Abstract
Reactive oxygen species (ROS)-generating anticancer agents can act through two different mechanisms: (i) elevation of endogenous ROS production in mitochondria, or (ii) formation/delivery of exogenous ROS within cells. However, there is a lack of research on the development of ROS-generating nanosystems that combine endogenous and exogenous ROS to enhance oxidative stress-mediated cancer cell death.
Methods: A ROS-generating agent based on polymer-modified zinc peroxide nanoparticles (ZnO2 NPs) was presented, which simultaneously delivered exogenous H2O2 and Zn2+ capable of amplifying endogenous ROS production for synergistic cancer therapy.
Results: After internalization into tumor cells, ZnO2 NPs underwent decomposition in response to mild acidic pH, resulting in controlled release of H2O2 and Zn2+. Intriguingly, Zn2+ could increase the production of mitochondrial O2·- and H2O2 by inhibiting the electron transport chain, and thus exerted anticancer effect in a synergistic manner with the exogenously released H2O2 to promote cancer cell killing. Furthermore, ZnO2 NPs were doped with manganese via cation exchange, making them an activatable magnetic resonance imaging contrast agent.
Conclusion: This study establishes a ZnO2-based theranostic nanoplatform which achieves enhanced oxidative damage to cancer cells by a two-pronged approach of combining endogenous and exogenous ROS.
Keywords: reactive oxygen species, zinc peroxide nanoparticles, pH-responsiveness, magnetic resonance imaging, cancer therapy
Introduction
Reactive oxygen species (ROS) including hydrogen peroxide (H2O2), superoxide anion radical (O2·-), singlet oxygen, and hydroxyl radical can damage lipids, proteins, and DNA, which would lead to cell death when the ROS level exceeds the cellular antioxidant capacity, a condition referred to as oxidative stress 1-6. Cells constantly generate endogenous ROS as by-products of aerobic metabolism in mitochondria, and maintain redox homeostasis by controlling the balance between ROS formation and scavenging 7. More importantly, it has been found that cancer cells show elevated mitochondrial ROS production due to oncogenic stimulation and active metabolism 8-10. Even though cancer cells enhance antioxidant capacity to counterbalance the overproduction of ROS, their ROS levels are still closer to the toxicity threshold than that of normal cells, making them more susceptible to further ROS formation induced by exogenous agents 11,12. Therefore, the development of ROS-generating agents that can effectively raise intracellular ROS levels above the toxicity threshold and cause oxidative stress-mediated cell death would be of great interest in cancer therapy.
There are two possible working mechanisms for ROS-generating anticancer agents: (i) enhancement of endogenous ROS production, and (ii) formation/delivery of exogenous ROS. On the one hand, it is well known that mitochondria are the main source of endogenous ROS, and that inhibition of mitochondrial electron transport chain (ETC) can promote the production of O2·- and H2O2 by increasing leakage of electrons to oxygen (O2) at complexes I and III of the ETC 13,14. Therefore, several ETC inhibitors have been used to kill tumor cells through endogenous ROS-mediated apoptosis 15. On the other hand, anticancer agents with exogenous ROS-generating ability, such as photodynamic and sonodynamic sensitizers, are attracting more and more attention 16-21. In particular, stimuli-responsive nanoplatforms have been actively explored for the formation of exogenous ROS in tumor cells 22-28. However, to the best of our knowledge, there is a paucity of studies regarding the design of ROS-generating nanosystems that combine endogenous and exogenous ROS to potentiate oxidative stress-induced cancer cell death.
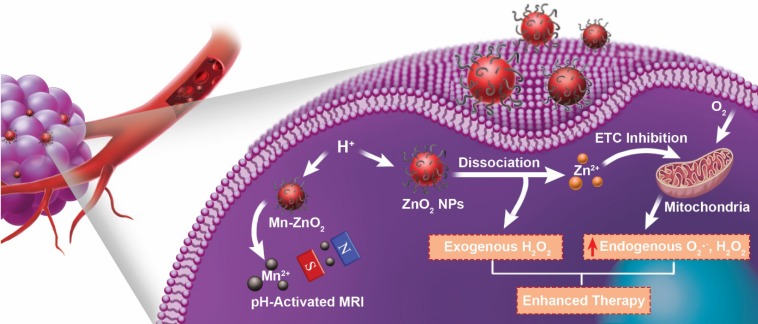
Herein, we report a novel ROS-generating agent based on zinc peroxide nanoparticles (ZnO2 NPs), which simultaneously delivers exogenous H2O2 and Zn2+ with the capability of intensifying endogenous ROS production for synergistic cancer therapy (Figure 1). The ZnO2 NPs were stable at neutral pH but decomposed to Zn2+ and H2O2 at mild acidic pH. In fact, it has been proved that zinc exerts its antitumor effects through inhibition of ETC and consequent elevation of mitochondrial ROS production 29-34. As compared to conventional zinc ionophores that have been utilized to increase Zn2+ accumulation in cancer cells 35-37, controlled Zn2+ delivery systems possess the potential for providing desirable therapeutic outcomes with reduced side effects. In addition, although formation of exogenous H2O2 within cells has been recognized as a promising strategy for tumor therapy 38,39, there has been little work on the preparation of H2O2-releasing systems with stimuli-responsive property. With these considerations in mind, we designed and synthesized poly(vinylpyrrolidone) (PVP)-modified ZnO2 NPs as a pH-triggered ROS-generating agent. Upon internalization in tumor cells, ZnO2 NPs would release exogenous H2O2 and Zn2+ able to promote endogenous ROS production in mitochondria, which functioned in a synergistic manner to enhance oxidative stress-based cancer cell killing. The vulnerability of tumor cells to additional ROS and the pH-responsiveness of ZnO2 NPs enabled this ZnO2-based ROS-generating anticancer agent to achieve good therapeutic efficacy with low side effects. Moreover, the ZnO2 NPs was successfully doped with paramagnetic manganese (Mn) via a cation-exchange method. The pH-stimulated Mn2+ release during the decomposition of Mn-doped ZnO2 (Mn-ZnO2) NPs endowed them with activatable magnetic resonance imaging (MRI) contrast ability, which is useful to monitor the dissociation of ZnO2 NPs as well as the subsequent therapeutic process. This study not only highlights the great potential of ZnO2 nanomaterials in cancer theranostics, but also provides a paradigm for designing stimuli-responsive ROS-generating nanoagents that exacerbate oxidative damage to cancer cells through collaboration between endogenous and exogenous ROS.
Figure 1.
Schematic illustration of theranostic ZnO2 NPs for MRI and enhanced oxidative stress-based cancer therapy. Upon endocytosis by tumor cells, ZnO2 NPs undergo dissociation in response to mild acidic pH, causing the release of H2O2 and Zn2+. The exogenously released H2O2 and Zn2+, that can increase the production of mitochondrial O2·- and H2O2 by inhibiting the electron transport chain (ETC), act synergistically to promote cancer cell killing through the cooperation of endogenous and exogenous ROS. Moreover, Mn-doping via partial cation exchange imparts ZnO2 NPs with pH-activated MRI contrast ability.
