Abstract
Background:
Increased posterior tibial slope has been identified as a possible risk factor for injury to the anterior cruciate ligament (ACL) and has also been shown to be associated with ACL reconstruction graft failure. It is currently unknown whether increased posterior tibial slope is an additional risk factor for further injury in the context of revision ACL reconstruction.
Purpose:
To determine the relationship between posterior tibial slope and further ACL injury in patients who have already undergone revision ACL reconstruction.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A total of 330 eligible patients who had undergone revision ACL reconstruction between January 2007 and December 2015 were identified from a clinical database. The slope of the medial and lateral tibial plateaus was measured on perioperative lateral radiographs by 2 fellowship-trained orthopaedic surgeons using a digital software application. The number of subsequent ACL injuries (graft rupture or a contralateral injury to the native ACL) was determined at a minimum follow-up of 2 years (range, 2-8 years). Tibial slope measurements were compared between patients who sustained further ACL injury to either knee and those who did not.
Results:
There were 50 patients who sustained a third ACL injury: 24 of these injuries were to the knee that underwent revision ACL reconstruction, and 26 were to the contralateral knee. Medial and lateral slope values were significantly greater for the third-injury group compared with the no–third injury group (medial, 7.5° vs 6.3° [P = .01]; lateral, 13.6° vs 11.9° [P = .001]).
Conclusion:
Increased posterior tibial slope, as measured from lateral knee radiographs, was associated with increased risk of graft rupture and contralateral ACL injury after revision ACL reconstruction. This is consistent with the concept that increased posterior slope, particularly of the lateral tibial plateau, is an important risk factor for recurrent ACL injury.
Keywords: tibial slope, revision, anterior cruciate ligament, recurrent injury
With increasing numbers of anterior cruciate ligament (ACL) reconstructions being performed globally each year, the number of revision ACL reconstructions also continues to rise.19,22,23,35,38 A significant volume of literature exists evaluating ACL reconstruction outcomes following primary surgery,1,2,9,26,41 but fewer studies have focused on outcomes following revision surgery. Reports from the Multicenter ACL Revision Study and the Kaiser Permanente registry have demonstrated an incidence of 3.3% and 4.3%, respectively, for a third ACL injury in all age groups at 2 years.4,39 However, these rates are even higher in patients younger than 18 years: 15% for revision ACL reconstruction graft rupture and 12% for contralateral ACL rupture.4,39
Risk factors associated with ACL injury are broadly classified as either extrinsic or intrinsic. Extrinsic factors are considered modifiable. However, a greater challenge exists in dealing with the intrinsic factors, which relate to genetic makeup and are often much more difficult to correct, such as hypermobility, bony morphology (eg, femoral notch size), and lower limb alignment.
The role of the bony morphology of the tibia has also been studied to determine whether any association exists between an increased tibial slope and ACL injury.7,16 Biomechanically, an increased tibial slope in the presence of a compressive axial load has been shown to generate a greater anterior shear force in the tibiofemoral joint.12,15 As the ACL is the primary restraint against anterior tibial translation, an increase in posterior tibial slope will increase the load within the ACL and potentially increase the risk of ACL rupture.13 Dejour and Bonnin12 showed that in both ACL-intact and ACL-deficient knees, there was an increase of 6 mm in anterior tibial translation for every 10° of increased tibial slope.24
Despite several reports associating an increased medial or lateral posterior tibial slope with ACL injury and graft failure,7,16,30,32 the level of risk posed by this intrinsic factor in the setting of revision ACL reconstruction remains unclear. Therefore, the aim of this study was to build on previous research to determine whether there is a relationship between posterior tibial slope and further ACL injury in patients who had already undergone revision ACL reconstruction, with the hypothesis that an increased tibial slope would be associated with a greater risk of further ACL injury.
Methods
A total of 442 patients who underwent ACL revision surgery between January 2007 and December 2015 were identified from a clinical database and their cases were retrospectively reviewed. Patients were excluded if no perioperative lateral knee radiographs were available for analysis, if the available radiographs were rotated (inadequate overlap of femoral condyles) to make an assessment of tibial slope infeasible, or if patients had additional ligament surgery at the time of revision. Patients with prior contralateral ACL injury were excluded. In sum, 112 patients were excluded (n = 97, no radiographs; n = 3, unsatisfactory radiographs; n = 12, additional ligament surgery), leaving 330 patients available for the study.
