Very infrequently, gastric melanosis and pseudomelanosis have been described.1, 2, 3, 4, 5, 6 Melanosis refers to melanin deposition, and pseudomelanosis is due to hemosiderin deposition. The etiology of these entities is poorly understood, and endoscopically, it is generally very difficult to differentiate between melanosis and pseudomelanosis. They are, likely, incidental endoscopic findings with minimal clinical significance. Gastric and duodenal pseudomelanosis manifests as speckled black pigmentation or black spots in the mucosa.
Pseudomelanosis is a rare, benign condition in which dark pigment accumulates in macrophages located in the lamina propria. There is no known association with pigmentation elsewhere in the GI tract or with the use of laxatives. Pseudomelanosis is more common in patients with hypertension, chronic renal failure, diabetes mellitus, history of upper-GI bleeding, and oral iron intake. The pigment is usually located in the lysosomes of mucosal macrophages. Histochemical studies and electron probe microanalysis suggest that several pigments may result in this endoscopic appearance, including lipomelanin, ceroid, iron sulfide, and hemosiderin.
We report a case of gastric and duodenal pseudomelanosis. Its full development was documented on serial upper endoscopies over 2 years, preceded by 18 months of a daily iron supplement, interval development of iron pill–induced mucositis at the dependent portions of the stomach, and subsequent development of diffuse mucosal pseudomelanosis within the dependent portions of the stomach (Figs. 1 and 2). Biopsy specimens from the normal-appearing stomach showed a normal pathologic appearance without iron deposits, whereas the biopsy specimens from the pigmented gastric mucosa showed iron deposits (Figure 3, Figure 4, Figure 5). The patient was not taking other prescription or over-the-counter medications that might have caused pigment deposits.
Figure 1.
Endoscopic image showing diffuse pseudomelanosis at the dependent portion of the stomach (posterior wall and greater curvature).
Figure 2.
Endoscopic image showing diffuse pseudomelanosis in the duodenum.
Figure 3.
Endoscopic image showing the relatively normal jejunum.
Figure 4.
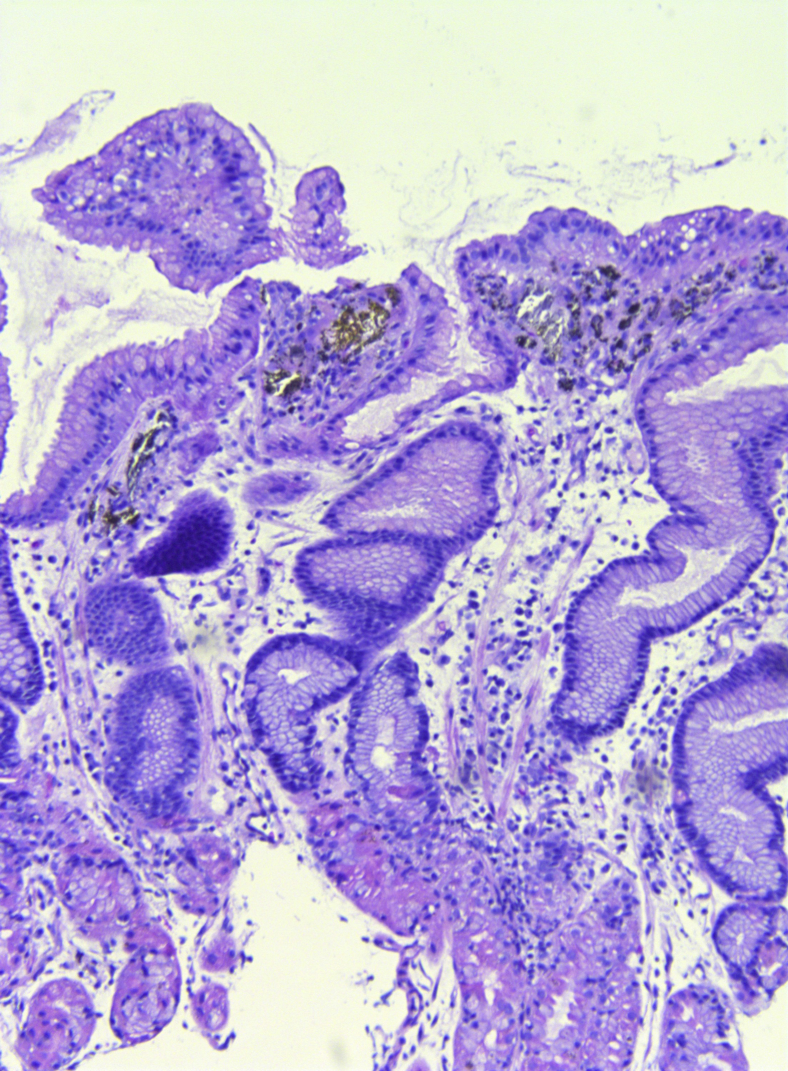
Histopathologic image demonstrating refractile pigment in the gastric lamina propria (H&E, orig. mag. ×10).
Figure 5.
Histopathologic image demonstrating iron pigment in the gastric lamina propria (iron staining, orig. mag. ×10).
We hypothesize that pill-induced mucosal injury exposes macrophages within the gastric mucosa to iron and other pigments. This generally occurs at the dependent portions of the stomach such as the posterior wall when the patient is supine and the greater curvature when the patient is standing or sitting. The duodenum is the absorptive organ for iron and other pigments. The jejunum is usually spared because of the lack of absorption by its mucosa (Video 1, available online at www.VideoGIE.org).
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Tang at sjtang2000@yahoo.com.
Supplementary data
Gastric and duodenal pseudomelanosis.
References
- 1.Tang S.J., Wu R., Bhaijee F. Gastrointestinal sarcoidosis and gastric melanosis (video) Video J and Encyclopedia of GI Endosc. 2014;2:95–98. [Google Scholar]
- 2.Tang SJ, Bhaijee F. Pseudomelanosis duodeni. Video J and Encyclopedia of GI Endosc 2013;1:272-273.
- 3.Yamase H., Norris M., Gillies C. Pseudomelanosis duodeni: a clinicopathologic entity. Gastrointest Endosc. 1985;31:83–86. doi: 10.1016/s0016-5107(85)72001-9. [DOI] [PubMed] [Google Scholar]
- 4.West B. Pseudomelanosis duodeni. J Clin Gastroenterol. 1988;10:127–129. [PubMed] [Google Scholar]
- 5.Rex D.K., Jersild R.A., Jr. Further characterization of the pigment in pseudomelanosis duodeni in three patients. Gastroenterology. 1988;95:177–182. doi: 10.1016/0016-5085(88)90308-3. [DOI] [PubMed] [Google Scholar]
- 6.Giusto D., Jakate S. Pseudomelanosis duodeni: associated with multiple clinical conditions and unpredictable iron stainability - a case series. Endoscopy. 2008;40:165–167. doi: 10.1055/s-2007-995472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Gastric and duodenal pseudomelanosis.