Materials and methods
Materials
Zinc acetate (Zn(OAc)2, 99.99%), polyvinylpyrrolidone (PVP, Mw = 10000), hydrogen peroxide (H2O2, 30 wt. % in H2O), manganese(II) chloride (MnCl2, 99%), zinc chloride (ZnCl2, 99.999%), zinc oxide nanoparticles (ZnO NPs, 20 wt. % in H2O), zinquin ethyl ester (95%), 3-(N-morpholino)propanesulfonic acid (MOPS, 99.5%), sodium acetate (99%), acetic acid (99.7%), 2',7'-dichlorofluorescin diacetate (DCFH-DA, 97%), thiazolyl blue tetrazolium bromide (MTT, 97.5%), and propidium iodide (PI, 94%) were purchased from Sigma-Aldrich. Apoptosis kit with annexin V-FITC and PI, hydrogen peroxide assay kit, and calcein-AM were obtained from Fisher Scientific.
Synthesis of PVP-modified ZnO2 NPs
0.1 g of Zn(OAc)2 and 0.1 g of PVP were dissolved in 5.0 mL of water. Then, 0.5 mL of H2O2 was added quickly with vigorous stirring. After reaction for 24 h, the resulting PVP-modified ZnO2 NPs were washed several times and then re-dispersed in water.
Synthesis of Mn-ZnO2 NPs
The Mn-doping was achieved by a cation-exchange approach. Briefly, the aqueous solution of ZnO2 NPs was mixed with the same volume of MnCl2 with different Mn concentrations. After stirring at room temperature for 4 h, the obtained Mn-ZnO2 NPs were collected by centrifugation (15000 rpm, 15 min).
Decomposition of ZnO2 NPs
The release of Zn2+ and H2O2 from ZnO2 NPs was determined by dialysis. The aqueous solution of ZnO2 NPs was dialyzed against acetate buffer (pH 5.5) or MOPS buffer (pH 7.4). The Zn2+ was measured by inductively coupled plasma optical emission spectrometry (ICP-OES) and the H2O2 was measured by using a hydrogen peroxide assay kit.
Intracellular release of Zn2+
Zinquin ethyl ester, a cell-permeable fluorescent probe for Zn2+, was used to evaluate intracellular Zn2+ release. After incubation with ZnO2 NPs for 4 h, U87MG cells were stained with 25 μM zinquin ethyl ester at 37 °C for 30 min. Then, the fluorescence images were collected by an Olympus IX81 fluorescence microscope.
Oxidative stress assessment
Intracellular oxidative stress was determined by using DCFH-DA as a probe. U87MG cells seeded in 6-well plates (2×105 cells/well) were exposed to H2O2, ZnCl2, H2O2 plus ZnCl2, or ZnO2 NPs for 4 h. After staining with 10 μM DCFH-DA at 37 °C for 30 min, the fluorescence images were obtained.
In vitro cancer therapy
To demonstrate the synergistic anticancer effect of Zn2+ and H2O2, U87MG cells (5×103 cells/well) seeded in 96-well plates were incubated with H2O2, ZnCl2, or H2O2 plus ZnCl2 (molar ratio, 1:1) for 24 h. Then, the cell viability was measured by MTT assay. Similarly, the in vitro anticancer activity of PVP-modified ZnO2 NPs was examined.
Magnetic resonance imaging
To confirm the pH-activated MRI contrast effect, the Mn-ZnO2 NPs were dispersed in different buffer solutions for 4 h, and then the samples were imaged by an MRI scanner. For in vivo MRI, U87MG tumor-bearing mice were injected with Mn-ZnO2 NPs (200 μL, [Mn] = 1 mM) through the tail vein. Then, the T1-weighted MRI images were obtained by an MRI scanner.
In vivo tumor growth inhibition
Mice bearing U87MG tumors (~50 mm3) were injected intravenously with different formulations every other day for four doses, including (1) saline, (2) H2O2, (3) ZnCl2, and (4) ZnO2 NPs. Each dose of H2O2: 0.05 mmol/kg, ZnCl2: 0.05 mmol/kg, ZnO2 NPs: 5 mg/kg. The tumor volume and body weight of each mouse were recorded every 2 days.
Results and discussion
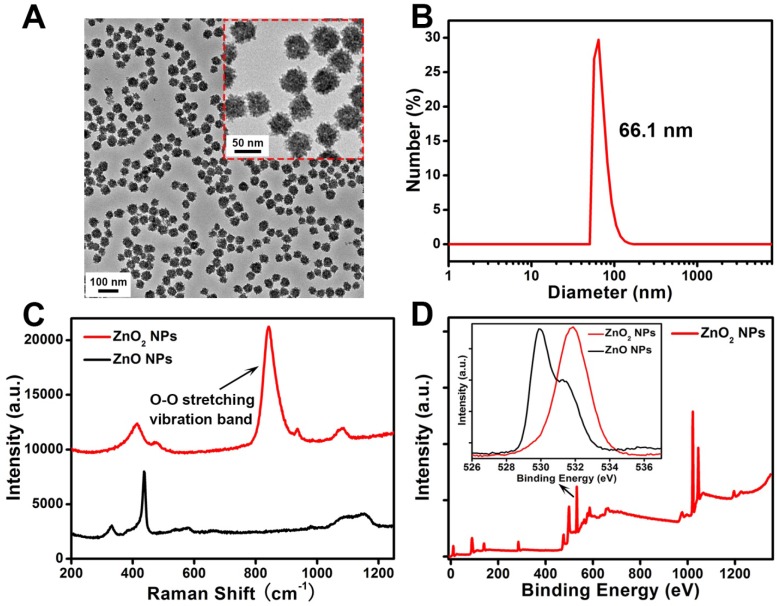
The ZnO2 NPs were fabricated by reacting zinc acetate with H2O2 in the presence of PVP at room temperature for 24 h. As shown in the transmission electron microscopy (TEM) image (Figure 2A), the as-prepared ZnO2 NPs had a uniform particle size of about 50 nm. Dynamic light scattering (DLS) results revealed that the average hydrodynamic diameter of ZnO2 NPs was ~66.1 nm (Figure 2B). In contrast to zinc oxide nanoparticles (ZnO NPs), ZnO2 NPs exhibited a strong band at 840 cm-1 in the Raman spectra assigned to O-O stretching vibration (Figure 2C) 40, clearly demonstrating the existence of peroxide ions (O22-). Moreover, the successful synthesis of ZnO2 NPs was further confirmed by X-ray photoelectron spectroscopy (XPS). An O 1s peak with binding energy of 532 eV corresponding to O22- was observed for the ZnO2 NPs, whereas the O 1s peak of ZnO NPs was located at 530 eV attributed to O2- (Figure 2D, Figure S1) 41.
