in China.[6,7] They often suffer rapid and severe physical deterioration and they are aware of their poor prognosis. It is therefore unsurprising that they also suffer an especially high rate of depression and anxiety.
There is strong evidence that supportive group psychotherapy (SGP) intervention for cancer patients improves the quality of life, reduces the psychological distress, enhances the coping skills and attenuates the distress associated with symptoms such as pain.[8] Early researches revealed that 1-year SGP reduced psychological distress and improved quality of life for patients with metastatic cancer and dying patients and patients with the terminally ill.[9–11] China is a developing country with undeveloped development of SGP for cancers. It has some barriers among cancer survivors to accessing psychosocial support including a sense of stigma preventing them from seeking mental health service; the failure of healthcare providers to ask about emotional distress; a lack of awareness among survivors of available resources and not believing they require mental health services.
Given that the patients with lung cancer undergoing gamma knife surgery (GKS) have psychological problems which negatively affect their quality of life, the present study was designed to examine the efficacy of SGP on anxiety, depression and overall quality of life in these patients in order to improve their quality of life and reshape the hope of the life. The results showed that SGP can alleviate anxiety and depression in patients with lung cancer following GKS and improve the overall quality of life.
2. Method
2.1. Participants
Lung cancer patients undergoing GKS were recruited from No. 323 Hospital of People's Liberation Army, Xi’an, China between March, 2017 and March, 2018. Eligible patients were diagnosed with stage III or IV lung cancers over 18 years old, who were treated with GKS. Participants needed for psychological help/support for a psychosocial problem (e.g., anxiety, depression, coping issues, and life questions) and had ability to attend all therapy sessions. Patients were excluded if they had significant cognitive impairment or psychosis and had current psychological treatment. Prospective participants were informed of the risks and benefits of study participation and provided written informed consent. The study was approved by the Ethics Review Committee of No. 323 Hospital of People's Liberation Army, China. 160 patients were randomly divided into SGP group (n = 82) and care as usual (CAU) group (n = 78). Patients in SGP group received 90 minutes’ group psychotherapy intervention once a week for 8 weeks, while patients in care as usual (CAU) group received usual care. Patients in SGP group were randomized in groups of 8 to 10. The lost numbers in SGP group are 2 and 5 after treatment and at 3-months follow-up respectively, while lost numbers in CAU are 3 and 6 respectively. Outcome measures were administered before and after the intervention and at 3-months follow-up. The primary outcome measures were the 14-item Hospital Anxiety and Depression Scale (HADS) and the secondary outcome measures were the 30-item European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30).
The HADS is a 14-item self-assessment scale for measuring distress with 2 subscales, anxiety and depression. The HADS was specifically designed for use in the medically ill.[12]
The 30-item EORTC QLQ-C30 (version 3.0) includes a global HRQOL scale (2 items) and comprises 5 functional scales: physical functioning (5 items), role functioning (2 items), emotional functioning (4 items), cognitive functioning (2 items) and social functioning (2 items). There are 3 symptom scales (nausea and vomiting (2 items), fatigue (3 items) and pain (2 items) and 6 single items relating to dyspnoea, insomnia, loss of appetite, constipation, diarrhoea and financial difficulties.[12]
2.2. Supportive group psychotherapy
Based on the seminal work of Cain et al,[13] SGP program was developed formal models of group psychological interventions in cancer survivors. The SGP was conducted by 2 accredited psychologists, once per week for 90 minutes. Each weekly session was based around 8 themes, reflecting the ongoing needs of cancer survivors.[14,15] The themes were:
-
1.
exploration of life stories,
-
2.
implications of living with cancer,
-
3.
stress coping,
-
4.
mindfulness and feeling anxious,
-
5.
relationships and support,
-
6.
self-identity,
-
7.
hope, and
-
8.
moving forward.
Each SGP session included opportunity for individual expression, group discussion, teaching, and problem solving.[13,16,17] The proposed benefits of participating in these experiences together were creating a sense of belonging and normalcy, sharing and reshaping their identities, feeling a sense of mutual aid, and creating hope by comparison of coping success.