Patients were followed up with at a minimum of 2 years (range, 2-8 years) to identify those who had sustained a further ACL injury to either leg. Follow-up consisted of a combination of emailed patient surveys, telephone calls, and chart review. All further ACL injuries had been confirmed by clinical examination and magnetic resonance imaging (MRI).
The perioperative lateral knee radiographs were reviewed by 1 of 2 fellowship-trained orthopaedic surgeons. Both surgeons were blinded to the injury status of the patients during radiograph assessment. Analysis was performed using InteleViewer software (Intelerad Medical Systems). The medial and lateral posterior radiographic tibial slopes were defined as 90° minus the angle between the proximal tibial anatomic axis and a tangential line drawn along each plateau.
The anatomic axis of the tibia was determined using 2 circles positioned at 5 and 15 cm distal to the tibial joint surface to the level of the outer cortex, as described in previous studies.15,17,36 A line passing through the center of these 2 circles represented the tibial anatomic axis (Figure 1). The proximal tibial anatomic axis was chosen as the reference, as it has been shown to accurately represent the mechanical axis of the tibia on short lateral knee radiographs.22
Figure 1.
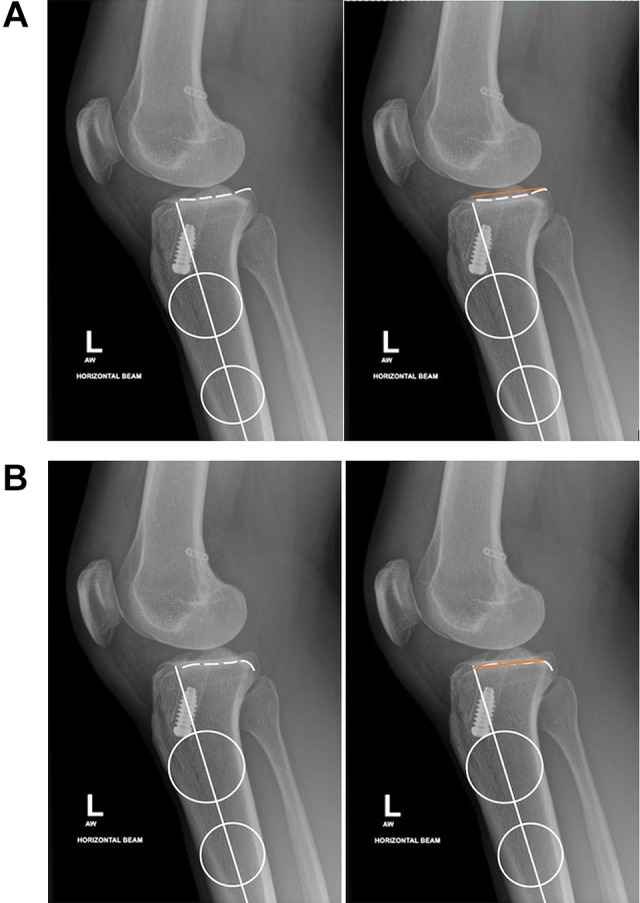
Posterior tibial slope was measured on the lateral radiograph relative to the central axis of the tibia, which was identified by applying 2 circles to the proximal tibia at 5 and 15 cm distal to the joint surface and drawing a line connecting their centers. (A) The surface of the medial tibial plateau was identified and a tangential line (orange) drawn. The angle between the tangential line and the central axis of the tibia was measured. (B) The lateral posterior tibial slope was identified and measured in a similar manner.
Independent analysis was performed on a sample of the study population (n = 40) to determine the interobserver correlation coefficient (ICC) between the reviewers. Intraobserver analysis for medial and lateral slope measurements was also calculated.
Statistical Analysis
Data were checked for normality using the Kolmogorov-Smirnov test, and posterior tibial slope values between the patients who sustained a third ACL injury and those who did not were compared using independent-samples t tests. Separate analyses were conducted for medial and lateral slope data, as well as for those in the injured group who sustained a graft rupture or contralateral ACL injury. Effect sizes were calculated using Cohen d. Tibial slope data were also divided into 3 groups according to whether the values fell below, within, or above the 50% percentile . This was done separately for the medial and lateral slope values, and all further ACL injury rates were compared between groups using chi-square analysis. All statistical analyses were performed using SPSS (v 21; IBM), and a significance level of P ≤ .05 was set.
