Abstract
Background:
This study assessed the effectiveness of mirror therapy (MT) on muscle elasticity, pain, and function in patients with mutilating injuries.
Methods:
Thirty patients with impaired function due to mutilating injuries were assigned randomly to experimental or control group. The experimental group (n = 15) received MT (30 minutes a day, 3 days a week for 4 weeks) and conventional physical therapy after each MT session while the control group (n = 15) only received conventional physical therapy.
Results:
There were significant differences in pain and hand function within each group (pre-intervention vs post-intervention) and between groups (experimental vs control) (P < .05). However, there was no significant difference in muscle elasticity between groups (P > .05).
Conclusion:
Although MT cannot result in significant changes in muscle elasticity in a clinical setting, it does have positive effects by reducing pain and improving hand function. Thus, MT can be effective for patients with impaired function due to mutilating injuries.
Keywords: hand function, mirror therapy, muscle elasticity, mutilating injury, pain
1. Introduction
Our hands are exposed to risk of being damaged during use at any time. Even if the damage is minor at first, it may lead to stiffness and loss of function of finger. It also increases the risk of hand function loss depending on the size of injury.[1] Severe trauma on extremity often causes major injuries to various soft tissue components. Such traumatic injuries can lead to mutilated injuries.[2]
Due to mutilated injuries, multiple injuries to skin, vascular, nerve, tendon, muscle, bone, and soft tissue envelope around joints might occur.[3] For these reasons, we need to establish appropriate treatment plan with meticulous execution to recover original hand function because various tissues are lost in mutilated injuries.[4] Outcome/prognosis depends on the severity, type, and location of the injury.[5] It also greatly depends on the method of surgery and postoperative treatment.[6]
Patient with mutilated injury might experience various problems in combination. Pain is the most common problem encountered by such patient. It is associated with complex regional pain syndrome or dysfunction due to cumulated trauma. Approximately 80% of patients with amputation complain of persistent pain due to neuroma formation and complex regional pain syndrome.[2]
In addition, patients with mutilated hand injuries of fingers or concurrent injuries in various tissues have limited whole body function and limited daily living and occupational activities besides hand dysfunction. In these patients, loss of muscle may occur due to amputation. In addition, the use of many digits becomes impossible, resulting in instability of wrist and weakness of intrinsic muscle, extrinsic muscle of the hand, and muscles around the wrist.
If there is a mechanical deficit in the hand, sensorimotor contribution can affect dynamic stability of the joint since afferent input of the mechanoreceptor is reduced.[7] Flexor carpi ulnaris (FCU), flexor carpi radialis (FCR), and extensor carpi radialis (ECR) are muscles that aid in wrist stabilization.[8] The dynamic stability is influenced by proprioceptive information and neuromuscular activity essential for neuromuscular control.[9,10]
To improve proprioception, various methods have recently been proposed. One of such methods is mirror therapy (MT), a simple, easy to understand, cost-effective, and patient-centered treatment.[11] MT is also applicable to patients with mutilated hand injuries that can be treated without direct movement of the affected side or physical force.
MT was first introduced by Ramachandran and Rogers-Ramachandran.[12] It was designed to treat patients with phantom pain in upper extremity amputation by using visual illusion and phantom. When performing a MT, the patient puts both hands on either sides of the mirror, placing the injured hand behind the mirror, the non-injured hand in front of the mirror, and paying full attention to the mirror. In this state, the patient sees the reflected image of the healthy hand instead of the injured hand, resulting in recognition of his/her 2 normal hands.[13]
It is generally accepted that brain can recognize feedback on visual sensory rather than feedback on somatosensory and proprioception. According to this principle, MT is a treatment method based on neuroplasticity of the brain.[14] The visual effect on motor sensory is important. Even an illusion of a moving hand can activate the cerebral cortex just like a real hand move.[15]
In a study of functional brain image, we have observed that a normal person’ brain in the primary motor area which is connected to the opposite hand is also excited by the illusion of moving hand using a mirror.[16] Based on observation of waist motion, illusion of motor sensory can be generated in injured wrist. It even stimulates activity in somatosensory,[17] thus improving reeducation of functional proprioception and contributing to important cortex control.[18]
In previous studies, successful MT for complex regional pain syndrome,[19,20] phantom pain,[21,22] and stroke[23] treatment has been reported. Although recent studies have demonstrated the benefit of mirror therapy for various diseases, research that applies MT to improve the restorative capability of hand function of patients with reduced hand function due to mutilated injury has not been reported yet. Therefore, the objective of this study was to apply MT to patients with mutilated hand injury and examine the effect of MT on muscle function, pain, and activities of daily living so that we could establish a clinical basis to provide better functional recovery.
