Abstract
Undiagnosed type 2 diabetes mellitus constitutes a significant threat to the health of commercial taxi drivers, safety of the passengers and other road users. This study determines the prevalence of pre-diabetes and type 2 diabetes mellitus among commercial taxi drivers in Buffalo City Metropolitan Municipality (BCMM), Eastern Cape and examines the factors associated with type 2 diabetes mellitus.
A cross-sectional survey of 403 commercial taxi drivers was undertaken using the World Health Organization (WHO) STEPwise approach. Anthropometric, blood pressure, and blood glucose measurements followed standard procedure. Diabetes status was determined using the fasting blood glucose (FBG) test. Diabetes was defined as a FBG ≥7.0mmol/L or self-reported history of diabetes or current diabetes medication use (treatment), while pre-diabetes was defined as a FBG of 5.6 to 6.9 mmol/L. Awareness of diabetes was defined as a self-reported history of diabetes.
The mean age of the study participants was 43.3 ± 12.5years. Prevalence of pre-diabetes and diabetes were 17% (95% CI: 13.4–20.6) and 16% (95% CI: 12.4–19.6), respectively. Of those who had diabetes (n = 63), the majority were aware of their diabetes status (n = 43) and were on treatment (n = 30). In the unadjusted logistic regression, age, ever married, hypertension, obesity, and driving for more than 5 years were independently associated with diabetes. However, only age >35 (adjusted odds ratio [AOR]= 3.65, CI: 1.17–11.32), ever married (AOR= 3.26, CI: 1.52–6.99) and hypertension (AOR= 3.23, CI: 1.56–6.69) were associated with diabetes in the adjusted logistic regression model.
The prevalence of diabetes among commercial taxi drivers in this study is high, almost twice the national prevalence of diabetes in South Africa. Periodic health screening among this sub-population group is important to bridge the gap of undiagnosed diabetes in South Africa.
Keywords: commercial taxi drivers, hypertension, pre-diabetes, South Africa, type 2 diabetes mellitus
1. Introduction
Diabetes mellitus is a significant public health challenge. Although previously considered as a disease of rich nations, diabetes mellitus is now growing rapidly in developing nations.[1] South Africa is one of the countries with the highest prevalence of diabetes in sub-Saharan African.[2] It was estimated that about 2.28 million (8.3%) of the population were living with diabetes in the country in 2015.[3] Diabetes is the second leading cause of morbidity and mortality in South Africa.[4]
Diabetes constitutes a significant threat to the health of commercial taxi drivers, the transport industry and the public safety.[5] The threats posed by diabetes is worse among drivers who are being treated with insulin and at the risk of developing hypoglycaemic episodes.[6] Diabetes is also associated with psychological disturbance with a resultant functional impairment,[6] which might affect drivers’ performance at work and increase the risks of road traffic accidents.[7] In the light of the highlighted risks, several countries require medical fitness for issuance of drivers’ licenses to individuals living with diabetes who may want to venture into driving commercial taxi.[8–10] However, there are currently no measures in place in South Africa, partly because the health status of the commercial taxi drivers is often neglected. This is evidenced by a dearth of information on the prevalence, awareness, treatment, and determinants of diabetes and pre-diabetes among commercial taxi drivers in South Africa.
Anecdotally, the nature of the work of commercial taxi drivers affords them little opportunity to seek healthcare. Yet, commercial drivers indulge in unhealthy lifestyle behaviors such as physical inactivity, smoking, excessive alcohol consumption, and poor diet,[11] which are deleterious to health. These behaviors specifically increase risk of developing cardiometabolic diseases.[12,13] Considering the important role commercial taxi drivers play in the transport industry of any given nation, their health status should be critically assessed for better health and public safety. The aims of our study were:
-
(i)
to determine the prevalence of pre-diabetes and type-2 diabetes mellitus among commercial taxi drivers in Buffalo City Metropolitan Municipality (BCMM), East London, and
-
(ii)
to examine the factors associated with type 2 diabetes mellitus.
