Abstract
Rationale:
We present 2 cases of lateral incomplete impending fracture of the femoral neck without trauma in elderly patients taking long-term bisphosphonate (BP) treatment, and we defined it as atypical femoral neck fracture (AFNF). To the best of our knowledge, this is the first report on the follow-up results of AFNF.
Patient concerns:
Patients in both cases had been taking BP drugs for a long time with osteoporosis. The duration of BP treatment was 6 years, and there was no history of repeated stresses.
Diagnoses:
All fractures were linear at the lateral aspect of the mid portion of the femoral neck, and the BMD of the femoral neck was −0.9, and −1.8, respectively.
Interventions:
Internal fixation was performed in both cases (73 years, 68 years) using cannulated screws.
Outcomes:
In both patients who underwent screw fixation, the fracture line started to extend distally at 4 weeks and 2 weeks following surgery. In the 3-month follow-up image, the length of the fracture increased by 20.1 mm and 9.9 mm, respectively. There was a problem with active rehabilitation, and the possibility of revision was also found to be a burden in terms of mortality and cost in older patients.
Lessons:
In the case of AFNF, guidelines for treatment should be set in consideration of the decreased bone healing, even when the fracture pattern is simple. Arthroplasty based on a wider indication may be worth considering.
Keywords: atraumatic, atypical, bisphosphonate, femoral neck fracture, osteoporosis
1. Introduction
Bisphosphonates (BP) reduce the incidence of vertebral and nonvertebral fractures by inhibiting bone remodeling processes, increasing bone mineral density (BMD), and increasing bone mechanical properties such as toughness.[1] However, prolonged use of BP may result in the accumulation of microdamage due to a decrease in long-term osteoclast function[2,3] and bone heterogeneity, leading to the deterioration of bone quality and eventual complications of atypical femoral fractures (AFF).[4]
Since the first publication of AFF by Odvina et al in 2005,[5] reports and studies on AFF have continuously been published. In 2010, the American Society for Bone and Mineral Research (ASMBR) published diagnostic criteria for AFF by reviewing the published literature on AFF.[6] In 2014, a revised version of this criteria was announced.[7] According to ASMBR, the premise of the definition of AFF is that the fracture line should be located in the femoral diaphysis area, just proximal to the supracondylar flare and just distal to the lesser trochanter.
In this paper, we report 2 cases of lateral incomplete impending fracture of the femoral neck without trauma in elderly patients taking long-term BP treatment. We named it atypical femoral neck fracture (AFNF). To the best of our knowledge, this report is the first on follow-up results for AFNF in patients taking long-term BP.
2. Case 1
A 68-year-old female patient was admitted to our hospital with right hip pain starting 3 days prior with no history of a specific trauma. The patient had no history of specific medical history, but she had undergone bipolar hemiarthroplasty at our hospital because of a left femoral neck fracture four years prior. On the X-ray taken at the emergency room, a linear fracture of the lateral side of the right femoral neck with a Pauwel angle of approximately 63.6° was observed, and minimal sclerosis was observed around the fractured site as well (Fig. 1). The patient did not have high physical activity and had no history of repeated stress, with a pre-injury Harris hip score (HHS) of 94 points.
Figure 1.