2. Methods
Subjects were patients who underwent physical therapy after surgery due to mutilated hand injury in W hospital located in D city. Inclusion criteria were: scored ≥70 in patient-rated wrist evaluation among subjects with lower hand function due to mutilated hand injuries, scored ≥100 in hand injury severity scoring system,[24] not showing dysfunction of the non-involved side, no visual field defect, no difficulty in performing MT due to cognitive impairment, and no paralysis due to peripheral neuropathy. Patients with other pathological symptoms in the hand and wrist and patients who had metabolic diseases such as diabetes mellitus and blood pressure that could affect restoration of the involved side were excluded.
Thirty patients who met the inclusion criteria were finally enrolled. The Research Ethics Committee of Daegu University approved this study (1040621–201801-HR-001–02). All participants provided informed written consent prior to enrollment in the study. After initial assessment was completed, subjects were randomly assigned to an experimental group (n = 15) or a control group (n = 15). For randomization, sealed envelopes were prepared in advance and marked inside with A (experimental group) or B (control group). The randomization was done by a third party who was unaware of the study content. Subjects’ characteristics and all outcome measures before and after treatment were assessed by Physician 1 who was blinded to treatment allocations. The intervention was administered in a closed room by Physician 2 who was not involved in the assessment of subjects. Both physicians were instructed not to communicate with subjects about possible goals or rationale of either treatment.
The sample size this study was calculated using the G∗ Power program 3.1.0 (G power program Version 3.1, Heinrich-Heine-University Düsseldorf, Düsseldorf, Germany). Based on data from Ji and Kim study,[25] the estimated sample size required to obtain minimum power of 80% at a significant alpha level of 95% was 28. Accordingly, 30 participants were recruited to account for a potential dropout rate of 20%.
2.1. Interventions
Subjects in the experimental group received mirror therapy and conventional rehabilitation therapy for a total of 60 minutes (MT: 30 minutes, conventional rehabilitation therapy: 30 minutes) per day. Subjects in the experimental group received training 3 days per week for 4 weeks. For the MT, we applied intervention by modifying the program used in the study of Rosén and Lundborg[26] and Rostami et al.[13]
To implement this mirror therapy, we used bilateral method to receive their visual feedback from the mirror. We asked subjects to sit in front of the table, insert an involved hand in the mirror box on their midline, and see the non-involved hand reflected in the mirror. This MT consisted of 3 parts as follows: during the first 10 minutes, the subject was asked to follow the involved hand that did the mimicking while the non-involved side was performing wrist flexion, wrist extension, ulnar deviation, radial deviation, supination, pronation, and closing hand and opening hand (Fig. 1); during the next 10 minutes, subjects were instructed to perform a sandbag, putty, and hand grip exercise with a resistive exercise for the non-involved side (Fig. 2); during the last 10 minutes, subjects were instructed to perform a moving small object (ball of wool) and card flip operation to induce wrist and finger movements as functional activities (Fig. 3). Subjects were given a rest time of 20 seconds in each activity and a 1-minute break in each segment in order to reduce fatigue of the non-involved hand. Conventional rehabilitation therapy consisting of whirlpool, transcutaneous electrical nerve stimulation, range of motion exercise was administered by therapists blinded to the study protocol and subjects’ group assignment. Subjects in the control group only received conventional rehabilitation therapy for a total of 30 minutes per day on the same day.
Figure 1.