2. Method
2.1. Study area and design
This was a cross-sectional study involving 403 commercial taxi drivers selected across different taxi ranks in BCMM, Eastern Cape Province, South Africa. BCMM is one of the 8 districts in the Eastern Cape Province. It is made up of some towns in the Eastern Cape which include East London, Bisho, King Williams Town, and Mdanstane and it is largely populated (85.2%) by Black South Africans. The transport industry makes up 12% of its economic sector.[14]
2.2. Participants and sample size
According to the statistics retrieved from Eastern Cape Department of Transport, the numbers of commercial vehicles registered in East London are 3559. Those operating under East London district Taxi Association are 315 and those under the East London Taxi Association are 765. While the numbers of vehicle registered for Mdanstane includes, 1514 under the Mdantsane East London Districts Taxi Association, 288 under the Mdantsane East London Taxi association and 677 under the Mdantsane UNCEDO service Taxi Association. These make up the 3559 vehicles drivers in East London and Mdantsane. The sample size for this study was based on the estimated number of commercial taxi drivers in the district. The appropriate sample size was determined using the Creative Research Systems sample size calculator [15] at a confidence level of 95%, confidence interval (CI) of ±4.6, and population of 3559. The required sample size was 403 participants. To recruit participants, all the 10 taxi ranks serving the BCMM were included in the study. All commercial taxi drivers available at the taxi rank on the days of the study were offered the fasting blood glucose (FBG) test. The recruitment of study participants took place on average of 4 days in each taxi rank. Only commercial taxi drivers who were available, willing and met the inclusion criteria were recruited into the study. This study was conducted in March and April, 2017.
2.3. Eligibility criteria
Participants were included if they were commercial taxi drivers, 18 years and above, held membership of a recognized taxi association, worked for at least 6 months and had fulfilled the mandatory 8 hours fasting preceding the study.
2.4. Study instrument
The participants were interviewed using the validated World Health Organization [WHO] STEPwise questionnaire[16] which comprises 3 major items; demographic, behavioral data, and measurements. A pilot study was conducted on 20 commercial taxi drivers to test its suitability in the settings and the effectiveness of the research process. The results of the pilot study were not included in the main study.
2.5. Ethical approval
Ethical approval for the study was obtained from the University of Fort Hare Research Ethics Committee (Reference number: GOO121SADE01) and the Eastern Cape Department of Health. The Director of the District Department of Transport, as well as the taxi rank chairpersons, gave permission before data collection. All participants provided written informed consent to participate in this study. Rights to confidentiality and anonymity were ensured throughout the study.
2.6. Data collection procedure
Data were obtained through personal interviews on socio-demographic variables: sex, age, race, level of education, marital status, and occupational history. Participants’ occupational history was categorized as period of driving below 2 years, within 2 to 5 years, 6 to 10 years, and above 10 years. Level of education was obtained by self-reporting of the highest grade level attained in school and was categorized as; no formal education, primary (grade 1–7), secondary (grade 8–12) and tertiary education. Behavioural variables; cigarette smoking (yes/no), alcohol use (yes/no), and consumption of sugar-sweetened beverages (never/rarely/sometimes/often) were obtained by self-reporting. Physical activity of the participants was obtained by self-reporting and categorized based on their engagement in moderate exercise (such as gardening) (yes/no) leading to an increase in heart rate and respiratory rate. Participants with less than 150 minutes of moderate-intense aerobic physical activity throughout the week were considered physically inactive.
2.7. Measurements
FBG of each participant was measured with a validated ACCU-CHEK glucose monitoring apparatus (Mannheim, Germany) in fasting state following standard procedure. Participants were diagnosed as having diabetes if the FBG was ≥7.0mmol/L or a self-reported history of diabetes or current use of anti-diabetic therapy, while pre-diabetes was defined as a FBG of 5.6 to 6.9 mmol/L.[17] Blood pressure was measured in accordance with standard protocols[18] with a Medic+ Digital Blood Pressure Monitor Model 1219 (Hamburg, Germany). Hypertension was defined according to the Eight Joint National Committee (JNC-8) Criteria as the average of 2 systolic blood pressure ≥140mmHg and diastolic ≥90mmHg or a history of hypertension or current medication use.[19] Using a SECA weighing scale and standiometer (Hamburg, Germany), body weight was measured in light clothes to the nearest 0.01 kg in the standing position and height was measured to the nearest 0.1 cm in standing position with closed feet (without shoes).[20] Body mass index (BMI) was calculated as weight in kilogram (kg) divided by height in square metres (kgm−2). BMI was categorized as not obese (<18.5 kgm−2–29.9 kg/m 2) or obese (≥30 kg/ m2).[21]
2.8. Statistical analysis
Data were expressed as mean values ± standard deviations (SD) for continuous variables. Counts (frequencies=n) and proportions (%) were reported for categorical variables. Pearson Chi-Square statistics were used to identify the factors significantly associated with diabetes at a 95% confidence level. Adjusted and unadjusted logistic regression was used to determine predictors of diabetes mellitus among the study participants. All statistical analyses were performed using the Statistical Package for Social Science (SPSS) version 22. A P value <.05 was considered statistically significant.
