Abstract
Background
Psoriasis is an inflammatory skin disease associated with atherosclerotic cardiovascular disease (ASCVD) risk factors and vascular disease. The relative impact of psoriasis on vascular disease is the strongest in young patients with psoriasis, yet data are lacking on how sex differences influence cardiovascular risk factors and vascular disease in these patients.
Objective
This observational study aimed to identify the burden of cardiovascular risk factors and vascular disease in patients with psoriasis and to explore whether this burden is different between men and women age < 35 years.
Methods
Young (age ≥ 20 and < 35 years) hospitalized patients with psoriasis from the United States National Inpatient Sample were compared with those matched patients without psoriasis. Vascular disease was defined as ASCVD and/or venous thromboembolic disease. Multivariable logistic regression was used to determine the associations between psoriasis, sex, ASCVD risk factors, and vascular disease.
Results
Overall, patients with psoriasis (n = 18,353) were more often obese (16% vs. 6%); smokers (31% vs. 17%); and diagnosed with diabetes mellitus (10% vs. 6%), hypertension (16% vs. 8%), hyperlipidemia (6% vs. 2%), ASCVD (2.2% vs. 1.6%), and deep vein thrombosis (6% vs. 4%; all p < .001) compared with patients without psoriasis (n = 55,059; matched by age, sex, and race). When stratified by sex, women with psoriasis were more likely to have multiple cardiovascular risk factors and ASCVD (odds ratio: 2.6; 95% confidence interval [2.1-3.1]) compared with men with psoriasis (odds ratio: 1.2; 95% confidence interval [0.9-1.4]; interaction p < .01). The association between psoriasis and ASCVD in women remained unchanged after multivariable adjustment for traditional cardiovascular risk factors.
Conclusion
Psoriasis was associated with cardiovascular disease and risk factors in young hospitalized patients, with stronger associations among women than among men.
Keywords: Psoriasis, sex differences, vascular disease
Introduction
Psoriasis is a chronic autoimmune inflammatory disease of the skin that affects 2% to 3% of the population in the United States. Psoriasis is linked to traditional cardiovascular risk factors, such as hypertension (HTN), hyperlipidemia (HLD), obesity, diabetes mellitus (DM), and tobacco use (Hu and Lan, 2017). Patients with psoriasis are also at a higher risk of atherosclerotic cardiovascular disease (ASCVD), with up to a 50% greater prevalence of vascular disease than age- and sex-matched controls without psoriasis (Boehncke and Boehncke, 2012, Miller et al., 2013). Furthermore, psoriasis has been reported to be an independent risk factor for myocardial infarction, and the magnitude of this association is particularly strong among patients with psoriasis who are in their 20s and 30s (Gelfand et al., 2006).
Despite the overall high prevalence of psoriasis in the U.S. population, studies evaluating the associations between cardiovascular risk factors and ASCVD in young patients with psoriasis have been relatively small (Gelfand et al., 2006). Additionally, specific subtypes of vascular disease, such as venous thromboembolism (VTE), have not been fully studied; sex differences in the rates of ASCVD-associated comorbidities and vascular disease, although speculated (Egeberg et al., 2016, Gelfand et al., 2006, Hu and Lan, 2017, Levesque et al., 2013, Li et al., 2012, Qureshi et al., 2009, Wu et al., 2015), have yet to be fully addressed. Therefore, the objectives of this observational study were to identify the burden of cardiovascular risk factors and vascular disease in patients with psoriasis and to explore whether this burden is different between men and women age < 35 years.
Methods
This was a cross-sectional study based on the Healthcare Cost and Utilization Project’s National Inpatient Sample (NIS) data from January 1, 2008 through December 31, 2014. The NIS is a large, de-identified, administrative database with discharge-level coded data from a 20% sample of all hospitals in the United States and includes data from approximately 8 million hospitalizations per year (Smilowitz et al., 2017). We queried the NIS to identify hospitalized adults age ≥ 20 and < 35 years with a diagnosis of psoriasis (Egeberg et al., 2016, Gelfand et al., 2006). The upper limit of the age inclusion criterion (< 35 years) was based on the average age reported in other studies assessing ASCVD risk in young patients with psoriasis (Egeberg et al., 2017). The lower limit of the age inclusion criterion (≥ 20 years) was based on American Heart Association publications and figures defining young adults in the National Health and Nutrition Examination Survey population (Benjamin et al., 2018).