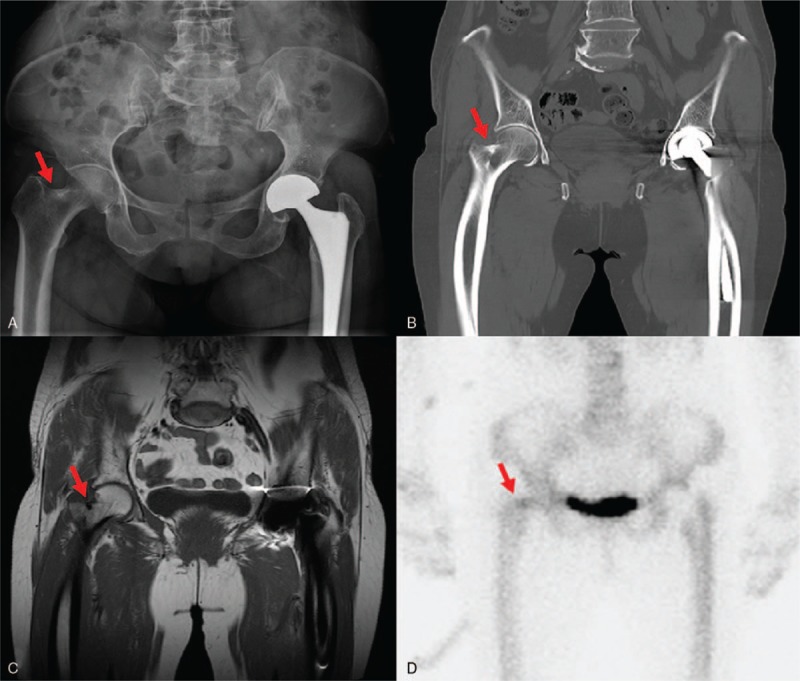
Preoperative images showing incomplete fracture of lateral cortex of femoral neck (red arrows). A, X-ray. B, CT scan (coronal view). C, T1-weighted MR image (coronal view). D, bone scan image showing small focal increased bone uptake at the fracture site.
In the BMD test performed 4 years prior, the T score of the spine was −3.2, indicating osteoporosis, and the T score of the right femur neck was −1.8. In addition, in the BMD test taken at this visit, the T score of spine was −2.9 and the T score of the right femur neck was −0.9. The 2 BMDs were all taken with GE Lunar iDXA (GE Healthcare, Waukesha, WI). The patient had been taking risendronate for 6 years with osteoporosis. In the lab, total calcium was found to be 9.1 mg/dL (normal 8.6∼10.2) and P (phosphorus) was 3.9 mg/dL (normal 2.5∼4.5) with normal full blood count.
Preoperative pelvic bone 3D CT and MRI showed the same incomplete linear fracture of the femoral neck as the X-ray findings, and we could confirm the hot uptake of the fracture site in bone scan.
The patient underwent internal fixation using 3 cannulated screws 6 days after the pain developed, and partial weight bearing rehabilitation was performed within 3 days after the operation. We could observe the distal extension of the fracture line without additional trauma on follow-up X-ray for 1 month after surgery. In the 3-month follow-up, the fracture line progressed to the lesser trochanteric area and the fracture length increased from 9.3 mm to 29.4 mm in the pelvis anteroposterior X-ray. In the follow-up image of 6 months, the distal fracture line was healed, but the proximal fracture gap did not change significantly (Fig. 2). In the meantime, the patient was able to walk with weight bearing with slight pain. At 3 months follow up, the HHS was 71 points.
Figure 2.
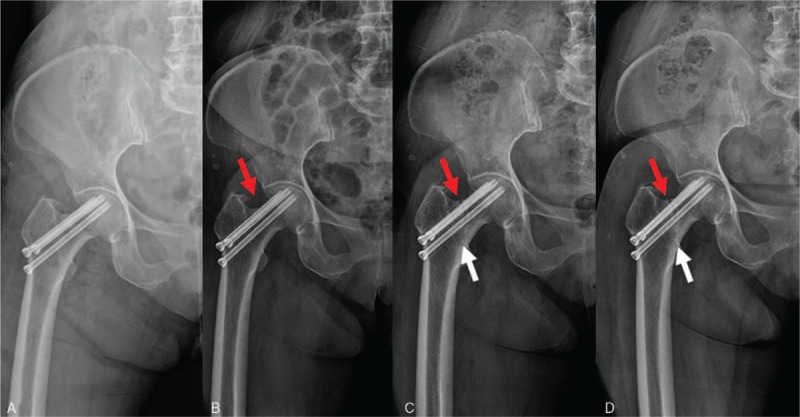
Postoperative X-rays. A, Immediate postoperative image. B, 1-month follow-up image showing distal extension of fracture line (red arrow). C, 3-month follow-up image showing progression of fracture line to the lesser trochanteric area (red and white arrow). D, 6-month follow-up image showing that the distal fracture line was healed (white arrow), but that the proximal fracture gap did not change significantly (red arrow).