3. Results
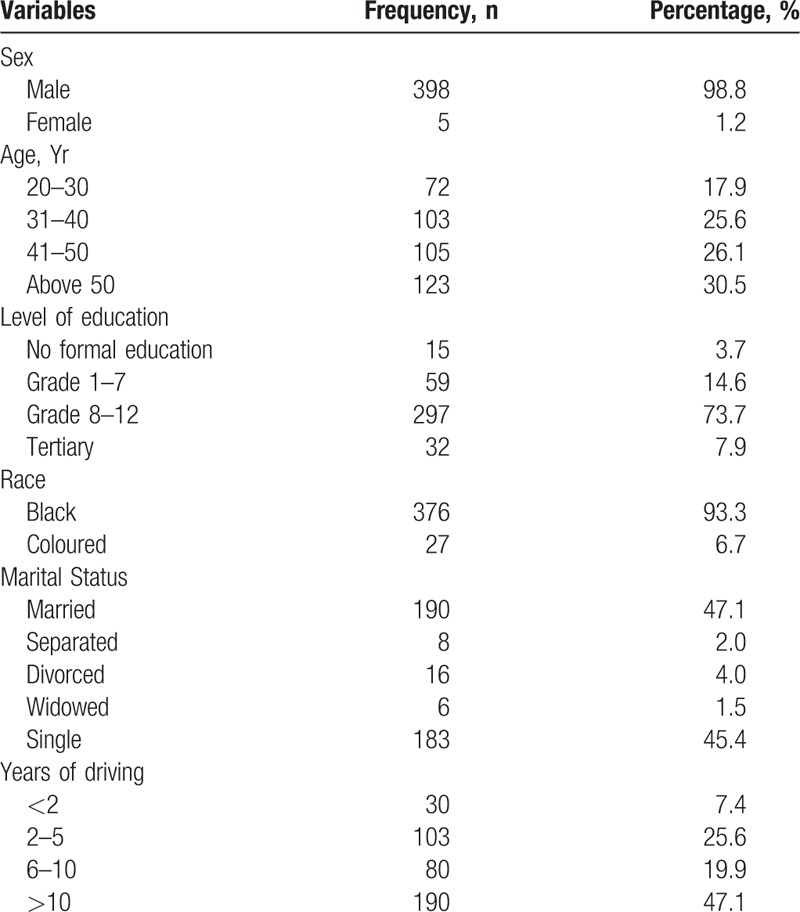
The mean age of the participants was 43.3 ± 12.5 years. The majority of the participants were male, had grade 8 to 12 educational level, were of black race, and had been driving for over 6 years (Table 1).
Table 1.
Demographic characteristics of study participants.
The prevalence of pre-diabetes and diabetes was 17% (95% CI: 13.4–20.6) and 16% (95% CI: 12.4–19.6), respectively. Of those who were diagnosed with diabetes (n = 63), 43 (68%) were aware of their diabetes status and 30 were already on treatment. Newly diagnosed participants were referred to clinics for confirmatory test and treatment.
