Abstract
Epidemiologic studies of pediatric bone and joint infection have been done mostly by developed Western countries, and such results could be expected to be biased. Therefore, an epidemiologic study to identify the distinct features of an Eastern country would be beneficial to improve their health outcomes and to reduce health care cost. A study was planned to investigate the epidemiology of pediatric osteomyelitis and septic arthritis in South Korea and to find out epidemiologic factors related with the occurrence of surgery.
We conducted a cross-sectional study among hospitalized pediatric patients (<18 years old) with osteomyelitis and septic arthritis using nationwide cohort based on the Health Insurance Review and Assessment Service (HIRA) from 2008 to 2016. Percentage of hospitalization was additionally calculated according to several epidemiologic factors including age, month, site of infection, and region of residence. Logistic regression analysis was performed to find out the association between epidemiologic factors and occurrence of surgery
Annual hospitalization rates (per 100,000) in our country were 7.8 to 9.1 for osteomyelitis, and 11.9 to 20.8 for septic arthritis. Frequent sites of osteomyelitis and septic arthritis were pelvis and lower extremity. The hospitalization rates of osteomyelitis and septic arthritis showed increasing trend with age. After multivariate logistic regression analysis, female gender, children, and adolescents rather than infants, rural area rather than urban area were associated with significantly increased odd ratios for surgery.
The hospitalization rate of septic arthritis (11.9 to 20.8 per 100,000) in South Korea was higher than the Western countries (1.1 to 11 per 100,000), and the hospitalization rate of osteomyelitis (peak at 12 years) and septic arthritis (peak at 17 years) showed increasing trend with age, which was different from those of the developed Western countries showing higher incidence in children aged under 5 years. After multivariate logistic regression analysis, our study identified female gender, higher age group including children, and adolescents, and rural residence as epidemiologic risk factors associated with surgery.
Keywords: epidemiology, South Korea, osteomyelitis, pediatric, septic arthritis
1. Introduction
Osteomyelitis and septic arthritis are 2 major forms of pediatric bone and joint infection primarily caused by bacterial infection. A study from French National Hospital Discharge Database showed that medical cost for pediatric bone and joint infection was €5,200 ($5,900) per hospital day (mean 8.4 hospital days)[1] and a study from US Nationwide Emergency Department Sample showed that mean charges per visit for admitted patients with septic arthritis was $55,354.[2]
Osteomyelitis and septic arthritis can be catastrophic causing various degree of disabilities.[3,4] Prompt diagnosis and appropriate treatment are mandatory to minimize complications including avascular necrosis, growth disturbance, pathologic fractures, deep vein thrombosis, and sepsis.[5,6] In an effort to reduce such complications, advances in imaging techniques including magnetic resonance imaging has enabled early diagnosis of osteomyelitis and septic arthritis.[7,8] Development of new antibiotics and vaccination,[9] along with advances in surgical techniques have improved the treatment outcome of the diseases.[10,11] In this respect, the epidemiology of bone and joint infection are expected to be evolutionary in nature.[12]
A few studies based on single center, population-based multicenter, or nationwide database have evaluated epidemiology of the osteomyelitis and septic arthritis in children. Such studies have evaluated the population of developed countries in North America or Europe,[13–17] and underdeveloped countries in Africa or Oceania.[18–20] The epidemiology including incidence and location of these 2 types of pediatric infections between developed countries and underdeveloped countries was significantly different.[18]
Despite such changing nature and regional difference in the epidemiology of bone and joint infection, epidemiologic studies of pediatric bone and joint infection have been done mostly by developed Western countries, and such results could be expected to be biased. In these circumstances, an epidemiologic study to identify the distinct features of an Eastern country would be beneficial to improve their health outcomes and to reduce health care cost. A study was planned to investigate the epidemiology of pediatric osteomyelitis and septic arthritis in South Korea and to find out epidemiologic factors related with the occurrence of surgery.
2. Methods
2.1. Database
South Korea has a public medical insurance system which covers almost all patients. National Health Insurance (NHI) covers approximately 97% of the population.[21] Health Insurance Review and Assessment Service (HIRA) databases is a government-operated organization that builds accurate review and quality assessment systems for claims for NHI. Claims data that healthcare service providers submit to HIRA for reimbursement for a service provided to patients are collected by HIRA. Because claims data for the remaining 3% of the population, who are covered by the National Medical Aid program, are also reviewed by HIRA, the HIRA database contains almost all inpatient and outpatient data from hospitals and community clinics in South Korea, respectively, making a nationwide population study feasible. In addition, the medical cost from diseases is reduced to at most 30% of total cost according to the economic status of the patients with help of this insurance system. As a result, the dependence on individual financial status in the accessibility of medical aid is greatly reduced. Such wide coverage and lower insurance rates make HIRA reliable for this epidemiologic study.