Patients hospitalized with psoriasis were identified if they were assigned an International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code of 696.1 or 696.0 (Asgari et al., 2013). Young adults hospitalized with psoriasis (n = 18,353 consecutive hospitalizations within the study period) in the NIS were then matched by age, sex, race/ethnicity, and year of admission to patients without psoriasis (n = 55,059) in a 1:3 ratio. In this large administrative database, medical comorbidities associated with ASCVD, including HTN, HLD, DM, obesity, and a history of tobacco use, were defined by their appropriate ICD-9 codes as previously described (Birman-Deych et al., 2005).
The outcome variable of interest was vascular disease, evaluated using a diagnosis of ASCVD or VTE. ASCVD was defined as a composite of any ICD-9 diagnoses of coronary artery disease (CAD), cerebrovascular disease (CVA), or peripheral artery disease (PAD). Key ASCVD subgroups were evaluated separately, including acute myocardial infarction (identified by ICD-9 diagnosis codes for ST-segment [410.4] and non-ST-segment elevation myocardial infarction [410.71]) and acute ischemic stroke (433.x1, 434.x1, 436, and 437.1). We evaluated the prevalence of VTE by identifying diagnoses of pulmonary embolism (PE; 415.1) and deep vein thrombosis (DVT; 453.40).
Continuous variables were reported as mean (standard deviation), and categorical variables were reported as percentages. Multivariable conditional logistic regression was used to calculate prevalence odds ratios (ORs) and to account for cardiovascular risk factors, including HTN, HLD, obesity, DM, and tobacco use. When examining the association between cardiovascular risk factors and psoriasis, we restricted our sample to patients without ASCVD. This subgroup allowed us to remove potential reverse causation (patients with diagnosed ASCVD may present subsequent modified cardiovascular risk factors) and allow us to explore an earlier phase in the natural history of atherosclerotic disease. We tested for interactions and performed stratified analyses by sex. All analyses were performed in STATA, version14 (StataCorp LP, College Station, TX).
Results
Psoriasis and cardiovascular risk factors
Clinical characteristics of hospitalized young patients with and without psoriasis are shown in Table 1. Overall, the mean age was 28.7 ± 4 years, 62% of patients were white, and 58% were women. Obesity, HTN, HLD, DM, and past or present tobacco use were significantly more common in young patients with psoriasis compared with matched patients without psoriasis (Table 1). At least one ASCVD risk factor was present in 52% of young patients with psoriasis compared with 30% of the matched patients without psoriasis (all comparison p < .001).
Table 1.
Clinical characteristics of all patients with psoriasis compared those of matched patients without psoriasis
| Characteristic | Psoriasis, n (%) |
No psoriasis, n (%)⁎ |
|---|---|---|
| n = 18,353 | n = 55,059 | |
| Age, mean (standard deviation), year | 28.7 ± 4 | 28.7 ± 4 |
| Men | 7796 (42) | 23,388 (42) |
| Race/ethnicity | ||
| White | 11,392 (62.0) | 34,176 (62.0) |
| Black non-Hispanic | 1245 (6.8) | 3735 (6.8) |
| Hispanic | 1660 (9.0) | 4980 (9.0) |
| Obesity | 2881 (15.7) | 3514 (6.4) |
| Hypertension | 2835 (15.5) | 4345 (7.9) |
| Hyperlipidemia | 1010 (5.5) | 1225 (2.2) |
| Diabetes mellitus | 1846 (10.1) | 2976 (5.4) |
| Tobacco use | 5596 (30.5) | 9489 (17.2) |
Matched by age, sex, race/ethnicity and year of hospital admission. P-values for all other characteristics < .001.