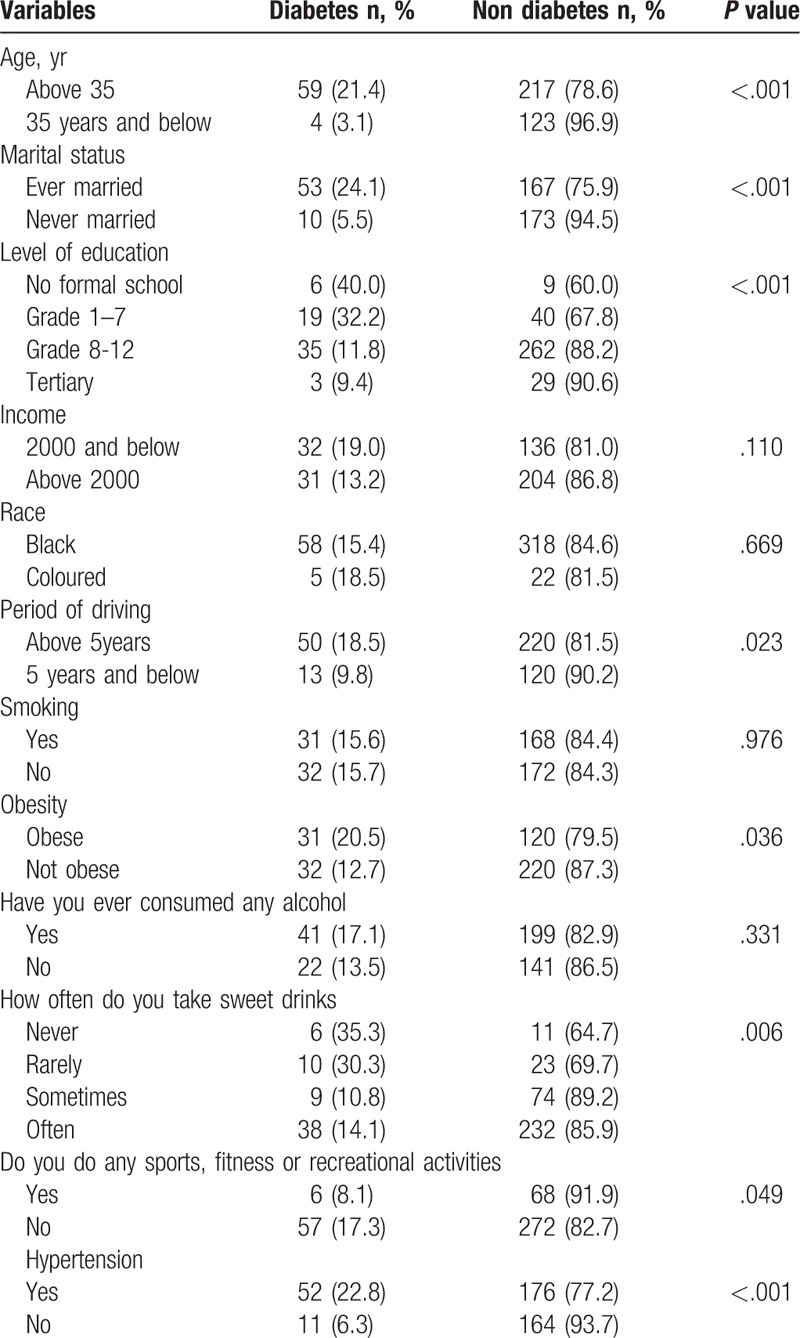
3.1. Associated risk factors with Diabetes
Age, marital status, level of education, period of driving, obesity, physical activity, and hypertension were significantly associated with diabetes mellitus. Race, alcohol use, and smoking were not significantly associated with diabetes. The prevalence of diabetes was higher among participants aged above 35 years compared to participants aged 35 years and below (21.4% vs 3.1%, P <.001). The participants who were ever married, with no formal education and a minimum level of education (grade 1–7) (32.2%) had a higher prevalence of diabetes compared to never-married participants (24.1% vs 5.5%, P <.001) and those with a higher level of education (40.0% vs 9.4%, P <.001). Also, there was a high prevalence of diabetes among participants who were obese (20.5% vs 12.7%, P <.036) and hypertensive (23% vs 6.3%, P <.001). Prevalence of diabetes among physically inactive participants (17.3% vs 8.1%, P <.049) was double the prevalence found among those physically active (Table 2).
Table 2.
Factors associated with diabetes.