3. Case 2
A 73-year-old female patient without limitations in activity (pre-injury HSS of 100 points) visited our hospital due to pain in the left hip starting from four days prior. The patient had a history of HTN and breast cancer that had been cured after mastectomy 6 years prior. She could barely walk after the hip pain had begun to occur, and simple radiographs showed a vertical fracture line visible incomplete fracture of Pauwel classification 3 (Pauwel angle 76.4°) on the lateral side of the femoral neck. And, the preoperative CT scan showed multiple cyst formation in both femoral neck areas and a linear fracture in the lateral cortex of the left femoral neck. On MR scan, we could also observe vertical fracture with bone marrow edema showing high signal intensity in T2-weighted image. In addition, focal hot uptake of the fracture site was confirmed by immediate postoperative SPECT-CT image (Fig. 3). She was an osteoporosis patient who had been taking risedronate and calcium for 6 years, and T score was −3.7 in spine and −1.8 in femoral neck in BMD performed on admission.
Figure 3.
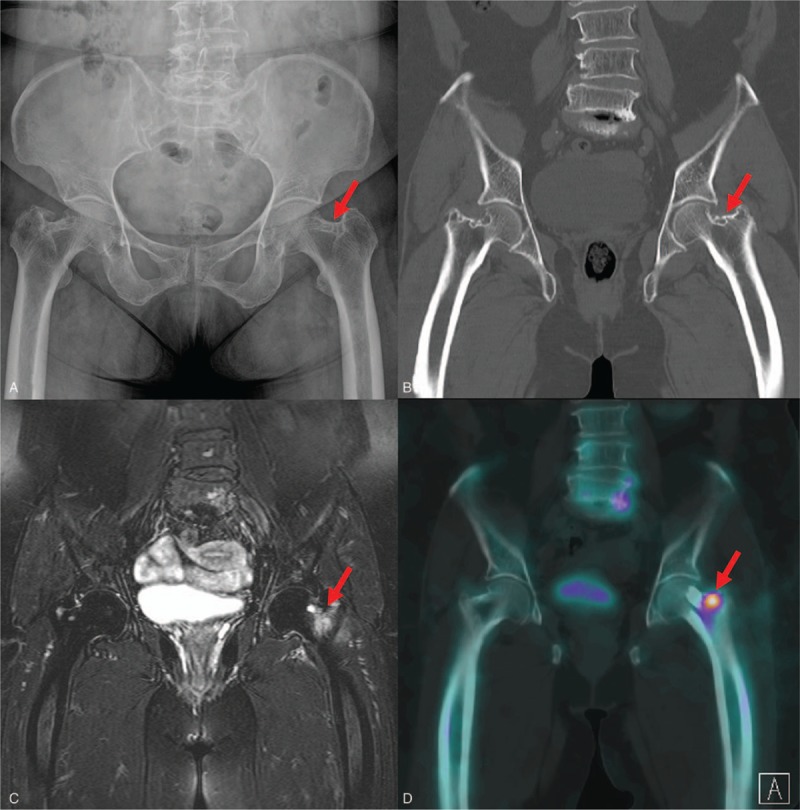
Preoperative images showing incomplete fracture of lateral cortex of femoral neck (red arrows). A, X-ray. B, CT scan (coronal view). C, T2-weighted MR image (coronal view). D, Postoperative SPECT-CT scan image (coronal view) showing focal hot uptake at the fracture site.
Internal fixation was performed using cannulated screws within 1 day after diagnosis of femoral neck fracture, and partial weight bearing rehabilitation was performed from the fifth postoperative day. In the follow-up X-ray taken 2 weeks postoperatively, we could observe the distal extension of the original fracture line. In addition, we observed extension of fracture line by 10 mm (8.5 mm to 18.4 mm) and widening of the fracture site at 3 months follow-up, and there was mild varus deformity with NS angle decreased to 129.1°, which was 132.7° postoperatively (Fig. 4). At 3 months follow up, the HHS was 58 points, and the patient still complained of pain at the fracture site.