The data generated by HIRA are from the claims payments made during patient visits or admissions to medical institutions, and include patient demographics (gender, age, living area), and clinical data (diagnosis, procedures, and prescriptions). Access to HIRA data is regulated by the Rules for Data Exploration and Utilization of the HIRA, and we used data with the approval of the HIRA data access committee. All data were delivered anonymously, and no researchers had access to any potentially identifying personal information, including names, addresses, and date of birth.
This study was approved by the institutional review board (IRB) of the Kangdong Sacred Heart Hospital (IRB No. 2017-11-008-002).
2.2. Study population
We conducted a cross-sectional study among hospitalized pediatric patients (<18 years old) with osteomyelitis and septic arthritis using nationwide cohort based on the HIRA from January 2008 to December 2016. According to previous reports,[16,17] we selected any hospitalization with a principal or secondary diagnosis of osteomyelitis and septic (pyogenic) arthritis. International Classification of Disease 10 (ICD-10) codes included M00 (pyogenic arthritis), and M86 (osteomyelitis).
As with the previous reports,[16,17] the infection of spine was not included in the analysis because the incidence of spine infection is much lower than other site of bone and joint infect in pediatric patients,[22] and it could not be clearly classified into osteomyelitis or septic arthritis.[22] The affected sites of osteomyelitis and septic arthritis were identified using ICD-10 codes, and divided into shoulder (MXX.X1), upper arm (MXX.X2), forearm (MXX.X3), hand (MXX.X4), pelvic or thigh (MXX.X5), lower leg (MXX.X6), and ankle or foot (MXX.X7). The exact bone or joint of infection could not be identified using ICD-10 coding, and the affected sites were finally divided into the 2 groups; upper extremity and pelvis and lower extremity.
2.3. Investigation of epidemiologic factors
Despite controversy about the influence of physical activity on bone and joint infection,[23,24], physical activity is regarded as a reliable etiologic factor related with pediatric bone and joint infection. Individual physical activity of pediatric population is strongly affected by season, and we hypothesized that the hospitalization rates might have an association with season. Seasons at diagnosis were categorized as spring (March–May), summer (June–August), fall (September–November), and winter (January, February, and December).
Region of residence at diagnosis was categorized as urban and rural according to the previous study.[25] Among the 16 administrative districts where this survey was conducted, Seoul (the capital city of South Korea) and the surrounding metropolitan area (Gyeonggi), and 6 other metropolitan cities (Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan) of South Korea were grouped as urban areas. The remainder of the regions (Gangwon, Chungbuk, Chungnam, Jeonbuk, Jeonnam, Gyeongbuk, Gyeongnam, and Jeju) were grouped as rural areas.
2.4. Statistical analysis
The number of hospitalized pediatric patients with osteomyelitis and septic arthritis were counted for each year during the study period (2008–2016). Estimated year-specific, and gender-specific populations in South Korea were obtained from the “Statistics Korea” website (http://www.kosis.kr).
Then, annual gender-specific hospitalization rates for osteomyelitis and septic arthritis were calculated from the population of each gender group in South Korea for a given study year (per 100,000 persons) (Fig. 1). Percentage of hospitalization according to the age was calculated by dividing the number of age-specific pediatric patients by the total number of pediatric patients during the study period (Fig. 2). Percentage of hospitalization by month was calculated by dividing the monthly number of patients by the total number of pediatric patients during the study period (Fig. 3). The ratio for hospitalization rates according to the region (rural/urban) during the study period was calculated as the ratio of the number of hospitalization due to osteomyelitis or septic arthritis divided by the mean number of population in each rural and urban area during the study period. Proportions of infection site was shown according to the age group (Fig. 4), categorized as infant (≤ 1 year), children (between 2 and 11 years), and adolescent (between 12 and 18 years). A linear-by-linear association test or chi square test was performed to assess the trend in epidemiologic data. Logistic regression analysis was performed to find out the association between epidemiologic factors and occurrence of surgery, and all variables in the univariate analysis were included in a multivariate logistic regression analysis. All analyses were performed with SAS Enterprise Guide (SAS Institute, Inc., Cary, NC). All statistical tests were 2-sided, and a P-value<.05 was considered statistically significant.
Figure 1.
