Abstract
Objective:
During the past decade, the availability of health information online has increased dramatically. We assessed progress toward the Healthy People 2020 (HP2020) health communication and health information technology objective of increasing the proportion of health information seekers who easily access health information online.
Methods:
We used data from 4 administrations of the Health Information National Trends Survey (HINTS 2008-2017) (N = 18 103). We conducted multivariable logistic regression analysis to evaluate trends over time in experiences with accessing health information and to examine differences by sociodemographic variables (sex, age, race/ethnicity, education, income, metropolitan status) separately for those who used the internet (vs other information sources) during their most recent search for health information.
Results:
Among US adults who looked for health information and used the internet for their most recent search, the percentage who reported accessing health information without frustration was stable during the study period (from 37.2% in 2008 to 38.5% in 2017). Accessing information online without frustration was significantly and independently associated with age 35-49 (vs age 18-34) (odds ratio [OR] = 1.34; 95% confidence interval [CI], 1.03 -1.73), non-Hispanic black (vs non-Hispanic white) race/ethnicity (OR = 2.15; 95% CI, 1.55-2.97), and annual household income <$20 000 (vs >$75 000) (OR = 0.66; 95% CI, 0.47-0.93). The percentage of adults who used an information source other than the internet and reported accessing health information online without frustration ranged from 31.3% in 2008 to 42.7% in 2017. Survey year 2017 (vs 2008) (OR = 1.61; 95% CI, 1.09-2.35) and high school graduate education (vs college graduate) (OR = 0.69; 95% CI, 0.49-0.97) were significantly and independently associated with accessing health information without frustration from sources other than the internet.
Conclusions:
The percentage of online health information seekers reporting easily accessing health information did not meet the HP2020 objective. Continued efforts are needed to enable easy access to online health information among diverse populations.
Keywords: health communication, Healthy People programs, frustration, access to information, internet
Large amounts of health information can now be accessed online,1-3 and patients and caregivers are particularly likely to seek health information online.4-7 The ability to easily seek and obtain health information online is becoming an increasingly important component of health and disease management.2,4,5,8,9 However, the experience of searching for health information online may differ by sociodemographic group.3,10,11 For example, in studies published during the last decade, persons who reported greater difficulty in seeking health information online were more likely to be from socially disadvantaged groups, including racial/ethnic minority groups, older adults, those with lower incomes, and persons living in rural areas; more likely to report negative perceptions about health care; and more likely to be misinformed about cancer prevention than those from relatively advantaged groups.8,11,12
In general, the benefits of health information seeking include enhanced patient involvement in and satisfaction with medical decision-making, improved communication with informal care providers, and improvements in quality of life.13-15 As health care moves toward a patient-centered delivery model, seeking and accessing health information online can help patients become informed consumers of health care. Recognizing the importance of having access to health information, the US Department of Health and Human Services’ Healthy People 2020 (HP2020) initiative developed objectives focused on health communication and health information technology (HC/HIT).16,17 HC/HIT, which has been a topic area with associated objectives since 2010, emphasizes patient-centered communication and electronic communication.16,17 HP2020 added an objective to increase the proportion of information seekers who report easily accessing health information online to 45.0% by 2020, from the baseline of 40.9% reported in 2008 by the National Cancer Institute’s Health Information National Trends Survey (HINTS).16,18-20
Examining trends and disparities in experiences with seeking health information online can provide insight into methods for reducing health inequities stemming from the digital divide and may facilitate patient-centered care and decision-making. To assess population-level changes in persons’ perceptions about their experiences with seeking health information, we used data from HINTS, a nationally representative, cross-sectional survey administered by the National Cancer Institute that tracks access to and use of health information among adults aged ≥18. The HINTS program provides data to the US Department of Health and Human Services’ Office of Disease Prevention and Health Promotion to track several HP2020 HC/HIT objectives.20 The objectives of this study were to (1) track experiences with seeking health information online over time among US adults and (2) examine differences in information-seeking experiences by sociodemographic characteristics.
Methods
Survey Population and Data Collection
We used data from HINTS on the population need for, access to, and use of health information.17 We integrated data from 4 administrations of HINTS collected from January 2008 through 2017 (N = 18 103) (Table 1). Each HINTS administration was reviewed and approved by the Westat Institutional Review Board and subsequently deemed exempt by the US National Institutes of Health Office of Human Subjects Research Protections. Details about survey design and implementation are available elsewhere.22-25
Table 1.