Figure 2.
(A) TEM image and (B) DLS data of ZnO2 NPs. (C) Raman spectra of ZnO NPs and ZnO2 NPs. (D) XPS survey spectra and O 1s peak (inset) of ZnO2 NPs.
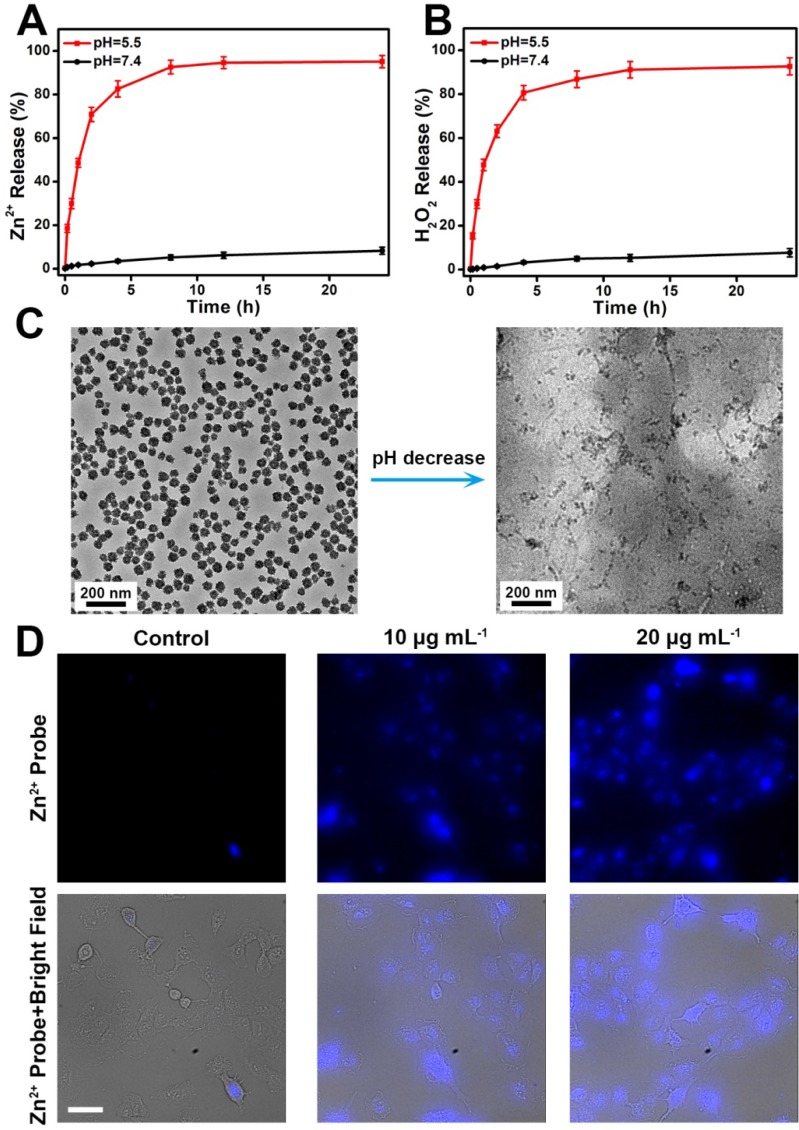
To demonstrate the pH-dependent dissociation behavior of ZnO2 NPs, we measured the release of Zn2+ and H2O2 from ZnO2 NPs under neutral (pH 7.4) or acidic (pH 5.5) conditions. It can be seen in Figure 3A,B that both Zn2+ and H2O2 were gradually released from the ZnO2 NPs at pH 5.5. In contrast, the release rates were relatively slow in pH 7.4 buffer solution. As shown by TEM (Figure 3C), ZnO2 NPs were stable at pH 7.4 but degraded at pH 5.5. Thus, the accelerated release in mild acidic environment can be ascribed to the pH-responsive degradation of ZnO2 NPs, which is favorable for in vivo tumor treatment since the acidic endo/lysosomes (pH 5.0-6.0) of cancer cells can trigger the release of H2O2 and Zn2+ on demand. Then, the decomposition of ZnO2 NPs in cancer cells was confirmed by evaluating the intracellular release of Zn2+ with a cell-permeable fluorescent Zn2+ probe, zinquin ethyl ester 42-45. As expected, ZnO2 NPs-incubated U87MG cancer cells exhibited stronger blue fluorescence than control untreated cells, and the blue fluorescence increased with increasing concentration of ZnO2 NPs (Figure 3D, Figure S2), demonstrating the intracellular degradation of ZnO2 NPs.
Figure 3.
Release profiles of (A) Zn2+ and (B) H2O2 from ZnO2 NPs at different pH values. (C) TEM images of ZnO2 NPs after 2 h of incubation in pH 7.4 (left) and pH 5.5 (right) buffer solutions. (D) Fluorescence images of zinquin ethyl ester-stained U87MG cells after incubation with different concentration of ZnO2 NPs for 4 h. Scale bar, 50 μm.