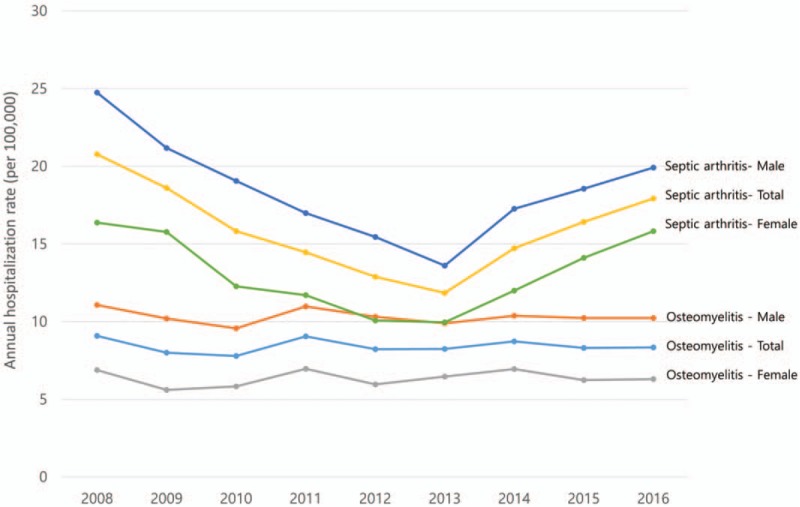
The annual hospitalization rates because of osteomyelitis and septic arthritis.
Figure 2.
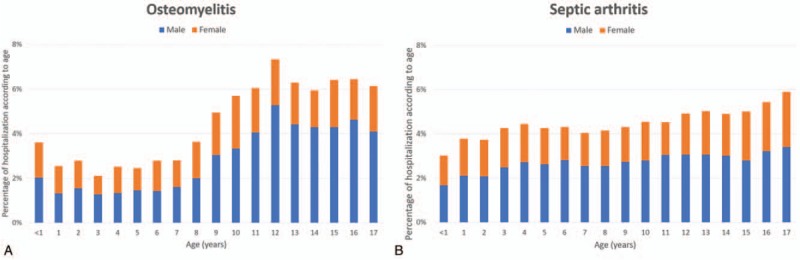
Percentage of hospitalization according to age during study period (2008–2016).
Figure 3.
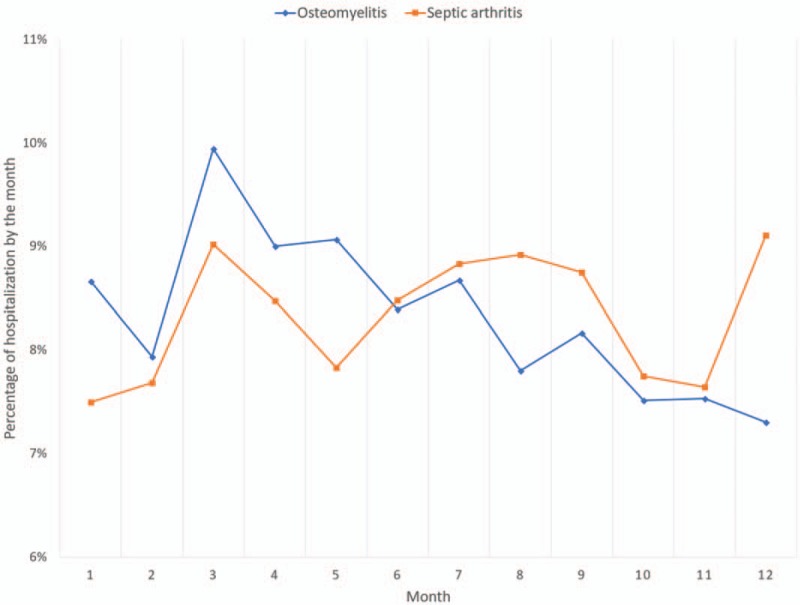
Percentage of hospitalization by the month during study period (2008–2016).
Figure 4.
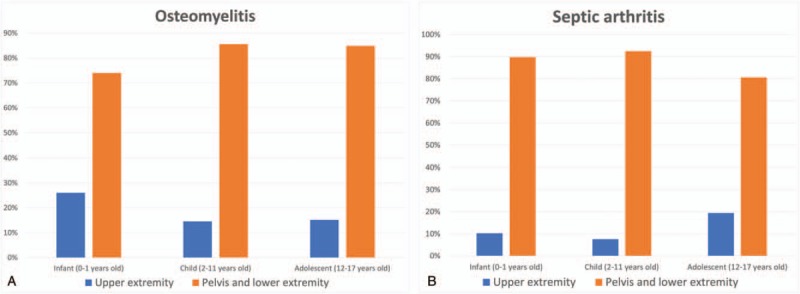
Proportions of infection site according to age groups during study period (2008–2016).
3. Results
A total of 21,522 pediatric patients fulfilled the criteria during the study period. 7422 patients were diagnosed as osteomyelitis and 14,100 patients were diagnosed as septic arthritis.
3.1. Annual hospitalization rates because of osteomyelitis and septic arthritis
Annual hospitalization rates (per 100,000) during the study period were 7.8 to 9.1 for osteomyelitis, and 11.9 to 20.8 for septic arthritis. Annual hospitalization rates due to osteomyelitis did not show any increasing or decreasing trend (Fig. 1). Although annual hospitalization rates for septic arthritis showed a decreasing trend between 2008 and 2013, the rate increased between 2014 and 2016 (Fig. 1). Male-to-female hospitalization rate during the study period was 1.8 for osteomyelitis, and 1.5 for septic arthritis. Annual hospitalization rate did not show any increasing or decreasing trends (P = .624 for osteomyelitis and P = .686 for septic arthritis).