Figure 4.
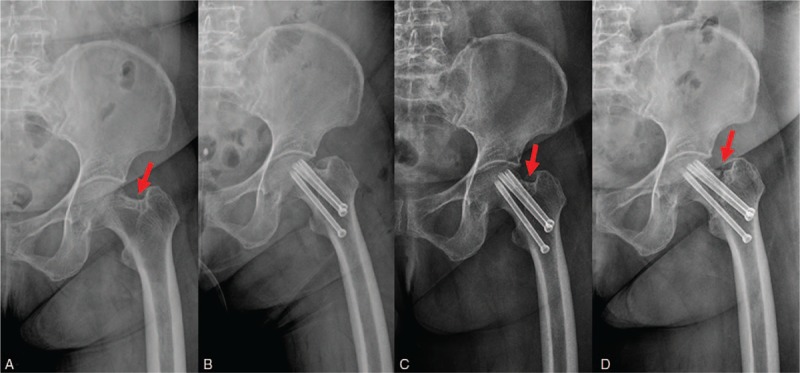
Serial X-rays of patient who underwent closed reduction and internal fixation (CRIF) for AFNF. A, Preoperative image showing linear fracture line of lateral femoral cortex (red arrow). B, Immediate postoperative image. C, 2-week follow-up image showing distal extension of fracture line (red arrow). D, 3-month follow-up image showing widening of fracture gap and mild Varus deformity (red arrow).
4. Discussion
BP can reduce the function of osteoclast and bone turnover and can eventually cause AFF complications by the accumulation of microdamages when used over a long period of time. Dell et al[8] reported that the incidence of AFF was only 1.78/100,000 person-y for patients older than 45 years of age who received BP therapy for 2 years or fewer, but 16.1/100,000 person-y for people who have received four to 6 years of continuous BP therapy, so the long-term use of BP is closely related to AFF.
The AFF diagnostic criteria for ASBMR revised in 2014 can diagnose AFF if four or more of the five major criteria are met. The major criteria are:
-
1.
Minimal or no trauma;
-
2.
transverse or oblique fracture line originating from lateral cortex;
-
3.
complete fracture with medial spike, incomplete fracture involving only lateral cortex;
-
4.
Non-comminuted or minimally; and
-
5.
periosteal thickening, previously a minor feature.
The accumulation of microdamages following BP treatment, such as alendronate, is mechanically different from cancellous and cortical sites.[9–11] The incidence of traditional osteoporotic fractures was reduced by the use of BP in the cancellous portion (e.g., femoral neck), which had mechanical strength with greater benefit from BP.[12] In addition, AFF is defined as an atypical fracture due to low energy trauma at the subtrochanteric and diaphysis sites, because long-term BP treatment has a more harmful effect on bone than in cancellous bone.[13]
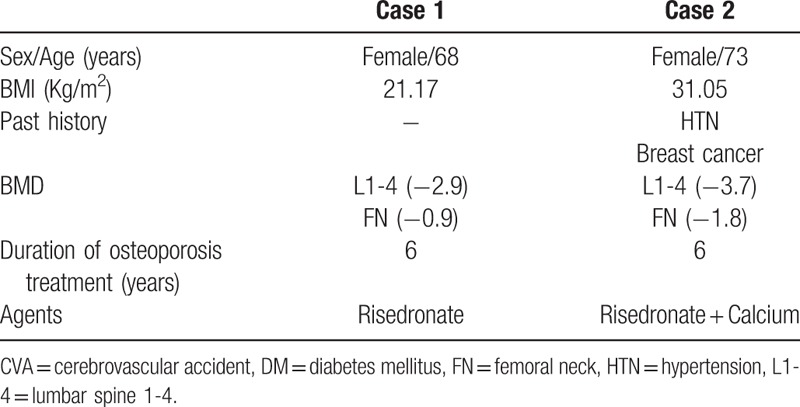
In the 2 cases we reported, all patients had been taking bisphosphonate for a long time and femoral neck fracture occurred without trauma (Table 1). The appearance of the fracture was linear in the lateral aspect of the femoral neck, and there was no history of repeated stresses and deformities such as coxa vara, so the possibility of a stress fracture could be excluded. In cases similar to these, Khan et al[14] reported 2 cases of femoral neck fracture without trauma history in a long-term use of BP. In that study, it was recommended that patients who have received long-term bisphosphonate should undergo radiographic imaging, even in the absence of trauma history in the event of thigh pain.