2.3. Care as usual
Cancer survivors assigned to the CAU group did not participate in the group interventions. If a participant requested psychological care, he or she was referred to the physician general practitioner.
2.4. Statistical analysis
The initial analysis of treatment effects was conducted within treatment groups using matched t tests. ANOVA was used to evaluate whether the treatment effects observed differed across the 2 groups. Post hoc tests were used to break down the 3 time points (before treatment, after treatment and 3-months follow-up), by contrasting before treatment and after treatment and 3-months follow-up. Descriptive analyses and chi-square tests of association were used as appropriate to analyze sample characteristics. P < .05 was considered significantly different.
3. Results
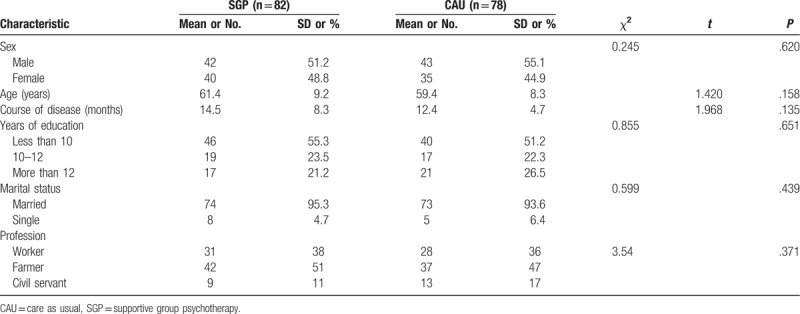
3.1. Demographic characteristics of lung cancer survivors undergoing GKS between GSP and CAU groups
One hundred Sixty lung cancer patients who received GKS were randomly into SGP and CAU groups, having 82 and 78 cases respectively (Table 1). Each group has even gender distribution with 42 (51.2%) males in SGP group and 43 (55.1%) males in CAU group respectively (χ2 = 0.245, P = .620). The mean ages are 61.4 years in SGP group and 59.4 years in CAU group respectively (t = 1.420, P = .158). No significant differences in years of education among 3 periods (less than 10 years, 10–12 years and more than 12 years) are found between 2 groups (χ2 = 0.855, P = .651). Similarly, marital status and profession also showed no significant difference between 2 groups (χ2 = 0.599, P = .439 for marital status and χ2 = 0.778, P = .371 for profession respectively).
Table 1.
Demographic characteristics of lung cancer survivors.
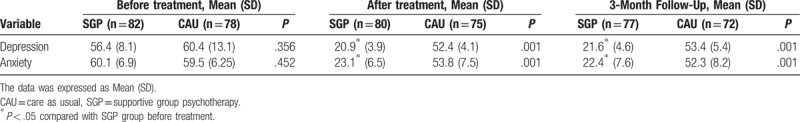
3.2. Psychological characteristics of lung cancer survivors undergoing GKS between GSP and CAU groups
Depression and anxiety are the main psychological problems for lung cancer survivors. Therefore, HADS was used to assess the status of depression and anxiety before and after treatment and at the 3-month follow-up in 2 groups. As shown in Table 2, the scores of depression and anxiety are comparable between SGP and CAU groups before treatment (56.4 vs 60.4, P = .356 for depression and 60.1 vs 59.5, P = .452 for anxiety, respectively). However, the depression scores in SGP group after treatment decreased significantly compared with that before treatment (20.9 vs 56.4, decreased by 62.9%, P < .05), which continuously kept stable till the 3-month follow-up. Similarly, the anxiety scores in SGP group after treatment reduced significantly compared with that before treatment (23.1 vs 60.1, reduced by 61.6%, P < .05), which continuously kept stable till the 3-Month Follow-Up. These results suggested that group psychotherapy intervention is an effective approach for patients with lung cancer survivors who received GKS to improve their depression and anxiety. On the contrary, the scores of both depression and anxiety in CAU group revealed no significant changes among before, after treatment and at 3-month follow-up. Expectedly, scores of both depression and anxiety in SGP group reduced significantly compared with that in CAU group after treatment (20.9 vs 52.4, P = .001 for depression and 21.6 vs 53.4, P = .001 for anxiety) and at 3-month follow-up (23.1 vs 53.8, P = .001 for depression and 22.4 vs 52.3, P = .001 for anxiety).