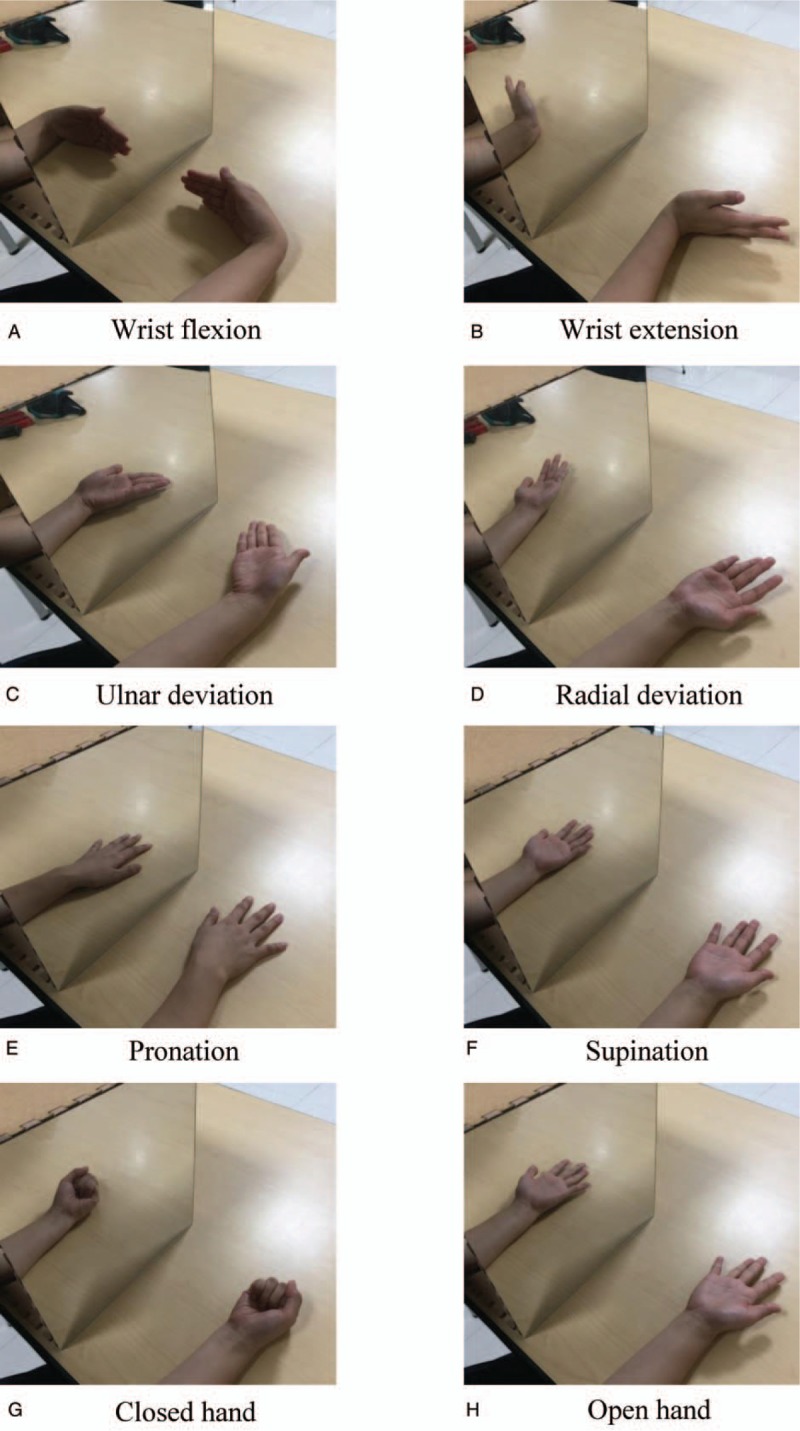
Imitating the motion. Subject was asked to follow the involved hand that did the mimicking while the non-involved side was performing wrist flexion, wrist extension, ulnar deviation, radial deviation, supination, pronation, and closing hand and opening hand.
Figure 2.
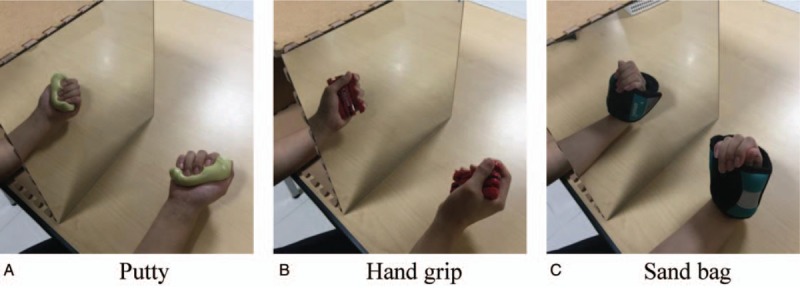
Resistive exercise. Subjects were instructed to perform a sandbag, putty, and hand grip exercise with a resistive exercise for the non-involved side.
Figure 3.