Results
Of the eligible 330 patients, 50 (15%) had sustained a third ACL injury to either the ACL-reconstructed knee or the contralateral knee (third-injury group). The demographic data of this group and the group of 280 patients who had not sustained a further ACL injury (no third injury) are shown in Table 1.
TABLE 1.
Patient Demographics by Group: No Third Injury vs Third Injury
| No Third Injury | Third Injury | |
|---|---|---|
| n (%) | 280 (85) | 50 (15) |
| Male, % | 75 | 88 |
| Age, y, mean ± SD | 27.7 ± 2.63 | 22.9 ± 2.19 |
ICC analysis between the observers showed excellent agreement (0.88 for medial slope and 0.79 for lateral slope). Intraobserver reliability also demonstrated excellent agreement (medial slope, ICC = 0.85 [95% CI, 0.74-0.92]; lateral slope, ICC = 0.89 [95% CI, 0.82-0.93]).
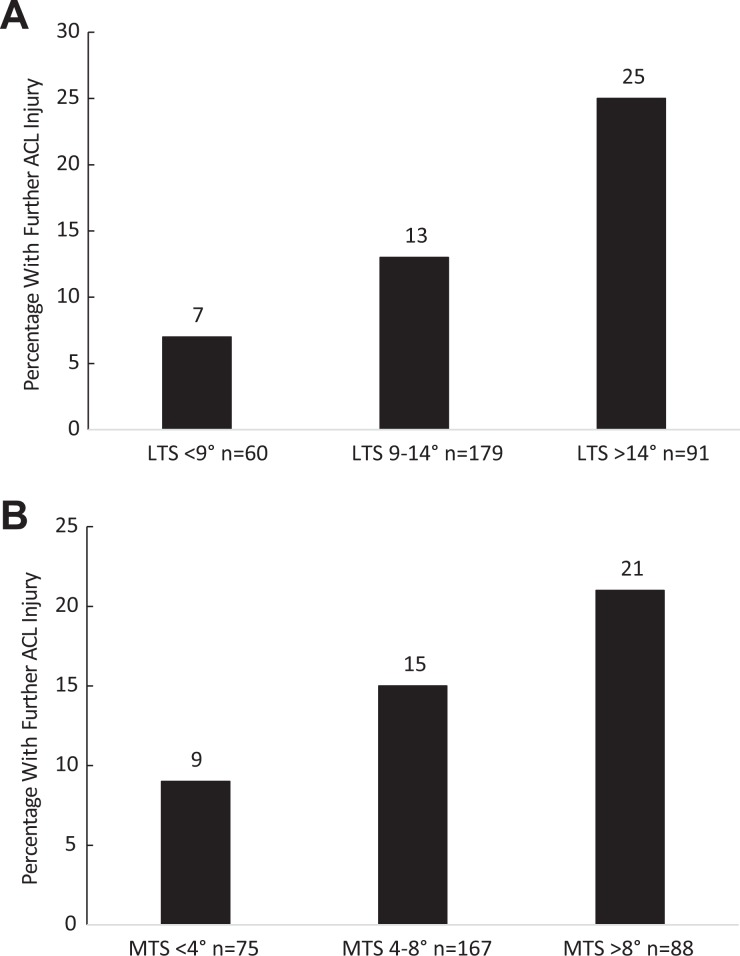
The mean medial and lateral slopes in the no–third injury group were 6.3° ± 2.7° and 11.9° ± 3.0°, respectively. The medial and lateral slopes in the third-injury group were significantly greater: medial, 7.5° ± 3.0° (P = .01; d = 0.37); lateral, 13.6° ± 3.1 (P = .001; d = 0.52) (Table 2). The incidence of further ACL injury increased with increasing tibial slope, with the difference between groups being statistically significant for the lateral slope values (P = .004) but not the medial slope values (P = .1) (Figure 2).
TABLE 2.