Sample design and response rates among adults aged ≥18 in the Health Information National Trends Survey (HINTS), 2008-2017 (N = 18 103), United Statesa
| Variable | HINTS 3 | HINTS 4 | HINTS 5, Cycle 1 | |
|---|---|---|---|---|
| Cycle 1 | Cycle 3 | |||
| Survey mode | Postal mail and random-digit dial | Postal mail | Postal mail | Postal mail |
| Data collection period | January 7–April 27, 2008 | October 25, 2011–February 21, 2012 | September 6–December 30, 2013 | January 25–May 5, 2017 |
| Sample size, no. | Postal mail, 3582; random-digit dial, 4092 | 3959 | 3185 | 3285 |
| Response rate | Postal mail, 40.0%; random-digit dial, 24.2% | 36.7% | 35.2% | 32.4% |
Measures
The metric HP2020 used to track progress toward the HC/HIT-9 objective (ie, increase the proportion of health information seekers who report easily accessing health information online) is derived from the following HINTS item: “Based on the results of your most recent search for information about health or medical topics, how much do you agree or disagree with the following statement? You felt frustrated during your search for the information.” Response options were measured on a 4-point scale (1-4), where 1 = strongly disagree and 4 = strongly agree. HP2020 tracks the percentage of the population who strongly disagree that they felt frustrated during their last search for information about health or medical topics. Therefore, strong disagreement with the statement “You felt frustrated during your search for the information” serves as a proxy for ease of health information seeking, per the HP2020 objective. The denominator for the HP2020 metric for this objective includes only HINTS respondents who reported that they had ever searched for health or medical information from any source and who used the internet first during their last search. All HINTS respondents were asked, “Have you ever looked for information about health or medical topics from any source?” Those who responded yes were asked, “The most recent time you looked for information about health or medical topics, where did you go first?” Response options for this item included various information sources (eg, books, brochures, cancer organizations, family, friend, coworker, physician or health care provider, internet, library, magazines, newspapers, telephone information line, or unconventional practitioner).
Statistical Analysis
We used full-sample and replicate weights to account for the complex sampling design and to derive valid population-level estimates. We conducted all analyses using SUDAAN version 11.0.126 and SAS/STAT version 9.4.27 We restricted analyses to respondents who had ever searched for health or medical information (N = 13 907). We conducted descriptive analyses for respondent characteristics by survey year and overall. We also cross-tabulated sociodemographic characteristics and health information source (internet vs other sources) with ratings of health information-seeking experience by using the Wald χ2 test of significance for categorical variables, with P < .05 considered significant.
We conducted 2 logistic regression analyses to assess the independent associations of survey year and sociodemographic characteristics with ratings of health information-seeking experience. In Model 1, we restricted our sample to respondents who used the internet during their most recent search for health or medical information to capture the appropriate denominator for tracking the HP2020 objective (n = 6794). In Model 2, we restricted our sample to respondents who used sources of information other than the internet (n = 4808) as a comparison group. We also calculated the percentage of the population indicating easily accessing health information by survey year, stratifying by source of health information (internet vs other) and controlling for sociodemographic characteristics. We included the following sociodemographic characteristics in each model: sex (male, female); age (18-34, 35-49, 50-64, 65-74, ≥75); race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic other [ie, all race categories and subcategories for American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander]); education (<high school graduate, high school graduate, some college, college graduate); annual household income (<$20 000, $20 000-$34 999, $35 000-$49 999, $50 000-$74 999, ≥$75 000); and geographic location (metropolitan vs non-metropolitan) using the US Department of Agriculture’s 2013 Rural–Urban Continuum codes, which distinguish metropolitan areas (≥20 000 population) from non-metropolitan areas (<20 000 population).28 Lastly, we tested polynomial trends across each of the 4 HINTS data administrations for easily accessing health information online and for other sources.
Results
Sociodemographic Characteristics
In each survey year, the majority of the population (range, 69.8%-81.5%) had ever searched for health or medical information, and 68.9% (95% confidence interval [CI], 67.8%-70.1%) across survey years reported using the internet first during their most recent search for health information (Table 2). Across survey years, most of the population who had ever sought health or medical information were female, younger than 50, and non-Hispanic white; had at least some college education and an annual household income ≥$50 000; and resided in a metropolitan area.
Table 2.