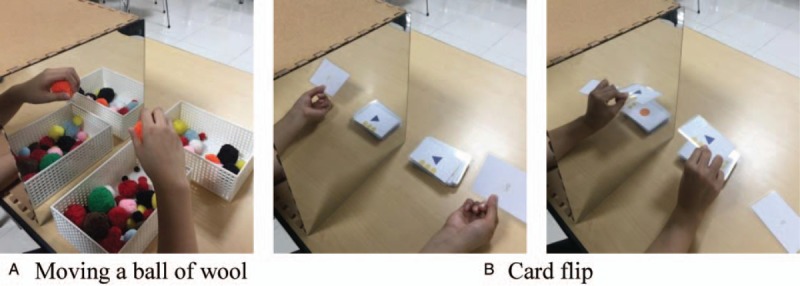
Functional activities. Subjects were instructed to perform a moving small object (ball of wool) and card flip operation to induce wrist and finger movements as functional activities.
2.2. Outcome measures
2.2.1. Muscle elasticity
A muscle elasticity measuring instrument (MyotonPRO, Myton AS, Estonia) was used in this study.
The MyotonPRO is a small, portable, handheld device for measuring mechanical muscle properties.[27] Measurement consists of 3 main components: exertion of mechanical impulse, registration of co-oscillation, and computation of parameters.
The tip of the 3-mm diameter probe is applied perpendicular to the skin surface above the muscle that is being measured. A constant prepressure (0.18 N) is applied, whereby the subcutaneous superficial tissues are slightly compressed. A brief (15 ms), low force (0.4 N) mechanical impulse is then transmitted to the underlying muscle. The subsequent dampened oscillation of the muscle is recorded by an accelerometer and simultaneously quantifies and displays the muscle properties.[27]
Such instrument provides portability with small cost clinically. It can create simple mechanical pressures on the body surface. Its approach is non-invasive using small probes.[28] Subjects were asked to sit in front of the table in a correct position, placing the forearm on the table. They were asked to take a neutral position. FCU, FCR, and ECR muscles of the involved side were measured and muscle elasticity of these muscles was measured at the center of the muscle belly. More specifically, the FCU is the proximal third segment between the medial epicondyle and ulna styloid process, the FCR muscle is 4 to 5 cm below the midpoint of the elbow crease, and the ECR is the proximal third segment between the lateral epicondyle and the styloid process of radius.[29] We measured 3 times for the above MT and conducted comparative analysis for the average value resulting from these measurements. In a study of muscle elasticity measurements using a muscle elasticity measuring instrument, there was a high interclass correlation coefficient (ICC 3.1 > 0.90).[30]
2.2.2. Pain
For each subject, the pain was measured by verbally questioning the condition of the involved side in the pre- and post-experiment. The Pain method measures patient's present condition on a 100 mm horizontal line. It uses a visual analogue scale with increments from 0 meaning no pain to 10 indicating severe pain. In a reliability analysis of patients with chronic musculature disease, 0.71 to 0.78 was shown on a visual analogue scale (VAS). This value was found to be more than moderate.[31]
2.2.3. Hand function
The hand function was assessed using the Korean version of patient rated wrist evaluation (PRWE).[32] Patient was rated with the wrist evaluation questionnaire consisting of 15 questions divided into 2 subscales to assess pain (5 questions) and function (10 questions). The function subscale was further subdivided into special activities (5 questions) and usual activities (5 questions). Questions were scored on a 10-point Likert scale ranging from no pain or no difficulty (0 point) to worst pain imaginable or unable to perform the task (10 points). PRWE-pain score was the sum of scored responses to the 5 pain questions, with a maximum score of 50. PRWE-function score was the sum of scored responses to the 10 questions divided by 2. PRWE-pain and PRWE-function scores were then summed to obtain PRWE score. The test–retest reliability (ICCs > 0.90) of the patient-rated wrist evaluation was very high.[33] Cronbach α and ICCs of the Korean version of patient-wrist evaluation were 0.94 and 0.96, respectively.[32]
2.3. Data analysis
Before therapy, differences in general characteristics of the experimental group and the control group were compared using independent t test and chi-square test. Comparisons of variables before and after training within each group were made using paired samples t test. Comparisons of pre- and post-test differences in variables between the experimental group and the control group were performed using independent t test. Statistical software SPSS version 20.0 (SPSS, Chicago, IL) was used for all statistical analyses. The level of significance was set at P < .05.
3. Results
Flow chart for this study is shown in Fig. 4. Table 1 provides a summary of clinical and demographic features of the sample (n = 30). There were no significant (P > .05) differences in baseline characteristics between the 2 groups. Thirty subjects (experimental group = 15, control group = 15) completed this experiment. Characteristics of the 2 groups (n = 30) before and after intervention are shown in Table 2. The experimental group showed significant improvements of ECR in muscle elasticity, VAS, and PRWE score after intervention compared with preintervention results (P < .05). The control group also showed significant improvements in VAS and PRWE score after the intervention compared with preintervention results (P < .05). There were also significant differences in post-training gains of VAS and PRWE score between the experimental group and the control group (P < .05). In addition, the effect size for gains in the experimental and control groups was strong (effect size = 0.78, 1, 18, respectively) (Tables 3 and 4).