Medial and Lateral Tibial Slope Values Between Groups: Third Injury vs No Third Injurya
| Further ACL Injury | ||||
|---|---|---|---|---|
| No Third Injury | All | Ipsilateral (n = 24) | Contralateral (n = 26) | |
| Slope, deg, mean ± SD | ||||
| Medial | 6.3 ± 2.7 | 7.5 ± 3.0 | 7.5 ± 3.5 | 7.2 ± 2.6 |
| Lateral | 11.9 ± 3.0 | 13.6 ± 3.1 | 13.3 ± 3.0 | 13.7 ± 3.2 |
| P value (effect size) | ||||
| Medial | .01 (d = 0.37) | .03 (d = 0.40) | .09 (d = 0.35) | |
| Lateral | .001 (d = 0.52) | .04 (d = 0.44) | .005 (d = 0.57) | |
aACL, anterior cruciate ligament.
Figure 2.
Incidence of further ACL injuries with increasing (A) LTS and (B) MTS. For LTS, there was a significant difference among the 3 groups (P = .004). ACL, anterior cruciate ligament; LTS, lateral tibial slope; MTS, medial tibial slope.
Of the 50 injuries in the third injury group, 24 were to the ACL-reconstructed knee and 26 to the contralateral knee. When the analysis was repeated for each group, the group with further ACL graft injuries had significantly greater medial and lateral tibial slope values than the no–third injury group (Table 2). Patients who sustained a subsequent contralateral injury had significantly greater lateral tibial slope values than the no–third injury group.
Discussion
The main finding of this large cohort study was that patients who had a third ACL injury following previous revision ACL reconstruction had greater mean radiographic posterior tibial slope values than those who did not sustain a further ACL injury. Patients experiencing further ACL graft ruptures had significantly greater medial and lateral tibial slope values, whereas patients with a contralateral ACL injury had significantly greater lateral tibial slope values only. The results of this study support previous studies suggesting that increased posterior tibial slope is associated with both an increased risk of primary ACL injury and further ACL injury after ACL reconstruction.6,7,10,15,16,32–34,37
Previous work investigating the influence of tibial slope on primary ACL injury utilized non-ACL injury cohorts as the control group.7,16,32–34 Todd et al34 reported significantly greater medial slope (9.39° ± 2.58°) in 140 noncontact ACL-injured knees as compared with controls (8.50° ± 2.67°) (P = .003).27 Brandon et al7 also found higher medial tibial slopes in patients with ACL rupture and stated that higher medial tibial slope increased the risk of ACL injury.
Fewer studies, however, have documented the role of tibial slope on reinjury. Christensen et al10 compared ACL reconstruction cases with a graft rupture with those without graft rupture and found that regardless of graft type, lateral tibial plateau slope was a risk factor for early graft failure (mean slope, 8.4°). Webb et al37 reported the medial tibial slope to be a risk factor for graft rupture (9.9°) and contralateral ACL injury (12.9°) after primary ACL reconstruction as compared with the no–further injury group (8.5°). The current study shows a similar association following revision ACL reconstruction and suggests a stronger association of reinjury with lateral tibial slope than with medial tibial slope.
Stijak et al32 measured medial and lateral tibial slopes in ACL-deficient knees using MRI and suggested that the lateral slope may be a more significant risk factor than the medial slope. McLean et al21 suggested that in knees with a higher lateral tibial slope, greater anterior motion of the lateral compartment may occur, creating a net internal rotation of the tibia with respect to the femur, potentially increasing the ACL load.14,20,28 However, Vyas et al36 recorded medial and lateral tibial slope on lateral radiographs in a pediatric population with open physes, with and without ACL injury, and reported a greater medial tibial slope (P = .009) in the ACL-injured group but no difference in lateral slope values.
The variability within the literature for tibial slope values is likely to be due to the complex and asymmetric geometry of the plateau and to the variation in techniques for measuring slope.16,40 Brazier et al8 evaluated 6 techniques and observed differences of up to 5° among methods. They also noted that using the anterior tibial cortex as the reference line gave the highest values for posterior tibial slope, while using the posterior tibial cortex gave the lowest values. However, a subsequent study measured tibial slope from 3-dimensional-reconstructed computed tomographic models of the tibia and reported similar findings for anterior tibial cortex–referenced and posterior tibial cortex–referenced measurements.43
Lee et al18 demonstrated increased tibial slope with lateral radiographs as compared with sagittal plane MRI, and these differences were more significant on the lateral side. Sagittal MRI measurements present difficulties in consistently determining the long axis of the tibia.5 Results vary in the literature for tibial slope based on MRI, even among studies using the same methodology (as originally described by Hashemi et al16).5,29,33 As yet, there is no consensus regarding the best method for measuring tibial slope. The technique in the current study used the proximal tibial anatomic axis as the reference axis, as it has been shown to accurately represent the mechanical axis of the tibia when short lateral knee radiographs are used.42 The high interobserver correlation for medial and lateral measurements in this study supported the choice of this method.