3.2. Percentage of hospitalization according to age during the study period (2008–2016)
Percentage of hospitalization showed increasing trend with aging for both osteomyelitis and septic arthritis (Fig. 2). In osteomyelitis, there were 2 peaks of hospitalization percentage in age below 1 years and 12 years (Fig. 2A). Percentage of hospitalization showed increasing trends with age (P < .001 for osteomyelitis and P < .001 for septic arthritis). There were also significant increasing trends in male to female ratios with age (P < .001 for osteomyelitis and P < .001 for septic arthritis).
3.3. Percentage of hospitalization by month during the study period (2008–2016)
Percentage of hospitalization was higher in spring including March, April, and May for osteomyelitis (Fig. 3), and the percentage decreased thereafter. In septic arthritis, there were 3 peaks in percentage of hospitalization in March, August, and December, and the percentage of hospitalization was lowest in January (Fig. 3). Percentage of hospitalization by month did not show trend (P = .642 for osteomyelitis and P = .916 for septic arthritis).
3.4. Comparison of the regional hospitalization rate during the study period (2008–2016)
The ratio for regional hospitalization rate (rural: urban) was 0.9:1 for osteomyelitis and 1.2:1 for septic arthritis. Hospitalization rate was higher in urban area for osteomyelitis and higher in rural area for septic arthritis.
3.5. Proportions of infection sites according to age groups during the study period (2008–2016)
Both osteomyelitis and septic arthritis were more common in pelvis and lower extremity rather than upper extremity in all aged groups (Fig. 4).
3.6. Annual rate of surgery due to osteomyelitis and septic arthritis during the study period (2008–2016)
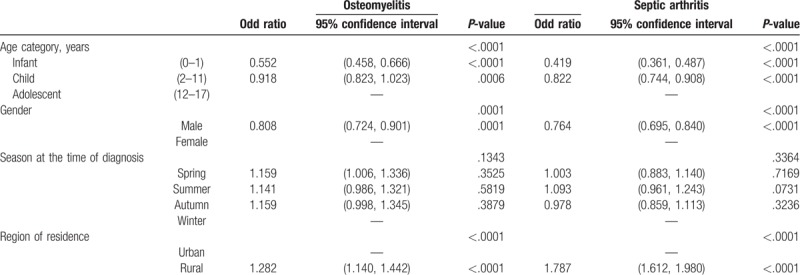
Around 2023 (27.5%) of 7348 (incomplete data in 74 cases) patients with osteomyelitis received at least one surgery during the period, and 2291 (16.4%) of 13972 (incomplete data in 128 cases) patients with septic arthritis received at least one surgery during the study period. Annual rate of surgery (per 100,000) during the study period were 1.3 to 1.8 for osteomyelitis, and 1.8 to 2.4 for septic arthritis. Annual rate of surgery due to osteomyelitis and septic arthritis did not show any increasing or decreasing trend. Logistic regression analysis was performed to identify the associations between age categories, gender, season at time of diagnosis, geographic region and surgery (Tables 1 and 2). After multivariate logistic regression analysis, younger age group including infants and children showed significantly lower odd ratios for receiving surgery than adolescent group in both osteomyelitis and septic arthritis (0.552 for infant and 0.918 for child in osteomyelitis, and 0.419 for infant and 0.822 for child in septic arthritis) (Table 2). Male gender was also associated with lower risk for surgery in both osteomyelitis and septic arthritis (0.808 in osteomyelitis, and 0.764 in septic arthritis) (Table 2). In addition, rural patient had significantly higher odd ratios for receiving surgery than urban patients (1.282 in osteomyelitis, 1.787 in septic arthritis) (Table 2). There was no association between season at diagnosis and risk of surgery (Table 2).
Table 1.
Univariate logistic regression for the association between age categories, gender, season at the time of diagnosis, region of residence and surgery.
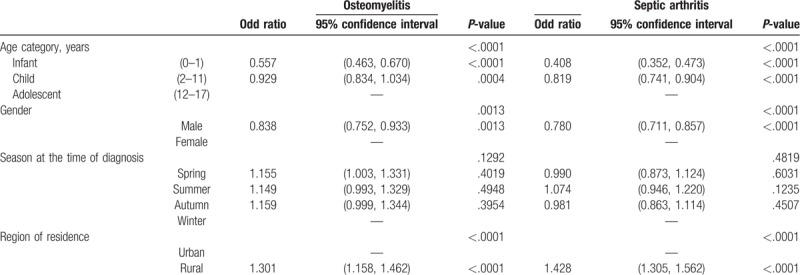
Table 2.