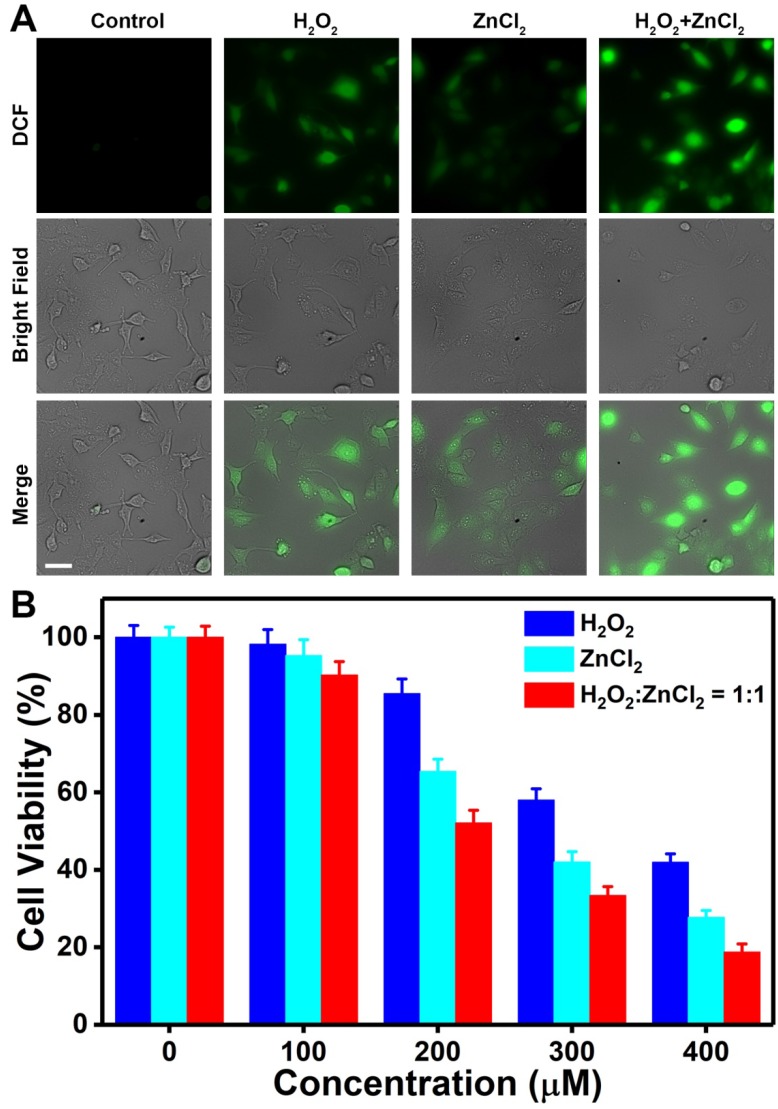
To determine whether Zn2+ and H2O2 could exert anticancer activity in a synergistic manner, we assessed their ability to induce oxidative stress and cytotoxicity. First, the intracellular oxidative stress caused by H2O2 or Zn2+ was examined by employing 2',7'-dichlorofluorescin diacetate (DCFH-DA) as the probe. After being deacetylated by cellular esterases, DCFH-DA is converted to DCFH that can interact with ROS to generate fluorescent 2',7'-dichlorofluorescein (DCF) 46-51. As shown in Figure 4A, U87MG cells incubated with either H2O2 or ZnCl2 displayed significantly greater DCF fluorescence compared with untreated control cells, implying the occurrence of oxidative stress in cancer cells upon H2O2 or Zn2+ exposure. The Zn2+-dependent oxidative stress could be mainly attributed to the increased mitochondrial ROS production 29-34. Moreover, the DCF fluorescence in U87MG cells co-incubated with H2O2 and ZnCl2 was higher than that in cells incubated with H2O2 or ZnCl2 alone, which indicated the combined effect of H2O2 and Zn2+ on amplification of oxidative stress. The oxidative stress-mediated cytotoxicity of H2O2 and Zn2+ was further evaluated by MTT assay. As expected, both H2O2 and ZnCl2 exhibited concentration-dependent toxicity (Figure 4B). More importantly, the viability of U87MG cells co-treated with H2O2 and ZnCl2 at a molar ratio of 1:1 was lower than that of cells treated with ZnCl2 or H2O2 alone, demonstrating the synergistic anticancer effect of H2O2 and Zn2+. It has been reported that mitochondria, one of the most important organelles responsible for energy metabolism, are particularly vulnerable to oxidative damage as they are constantly exposed to high levels of endogenous ROS 52. Therefore, the synergy between H2O2 and Zn2+ is probably because large amount of exogenously released H2O2 is able to disturb cellular redox homeostasis and then the enhanced mitochondrial ROS production resulting from inhibition of ETC by Zn2+ can lead to the impairment of mitochondria. These results suggested that exogenous H2O2 and Zn2+ with the capability of promoting endogenous ROS production could function cooperatively to enhance oxidative stress-induced tumor cell death.
Figure 4.
(A) DCF fluorescence of U87MG cells after different treatments. [H2O2] = 200 μM, [ZnCl2] = 200 μM. Scale bar, 50 μm. (B) Cell viability after 24 h of exposure to H2O2, ZnCl2, or H2O2 plus ZnCl2 (molar ratio, 1:1).
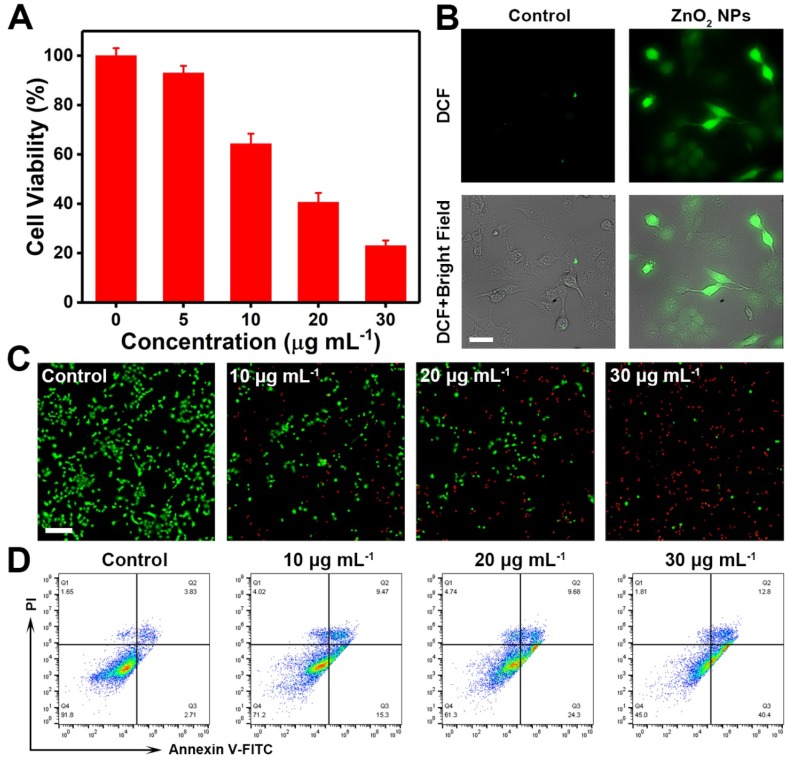
Next, the in vitro anticancer effect of PVP-modified ZnO2 NPs was examined. As can be seen in Figure 5A, the PVP-modified ZnO2 NPs exerted remarkable therapeutic efficacy against cancer cells, which could be ascribed to the pH-responsive release of H2O2 and Zn2+ from ZnO2 NPs in acidic endo/lysosomes and the subsequent occurrence of oxidative stress (Figure 5B). In addition, ZnO2 NPs exhibited a time- and dose-dependent cytotoxicity (Figure S3). To further confirm ZnO2 NPs-caused cancer cell death, the fluorescent indicators calcein-AM and propidium iodide (PI) were used to stain live (green) and dead (red) cells, respectively. Effective cell killing was observed when U87MG cells were exposed to ZnO2 NPs for 24 h (Figure 5C). The oxidative stress-triggered cancer cell apoptosis was then determined by annexin V-FITC/PI apoptosis detection kit. As shown in flow cytometry profiles (Figure 5D, Figure S4), U87MG cells underwent apoptosis after treatment with ZnO2 NPs for 12 h. Furthermore, the percentage of apoptotic cancer cells increased with increasing dose of ZnO2 NPs. The above results demonstrated the potential of pH-responsive ZnO2 NPs as an efficient therapeutic agent to cause oxidative stress and cancer cell apoptosis.
Figure 5.