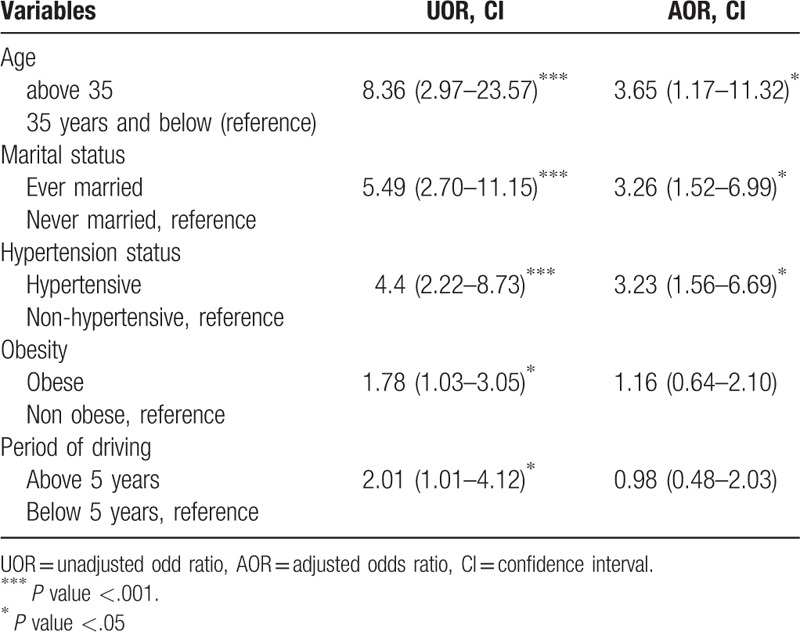
3.2. Logistic regression showing determinants of diabetes
In the unadjusted logistic regression, age, ever married, hypertension, obesity, and driving for more than 5 years were independently associated with diabetes. However, only age >35 (adjusted odds ratio [AOR] = 3.65, CI: 1.17–11.32), ever married (AOR= 3.26, CI: 1.52–6.99), and hypertension (AOR= 3.23, CI: 1.56–6.69) were associated with diabetes in the adjusted logistic regression model. Participants aged above 35 years were about 4 times more likely to develop diabetes compared to participants aged 35 and below. Participants who were ever married were 3 times more likely to develop diabetes compared to those never married. Hypertensive participants had thrice the likelihood of developing diabetes compared to those not hypertensive (Table 3).
Table 3.
Adjusted and unadjusted binary logistic regression showing determinants of diabetes.
4. Discussion
This present study determined the prevalence, awareness, treatment, and determinants of diabetes and pre-diabetes among commercial taxi drivers in BCMM, South Africa. This study is among the few studies reporting the prevalence of diabetes and pre-diabetes among commercial taxi drivers in South Africa. The findings of this study revealed an overall prevalence of 16% and 17% for diabetes and pre-diabetes, respectively. The prevalence of diabetes in this study is higher than studies carried out among drivers in countries like Hong Kong,[22] Iran,[7,23,24] and Brazil[25,26]; although, Sangaleti et al[27] reported a similar finding (16.4%) among commercial taxi drivers in South Brazil. However, when compared to a study conducted among the general population of South Africa, the prevalence rate found in this study is more than the 8.3% overall prevalence of diabetes in South Africa.[2] Diabetes mellitus is a metabolic disorder that poses a significant threat to the life of drivers, passengers, and other road users.[6] With the incessant projection of an increase in the prevalence of diabetes, coupled with the high prevalence of pre-diabetes found among the study participants, there is a need for prompt interventions to curb this growing menace, especially among this high-risk population group.
The analysis reveals that 68% (n = 43) of participants diagnosed in this study were already aware of their diabetes status and of these, the majority (n = 30) reported being on treatment. This result is close to that of Sangaleti et al,[27] who reported an awareness rate of 63% among drivers in Brazil. Diabetes awareness and treatment rate among the study participants is commendable. Also, as practiced in some countries,[7,8,23] adoption of mandatory medical fitness test for commercial drivers living with diabetes in South Africa could assist in improving awareness, treatment, and control. This could also ensure the safety of the commercial drivers, passengers, and other road users.
This study found that older age is associated with diabetes, which is consistent with previous studies conducted among drivers in Iran[7] and Hong Kong.[22] Aging increases susceptibility to diabetes.[28] Older age is associated with reduction in physical activities and weight gain, which are risk factors for diabetes.[29] Also, aging has been reported to be associated with a higher incidence of insulin resistance, inflammation, and impaired insulin secretion precipitated by impairment in the functioning and proliferative capacity of the islet cells with a resultant development of diabetes.[29–31] Thus, the American Diabetes Association[32] specified the need for regular diabetes screening among older adults.
A higher prevalence of diabetes was also found among the married commercial taxi drivers. This is similar to the findings of Owolabi et al[33] among adults in BCMM, South Africa. The association between diabetes and marriage is unclear. It could be due to the influence of clusters of modifiable and non-modifiable risk factors among the study participants.[34] Also, it might be that married participants have better and regular access to staple foods like maize meal coupled with regular snacking and unhealthy diets commonly eaten at various taxi ranks.