Table 2.
Psychological characteristics of lung cancer survivors.
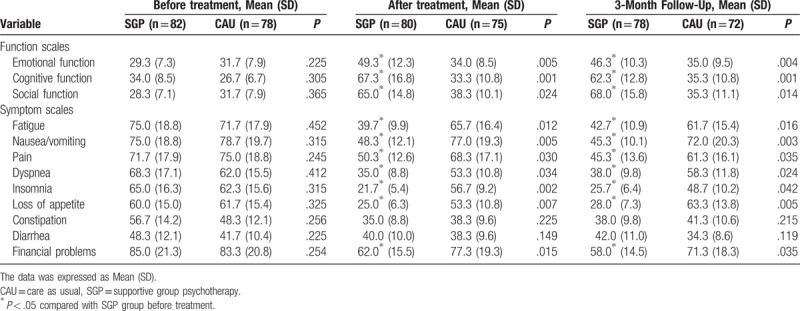
3.3. Functional and symptomatic characteristics of lung cancer survivors undergoing GKS between GSP and CAU groups
Functional and symptomatic problems always negatively affect the life of quality of lung cancer survivors. Thereafter, EORTC QLQ-C30 was employed to evaluate the status of functional and symptomatic characteristics before and after treatment and at the 3-month follow-up in 2 groups. As shown in Table 3, the scales of all functional and symptomatic variables demonstrated comparable between 2 groups before treatment. However, the function scales including emotion, cognition and society in SGP group after treatment increased significantly compared with that before treatment (49.3 vs 29.3, P = .005 for emotion, 67.3 vs 34.0, P = .001 for cognition and 65.0 vs 28.3, P = .024 for society, increased by 68.3%, 97.9%, and 129.7%, respectively). These results suggested that group psychotherapy intervention for 8 weeks significantly improves these functions of lung cancer survivors. Furthermore, the improvement remained at 3-month follow-up. On the contrary, patients in CAU group showed no improvement of these functions after treatment and at 3-month follow-up compared with that before treatment. In addition, the symptom scales including fatigue, nausea/vomiting, pain, dyspnea, insomnia, loss of appetite, and financial problems in SGP after treatment and at 3-month follow-up significantly decreased compared with that before treatment. On the contrary, patients in CAU group showed no changes in these symptom scales after treatment and at 3-month follow-up.
Table 3.
Functional and symptomatic characteristics of lung cancer survivors (Mean (SD)).
4. Discussion
In the present study, we found that SGP intervention attenuates the depression and anxiety and improves the functional and symptomatic characteristics in patients with lung cancer undergoing GKS. These results are consistent with the reports revealing that SGP lessens anxiety and depression and builds up global quality of life in 31 patients with advanced cancer in China[18] and that SGP improves self-efficacy, quality of life, symptom distress, communication and uncertainty of patients with prostate cancer and their partners in the United Kingdom.[8]
Lung cancer patients generally bear the pressure of surgery, follow-up treatment and the poor prognosis. Long-term stress leads to anxiety, depression and other negative emotions.[7] Studies showed that the prognosis of malignant tumors is closely related with the emotional changes. Negative emotion reduces the immunity of the patients, promotes the proliferation of cancer cells and enhances the metastasis. Therefore, the necessary psychological intervention should be taken to improve the unhealthy psychological state of lung cancer patients and improve their quality of life.
SGP was based on the model developed by Cain et al[13,19] and manualized by Payne et al[20] The 8 weekly 90-minutes sessions focused on discussion of issues themes that emerge for patients coping with cancer. Utilizing a supportive approach, therapists focused on encouraging patients to share concerns related to the cancer diagnosis and treatment, to describe their experiences and emotions related to these experiences, voice problems that they have in coping with cancer, and offer support and advice to other group members. Each SGP session included opportunity for individual expression, group discussion, teaching, and problem solving.[13,16,17] The proposed benefits of participating in these experiences together were creating a sense of belonging and normalcy, sharing and reshaping their identities, feeling a sense of mutual aid, and creating hope by comparison of coping success.