Figure 4.
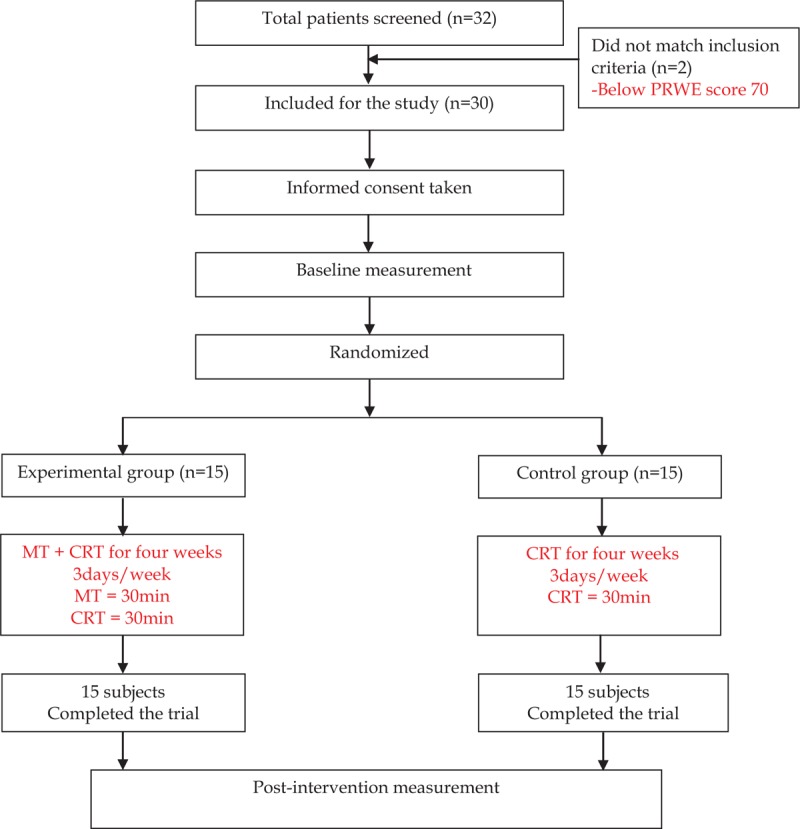
Study flowchart. Flow chart for this study is shown.
Table 1.
General characteristics of subjects (n = 30).
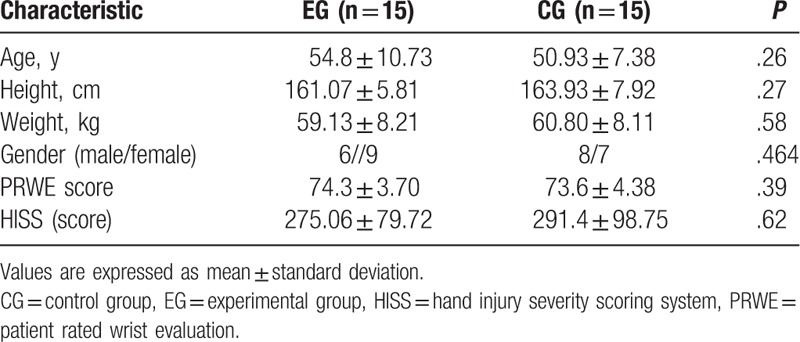
Table 2.
Comparison of changes in muscle elasticity of the experimental group and control group with values presented as mean (standard deviation).
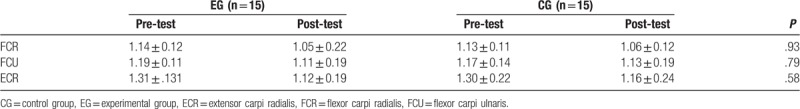
Table 3.
Comparison of changes in pain of the experimental group and control group with values presented as mean (standard deviation).
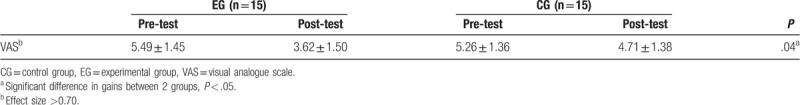
Table 4.
Comparison of changes in hand function of the experimental group and control group with values presented as mean (standard deviation).