The absolute difference in tibial slope values between the injured and uninjured groups in the current study was small, despite the statistical significance and with considerable overlap between the groups. As such, using the tibial slope to identify individual patients as being at risk would be a challenge. Furthermore, and from a practical point of view, how to use information about tibial slope remains to be determined. Proximal tibial slope–altering osteotomies are not without risk. A French study of 5 patients undergoing combined tibial deflexion osteotomy with re-revision ACL reconstruction reported a mean tibial slope of 9.2° postoperatively versus 13.6° preoperatively.31 The authors reported good outcomes in all patients, with no reinjuries at a minimum 2-year follow-up, but noted that the functional results remained less favorable than primary ACL reconstruction and with greater potential morbidity. Dejour et al11 reported satisfactory results (mean, 4-year follow-up) of 9 retrospectively reviewed patients who underwent revision ACL reconstruction combined with a tibial deflexion osteotomy distal to the patellar tendon insertion.
Limitations of this study include its being a retrospective analysis, even though data were collected prospectively, and the recognized difficulties of measuring tibial slope from radiographs.5,16 Although challenges exist with all imaging modalities, lateral radiographs are readily available in clinical practice and without the expense of MRI or the radiation exposure of computed tomography scanning. Data regarding previous meniscal injury or debridement were unavailable, but the posterior horn of the medial meniscus is recognized as an important secondary stabilizer against anterior tibial translation and ACL reconstruction failure.25,39 An assumption was also made that tibial slope is comparable in both knees. Assessment of knee hyperextension was beyond the scope of this study but may play a significant biomechanical role, as it could accentuate the influence of the tibial slope.33 Patients within the third-injury group were younger than those in the no–third injury group. Age is a recognized risk factor for ACL reinjury,1,2,38 but it is unclear whether this age risk represents a surrogate for other risk factors, such as returning to higher activity levels or high-risk sports.3,9,38
Conclusion
An increased posterior tibial slope was associated with further ACL injuries in patients who had already undergone revision ACL reconstruction. The reasons for recurrent injury are multifactorial, but the data presented here support the concept that there may be an intrinsic predisposition related to increased posterior tibial slope. Measuring the medial and lateral posterior tibial slope on lateral radiographs of the knee is a simple and inexpensive screening tool that can be used as an additional source of information when assessing a patient’s overall risk profile for reinjury. Identifying “at-risk” patients may allow for better counseling and management of expectations regarding contralateral injury. However, whether there is a role for correction of increased tibial slope remains to be determined.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Science, Health and Engineering College Human Ethics Sub-committee of La Trobe University.