Table 1.
Characteristics of case patients.
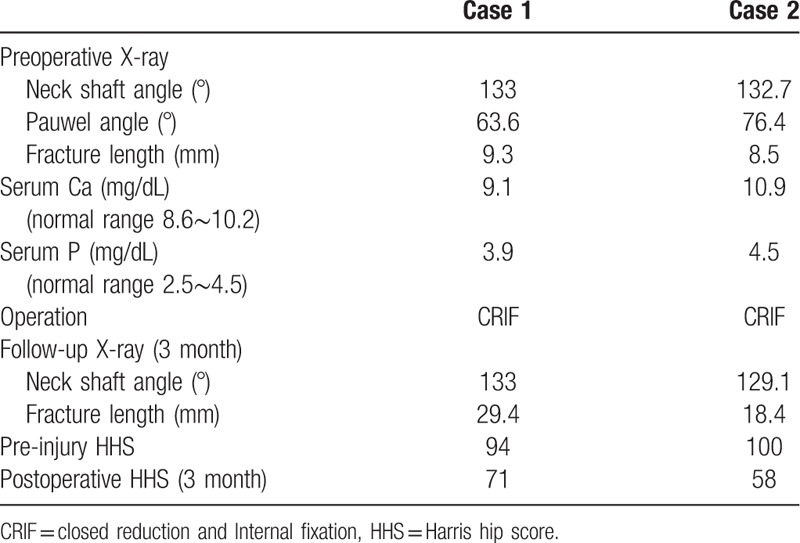
Screw fixation was performed in both patients. But the fracture line started to extend distally at four weeks and 2 weeks following surgery. In the 3-month follow-up image, the length of the fracture increased by 20.1 mm and 9.9 mm, respectively (Table 2). There was a problem with active rehabilitation, and the possibility of revision was also found to be a burden in terms of mortality and cost in older patients.
Table 2.
Preoperative image findings, blood tests, and treatment progress.
The clinical significance of AFF is that, in addition to non-specific fractures and insufficiency fractures that may occur with low-energy trauma, there is a high delayed union and nonunion rate in the bone healing process. There are also studies that have reported difficulties in obtaining bone healing with delayed union and nonunion rates of 50% and 46%, respectively, in the case of intramedullary nail fixation.[15,16] We present atypical incomplete fracture of femoral neck in patients who underwent long-term BP treatment through these 2 cases, and we report these cases with a review of the literature because we experienced difficulty in obtaining bone union due to decreased healing potential when treated with internal fixation.
5. Conclusion
We will define 2 cases with common features as AFNF:
-
1.
in patients with long-term BP treatment,
-
2.
without a history of repeated stress or trauma, and
-
3.
a linear incomplete fracture in the lateral cortex of the femoral neck.
In the case of general undisplaced femoral neck fractures, rigid internal fixation and early mobilization are standard treatments.[17] However, as in these cases, it is difficult to expect normal osteosynthesis, even if the fracture is an incomplete fracture of the femoral neck in patients with long-term use of BP, which inhibits bone healing. The possibility of revision surgery in the event of failure of osteosynthesis is a major burden on elderly patients. Therefore, in the case of AFNF in patients who have undergone long-term BP treatment, the guideline for treatment should be set in consideration of the decrease of bone healing, even if the fracture pattern is simple. Arthroplasty based on a wider indication may be worth considering as well.