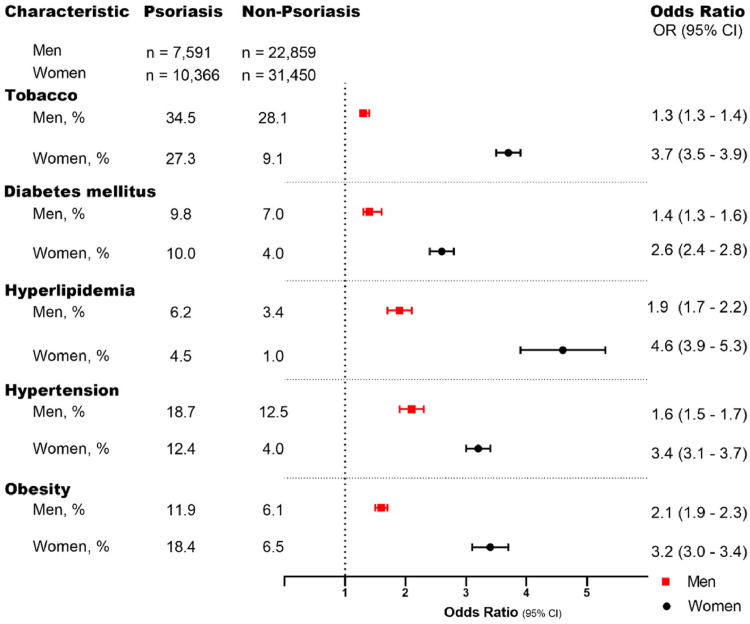
The prevalence and ORs of cardiovascular risk factors in patients with psoriasis are presented in patients without preexisting vascular disease to limit any potential confounding. In the stratified analysis, the prevalence rates of smoking, HLD, and HTN were all higher in men than in women with psoriasis, but women with psoriasis had higher rates of obesity and DM (Fig. 1). The association between psoriasis and traditional cardiovascular risk factors was consistently stronger in women than in men across all cardiovascular risk factors (Fig. 1).
Fig. 1.
Sex-specific prevalence of cardiovascular risk factors and their association with psoriasis case status among patients without atherosclerotic cardiovascular disease. Unadjusted odds ratio (OR) with confidence interval (95% CI)
Psoriasis and atherosclerotic cardiovascular disease
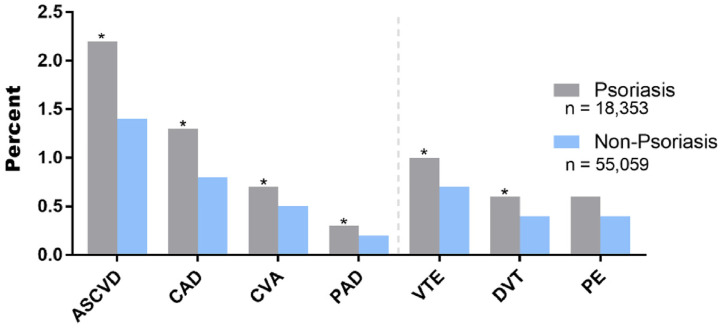
Young hospitalized patients with psoriasis had a higher prevalence of ASCVD compared with matched patients without psoriasis (2.2% vs. 1.4%; p < .01). Additionally, the individual subcomponents of ASCVD, including CAD, CVA, and PAD, were more common in patients with psoriasis (Fig. 2). VTE, including DVT, was also more common in patients with psoriasis (Fig. 2); however, psoriasis was not associated with a significantly greater frequency of acute PE.
Fig. 2.