References
- 1. Andernord D, Desai N, Bjornsson H, Gillen S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction: a cohort study of 9061 patients with 5-year follow-up. Am J Sports Med. 2015;43(2):295–302. [DOI] [PubMed] [Google Scholar]
- 2. Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43(1):121–127. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. [DOI] [PubMed] [Google Scholar]
- 4. Arianjam A, Inacio MCS, Funahashi TT, Maletis GB. Analysis of 2019 patients undergoing revision anterior cruciate ligament reconstruction from a community-based registry. Am J Sports Med. 2017;45(7):1574–1580. [DOI] [PubMed] [Google Scholar]
- 5. Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case- control study. Arthroscopy. 2010;26(7):901–906. [DOI] [PubMed] [Google Scholar]
- 6. Boden BP, Breit I, Sheehan FT. Tibiofemoral alignment: contributing factors to noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2009;91(10):2381–2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22(8):894–899. [DOI] [PubMed] [Google Scholar]
- 8. Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. Evaluation of methods for radiographic measurement of the tibial slope: a study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200. [PubMed] [Google Scholar]
- 9. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. [DOI] [PubMed] [Google Scholar]
- 11. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–2852. [DOI] [PubMed] [Google Scholar]
- 12. Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–749. [PubMed] [Google Scholar]
- 13. Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):134–145. [DOI] [PubMed] [Google Scholar]
- 14. Fleming BC, Renstrom PA, Beynnon BD, et al. The effect of weight bearing and external loading on anterior cruciate ligament strain. J Biomech. 2001;34(2):163–170. [DOI] [PubMed] [Google Scholar]
- 15. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–382. [DOI] [PubMed] [Google Scholar]
- 16. Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kamath GV, Murphy T, Creighton RA, Viradia N, Taft TN, Spang JT. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. [DOI] [PubMed] [Google Scholar]
- 18. Lee YS, Kim JG, Lim HC, et al. The relationship between tibial slope and meniscal insertion. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1416–1420. [DOI] [PubMed] [Google Scholar]
- 19. Lynch TS, Parker RD, Patel RM, et al. The impact of the Multicenter Orthopaedic Outcomes Network (MOON) research on anterior cruciate ligament reconstruction and orthopaedic practice. J Am Acad Orthop Surg. 2015;23(3):154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GAM, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. [DOI] [PubMed] [Google Scholar]
- 21. McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech. 2010;25(8):781–788. [DOI] [PubMed] [Google Scholar]
- 22. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44:384–392. [DOI] [PubMed] [Google Scholar]
- 23. Noyes FR, Barber-Westin SD. Revision anterior cruciate ligament surgery: experience from Cincinnati. Clin Orthop Relat Res. 1996;325:116–129. [DOI] [PubMed] [Google Scholar]
- 24. Pauzenberger L, Syre S, Shurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–1721. [DOI] [PubMed] [Google Scholar]
- 25. Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. [DOI] [PubMed] [Google Scholar]
- 26. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285–291. [DOI] [PubMed] [Google Scholar]
- 27. Rambaud AJ, Semay B, Samozino P, et al. Criteria for return to sport after anterior cruciate ligament reconstruction with lower reinjury risk (CR’STAL study): protocol for a prospective observational study in France. BMJ Open. 2017;7(6):e015087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shimokochi Y, Shultz SJ. Mechanisms of noncontact anterior cruciate ligament injury. J Athl Train. 2008;43(4):396–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sonnery-Cottet B, Archbold P, Cucurulo T, et al. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg Br. 2011;93(11):1475–1478. [DOI] [PubMed] [Google Scholar]
- 31. Sonnery-Cottet B, Mogos S, Thaunat M, et al. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(8):1873–1880. [DOI] [PubMed] [Google Scholar]
- 32. Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):112–117. [DOI] [PubMed] [Google Scholar]
- 33. Terauchi M, Hatayama K, Yanagisawa S, Saito K, Takagishi K. Sagittal alignment of the knee and its relationship to noncontact anterior cruciate ligament injuries. Am J Sports Med. 2011;39(5):1090–1094. [DOI] [PubMed] [Google Scholar]
- 34. Todd MS, Lalliss S, Garcia ES, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63–67. [DOI] [PubMed] [Google Scholar]
- 35. Uribe JW, Hechtman KS, Zvijac JE, Tjin-A-Tsoi EW. Revision anterior cruciate ligament surgery: experience from Miami. Clin Orthop Relat Res. 1996;325:91–99. [DOI] [PubMed] [Google Scholar]
- 36. Vyas S, van Eck CF, Vyas N, Fu FH, Otsuka NY. Increased medial tibial slope in teenage pediatric population with open physes and anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):372–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 38. Webster KE, Feller JA. Exploring the high re-injury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 39. Webster KE, Feller JA, Kimp AJ, Whitehead TS. Revision anterior cruciate ligament reconstruction outcomes in younger patients: medial meniscal pathology and high rates of return to sport are associated with third ACL injuries. Am J Sports Med. 2018;46(5):1137–1142. [DOI] [PubMed] [Google Scholar]
- 40. Wordeman SC, Quatman CE, Kaeding CC, Hewett TE. In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med. 2012;40(7):1673–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty. 2008;23(4):586–592. [DOI] [PubMed] [Google Scholar]
- 43. Zhang Y, Wang J, Xiao J, et al. Measurement and comparison of tibial posterior slope angle in different methods based on three-dimensional reconstruction. Knee. 2014;21(3):694–698. [DOI] [PubMed] [Google Scholar]