Also, hypertension was found to be associated with diabetes among the study participants. This is not surprising. Several studies have also reported similar association among drivers across various countries such as Iran,[7] Poland,[13] and Hong Kong.[22] This association is often linked to the similar metabolic pathways between both conditions as well as their shared risk factors, which range from genetics, behavioral, metabolic, and demographic to physiological factors.[35–37]
There is a tendency of obesity to be related with diabetes,[33,38] however we are unable to confirm this association after controlling for important covariates, Most of the commercial taxi drivers usually sit for long hours (sedentary) without engaging in any physical activity. They work in a stressful environment and with fewer hours of sleep (6.37 ± 1.6).[32] These lifestyle behaviors could lead to obesity and the development of diabetes.[38,39]
Surprisingly, a higher prevalence of diabetes was found among participants who reported not taking sweet beverages. This is contrary to several studies that illustrate the harmful effect of sweet beverages and their negative effect on type 2 diabetes.[40–42] One plausible explanation for our result is that taxi driver already diagnosed with diabetes may have stopped consuming sweet beverages, while those who consume sweet beverages are still to develop diabetes.
5. Strengths and limitations
The study provides useful data on the health condition of the commercial drivers in South Africa. However, some study limitations should also be acknowledged. First, the cross-sectional study design does not allow establishing causality between the risk factors and diabetes. Also, the diagnosis of diabetes among participants without previous history was based on a single fasting capillary glycaemia, which is associated with diagnostic bias. It is noteworthy that the 20 newly diagnosed diabetics were referred to clinics but we lack their results, which would have added value to the study and would have confirmed the prevalence results. The use of capillary glycaemia is a convenient method for diabetes diagnosis in epidemiological study.[43] In addition, our sampling strategy was not random, which is the best technique for providing an unbiased representative sample of a target population. This is because we were unable to get the sampling frame of drivers in East London. However, in order to reduce the bias of the opportunity sampling adopted in this study, we gave every driver in each taxi rank a chance to be chosen for the study by spending a minimum of 4 days in each taxi rank in the study settings. Data collection took place only on working days (Monday to Friday), when all drivers are more likely to be present at the taxi Rank. Despite our sampling limitations, our study provides much-needed data on the prevalence and awareness of diabetes among commercial drivers in South Africa.
6. Conclusion
The prevalence of diabetes mellitus among commercial taxi drivers in this study is high; almost twice the national prevalence of diabetes in South Africa, and higher than the reported prevalence in other developing countries. Age, ever married, and hypertension were the significant and independent predictors of diabetes among the study participants. The majority of the drivers living with diabetes were aware of their status and already on treatment. There is a need to further encourage and organize opportunistic screening for diabetes among this cohort in order to further reduce the burden of undiagnosed diabetes in the country.
Acknowledgments
The authors wish to acknowledge the support of drivers who participated in the study.
Author contributions
AOA, DTG, EOO, OVA and AIA contributed to study conception and manuscript preparation. AOA EOO and AIA contributed to the collection of data, data analysis and manuscript preparation. All authors read, and approved the final manuscript before submission.
Conceptualization: Aanuoluwa Odunayo Adedokun, Daniel Ter Goon, Eyitayo Omolara Owolabi, Oladele Vincent Adeniyi.
Data curation: Aanuoluwa Odunayo Adedokun, Anthony Idowu Ajayi.
Formal analysis: Anthony Idowu Ajayi.
Methodology: Aanuoluwa Odunayo Adedokun, Daniel Ter Goon, Eyitayo Omolara Owolabi.
Software: Anthony Idowu Ajayi.
Supervision: Daniel Ter Goon, Oladele Vincent Adeniyi.
Validation: Daniel Ter Goon, Oladele Vincent Adeniyi.
Visualization: Aanuoluwa Odunayo Adedokun, Eyitayo Omolara Owolabi, Anthony Idowu Ajayi.
Writing – original draft: Aanuoluwa Odunayo Adedokun, Eyitayo Omolara Owolabi.
Writing – review & editing: Daniel Ter Goon, Oladele Vincent Adeniyi, Anthony Idowu Ajayi.
Aanuoluwa Odunayo Adedokun orcid: 0000-0003-3850-2578.
Aanuoluwa Odunayo Adedokun orcid: 0000-0003-3850-2578.
Footnotes
Abbreviations: AOR = adjusted odds ratio, BCMM = Buffalo City Metropolitan Municipality, CI = confidence interval, FBG = fasting blood glucose.