Multivariate logistic regression for the association between age categories, gender, season at the time of diagnosis, region of residence and surgery.
4. Discussion
From this nationwide epidemiological study from South Korea, annual hospitalization rates (per 100,000) in our country were 7.8 to 9.1 for osteomyelitis, and 11.9 to 20.8 for septic arthritis. The hospitalization rates for osteomyelitis were similar with those of developed countries including USA and European countries (Table 3). However, the hospitalization rates for septic arthritis were even higher than those countries (Table 3). In addition, the hospitalization rates of osteomyelitis and septic arthritis showed increasing trend with age (P < .001 for osteomyelitis and P < .001 for septic arthritis, Fig. 2), which was different from those patterns of the developed Western countries, which show high incidence in children aged under 5 years.[26] The frequent sites of infection for osteomyelitis and septic arthritis were similar with those of the developed countries.[16,17]
Table 3.
Incidence of ostemyelitis and septic arthritis according to the previous studies.
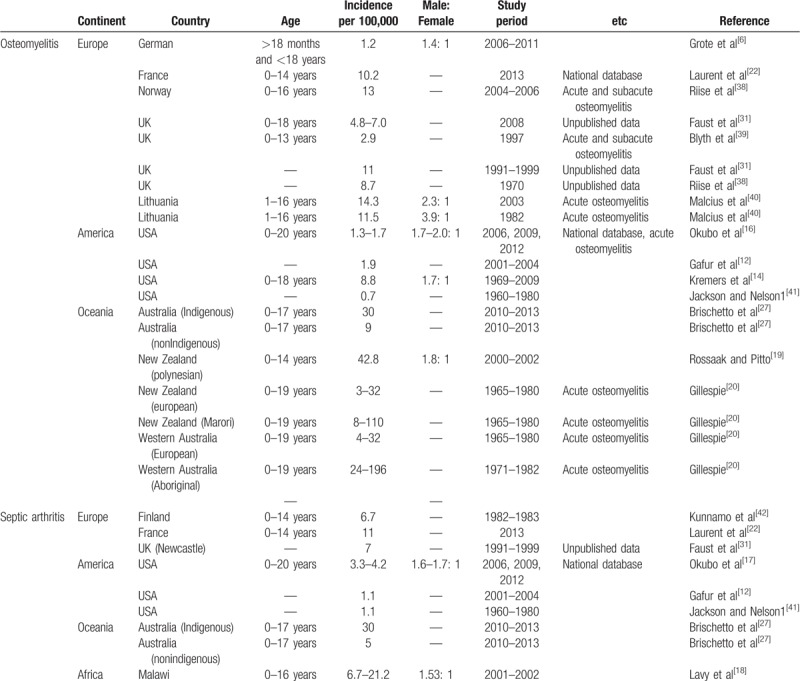
According to the previous reports, incidence of osteomyelitis ranges from 0.7 to 196 per 100,000 children, with septic arthritis from 1.1 to 21.2 (Table 3). Lower socioeconomic status such as over-crowding, poor hygiene, and sanitation have been proposed as causes of the increased infection rates,[27] and the incidence was reported to be high in developing countries (Table 3). However, these previous studies have greater risk of bias as an epidemiologic study. In addition to bias from their small sample size, specific data based on major hospitals or limited geographical areas could be strongly biased by patients’ socioeconomic status and regional difference in medical resources.
Recently, 3 nationwide surveys in 2 Western countries including United States and France have investigated the epidemiology of osteomyelitis and septic arthritis in children.[16,17,22] They reported that annual hospitalization rates ranged from 1.3 to 1.7/100,000 children for acute osteomyelitis, 10.2 for overall osteomyelitis, and 3.3 to 11 for septic arthritis. These results were grossly in line with the previous results (Table 3). In their studies, they also confirmed male predominance of infection, and that the proportions of hospitalizations were high among children living in lower income areas, and that large bone joints at the lower limbs were the most frequently affected sites of infection. As a fourth epidemiologic study using national database based on ICD codes, the methodology of our study is thought to be reliable.
The most interesting finding of our study is the increased hospitalization rate for septic arthritis in South Korea, which was even higher than those of the developed Western countries and similar to underdeveloped areas of Oceania and Africa (Table 3). On the other hand, most common site of septic arthritis in our country was pelvis and lower extremities, which is similar to the result of Western countries and different from the result of undeveloped areas such as Malawi, which showed shoulder was one of the frequent site for septic arthritis.[18]
Although identifying the cause of the increased hospitalization rate for septic arthritics is beyond the scope of our study, such conflicting result might be explained by the association with trauma. It is definite that major trauma including penetrating trauma or open fracture can lead to osteomyelitis.[28] As one of the most rapidly developed country, the incidence of major trauma such as life-threatening traffic accident was greatly decreased in South Korea,[29] which we might regard as a major cause of the similar hospitalization rates for osteomyelitis in South Korea compared with the developed countries. However, the increasing trend with age in the hospitalization rate of osteomyelitis and septic arthritis is also different from the pattern of developed Western countries, which show high incidence in children aged under 5 years.[26] We guess that such trend could have resulted from remarkably decreasing birth rate becoming a social problem in our country.[30] Such a low birth rate caused cultural overprotection of infants and children, which significantly reduced their physical activity. In other words, the increased hospitalization rates in adolescent group compared to the other lower age groups might be explained by relatively reduced physical activity and resultant decrease in trauma within the lower age groups. Interestingly, the hospitalization rate for septic arthritis was lowest in 2013, which might also correspond to the lowest occurrence for national road traffic accident of children in 2013 between 2010 and 2015 (http://taas.koroad.or.kr).