Prevalence of vascular disease diagnoses in hospitalized patients with psoriasis compared with that of matched hospitalized patients without psoriasis. ⁎p < .01. ASCVD, atherosclerotic cardiovascular disease (CAD + CVA + PAD); CAD, coronary artery disease; CVA, cerebrovascular disease; DVT, deep vein thrombosis; PAD, peripheral artery disease; PE, pulmonary embolism; VTE, venous thromboembolism (DVT + PE)
When stratified by sex, the prevalence of ASCVD among young patients with psoriasis was 1.8% in women and 2.6% in men. Among the controls, the prevalence of ASCVD was 0.7% in women and 2.3% in men. Overall, the associations between psoriasis and ASCVD were stronger in women with psoriasis than in men (Table 2). Compared with women without psoriasis, women with psoriasis had higher odds of ASCVD in the unadjusted analyses (OR: 2.6; 95% confidence interval [CI; 2.1-3.2]) and after adjustment for cardiovascular risk factors (adjusted OR: 1.4; 95% CI [1.1-1.8]). Similarly, psoriasis was associated with the individual subgroups of CAD, CVA, and PAD among women (Table 2). In contrast, men with psoriasis did not have higher odds of ASCVD compared with those without psoriasis in the unadjusted analyses (OR: 1.2; 95% CI [0.9-1.4]) or after multivariable adjustment.
Table 2.
Odds of vascular disease in patients with psoriasis compared with matched patients without psoriasis, stratified by sex
| Women | Psoriasis, n (%) |
No psoriasis, n (%) |
OR (95% CI) |
Adjusted OR (95% CI)⁎ |
|---|---|---|---|---|
| n = 10,557 | n = 31,671 | |||
| Atherosclerotic CVD | ||||
| Any atherosclerosis | 191 (1.8) | 221 (0.7) | 2.6 (2.1-3.2) | 1.4 (1.1-1.8) |
| Coronary artery disease | 89 (0.8) | 93 (0.3) | 2.9 (2.1-3.9) | 1.2 (0.8-1.8) |
| Acute myocardial infarction | 16 (0.2) | 17 (0.05) | 1.9 (1.3-2.9) | 1.3 (0.6-2.9) |
| Cerebrovascular disease | 71 (0.7) | 97 (0.3) | 2.3 (1.6-3.0) | 1.5 (1.0-2.0) |
| Acute ischemic stroke | 27 (0.3) | 37 (0.1) | 2.2 (1.3-3.6) | 1.7 (0.9-2.9) |
| Peripheral artery disease | 40 (0.4) | 40 (0.1) | 3.0 (1.9-4.7) | 1.9 (1.1-3.2) |
| Venous thromboembolism | ||||
| Any venous thromboembolism | 94 (0.9) | 142 (0.5) | 2.0 (1.5-2.6) | 1.3 (0.9-1.8) |
| Deep vein thrombosis | 51 (0.5) | 73 (0.2) | 2.1 (1.5-3.0) | 1.8 (1.2-2.7) |
| Pulmonary embolism | 59 (0.6) | 88 (0.3) | 2.0 (1.4-2.8) | 1.2 (0.8-1.7) |
| Men | n = 7796 | n = 23,388 | ||
| Atherosclerotic CVD | ||||
| Any atherosclerosis | 205 (2.6) | 529 (2.3) | 1.2 (0.9-1.4) | 0.9 (0.8-1.10) |
| Coronary artery disease | 142 (1.8) | 329 (1.4) | 1.3 (1.1-1.6) | 1.0 (0.8-1.2) |
| Acute myocardial infarction | 51 (0.7) | 91 (0.4) | 1.7 (1.2-2.4) | 1.4 (1.0-1.9) |
| Cerebrovascular disease | 50 (0.6) | 152 (0.7) | 1.0 (0.7-1.4) | 0.9 (0.6-1.2) |
| Acute ischemic stroke | 23 (0.3) | 66 (0.3) | 1.0 (0.7-1.7) | 1.0 (0.6-1.6) |
| Peripheral artery disease | 31 (0.3) | 72 (0.3) | 0.9 (0.5-1.4) | 0.8 (0.5-1.3) |
| Venous thromboembolism | ||||
| Any venous thromboembolism | 83 (1.1) | 261 (1.1) | 0.9 (0.7-1.2) | 0.9 (0.7-1.2) |
| Deep vein thrombosis | 51 (0.7) | 141 (0.6) | 1.1 (0.8-1.5) | 1.0 (0.7-1.4) |
| Pulmonary embolism | 42 (0.5) | 153 (0.7) | 0.8 (0.6-1.2) | 0.8 (0.6-1.1) |
CI, confidence interval; CVD, cardiovascular disease; OR, odds ratio
OR adjusted for age, race/ethnicity, and year of hospital admission.