(A) In vitro anticancer activity of ZnO2 NPs after 24 h of incubation. (B) DCF fluorescence of U87MG cells after 4 h of incubation with 10 μg mL-1 ZnO2 NPs. Scale bar, 50 μm. (C) Calcein-AM (green, live cells) and PI (red, dead cells) co-stained fluorescence images of cells treated with different concentrations of ZnO2 NPs for 24 h. Scale bar, 100 μm. (D) Flow cytometry data showing apoptosis in U87MG cells after exposure to ZnO2 NPs for 12 h.
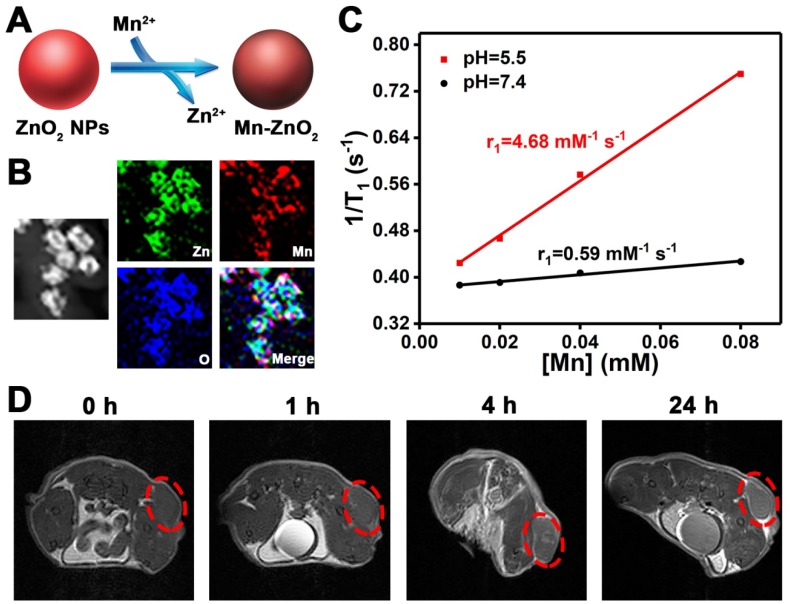
Theranostic agents that integrate diagnostic and therapeutic functions into a single nanoplatform offer great opportunities for personalized cancer treatment 53-59. In order to endow ZnO2 NPs with MRI contrast ability, a facile cation-exchange strategy was employed for the construction of Mn-doped ZnO2 NPs (Figure 6A). The multifunctional Mn-ZnO2 NPs were synthesized by mixing ZnO2 NPs with different amounts of MnCl2 at room temperature for 4 h. An obvious color change was observed after treatment of ZnO2 NPs with MnCl2 (Figure S5). Importantly, there was no distinct morphology difference between ZnO2 and Mn-ZnO2 NPs when the weight fraction of Mn was 6.5% or below (Figure S6). The Mn-ZnO2 NPs with 6.5% of Mn were thus selected for the following studies. Moreover, the energy-dispersive X-ray spectroscopy (EDS) and EDS mapping data also verified the successful fabrication of Mn-ZnO2 NPs (Figure 6B, Figure S7).
Figure 6.
(A) Scheme showing the preparation of Mn-doped ZnO2 NPs through a facile cation-exchange approach. (B) EDS mapping of Mn-ZnO2 NPs. (C) The r1 values of Mn-ZnO2 NPs under different pH conditions. (D) T1-weighted MRI of U87MG tumor-bearing mice after intravenous injection of Mn-doped ZnO2 NPs. The red circles indicate the tumor area.
Inspired by the pH-dependent dissolution behavior of ZnO2 NPs, we compared the longitudinal (T1) relaxivity of Mn-ZnO2 NPs dispersed in buffer solutions with different pH values. Intriguingly, the T1 relaxation rate (r1) value increased from 0.59 to 4.68 mM-1 s-1 as the pH decreased from 7.4 to 5.5 (Figure 6C, Figure S8), revealing the pH-activated MRI contrast performance of Mn-ZnO2 NPs. Such an activatable T1 contrast effect is mainly due to the fact that pH-stimulated release of Mn2+ from Mn-ZnO2 NPs provides more efficient chemical exchange between Mn2+ ions and protons. The off-to-on contrast ability in response to specific stimuli makes Mn-ZnO2 NPs highly promising for tumor MRI in vivo. To verify this, U87MG tumor-bearing mice were injected with Mn-ZnO2 NPs through the tail vein and then imaged by an MRI scanner. As shown in Figure 6D, positive contrast effect was found at the tumor site after intravenous administration of Mn-ZnO2 NPs. Furthermore, the MRI T1 signal in the tumor region gradually increased with time, which could be attributed to the high tumor uptake of Mn-ZnO2 NPs. These results indicated that Mn-ZnO2 NPs is a promising MRI contrast agent for cancer imaging.
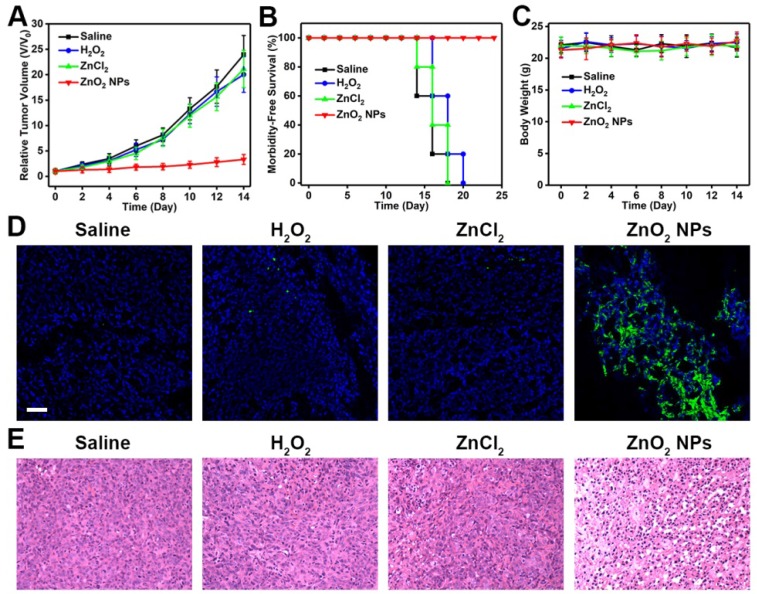
In view of the potent anticancer activity of PVP-modified ZnO2 NPs in vitro, we further investigated their feasibility for inhibiting tumor growth in vivo. Mice bearing U87MG tumors were treated with different formulations by intravenous injection, and tumor size was measured every other day using a caliper. As can be seen in Figure 7A, the growth of tumors in mice injected with ZnO2 NPs was significantly suppressed, demonstrating the high therapeutic efficacy of ZnO2-based oxidative stress inducers. In comparison, both H2O2 and ZnCl2 showed only limited tumor growth inhibition (Figure S9), most likely due to the rapid clearance after intravenous administration. Moreover, no significant body weight loss was observed after various treatments (Figure 7B,C). Hematoxylin and eosin (H&E)-stained images of major organs collected from different groups of mice at day 14 showed no obvious organ injury (Figure S10). Then, the oxidative stress-stimulated cancer cell apoptosis was determined by terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling (TUNEL) assay. Tumor tissues derived from mice treated with ZnO2 NPs had significantly more apoptotic cells as compared to that from saline-injected mice (Figure 7D). In addition, H&E staining indicated that tumors in ZnO2 NPs-treated mice exhibited severe damage (Figure 7E). The above results suggested that ZnO2 NPs are good candidates for cancer treatment in vivo.