4. Discussion
After 4 weeks of MT, significant improvements in hand function and decrease in pain were observed for the experimental group compared with the control group. These results supported the primary hypothesis that mirror therapy would have positive effects on function recovery in patients with mutilating injuries.
Muscle elasticity refers to the ability of a tissue to recover its shape after it has been deformed. The smaller the measured value, the higher the elasticity.[34] There was a significant difference in the elasticity of the ECR in the experimental group before and after the intervention. However, there was no significant difference for the control group. In addition, we found that elasticity of the experimental group was increased by 4.24% compared with that of the control group, although such difference was not statistically significant. After the intervention, the elasticity of the FCU or FCR was increased in both the experimental group and the control group. The experimental group tended to be 1.73% or 3.7% higher for the elasticity of the FCU or FCR, respectively, than the control group. However, the difference between the 2 groups was not statistically significant.
In this study, the elasticity of wrist extensor tended to be increased more than that of the wrist flexor for subjects in both experimental group and control group. This result suggests that intrinsic and extrinsic structures of the hand might have been damaged in patients with mutilated hand injury, resulting in loss of finger function and stiffness.[1] Wrist flexors might have also been used more often than wrist extensor because they are relatively stiffer or shorter due to repeated use.[35] Therefore, contraction of the wrist flexor might be caused by compensation during finger flexion contraction.
Ramachandran and Altschuler[36] have found that pain release associated with MT is due to combined manipulation of sensory and motor in the central nervous system and that some pain conditions could be mediated by inconsistent sensory information and motor information. Thus, they have suggested that sensory correction feedback is provided to restore coincidence between motor output and sensory input in MT.
In the present study, significant decrease in pain was observed in both experimental group and control group. In the comparison between the 2 groups, it was confirmed that there was a significant reduction (by 23.70%, P = .04) in pain in the experimental group compared with the control group. Thus, a synergic effect between the conventional physical therapy and MT might have been induced, leading to greater pain reduction effect in the experimental group.
Boesch et al[37] have shown that phantom limb and complex regional pain syndrome are significantly reduced (standardized mean difference = –1.11; 95% CI: –0.56 to –1.66; P < .0001) in meta-analysis of 2 randomized controlled trials on the effect of 4-week-long mirror therapy. The MT is usually used to reduce anxiety and fear associated with movement of painful body parts. Through visual feedback of the normally moving extremity, it breaks the link between fear of pain and movement.[38] MT can also help reduce sensory input and pain by removing the painful extremity without thinking about pain.[39]
In general, functional impairment due to amputation of the hand is affected by amputation level. Each finger has an inherent role. According to the guideline from the evaluation of permanent impairment conducted by the American medical association, loss of thumb is equal to 40% loss of function of the hand and 25% loss of the whole body function. Thumb has been confirmed to be important for grip strength.[1]
In this study, functional improvements in the experimental group (MT combined conventional physical therapy) and the control group (conventional physical therapy only) were examined. As a result, both the experimental group and the control group showed significant decrease in patient rated wrist evaluation. In the comparison of the 2 groups, the experimental group showed significantly more reduction (≥10%) than the control group.
Walenkamp et al[40] have reported that the value of minimal clinically important difference is about 11.5. In the present study, the difference in patient rated wrist evaluation score between before and after intervention was 12.90 ± 7.98 for the experimental group and 5.57 ± 4.45 for the control group. The difference in score in the control group exceeded the minimal clinically important difference values of PRWE claimed by previous researchers. Therefore, MT is significant in improving hand function based on patient rated wrist evaluation.
Rostami et al[13] have suggested that patients with orthopedic disorders of hand show better improvement in hand function than the control group, including significant improvements for total active motion and disability of the arm, shoulder and hand (DASH) in the MT group that received traditional physical therapy at same time.
The current study has some limitations. First, the small sample size might have influenced certain variables and the results. Therefore, these results cannot be generalized to all patients with mutilating injuries. Second, due to absence of follow-up after completion of MT, the durability of the effect of this intervention could not be determined. Third, various functional measurements were not performed to determine functional benefit in terms of activities of daily living. Hence, further studies with longer follow-up assessment are needed to evaluate the long-term benefit of mirror therapy.
5. Conclusion
There were significant differences in pain and hand function within each group (pre-intervention vs post-intervention) and between groups (experimental vs control). However, there was no significant difference in muscle elasticity between groups.
Therefore, we suggest that patients with mutilating injuries who received MT along with conventional physical therapy showed significant improvements in hand function and pain reduction.