Group cohesion of SGP is an effective therapeutic force.[19,20] A safe and receptive group environment allows each patient to talk freely about topics that they can’t talk about with their families and medical staff and to share and overcome their fears as well as to face the threat of disease to their lives. The present study showed that in initial phase of group therapy, most of the patients talk about optimistic ideas, making the treatment difficult. Under the guidance of a psychotherapist, a woman patient finally cried out in fear of death, which took the group therapy a big step forward. With the progress of treatment, the warmth of the group dissolves their loneliness and helplessness. At the end of the group, many patients were reluctant to leave the group and would try their best to help other patients. The efficacy was proven by our finding that the scores of both depression anxiety in SGP group after treatment decreased by 62.9% and 61.6%, respectively compared with that before treatment, both continuously kept stable till the 3-month follow-up. These results suggested that group psychotherapy intervention is an effective approach for patients with lung cancer survivors who received GKS to improve their depression and anxiety. Similarly, Wu and Wang reported that supportive psychotherapy reduces the depression and anxiety in 63 patients with lung cancer by 55.3%.[21]
Regarding the long-term (after 3 months of follow-up) effect of SGP for the patients with lung cancer following GKS, our experience revealed that the depression and anxiety of the patients were still significantly reduced and the ability of life adaptation was significantly improved. We also found that the patients’ desire for survival was stimulated, the compliance of treatment was improved and the endurance of pain was enhanced. This is because
-
1.
the patients fully express their problems and shares their views with other members through group therapy;
-
2.
they get support from each other and feel improved self-worth and
-
3.
they have witnessed the success of other members and tried to reshape the hope of life.
Besides the close association between severity of lung cancer with depression and anxiety, Pompili et al reported that patients affected by chronic and disabling conditions that are even comorbid with psychiatric disorders are usually nonadherent to mood disorders medications.[22] Specifically, the authors identified several predictors of nonadherence among patients with mood disorders including younger age, comorbidity with substance use and personality disorders, patients’ beliefs, poor insight, illness severity, treatment-related side effects, specific features of the disease and a poor therapeutic alliance.[22] The authors concluded that given the high social, clinical and economic impact of nonadherence among patients who are affected by mood disorders, it is critical to recognize patients at high risk of nonadherence in order to inform future strategies to examine and improve adherence to treatment.
The present study has several limitations. Firstly, the sample size of patients is relatively small. Secondly, the study is based on one center. Lastly, this study is focusing on the lung cancer patients instead of variety of cancers. These limitations can be solved in the future by increasing the sample size, expanding to multi-centers investigation and to other cancers.
5. Conclusion
The present study has suggested that SGP can alleviate anxiety and depression in patients with lung cancer following GKS and improve the overall quality of life. This study is of clinical significance for effectively using SGP to treat the psychological and functional problems for cancer patients.
Author contributions
Conceptualization: Wanxiu Peng, Hui Zhang.
Data curation: Wanxiu Peng, Zhongguo Li.
Formal analysis: Wanxiu Peng, Hui Zhang, Zhongguo Li.
Investigation: Wanxiu Peng.
Methodology: Wanxiu Peng, Zhongguo Li.
Software: Zhongguo Li.
Supervision: Hui Zhang.
Writing – original draft: Wanxiu Peng.
Writing – review & editing: Hui Zhang.
Footnotes
Abbreviations: CAU = care as usual, EORTC QLQ-C30 = 30-item European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30, GKS = gamma knife surgery, HADS = hospital anxiety and depression scale, SGP = supportive group psychotherapy.
The authors report no conflicts of interest.