Figure 7.
(A) Tumor growth curves of U87-bearing mice injected intravenously with different formulations. (B) Survival curves of mice in different groups. (C) Body weight changes of mice during the observation period. (D) TUNEL and (E) H&E staining of tumor tissues derived from different groups. Scale bar in d, 50 μm.
Conclusions
In summary, we have successfully developed a ZnO2 NPs-based ROS-generating nanoagent that enhances oxidative stress-mediated cancer cell killing through the collaboration of endogenous and exogenous ROS, and demonstrated its use in the fabrication of activatable theranostic nanoplatform for MRI-guided tumor treatment. After uptake by cancer cells, the pH-responsive ZnO2 NPs, in addition to releasing exogenous H2O2, also provide Zn2+ to facilitate the production of endogenous O2·- and H2O2 from mitochondrial ETC, enabling highly effective synergistic tumor therapy. The pH-dependent dissociation behavior of ZnO2 NPs, together with the fact that cancer cells are more vulnerable to additional ROS than normal cells, allows them to efficiently trigger cell apoptosis in tumor and show negligible damage to major organs. Moreover, manganese could be easily doped into ZnO2 NPs by cation exchange to impart them with pH-activated MRI contrast property, which is appropriate for monitoring the dissolution of ZnO2 NPs and subsequent therapeutic process. Our study not only demonstrates the utilization of ZnO2 nanomaterials for theranostic applications, but also provides a two-pronged strategy to further improve oxidative stress-based cancer therapy by stimulating cooperation between endogenous and exogenous ROS.
Supplementary Material
Supplementary figures and tables.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Nos. 81971621, 81671707), Natural Science Foundation of Guangdong Province (No. 2016A030311054), Research Projects of Guangzhou Science Technology and Innovation Commission (No. 201607010201), Research Fund for Lin He's Academician Workstation of New Medicine and Clinical Translation, Higher Education Colleges and Universities Innovation Strong School Project (Q17024072), and the Intramural Research Program (IRP) of the NIBIB, NIH.
Abbreviations
- ROS
Reactive oxygen species
- ZnO2 NPs
zinc peroxide nanoparticles
- H2O2
hydrogen peroxide
- O2·-
superoxide anion radical
- ETC
electron transport chain
- PVP
poly(vinylpyrrolidone)
- MOPS
3-(N-morpholino)propanesulfonic acid
- DCFH-DA
2',7'-dichlorofluorescin diacetate
- MTT
thiazolyl blue tetrazolium bromide
- PI
propidium iodide
- Mn-ZnO2
Mn-doped ZnO2
- MRI
magnetic resonance imaging
- TEM
transmission electron microscopy
- DLS
dynamic light scattering
- XPS
X-ray photoelectron spectroscopy
- DCFH-DA
2',7'-dichlorofluorescin diacetate
- H&E
hematoxylin and eosin
- TUNEL
terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling
References
- 1.Brynildsen MP, Winkler JA, Spina CS, MacDonald IC, Collins JJ. Potentiating antibacterial activity by predictably enhancing endogenous microbial ROS production. Nat Biotechnol. 2013;31:160–5. doi: 10.1038/nbt.2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma P, Xiao H, Yu C, Liu J, Cheng Z, Song H. et al. Enhanced cisplatin chemotherapy by iron oxide nanocarrier-mediated generation of highly toxic reactive oxygen species. Nano Lett. 2017;17:928–37. doi: 10.1021/acs.nanolett.6b04269. [DOI] [PubMed] [Google Scholar]
- 3.Lin LS, Song J, Song L, Ke K, Liu Y, Zhou Z. et al. Simultaneous Fenton-like ion delivery and glutathione depletion by MnO2-based nanoagent to enhance chemodynamic therapy. Angew Chem Int Ed Engl. 2018;57:4902–6. doi: 10.1002/anie.201712027. [DOI] [PubMed] [Google Scholar]
- 4.Tang Z, Zhang H, Liu Y, Ni D, Zhang H, Zhang J. et al. Antiferromagnetic pyrite as the tumor microenvironment-mediated nanoplatform for self-enhanced tumor imaging and therapy. Adv Mater. 2017;29:1701683. doi: 10.1002/adma.201701683. [DOI] [PubMed] [Google Scholar]
- 5.Su X, Shen Z, Yang Q, Sui F, Pu J, Ma J. et al. Vitamin C kills thyroid cancer cells through ROS-dependent inhibition of MAPK/ERK and PI3K/AKT pathways via distinct mechanisms. Theranostics. 2019;9:4461–73. doi: 10.7150/thno.35219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao J, Gao W, Cai X, Xu J, Zou D, Li Z. et al. Nanozyme-mediated catalytic nanotherapy for inflammatory bowel disease. Theranostics. 2019;9:2843–55. doi: 10.7150/thno.33727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giorgio M, Trinei M, Migliaccio E, Pelicci PG. Hydrogen peroxide: a metabolic by-product or a common mediator of ageing signals? Nat Rev Mol Cell Biol. 2007;8:722–8. doi: 10.1038/nrm2240. [DOI] [PubMed] [Google Scholar]
- 8.Trachootham D, Zhou Y, Zhang H, Demizu Y, Chen Z, Pelicano H. et al. Selective killing of oncogenically transformed cells through a ROS-mediated mechanism by β-phenylethyl isothiocyanate. Cancer Cell. 2006;10:241–52. doi: 10.1016/j.ccr.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 9.Gorrini C, Harris IS, Mak TW. Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discovery. 2013;12:931–47. doi: 10.1038/nrd4002. [DOI] [PubMed] [Google Scholar]
- 10.Ma X, Ren X, Guo X, Fu C, Wu Q, Tan L. et al. Multifunctional iron-based metal-organic framework as biodegradable nanozyme for microwave enhancing dynamic therapy. Biomaterials. 2019;214:119223. doi: 10.1016/j.biomaterials.2019.119223. [DOI] [PubMed] [Google Scholar]