This is the first study to explore the epidemiologic factors related with surgery for osteomyelitis and septic arthritis. Historically, early biopsy and surgery including debridement were recommended for osteomyelitis and septic arthritis despite little evidences.[31–33] However, there is an increasing trend toward the success of medical treatment.[31–33] According to the previous studies, the reported probability for surgical treatment is 17% to 34% for osteomyelitis,[13,34,35] and 12% to 53% for septic arthritis.[13,33,36] Our data from the nationwide database are also within these ranges (27.5% for osteomyelitis, 16.4% for septic arthritis). Compared with adolescents, infants and children had lower odd ratios for receiving surgery in both osteomyelitis and septic arthritis (Table 2). Although the ratio for regional hospitalization rate was similar between rural and urban areas (0.9:1 for osteomyelitis and 1.2:1 for septic arthritis), patients in rural area had significantly increased odd ratios for receiving surgery than those in urban area (1.282 for osteomyelitis, 1.787 for septic arthritis) (Table 2). There was no association between season at time of diagnosis and risk of surgery (Tables 1 and 2). Intriguingly, despite definite male predominance of osteomyelitis and septic arthritis (Table 3), male children showed significantly lower odd ratios for surgery (0.808 for osteomyelitis, 0.764 for septic arthritis) (Table 2). Inferring the cause of increased risk for surgery in female children is beyond the scope of our study. We can only guess that bone and joint infection in female children might have higher probability of non-traumatic origin including hematogenous spread from bacteremia or spread from local infection,[37] and diagnosis might be delayed.
From the results of our study, health professionals engaging for the treatment of pediatric bone and joint infection should be aware the different hospitalization rates and age trends according to the countries, which have been uniformly known from the data of developed Western countries. In addition, the risks for receiving surgery were significantly higher in pediatric patients in rural area who were socially vulnerable groups and in female patients who have been known to have lower incidence rates than male patients. Therefore, policy makers and health professionals should pay more attention to such groups of patients.
The main limitation of our study results from the miscoding of disease by ICD in hospital records. The studies using nationwide database based on ICD coding could not be free from miscoding. However, all ICD coding in hospitalized patients are strictly reviewed by HIRA in our country due to government subsidy of at least 70% of the total hospital cost. Second, due to limited information resulting from equivocal ICD coding, we could not exactly identify the exact locations of infected bone or joint. Third, detailed patients’ information, such as socioeconomic status, history of trauma, presence of previous surgery, symptoms, laboratory data including microorganism and complication was not available in the nationwide database, and such independent variables were not included in analysis. Fourth, hospitalization rates among the different countries cannot be theoretically compared as an actual incidence rate because of the difference in health insurance system, parental labour environments, and doctor's attitude to hospitalize diseased children. Therefore, the result of our study should be clinically applied with caution. Finally, the methodological bias resulting from the missing data should not be underestimated in the analysis of big data.
5. Conclusion
The hospitalization rate of septic arthritis (11.9–20.8 per 100,000) in South Korea was higher than the Western countries (1.1–11 per 100,000), and the hospitalization rate of osteomyelitis (peak at 12 years) and septic arthritis (peak at 17 years) showed increasing trend with age, which was different from those of the developed Western countries showing higher incidence in children aged under 5 years. After multivariate logistic regression analysis, our study identified female gender, higher age group including children and adolescents, and rural residence as epidemiologic risk factors associated with surgery.
Acknowledgments
We would like to acknowledge Dr Kim, Dr. Oh, Dr. Park, and Dr Jang for their review of the manuscript.
Author contributions
Conceptualization: Jihye Kim, Tae-Hwan Kim.
Data curation: Jihye Kim, Min Uk Lee, Tae-Hwan Kim.
Formal analysis: Jihye Kim, Tae-Hwan Kim.
Investigation: Jihye Kim, Tae-Hwan Kim.
Methodology: Jihye Kim, Min Uk Lee, Tae-Hwan Kim.
Project administration: Tae-Hwan Kim.
Resources: Min Uk Lee, Tae-Hwan Kim.