Multivariable model adjusted for age, race/ethnicity, obesity, hypertension, diabetes, hyperlipidemia, tobacco use, and year of hospital admission.
Sex differences in the association between psoriasis and VTE were also observed (interaction p < .01; Table 2). In the NIS sample, men had higher rates of VTE compared with women. However, among women, a diagnosis of psoriasis was associated with DVT (subcomponent of VTE; OR: 2.1; 95% CI [1.5-3.0]), which remained after multivariable adjustment; no such association was observed among men in the univariate analysis (OR: 1.1; 95% CI [0.8-1.2]) or after multivariable adjustment.
Discussion
In this analysis of 18,363 young hospitalized patients diagnosed with psoriasis and 55,059 matched hospitalized controls, we found that the prevalence of cardiovascular risk factors was higher among patients with psoriasis compared with those without psoriasis. We also found increased odds of vascular disease, independent of traditional cardiovascular risk factors. Significant sex differences were also observed, with stronger associations between psoriasis and cardiovascular risk factors, ASCVD, and DVT in women compared with men. To the best of our knowledge, this analysis is one of the largest studies to focus on cardiovascular risk factors as well as ASCVD, VTE and many of its subgroups in young patients with psoriasis and is one of the largest studies to describe sex differences in the association between psoriasis and vascular disease (Egeberg et al., 2016, Kimball et al., 2008, Lai and Yew, 2016, Levesque et al., 2013, Li et al., 2012, Wu et al., 2015).
Over the past decade, a number of studies have examined the association between psoriasis and ASCVD (Gelfand et al., 2006). In a 2006 study on the risk of ASCVD in patients with psoriasis from the United Kingdom, the odds of ASCVD were highest in 20-year-olds with severe psoriasis (Gelfand et al., 2006). Although the increased cardiovascular risk in young adults is well recognized, sex differences in the association between immunologic and vascular diseases remain understudied, and prior literature on this association yielded conflicting results (Samarasekera et al., 2013). For example, one small study showed that women with psoriasis had a higher prevalence of obesity but lower rates of metabolic syndrome than men with psoriasis (Sommer et al., 2006). Another larger study revealed that young women with psoriasis had three-fold higher rates of metabolic syndrome than young men with psoriasis (Danielsen et al., 2015). In other autoimmune diseases, such as rheumatoid arthritis, a small study showed that the relative risk of a cardiac event was several-fold higher in men compared with women with rheumatoid arthritis (del Rincon et al., 2001).
In our study, men with and without psoriasis had higher rates of ASCVD and VTE than women, a finding that is consistent with previous studies (Mosca et al., 2011). However, our analysis suggests that psoriasis is independently associated with ASCVD and DVT in young women, but in not men, which is a novel finding. In the present study, women with psoriasis had two- to three-fold higher odds of having a cardiovascular risk factor comorbidity and a higher prevalence of ASCVD or DVT than matched patients without psoriasis. In men, the odds of ASCVD, VTE, or cardiovascular risk factors were increased, but only upwards of two times that of matched without psoriasis, a finding that was largely driven by acute myocardial infarction.
Overall, these data suggest that with inflammatory autoimmune conditions such as psoriasis, complex inflammatory pathways (Garshick et al., 2019) potentially interacting with hormonal factors might be at play and deserve further investigation to explain how sex influences associations between psoriasis, ASCVD, and VTE, particularly among young patients.
There are several limitations to our study. Given the cross-sectional nature of our study, we cannot draw causal conclusions or exclude reverse causality. In any large administrative database, the potential of miscoding of data exists and adds bias and error to the analysis. Psoriasis disease severity, disease duration, and medications were not captured in this administrative database. Therefore, this analysis may have underestimated the association between psoriasis and vascular disease because we could not account for patients who received aspirin, statins, or other medications, which could potentially lower the occurrence of ASCVD. Finally, we chose to evaluate young (defined as < 35 years of age) hospitalized patients with psoriasis. We selected these age thresholds based on previously reported associations between psoriasis and ASCVD, which are the most pronounced in younger individuals, to permit comparisons with other published studies on young patients with psoriasis and because of the limited data in this population (Egeberg et al., 2017, Gelfand et al., 2006).