Ethical approval for the study was obtained in accordance with Helsinki II Declaration from the University of Fort Hare Research Ethics Committee (Reference number: GOO121SADE01) and the Eastern Cape Department of Health. The Director of the District Department of Transport, as well as the taxi rank chairpersons, gave permission before data collection. All participants provided written informed consent to participate in this study. Rights to confidentiality and anonymity were ensured throughout the study.
All authors approved the submission of this final draft towards publication in a peer-reviewed journal.
The authors declare no conflict of interest.
All the data analyzed in this study will be made available by the corresponding author on reasonable request.
References
- [1].Gill G. Diabetes in Africa—puzzles and challenges. Indian J Endocrinol Metab 2014;18:249–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137–49. [DOI] [PubMed] [Google Scholar]
- [3].International Diabetes Federation. IDF Africa Region 2017. Available at: https://www.idf.org/our-network/regions-members/africa/members/25-south-africa Accessed April 12, 2018 [Google Scholar]
- [4].Pillay-van Wyk V, Dorrington RE, Bradshaw V. Rapidly changing mortality profiles in South Africa in its nine province. S Afr Med J 2017;107:168–9. [DOI] [PubMed] [Google Scholar]
- [5].Abu Dabrh AM, Firwana B, Cowl CT, et al. Health assessment of commercial drivers: a meta-narrative systematic review. BMJ Open 2014;4:e003434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].de Grauw WJC, van de Lisdonk EH, Behr RRA, et al. The impact of type 2 diabetes mellitus on daily functioning. Fam Pract 1999;16:133–9. [DOI] [PubMed] [Google Scholar]
- [7].Izadi N, Malek M, Aminian O, et al. Medical risk factors of diabetes mellitus among professional drivers. J Diabetes Metab Disord 2013;12: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Thiese MS, Moffitt G, Hanowski RJ, et al. Commercial driver medical examinations: prevalence of obesity, comorbidities, and certification outcomes. J Occup Env Med 2015;57:659–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jones GC, Frier BM. Medical assessment for licensing of taxi drivers by Scottish Local Authorities. Occup Med 1997;47:40–4. [DOI] [PubMed] [Google Scholar]
- [10].Fitness to Drive [Internet]. 2016. [cited 9 July 2017]. Available at: https://patient.info/doctor/fitness-to-drive#ref-1 Accessed April 13, 2018 [Google Scholar]
- [11].Lakshman A, Manikath N, Rahim A, Anilakumari VP. Prevalence and Risk Factors of Hypertension among Male Occupational Bus Drivers in North Kerala, South India: A Cross-Sectional Study. ISRN Prev Med. 2014, 318532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sena JEA, Pontes LM, Ferreira UMG, et al. Body composition and relationship with the level of physical activity of taxi drivers and post men of João Pessoa (PB). Fit Perf J 2008;7:20–5. [Google Scholar]
- [13].Marcinkiewicz A, Szosland D. Selected risk factors of diabetes mellitus among road transport drivers. Int J Occup Med Environ Health 2010;23:175–80. [DOI] [PubMed] [Google Scholar]
- [14].Overview: Buffalo City Metropolitan Municipality [Internet]. 2017. [cited 14 June 2017]. Available at: https://www.localgovernment.co.za Accessed April 13, 2018 [Google Scholar]
- [15].Creative Research Systems. Sample size calculator 2015. Available at: https://www.surveysystem.com/sscalc.htm Accessed April 17, 2018 [Google Scholar]
- [16].World Health Organization. STEPS: A framework for surveillance: The WHO STEPwise approach to Surveillance of noncommunicable diseases (STEPS) 2003. Available at: www.who.int/ncd_surveillance/.../steps_framework_dec03.pdf Accessed April 13, 2018 [Google Scholar]
- [17].American Diabetes Association. Diagnosing Diabetes and Learning about Prediabetes 2014. Available at: http://www.diabetes.org/diabetesbasics/diagnosis/referrer=https://www.google.co.za/ Accessed April 16, 2018 [Google Scholar]
- [18].Seedat YK, Rayner BL, Veriava Y. South African hypertension practice guideline 2014. Cardiovasc J Afr 2014;25:288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bell K, Twiggs J, Olin BR. Hypertension: the silent killer: updated JNC-8 guideline recommendations. Alabama Pharm Assoc 2015;Available at: https://cdn.ymaws.com/www.aparx.org/resource/resmgr/CEs/CE_Hypertension_The_Silent_K.pdf Accessed April 5, 2018. [Google Scholar]