Author contributions
Conceptualization: Da-Eun Yun.
Data curation: Myoung-Kwon Kim.
Investigation: Da-Eun Yun.
Formal analysis: Da-Eun Yun.
Funding acquisition: Da-Eun Yun.
Methodology: Myoung-Kwon Kim.
Project administration: Myoung-Kwon Kim.
Resources: Myoung-Kwon Kim.
Software: Myoung-Kwon Kim.
Writing – original draft: Da-Eun Yun.
Writing – review & editing: Da-Eun Yun, Myoung-Kwon Kim.
Footnotes
Abbreviations: ECR = extensor carpi radialis, FCR = flexor carpi radialis, FCU = flexor carpi ulnaris, MT = mirror therapy, PRWE = patient rated wrist evaluation, VAS = visual analogue scale.
This study was supported by a Daegu University Research Grant (2018).
The authors have no conflicts of interest to disclose.
References
- [1].Neumeister MW, Brown RE. Mutilating hand injuries: principles and management. Hand Clin 2003;19:1–5. [DOI] [PubMed] [Google Scholar]
- [2].Ng ZY, Salgado CJ, Moran SL, et al. Soft tissue coverage of the mangled upper extremity. Semin Plast Surg 2015;29:48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Chan SW, LaStayo P. Hand therapy management following mutilating hand injuries. Hand Clin 2003;19:133–48. [DOI] [PubMed] [Google Scholar]
- [4].Alphonsus CK. Principles in the management of a mangled hand. Indian J Plast Surg 2011;44:219–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Waikakul S, Sakkarnkosol S, Vanadurongwan V, et al. Result of 1018 digital replantations in 552 patients. Inj Int J Care Injured 2000;31:33–40. [DOI] [PubMed] [Google Scholar]
- [6].Stewart Pettengill K. Rehabilitation of the Hand. St. Louis: Mosby; 2002. [Google Scholar]
- [7].Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Man Ther 2015;20:368–77. [DOI] [PubMed] [Google Scholar]
- [8].Salva-Coll G, Garcia-Elias M, Leon-Lopez MT, et al. Effects of forearm muscles on carpal stability. J Hand Surg Eur Vol 2011;2:553–9. [DOI] [PubMed] [Google Scholar]
- [9].Skirven TM. Rehabilitation of the Hand and Upper Extremity. 6th ed.Philadelphia: Elsevier Mosby; 2011. [Google Scholar]
- [10].Salva-Coll G, Garcia-Elias M, Hagert E. Scapholunate instability: proprioception and neuromuscular control. J Wrist Surg 2013;2:136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gunes Y, Ruud S, Nebahat S, et al. Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 2008;89:393–8. [DOI] [PubMed] [Google Scholar]
- [12].Ramachandran VS, Rogers-Ramachandran D. Synaesthesia in phantom limbs induced with mirrors. Proc Biol Sci 1996;263:377–86. [DOI] [PubMed] [Google Scholar]
- [13].Rostami HR, Arefi A, Tabatabaei S. Effect of mirror therapy on hand function in patients with hand orthopaedic injuries: a randomized controlled trial. Disabil Rehabil 2013;35:1647–51. [DOI] [PubMed] [Google Scholar]
- [14].Moseley GL, Gallace A, Spence C. Is mirror therapy all it is cracked up to be? Current evidence and future directions. Pain 2008;138:7–10. [DOI] [PubMed] [Google Scholar]
- [15].Naito E, Ehrsson HH. Kinesthetic illusion of wrist movement activates motor-related areas. Neuroreport 2001;12:3805–9. [DOI] [PubMed] [Google Scholar]
- [16].Garry MI, Loftus A, Summers J. Mirror, mirror on the wall: viewing a mirror reflection of unilateral hand movements facilitates ipsilateral M1 excitability. Exp Brain Res 2005;163:118–22. [DOI] [PubMed] [Google Scholar]
- [17].Avikainen S, Forss N, Hari R. Modulated activation of the human SI and SII cortices during observation of hand actions. Neuroimage 2002;15:640–6. [DOI] [PubMed] [Google Scholar]
- [18].Hagert E. Proprioception of the wrist joint: a review of current concepts and possible implications on the rehabilitation of the wrist. J Hand Ther 2010;23:2–16. [DOI] [PubMed] [Google Scholar]
- [19].McCabe CS, Haigh RC, Ring EF, et al. A controlled pilot study of the utility of mirror visual feedback in the treatment of complex regional pain syndrome (type 1). Rheumatology (Oxford) 2003;42:97–101. [DOI] [PubMed] [Google Scholar]