Conclusion
This is a hypothesis-generating study, and we found that young adults with psoriasis were more likely to have a diagnosis of cardiovascular disease risk factors, ASCVD, and DVT than young adults without psoriasis. These associations were primarily driven by women with psoriasis. Whether this finding reflects a heightened cardiovascular vulnerability in women with psoriasis compared with men with psoriasis should be explored in future mechanistic studies.
Additionally, traditional risk prediction scores do not adequately capture cardiovascular risk in young patients (Garshick and Underberg, 2017). Our findings help clinicians further recognize the relatively higher rate of ASCVD and ASCVD-related comorbidities in young patients, and may allow earlier initiation of therapeutic interventions designed to reduce ASCVD. Future studies are needed to confirm and explore the higher prevalence of risk factors and ASCVD noted in women with psoriasis and to determine the role of ASCVD risk factor modification therapies in young patients with psoriasis to mitigate vascular disease risk (Egeberg et al., 2017, Gelfand et al., 2006).
Footnotes
Sources of support: This study was funded by a National Institutes of Health training grant (T32HL098129), Glorney–Raisbeck Research Fellowship, National Institutes of Health Clinical and Translational Science Awards (UL1TR001445, KL2TR001446, and TL1TR001447), and an American Heart Association Career Development Grant (18CDA34080540), all awarded to Dr. Garshick.
Conflicts of interest: The authors report no conflicts of interest related to the current study.
References
- Asgari M.M., Wu J.J., Gelfand J.M., Salman C., Curtis J.R., Harrold L.R. Validity of diagnostic codes and prevalence of psoriasis and psoriatic arthritis in a managed care population, 1996-2009. Pharmacoepidemiol Drug Saf. 2013;22:842–849. doi: 10.1002/pds.3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin E.J., Virani S.S., Callaway C.W., Chamberlain A.M., Chang A.R., Cheng S. Heart disease and stroke statistics-2018 update: A report from the American Heart Association. Circulation. 2018;137:e67–492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- Birman-Deych E., Waterman A.D., Yan Y., Nilasena D.S., Radford M.J., Gage B.F. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- Boehncke W.H., Boehncke S. Cardiovascular mortality in psoriasis and psoriatic arthritis: Epidemiology, pathomechanisms, therapeutic implications, and perspectives. Curr Rheumatol Rep. 2012;14:343–348. doi: 10.1007/s11926-012-0260-8. [DOI] [PubMed] [Google Scholar]
- Danielsen K., Wilsgaard T., Olsen A.O., Eggen A.E., Olsen K., Cassano P.A. Elevated odds of metabolic syndrome in psoriasis: A population-based study of age and sex differences. Br J Dermatol. 2015;172:419–427. doi: 10.1111/bjd.13288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeberg A., Bruun L.E., Mallbris L., Gislason G.H., Skov L., Wu J.J. Family history predicts major adverse cardiovascular events (MACE) in young adults with psoriasis. J Am Acad Dermatol. 2016;75:340–346. doi: 10.1016/j.jaad.2016.02.1227. [DOI] [PubMed] [Google Scholar]
- Egeberg A, Skov L, Joshi AA, Mallbris L, Gislason GH, Wu JJ, et al. The relationship between duration of psoriasis, vascular inflammation, and cardiovascular events. J Am Acad Dermatol 2017;77:650–6.e3. [DOI] [PMC free article] [PubMed]
- Garshick M., Underberg J.A. The use of primary prevention statin therapy in those predisposed to atherosclerosis. Curr Atheroscler Rep. 2017;19:48. doi: 10.1007/s11883-017-0685-7. [DOI] [PubMed] [Google Scholar]