References
- [1].Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 2011;12:160–74. [DOI] [PubMed] [Google Scholar]
- [2].Brown LF, Kroenke K, Theobald DE, et al. The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psychooncology 2010;19:734–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kroenke K, Zhong X, Theobald D, et al. Somatic symptoms in patients with cancer experiencing pain or depression: prevalence, disability, and health care use. Arch Intern Med 2010;170:1686–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Didkowska J, Wojciechowska U, Manczuk M, et al. Lung cancer epidemiology: contemporary and future challenges worldwide. Ann Transl Med 2016;4:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med 2011;32:605–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Janssen-Heijnen ML, Schipper RM, Razenberg PP, et al. Prevalence of co-morbidity in lung cancer patients and its relationship with treatment: a population-based study. Lung Cancer 1998;21:105–13. [DOI] [PubMed] [Google Scholar]
- [7].De Ruysscher D, Botterweck A, Dirx M, et al. Eligibility for concurrent chemotherapy and radiotherapy of locally advanced lung cancer patients: a prospective, population-based study. Ann Oncol 2009;20:98–102. [DOI] [PubMed] [Google Scholar]
- [8].McCaughan E, Curran C, Northouse L, et al. Evaluating a psychosocial intervention for men with prostate cancer and their partners: Outcomes and lessons learned from a randomized controlled trial. Appl Nurs Res 2018;40:143–51. [DOI] [PubMed] [Google Scholar]
- [9].Yalom ID, Greaves C. Group therapy with the terminally ill. Am J Psychiatry 1977;134:396–400. [DOI] [PubMed] [Google Scholar]
- [10].Spiegel D, Bloom JR, Yalom I. Group support for patients with metastatic cancer. A randomized outcome study. Arch Gen Psychiatry 1981;38:527–33. [DOI] [PubMed] [Google Scholar]
- [11].Spiegel D, Yalom ID. A support group for dying patients. Int J Group Psychother 1978;28:233–45. [DOI] [PubMed] [Google Scholar]
- [12].van der Spek N, Vos J, van Uden-Kraan CF, et al. Effectiveness and cost-effectiveness of meaning-centered group psychotherapy in cancer survivors: protocol of a randomized controlled trial. BMC Psychiatry 2014;14:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cain EN, Kohorn EI, Quinlan DM, et al. Psychosocial benefits of a cancer support group. Cancer 1986;57:183–9. [DOI] [PubMed] [Google Scholar]
- [14].Jefford M, Karahalios E, Pollard A, et al. Survivorship issues following treatment completion–results from focus groups with Australian cancer survivors and health professionals. J Cancer Surviv 2008;2:20–32. [DOI] [PubMed] [Google Scholar]
- [15].Marlow B, Cartmill T, Cieplucha H, et al. An interactive process model of psychosocial support needs for women living with breast cancer. Psychooncology 2003;12:319–30. [DOI] [PubMed] [Google Scholar]
- [16].Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer 2002;10:272–80. [DOI] [PubMed] [Google Scholar]
- [17].Breitbart W, Rosenfeld B, Gibson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology 2010;19:21–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].2006;Wang H, Li M. Group psychotherapy for cancer patientsJT Chin J Ment Health. 20:817–9. [Google Scholar]
- [19].Martin E, Bulsara C, Battaglini C, et al. Breast and prostate cancer survivor responses to group exercise and supportive group psychotherapy. J Psychosoc Oncol 2015;33:620–34. [DOI] [PubMed] [Google Scholar]
- [20].Payne DK, Lundberg JC, Brennan MF, et al. A psychosocial intervention for patients with soft tissue sarcoma. Psychooncology 1997;6:65–71. [DOI] [PubMed] [Google Scholar]
- [21].Wu L. WS-J Psychotherapy improving depression and anxiety of patients treated with chemotherapy combined with radiotherapy. Chin J Clin Rehabil 2003;7:2462–3. [Google Scholar]
- [22].Pompili M, Venturini P, Palermo M, et al. Mood disorders medications: predictors of nonadherence - review of the current literature. Expert Rev Neurother 2013;13:809–25. [DOI] [PubMed] [Google Scholar]