- [20].Cacchio A, de Blasis E, de Blasis V, et al. Mirror therapy in complex regional pain syndrome type 1 of the upper limb in stroke patients. Neurorehabil Neural Repair 2009;23:792–9. [DOI] [PubMed] [Google Scholar]
- [21].Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med 2007;357:2206–7. [DOI] [PubMed] [Google Scholar]
- [22].Diers M, Christmann C, Koeppe C, et al. Mirrored, imagined and executed movements differentially activate sensorimotor cortex in amputees with and without phantom limb pain. Pain 2010;149:296–304. [DOI] [PubMed] [Google Scholar]
- [23].Yavuzer G, Selles R, Sezer N, et al. Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 2008;89:393–8. [DOI] [PubMed] [Google Scholar]
- [24].Campbell DA, Kay SP. The hand injury severity scoring system. J Hand Surg Br 1996;21:295–8. [DOI] [PubMed] [Google Scholar]
- [25].Ji SG, Kim MK. The effects of mirror therapy on the gait of subacute stroke patients: a randomized controlled trial. Clin Rehabil 2015;29:348–54. [DOI] [PubMed] [Google Scholar]
- [26].Rosén B, Lundborg G. Training with a mirror in rehabilitation of the hand. Scand J Plast Reconstr Surg Hand Surg 2005;39:104–8. [DOI] [PubMed] [Google Scholar]
- [27].Myoton MyotonPRO User Manual. 6 ed.London: Myoton; 2013. [Google Scholar]
- [28].Nair K, Masi AT, Andonian BJ, et al. Stiffness of resting lumbar myofascia in healthy young subjects quanti fied using a handheld myotonometer and concurrently with surface electromyography monitoring. J Bodyw Mov Ther 2016;20:388–96. [DOI] [PubMed] [Google Scholar]
- [29].Bizzini M, Mannion AF. Reliability of a new, handheld device for assessing skeletal muscle stiffness. Clin Biomech 2003;18:459–61. [DOI] [PubMed] [Google Scholar]
- [30].Aird L, Samuel D, Stokes M. Quadriceps muscle tone, elasticity and stiffness in older males: reliability and symmetry using the MyotonPRO. Arch Gerontol Geriatr 2012;55:e31–9. [DOI] [PubMed] [Google Scholar]
- [31].Boonstra AM, Schiphorst Preuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31:165–9. [DOI] [PubMed] [Google Scholar]
- [32].Kim JK, Kang JS. Evaluation of the Korean version of the patient-rated wrist evaluation. J Hand Ther 2013;26:238–43. [DOI] [PubMed] [Google Scholar]
- [33].MacDermid JC, Turgeon T, Richards RS, et al. Patient rating of wrist pain and disability: a reliable and valid measurement. J Orthop Trauma 1998;12:577–86. [DOI] [PubMed] [Google Scholar]
- [34].Gavronski G, Veraksits A, Vasar E, et al. Evaluation of viscoelastic parameters of the skeletal muscles in junior triathletes. Physiol Meas 2007;28:625–37. [DOI] [PubMed] [Google Scholar]
- [35].Sahrmann S. Movement System Impairment Syndromes of the Extremities, Cervical and Thoracic Spines. 2011;Philadelphia: Elsvier Mosby, 2011. [Google Scholar]
- [36].Ramachandran VS, Altschuler EL. The use of visual feedback, in particular mirror visual feedback. in restoring brain function. Brain 2009;132:1693–710. [DOI] [PubMed] [Google Scholar]
- [37].Boesch E, Bellan V, Moseley GL, et al. The effect of bodily illusions on clinical pain: a systematic review and meta-analysis. Pain 2016;157:516–29. [DOI] [PubMed] [Google Scholar]
- [38].Wand BM, Tulloch VM, George PJ, et al. Seeing it helps: movement-related back pain is reduced by visualization of the back during movement. Clin J Pain 2012;28:602–8. [DOI] [PubMed] [Google Scholar]
- [39].McCabe C. Mirror visual feedback therapy: a practical approach. J Hand Ther 2011;24:170–8. [DOI] [PubMed] [Google Scholar]
- [40].Walenkamp MM, de Muinck Keizer RJ, Goslings JC, et al. The minimum clinically important difference of the patient-rated wrist evaluation score for patients with distal radius fractures. Clin Orthop Relat Res 2015;473:3235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]