- Garshick M.S., Barrett T., Wechter T., Azarchi S., Scher J., Neimann A. Inflammasome signaling and impaired vascular health in psoriasis. Arterioscler Thromb Vasc Biol. 2019;39:787–798. doi: 10.1161/ATVBAHA.118.312246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand J.M., Neimann A.L., Shin D.B., Wang X., Margolis D.J., Troxel A.B. Risk of myocardial infarction in patients with psoriasis. JAMA. 2006;296:1735–1741. doi: 10.1001/jama.296.14.1735. [DOI] [PubMed] [Google Scholar]
- Hu S.C., Lan C.E. Psoriasis and cardiovascular comorbidities: Focusing on severe vascular events, cardiovascular risk factors and implications for treatment. Int J Mol Sci. 2017;18 doi: 10.3390/ijms18102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimball A.B., Robinson D., Jr., Wu Y., Guzzo C., Yeilding N., Paramore C. Cardiovascular disease and risk factors among psoriasis patients in two U.S. healthcare databases, 2001-2002. Dermatology. 2008;217:27–37. doi: 10.1159/000121333. [DOI] [PubMed] [Google Scholar]
- Lai Y.C., Yew Y.W. Psoriasis and thyroid profile: Analysis of the U.S. National Health and Nutrition Examination Survey database. Indian J Dermatol Venereol Leprol. 2016;82:310–312. doi: 10.4103/0378-6323.174382. [DOI] [PubMed] [Google Scholar]
- Levesque A., Lachaine J., Bissonnette R. Risk of myocardial infarction in canadian patients with psoriasis: A retrospective cohort study. J Cutan Med Surg. 2013;17:398–403. doi: 10.2310/7750.2013.13052. [DOI] [PubMed] [Google Scholar]
- Li W.Q., Han J.L., Manson J.E., Rimm E.B., Rexrode K.M., Curhan G.C. Psoriasis and risk of nonfatal cardiovascular disease in U.S. women: A cohort study. Br J Dermatol. 2012;166:811–818. doi: 10.1111/j.1365-2133.2011.10774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I.M., Ellervik C., Yazdanyar S., Jemec G.B. Meta-analysis of psoriasis, cardiovascular disease, and associated risk factors. J Am Acad Dermatol. 2013;69:1014–1024. doi: 10.1016/j.jaad.2013.06.053. [DOI] [PubMed] [Google Scholar]
- Mosca L., Barrett-Connor E., Wenger N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation. 2011;124:2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi A.A., Choi H.K., Setty A.R., Curhan G.C. Psoriasis and the risk of diabetes and hypertension: A prospective study of U. S female nurses Arch Dermatol. 2009;145:379–382. doi: 10.1001/archdermatol.2009.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Rincon I.D., Williams K., Stern M.P., Freeman G.L., Escalante A. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001;44:2737–2745. doi: 10.1002/1529-0131(200112)44:12<2737::AID-ART460>3.0.CO;2-%23. [DOI] [PubMed] [Google Scholar]
- Samarasekera E.J., Neilson J.M., Warren R.B., Parnham J., Smith C.H. Incidence of cardiovascular disease in individuals with psoriasis: A systematic review and meta-analysis. J Invest Dermatol. 2013;133:2340–2346. doi: 10.1038/jid.2013.149. [DOI] [PubMed] [Google Scholar]
- Smilowitz N.R., Gupta N., Ramakrishna H., Guo Y., Berger J.S., Bangalore S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol. 2017;2:181–187. doi: 10.1001/jamacardio.2016.4792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer D.M., Jenisch S., Suchan M., Christophers E., Weichenthal M. Increased prevalence of the metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res. 2006;298:321–328. doi: 10.1007/s00403-006-0703-z. [DOI] [PubMed] [Google Scholar]
- Wu J.J., Choi Y.M., Bebchuk J.D. Risk of myocardial infarction in psoriasis patients: A retrospective cohort study. J Dermatolog Treat. 2015;26:230–234. doi: 10.3109/09546634.2014.952609. [DOI] [PubMed] [Google Scholar]