- 11.Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discovery. 2009;8:579–91. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 12.Schumacker PT. Reactive oxygen species in cancer: a dance with the devil. Cancer Cell. 2015;27:156–7. doi: 10.1016/j.ccell.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Balaban RS, Nemoto S, Finkel T. Mitochondria, oxidants, and aging. Cell. 2005;120:483–95. doi: 10.1016/j.cell.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Esposito LA, Melov S, Panov A, Cottrell BA, Wallace DC. Mitochondrial disease in mouse results in increased oxidative stress. Proc Natl Acad Sci USA. 1999;96:4820–5. doi: 10.1073/pnas.96.9.4820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Indo HP, Davidson M, Yen HC, Suenaga S, Tomita K, Nishii T. et al. Evidence of ROS generation by mitochondria in cells with impaired electron transport chain and mitochondrial DNA damage. Mitochondrion. 2007;7:106–18. doi: 10.1016/j.mito.2006.11.026. [DOI] [PubMed] [Google Scholar]
- 16.Huang L, Li Z, Zhao Y, Yang J, Yang Y, Pendharkar AI. et al. Enhancing photodynamic therapy through resonance energy transfer constructed near-infrared photosensitized nanoparticles. Adv Mater. 2017;29:1604789. doi: 10.1002/adma.201604789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ni D, Ferreira CA, Barnhart TE, Quach V, Yu B, Jiang D. et al. Magnetic targeting of nanotheranostics enhances cerenkov radiation-induced photodynamic therapy. J Am Chem Soc. 2018;140:14971–9. doi: 10.1021/jacs.8b09374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, Lee D, Huang JD, Yoon J. Phthalocyanine-assembled nanodots as photosensitizers for highly efficient type I photoreactions in photodynamic therapy. Angew Chem Int Ed Engl. 2018;57:9885–90. doi: 10.1002/anie.201806551. [DOI] [PubMed] [Google Scholar]
- 19.Ju E, Dong K, Chen Z, Liu Z, Liu C, Huang Y. et al. Copper(II)-graphitic carbon nitride triggered synergy: improved ROS generation and reduced glutathione levels for enhanced photodynamic therapy. Angew Chem Int Ed Engl. 2016;55:11467–71. doi: 10.1002/anie.201605509. [DOI] [PubMed] [Google Scholar]
- 20.Zheng T, Wang W, Wu F, Zhang M, Shen J, Sun Y. Zwitterionic polymer-gated Au@TiO2 core-shell nanoparticles for imaging-guided combined cancer therapy. Theranostics. 2019;9:5035–48. doi: 10.7150/thno.35418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luby BM, Walsh CD, Zheng G. Advanced photosensitizer activation strategies for smarter photodynamic therapy beacons. Angew Chem Int Ed Engl. 2019;58:2558–69. doi: 10.1002/anie.201805246. [DOI] [PubMed] [Google Scholar]
- 22.Kolemen S, Ozdemir T, Lee D, Kim GM, Karatas T, Yoon J. et al. Remote-controlled release of singlet oxygen by the plasmonic heating of endoperoxide-modified gold nanorods: towards a paradigm change in photodynamic therapy. Angew Chem Int Ed Engl. 2016;55:3606–10. doi: 10.1002/anie.201510064. [DOI] [PubMed] [Google Scholar]
- 23.Li WP, Su CH, Chang YC, Lin YJ, Yeh CS. Ultrasound-induced reactive oxygen species mediated therapy and imaging using a Fenton reaction activable polymersome. ACS Nano. 2016;10:2017–27. doi: 10.1021/acsnano.5b06175. [DOI] [PubMed] [Google Scholar]
- 24.Huo M, Wang L, Chen Y, Shi J. Tumor-selective catalytic nanomedicine by nanocatalyst delivery. Nat Commun. 2017;8:357. doi: 10.1038/s41467-017-00424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang XQ, Gao F, Zhang XZ. Initiator-loaded gold nanocages as a light-induced free-radical generator for cancer therapy. Angew Chem Int Ed Engl. 2017;56:9029–33. doi: 10.1002/anie.201703159. [DOI] [PubMed] [Google Scholar]
- 26.Li J, Dirisala A, Ge Z, Wang Y, Yin W, Ke W. et al. Therapeutic vesicular nanoreactors with tumor-specific activation and self-destruction for synergistic tumor ablation. Angew Chem Int Ed Engl. 2017;56:14025–30. doi: 10.1002/anie.201706964. [DOI] [PubMed] [Google Scholar]
- 27.Wang S, Wang Z, Yu G, Zhou Z, Jacobson O, Liu Y. et al. Tumor-specific drug release and reactive oxygen species generation for cancer chemo/chemodynamic combination therapy. Adv Sci. 2019;6:1801986. doi: 10.1002/advs.201801986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang M, Shen B, Song R, Wang H, Lv B, Meng X. et al. Radiation-assisted metal ion interference tumor therapy by barium peroxide-based nanoparticles. Mater Horiz. 2019;6:1034–40. [Google Scholar]
- 29.Kolenko V, Teper E, Kutikov A, Uzzo R. Zinc and zinc transporters in prostate carcinogenesis. Nat Rev Urol. 2013;10:219–26. doi: 10.1038/nrurol.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Golovine K, Makhov P, Uzzo RG, Shaw T, Kunkle D, Kolenko VM. Overexpression of the zinc uptake transporter hZIP1 inhibits nuclear factor-kB and reduces the malignant potential of prostate cancer cells in vitro and in vivo. Clin Cancer Res. 2008;14:5376–84. doi: 10.1158/1078-0432.CCR-08-0455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franklin RB, Costello LC. Zinc as an anti-tumor agent in prostate cancer and in other cancers. Arch Biochem Biophys. 2007;463:211–7. doi: 10.1016/j.abb.2007.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dineley KE, Richards LL, Votyakova TV, Reynolds IJ. Zinc causes loss of membrane potential and elevates reactive oxygen species in rat brain mitochondria. Mitochondrion. 2005;5:55–65. doi: 10.1016/j.mito.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Kleiner D. The effect of Zn2+ ions on mitochondrial electron transport. Arch Biochem Biophys. 1974;165:121–5. doi: 10.1016/0003-9861(74)90148-9. [DOI] [PubMed] [Google Scholar]
- 34.Costello LC, Franklin RB. A comprehensive review of the role of zinc in normal prostate function and metabolism; and its implications in prostate cancer. Arch Biochem Biophys. 2016;611:100–12. doi: 10.1016/j.abb.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ding WQ, Liu B, Vaught JL, Yamauchi H, Lind SE. Anticancer activity of the antibiotic clioquinol. Cancer Res. 2005;65:3389–95. doi: 10.1158/0008-5472.CAN-04-3577. [DOI] [PubMed] [Google Scholar]