Software: Jihye Kim, Min Uk Lee, Tae-Hwan Kim.
Supervision: Tae-Hwan Kim.
Validation: Jihye Kim, Tae-Hwan Kim.
Visualization: Tae-Hwan Kim.
Writing – original draft: Jihye Kim, Tae-Hwan Kim.
Writing – review & editing: Jihye Kim, Tae-Hwan Kim.
Footnotes
Abbreviations: HIRA = Health Insurance Review and Assessment Service, ICD = International Classification of Disease, NHI = National Health Insurance.
The authors have no financial relationships relevant to this article to disclose
The authors have no funding and no conflicts of interest to disclose.
References
- [1].Grammatico Guillon L, Maakaroun Vermesse Z, Baron S, et al. Paediatric bone and joint infections are more common in boys and toddlers: a national epidemiology study. Acta Paediatr 2013;102:e120–5. [DOI] [PubMed] [Google Scholar]
- [2].Singh JA, Yu S. The burden of septic arthritis on the U.S. inpatient care: a national study. PLoS One 2017;12:e0182577–1182577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Chiappini E, Krzysztofiak A, Bozzola E, et al. Risk factors associated with complications/sequelae of acute and subacute haematogenous osteomyelitis: an Italian multicenter study. Expert Rev Anti Infect Ther 2018;16:351–8. [DOI] [PubMed] [Google Scholar]
- [4].Johari AN, Hampannavar A, Johari RA, et al. Coxa vara in postseptic arthritis of the hip in children. J Pediatr Orthop B 2017;26:313–9. [DOI] [PubMed] [Google Scholar]
- [5].Funk SS, Copley LA. Acute hematogenous osteomyelitis in children: pathogenesis, diagnosis, and treatment. Orthop Clin North Am 2017;48:199–208. [DOI] [PubMed] [Google Scholar]
- [6].Grote V, Silier CC, Voit AM, et al. Bacterial osteomyelitis or nonbacterial osteitis in children: a study involving the German surveillance unit for rare diseases in childhood. Pediatr Infect Dis J 2017;36:451–6. [DOI] [PubMed] [Google Scholar]
- [7].Strobel K, Stumpe KDM. PET/CT in musculoskeletal infection. Semin Musculoskelet Radiol 2007;11:353–64. [DOI] [PubMed] [Google Scholar]
- [8].Karchevsky M, Schweitzer ME, Morrison WB, et al. MRI findings of septic arthritis and associated osteomyelitis in adults. AJR Am J Roentgenol 2004;182:119–22. [DOI] [PubMed] [Google Scholar]
- [9].Olarte L, Romero J, Barson W, et al. Osteoarticular infections caused by Streptococcus pneumoniae in children in the post-pneumococcal conjugate vaccine era. Pediatr Infect Dis J 2017;36:1201–4. [DOI] [PubMed] [Google Scholar]
- [10].Pääkkönen M, Kallio MJ, Kallio PE, et al. Shortened hospital stay for childhood bone and joint infections: analysis of 265 prospectively collected culture-positive cases in 1983–2005. Scand J Infect Dis 2012;44:683–8. [DOI] [PubMed] [Google Scholar]
- [11].Canavese F, Corradin M, Khan A, et al. Successful treatment of chronic osteomyelitis in children with debridement, antibiotic-laden cement spacer and bone graft substitute. Eur J Orthop Surg Traumatol 2017;27:221–8. [DOI] [PubMed] [Google Scholar]
- [12].Gafur OA, Copley LA, Hollmig ST, et al. The impact of the current epidemiology of pediatric musculoskeletal infection on evaluation and treatment guidelines. J Pediatr Orthop 2008;28:777–85. [DOI] [PubMed] [Google Scholar]
- [13].Calvo C, Nunez E, Camacho M, et al. Epidemiology and management of acute, uncomplicated septic arthritis and osteomyelitis: Spanish Multicenter Study. Pediatr Infect Dis J 2016;35:1288–93. [DOI] [PubMed] [Google Scholar]
- [14].Kremers HM, Nwojo ME, Ransom JE, et al. Trends in the epidemiology of osteomyelitis: a population-based study, 1969 to 2009. J Bone Joint Surg Am 2015;97:837–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dahl LB, Hoyland AL, Dramsdahl H, et al. Acute osteomyelitis in children: a population-based retrospective study 1965 to 1994. Scand J Infect Dis 1998;30:573–7. [DOI] [PubMed] [Google Scholar]
- [16].Okubo Y, Nochioka K, Testa M. Nationwide survey of pediatric acute osteomyelitis in the USA. J Pediatr Orthop B 2017;26:501–6. [DOI] [PubMed] [Google Scholar]
- [17].Okubo Y, Nochioka K, Marcia T. Nationwide survey of pediatric septic arthritis in the United States. J Orthop 2017;14:342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lavy CB, Thyoka M, Pitani AD. Clinical features and microbiology in 204 cases of septic arthritis in Malawian children. J Bone Joint Surg Br 2005;87:1545–8. [DOI] [PubMed] [Google Scholar]