To the best of our knowledge, these 2 cases are the first to report the follow-up results of AFNF. This presentation has limitations in that it has only a few cases and is not a long-term follow-up and thus requires more cases and long-term follow-up studies; identifying the direct association between the use of long-term BP and AFNF is a challenge for the future.
Author contributions
Resources: Won-Seok Lee.
Supervision: Sung-Hun Won.
Visualization: Jae-Hwi Nho.
Writing – original draft: Byung-Woong Jang.
Writing – review & editing: You-Sung Suh, Byung-Woong Jang.
Footnotes
Abbreviations: AFNF = atypical femoral neck fracture, BMD = bone mineral density, BP = bisphosphonate.
All patients have provided informed consent for publication of the cases.
Funding/support: This work was supported by the Soonchunhyang University Research Fund.
The authors have no conflicts of interest to disclose.
References
- [1].Reid IR. Short-term and long-term effects of osteoporosis therapies. Nat Rev Endocrinol 2015;11:418–28. [DOI] [PubMed] [Google Scholar]
- [2].Mashiba T, Hirano T, Turner CH, et al. Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res 2000;15:613–20. [DOI] [PubMed] [Google Scholar]
- [3].Allen MR, Burr DB. Human femoral neck has less cellular periosteum, and more mineralized periosteum, than femoral diaphyseal bone. Bone 2005;36:311–6. [DOI] [PubMed] [Google Scholar]
- [4].Donnelly E, Meredith DS, Nguyen JT, et al. Reduced cortical bone compositional heterogeneity with bisphosphonate treatment in postmenopausal women with intertrochanteric and subtrochanteric fractures. J Bone Miner Res 2012;27:672–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Odvina CV, Zerwekh JE, Rao DS, et al. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 2005;90:1294–301. [DOI] [PubMed] [Google Scholar]
- [6].Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2010;25:2267–94. [DOI] [PubMed] [Google Scholar]
- [7].Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1–23. [DOI] [PubMed] [Google Scholar]
- [8].Dell RM, Adams AL, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012;27:2544–50. [DOI] [PubMed] [Google Scholar]
- [9].Allen MR, Iwata K, Phipps R, et al. Alterations in canine vertebral bone turnover, microdamage accumulation, and biomechanical properties following 1-year treatment with clinical treatment doses of risedronate or alendronate. Bone 2006;39:872–9. [DOI] [PubMed] [Google Scholar]
- [10].Burr DB, Turner CH, Naick P, et al. Does microdamage accumulation affect the mechanical properties of bone? J Biomech 1998;31:337–45. [DOI] [PubMed] [Google Scholar]
- [11].Mashiba T, Turner CH, Hirano T, et al. Effects of suppressed bone turnover by bisphosphonates on microdamage accumulation and biomechanical properties in clinically relevant skeletal sites in beagles. Bone 2001;28:524–31. [DOI] [PubMed] [Google Scholar]
- [12].Maravic M, Ostertag A, Cohen-Solal M. Subtrochanteric/femoral shaft versus hip fractures: incidences and identification of risk factors. J Bone Miner Res 2012;27:130–7. [DOI] [PubMed] [Google Scholar]
- [13].Lenart BA, Neviaser AS, Lyman S, et al. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporos Int 2009;20:1353–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Khan SK, Savaridas T, Hemers JS, et al. Atraumatic intracapsular neck of femur fractures after prolonged bisphosphonate treatment: a new atypical variant? Clin Cases Miner Bone Metab 2016;13:38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sasaki S, Miyakoshi N, Hongo M, et al. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab 2012;30:561–7. [DOI] [PubMed] [Google Scholar]
- [16].Weil YA, Rivkin G, Safran O, et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma 2011;71:186–90. [DOI] [PubMed] [Google Scholar]
- [17].Chen WC, Yu SW, Tseng IC, et al. Treatment of undisplaced femoral neck fractures in the elderly. J Trauma 2005;58:1035–9. discussion 1039. [DOI] [PubMed] [Google Scholar]