- [20].Marfell-Jones M, Olds T, Stew A, et al. International standards for anthropometric assessment. Potchefstroom, South Africa: International Society for the Advancement of Kinanthropometry; 2006. [Google Scholar]
- [21].World Health Organization. Definition, diagnosis & classification of diabetes mellitus and its complications: report of a WHO Consultation. Part 1: diagnosis andclassification of diabetes mellitus Geneva, 1999. Available at: http://www.who.int/iris/handle/10665/66040 Accessed April 15, 2018 [Google Scholar]
- [22].Siu SC, Wong KW, Lee KF, et al. Prevalence of undiagnosed diabetes mellitus and cardiovascular risk factors in Hong Kong professional drivers. Diabetes Res Clin Pract 2012;96:60–7. [DOI] [PubMed] [Google Scholar]
- [23].Tofangchihia S, Dehghan F, Saberi H. Diabetes mellitus in drivers: a cross-sectional study in Yazd, Iran, 2006–2009. Thrita 2014;3: [Google Scholar]
- [24].Saberi HR, Moravveji AR, Fakharian E, et al. Prevalence of metabolic syndrome in bus and truck drivers in Kashan. Iran Diabetol Metab Syndr 2011. 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hirata RP, Sampaio LM, Leitao Filho FS, et al. General characteristics and risk factors of cardiovascular disease among interstate bus drivers. Scientific World J 2012;2012:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Reis LAP, Costa CDD, Rodrigues DS, et al. Obesity, hypertension and diabetes among truck drivers in the middle-west, Brazil. Biosci J 2017;33:485–93. [Google Scholar]
- [27].Sangaleti CT, Trincaus MR, Baratieri T, et al. Prevalence of cardiovascular risk factors among truck drivers in the South of Brazil. BMC Public Health 1063;14: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gunasekaran U, Gannon M. Type 2 Diabetes and the Aging Pancreatic Beta Cell. Aging 2011;3:565–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Amati F, Dubé JJ, Coen PM, et al. Physical inactivity and obesity underlie the insulin resistance of aging. Diabetes Care 2009;32:1547–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Maedler K, Schumann DM, Schulthess F, et al. Aging correlates with decreased β-cell proliferative capacity and enhancedsensitivity to apoptosis a potential role for fas and pancreatic duodenal homeobox-1. Diabetes 2006;55:2455–62. [DOI] [PubMed] [Google Scholar]
- [31].Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in Older Adults. Diabetes Care 2012;35:2650–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes care 2013;36(Suppl 1):S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Owolabi EO, Goon DT, Seekoe E, et al. Correlates of pre-diabetes and Type 2 diabetes in Buffalo City Municipality, South Africa. AJPHES 2016;22:1019–35. [Google Scholar]
- [34].Leong A, Rahme E, Dasgupta K. Spousal diabetes as a diabetes risk factor: a systematic review and meta-analysis. BMC Med 2014;12:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Landsberg L, Molitch M. Diabetes and hypertension: pathogenesis, prevention and treatment. Clin Exp Hypertens 2004;26:621–8. [DOI] [PubMed] [Google Scholar]
- [36].Cheung BMY, Li C. Diabetes and hypertension: is there a common metabolic pathway. Cur Atheroscler Rep 2012;14:160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Tekola-Ayele F, Adeyemo AA, Rotimi CN. Genetics and epiemiology of type 2 diabetes and cardiovascular disease in Africa. Prog Cardiovasc Dis 2013;56:251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Marks R, Landaira M, Sleep Disturbances of sleep, stress and obesity: a narrative review. J Obes Eating Disord 2015;1: [Google Scholar]
- [39].Al-Quwaidhi A, Pearce M, Critchley J, et al. Obesity and type 2 diabetes mellitus: a complex association. Saudi J Obesity 2013;1:49–56. [Google Scholar]
- [40].Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14:606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007;97:667–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Imamura F, O’Connor L, Ye Z, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015;351:h3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Foss-Freitas MC, Andrade RC, Figueiredo RC, et al. Comparison of venous plasma glycemia and capillary glycemia for the screening of type 2 diabetes mellitus in the Japanese-Brazilian community of Mombuca (Guatapara-SP) Diabetol Metab Syndr 2010;2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]