- [19].Rossaak M, Pitto RP. Osteomyelitis in Polynesian children. Int Orthop 2005;29:55–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gillespie WJ. The epidemiology of acute haematogenous osteomyelitis of childhood. Int J Epidemiol 1985;14:600–6. [DOI] [PubMed] [Google Scholar]
- [21].Kim L, Kim J-A, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health 2014;36:e2014008–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Laurent E, Petit L, Maakaroun-Vermesse Z, et al. National epidemiological study reveals longer paediatric bone and joint infection stays for infants and in general hospitals. Acta Paediatr 2018;107:1270–5. [DOI] [PubMed] [Google Scholar]
- [23].Pääkkönen M, Kallio MJ, Lankinen P, et al. Preceding trauma in childhood hematogenous bone and joint infections. J Pediatr Orthop B 2014;23:196–9. [DOI] [PubMed] [Google Scholar]
- [24].Whalen JL, Fitzgerald RH, Jr, Morrissy RT. A histological study of acute hematogenous osteomyelitis following physeal injuries in rabbits. J Bone Joint Surg Am 1988;70:1383–92. [PubMed] [Google Scholar]
- [25].Choi HS, Oh HJ, Choi H, et al. Vitamin D insufficiency in Korea—a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 2011;96:643–51. [DOI] [PubMed] [Google Scholar]
- [26].Castellazzi L, Mantero M, Esposito S. Update on the management of pediatric acute osteomyelitis and septic arthritis. Int J Mol Sci 2016;17:E855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Brischetto A, Leung G, Marshall CS, et al. A retrospective case-series of children with bone and joint infection from Northern Australia. Medicine 2016;95:e2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tribble DR, Lewandowski LR, Potter BK, et al. Osteomyelitis risk factors related to combat trauma open tibia fractures: a case-control analysis. J Orthop Trauma 2018;32:e344–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lim D, Ha M, Song I. Trends in the leading causes of death in Korea 1983–2012. J Korean Med Sci 2014;29:1597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bae C-W. The changes in the birth and mortality rates of newborn in Korea. J Korean Med Assoc 2006;49:975–82. [Google Scholar]
- [31].Faust SN, Clark J, Pallett A, et al. Managing bone and joint infection in children. Arch Dis Child 2012;97:545–53. [DOI] [PubMed] [Google Scholar]
- [32].Dartnell J, Ramachandran M, Katchburian M. Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br 2012;94:584–95. [DOI] [PubMed] [Google Scholar]
- [33].Dodwell ER. Osteomyelitis and septic arthritis in children: current concepts. Curr Opin Pediatr 2013;25:58–63. [DOI] [PubMed] [Google Scholar]
- [34].Cohen E, Lifshitz K, Fruchtman Y, et al. Current data on acute haematogenous osteomyelitis in children in Southern Israel: epidemiology, microbiology, clinics and therapeutic consequences. Int Orthop 2016;40:1987–94. [DOI] [PubMed] [Google Scholar]
- [35].Chiappini E, Camposampiero C, Lazzeri S, et al. Epidemiology and management of acute haematogenous osteomyelitis in a tertiary paediatric center. Int J Environ Res Public Health 2017;14:E477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Paakkonen M, Kallio MJ, Peltola H, et al. Pediatric septic hip with or without arthrotomy: retrospective analysis of 62 consecutive nonneonatal culture-positive cases. J Pediatr Orthop B 2010;19:264–9. [DOI] [PubMed] [Google Scholar]
- [37].Whyte NS, Bielski RJ. Acute hematogenous osteomyelitis in children. Pediatr Ann 2016;45:e204–8. [DOI] [PubMed] [Google Scholar]
- [38].Riise OR, Kirkhus E, Handeland KS, et al. Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Blyth MJ, Kincaid R, Craigen MA, et al. The changing epidemiology of acute and subacute haematogenous osteomyelitis in children. J Bone Joint Surg Br 2001;83:99–102. [DOI] [PubMed] [Google Scholar]
- [40].Malcius D, Trumpulyte G, Barauskas V, et al. Two decades of acute hematogenous osteomyelitis in children: are there any changes? Pediatr Surg Int 2005;21:356–9. [DOI] [PubMed] [Google Scholar]
- [41].Jackson MA, Nelson JD. Etiology and medical management of acute suppurative bone and joint infections in pediatric patients. J Pediatr Orthop 1982;2:313–23. [PubMed] [Google Scholar]
- [42].Kunnamo I, Kallio P, Pelkonen P. Incidence of arthritis in urban Finnish children. A prospective study. Arthritis Rheum 1986;29:1232–8. [DOI] [PubMed] [Google Scholar]