- 36.Magda D, Lecane P, Wang Z, Hu W, Thiemann P, Ma X. et al. Synthesis and anticancer properties of water-soluble zinc ionophores. Cancer Res. 2008;68:5318–25. doi: 10.1158/0008-5472.CAN-08-0601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ding WQ, Yu HJ, Lind SE. Zinc-binding compounds induce cancer cell death via distinct modes of action. Cancer Lett. 2008;271:251–9. doi: 10.1016/j.canlet.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 38.Fang J, Sawa T, Akaike T, Maeda H. Tumor-targeted delivery of polyethylene glycol-conjugated D-amino acid oxidase for antitumor therapy via enzymatic generation of hydrogen peroxide. Cancer Res. 2002;62:3138–43. [PubMed] [Google Scholar]
- 39.Fang J, Deng D, Nakamura H, Akuta T, Qin H, Iyer AK. et al. Oxystress inducing antitumor therapeutics via tumor-targeted delivery of PEG-conjugated D-amino acid oxidase. Int J Cancer. 2008;122:1135–44. doi: 10.1002/ijc.22982. [DOI] [PubMed] [Google Scholar]
- 40.Bai H, Liu X. Green hydrothermal synthesis and photoluminescence property of ZnO2 nanoparticles. Materials Lett. 2010;64:341–3. [Google Scholar]
- 41.Dupin JC, Gonbeau D, Vinatier P, Levasseur A. Systematic XPS studies of metal oxides, hydroxides and peroxides. Phys Chem Chem Phys. 2000;2:1319–24. [Google Scholar]
- 42.Chen WH, Luo GF, Qiu WX, Lei Q, Hong S, Wang SB. et al. Programmed nanococktail for intracellular cascade reaction regulating self-synergistic tumor targeting therapy. Small. 2016;12:733–44. doi: 10.1002/smll.201503280. [DOI] [PubMed] [Google Scholar]
- 43.Ju E, Chen Z, Li W, Dong K, Wang Z, Liu Z. et al. Embedding magnetic nanoparticles into coordination polymers to mimic zinc ion transporters for targeted tumor therapy. Chem Commun. 2016;52:12598–601. doi: 10.1039/c6cc06467a. [DOI] [PubMed] [Google Scholar]
- 44.He D, He X, Yang X, Li HW. A smart ZnO@polydopamine-nucleic acid nanosystem for ultrasensitive live cell mRNA imaging by the target-triggered intracellular self-assembly of active DNAzyme nanostructures. Chem Sci. 2017;8:2832–40. doi: 10.1039/c6sc04633a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang ZY, Xu YD, Ma YY, Qiu LL, Wang Y, Kong JL. et al. Biodegradable ZnO@polymer core-shell nanocarriers: pH-triggered release of doxorubicin in vitro. Angew Chem Int Ed Engl. 2013;52:4127–31. doi: 10.1002/anie.201300431. [DOI] [PubMed] [Google Scholar]
- 46.Shen S, Zhu C, Huo D, Yang M, Xue J, Xia Y. A hybrid nanomaterial for the controlled generation of free radicals and oxidative destruction of hypoxic cancer cells. Angew Chem Int Ed Engl. 2017;56:8801–4. doi: 10.1002/anie.201702898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin LS, Huang T, Song J, Ou XY, Wang Z, Deng H. et al. Synthesis of copper peroxide nanodots for H2O2 self-supplying chemodynamic therapy. J Am Chem Soc. 2019;141:9937–45. doi: 10.1021/jacs.9b03457. [DOI] [PubMed] [Google Scholar]
- 48.Noh J, Kwon B, Han E, Park M, Yang W, Cho W. et al. Amplification of oxidative stress by a dual stimuli-responsive hybrid drug enhances cancer cell death. Nat Commun. 2015;6:6907. doi: 10.1038/ncomms7907. [DOI] [PubMed] [Google Scholar]
- 49.Lin LS, Cong ZX, Li J, Ke KM, Guo SS, Yang HH. et al. Graphitic-phase C3N4 nanosheets as efficient photosensitizers and pH-responsive drug nanocarriers for cancer imaging and therapy. J Mater Chem B. 2014;2:1031–7. doi: 10.1039/c3tb21479f. [DOI] [PubMed] [Google Scholar]
- 50.Qi T, Chen B, Wang Z, Du H, Liu D, Yin Q. et al. A pH-activatable nanoparticle for dual-stage precisely mitochondria-targeted photodynamic anticancer therapy. Biomaterials. 2019;213:119219. doi: 10.1016/j.biomaterials.2019.05.030. [DOI] [PubMed] [Google Scholar]
- 51.Cheng H, Zheng RR, Fan GL, Fan JH, Zhao LP, Jiang XY. et al. Mitochondria and plasma membrane dual-targeted chimeric peptide for single-agent synergistic photodynamic therapy. Biomaterials. 2019;188:1–11. doi: 10.1016/j.biomaterials.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 52.Szeto HH. Cell-permeable, mitochondrial-targeted, peptide antioxidants. AAPS J. 2006;8:E277. doi: 10.1007/BF02854898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin LS, Yang X, Zhou Z, Yang Z, Jacobson O, Liu Y. et al. Yolk-shell nanostructure: an ideal architecture to achieve harmonious integration of magnetic-plasmonic hybrid theranostic platform. Adv Mater. 2017;29:1606681. doi: 10.1002/adma.201606681. [DOI] [PubMed] [Google Scholar]
- 54.Ke K, Yang W, Xie X, Liu R, Wang LL, Lin WW. et al. Copper manganese sulfide nanoplates: a new two-dimensional theranostic nanoplatform for MRI/MSOT dual-modal imaging-guided photothermal therapy in the second near-infrared window. Theranostics. 2017;7:4763–76. doi: 10.7150/thno.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lin LS, Song J, Yang HH, Chen X. Yolk-shell nanostructures: design, synthesis, and biomedical applications. Adv Mater. 2018;30:1704639. doi: 10.1002/adma.201704639. [DOI] [PubMed] [Google Scholar]
- 56.Hameed S, Bhattarai P, Liang X, Zhang N, Xu Y, Chen M. et al. Self-assembly of porphyrin-grafted lipid into nanoparticles encapsulating doxorubicin for synergistic chemo-photodynamic therapy and fluorescence imaging. Theranostics. 2018;8:5501–18. doi: 10.7150/thno.27721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang S, Zhou Z, Wang Z, Liu Y, Jacobson O, Shen Z. et al. Gadolinium metallofullerene-based activatable contrast agent for tumor signal amplifcation and monitoring of drug release. Small. 2019;15:1900691. doi: 10.1002/smll.201900691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lin LS, Cong ZX, Cao JB, Ke KM, Peng QL, Gao J. et al. Multifunctional Fe3O4@polydopamine core-shell nanocomposites for intracellular mRNA detection and imaging-guided photothermal therapy. ACS Nano. 2014;8:3876–83. doi: 10.1021/nn500722y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang H, Lovell JF. Advanced functional nanomaterials for theranostics. Adv Funct Mater. 2017;27:1603524. doi: 10.1002/adfm.201603524. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures and tables.