Characteristics of adults aged ≥18 who searched for health or medical information, by survey year and overall,a Health Information National Trends Survey (HINTS), 2008-2017, United Statesb
| Characteristics | HINTS 3, January 7–April 27, 2008 (n = 5625) | HINTS 4 | HINTS 5, Cycle 1: January 25–May 5, 2017 (n = 2593) | Total (n = 13 907) | |
|---|---|---|---|---|---|
| Cycle 1: October 25, 2011–February 21, 2012 (n = 3181) | Cycle 3: September 6–December 30, 2013 (n = 2508) | ||||
| Sex | |||||
| Female | 55.8 (54.5-57.0) | 54.4 (52.9-56.0) | 53.8 (52.0-55.6) | 52.0 (50.6-53.4) | 53.9 (53.2-54.6) |
| Age, y | |||||
| 18-34 | 28.6 (27.4-29.9) | 29.8 (27.7-32.0) | 26.7 (24.3-29.2) | 22.5 (18.9-26.2) | 26.8 (25.5-28.1) |
| 35-49 | 31.5 (30.4-32.6) | 28.9 (27.7-30.1) | 29.9 (27.9-31.9) | 28.7 (24.8-32.7) | 29.7 (28.4-30.9) |
| 50-64 | 25.2 (24.4-26.1) | 25.7 (24.6-26.8) | 26.5 (25.0-28.0) | 30.4 (28.5-32.3) | 27.1 (26.3-27.8) |
| 65-74 | 8.1 (7.6-8.5) | 9.1 (8.5-9.8) | 9.6 (9.0-10.2) | 11.3 (10.6-12.0) | 9.6 (9.3-9.9) |
| ≥75 | 6.6 (6.1-7.1) | 6.4 (5.9-7.0) | 7.2 (6.4-8.1) | 7.0 (6.3-7.7) | 6.8 (6.5-7.2) |
| Race/ethnicity | |||||
| Hispanic | 9.1 (8.2-10.1) | 13.4 (12.4-14.5) | 13.5 (12.2-14.7) | 14.6 (13.5-15.8) | 12.8 (12.3-13.3) |
| Non-Hispanic white | 74.1 (73.0-75.3) | 69.6 (67.9-71.3) | 69.0 (67.3-70.6) | 68.8 (67.3-70.2) | 70.2 (69.5-70.9) |
| Non-Hispanic black | 10.4 (9.6-11.2) | 10.4 (9.2-11.6) | 10.3 (9.2-11.3) | 8.6 (7.4-9.8) | 9.9 (9.3-10.4) |
| Non-Hispanic otherc | 6.4 (5.7-7.0) | 6.6 (5.7-7.5) | 7.3 (6.2-8.4) | 8.0 (7.0-9.0) | 7.1 (6.6-7.6) |
| Education | |||||
| <High school graduate | 8.2 (7.3-9.2) | 9.7 (8.3-11.1) | 7.8 (6.3-9.2) | 5.8 (4.0-7.5) | 7.8 (7.1-8.6) |
| High school graduate | 21.9 (20.5-23.3) | 19.5 (17.6-21.4) | 20.1 (17.7-22.6) | 19.8 (17.7-21.8) | 20.2 (19.2-21.3) |
| Some college | 38.9 (37.6-40.3) | 33.1 (31.2-35.0) | 33.5 (31.4-35.6) | 34.3 (32.3-36.4) | 34.8 (33.9-35.7) |
| College graduate | 30.9 (30.1-31.8) | 37.7 (36.7-38.8) | 38.6 (37.0-40.2) | 40.1 (38.7-41.6) | 37.1 (36.5-37.8) |
| Annual household income, $ | |||||
| <20 000 | 16.0 (14.0-18.0) | 21.3 (18.7-23.8) | 17.8 (15.6-20.0) | 13.9 (11.6-16.3) | 17.3 (16.2-18.4) |
| 20 000-34 999 | 14.2 (12.4-16.0) | 16.0 (13.3-18.8) | 12.5 (10.3-14.7) | 12.2 (9.6-14.8) | 13.7 (12.5-14.9) |
| 35 000-49 999 | 14.1 (12.3-15.9) | 12.8 (10.9-14.6) | 14.3 (11.6-17.1) | 15.1 (12.4-17.7) | 14.1 (12.9-15.3) |
| 50 000-74 999 | 20.5 (18.8-22.3) | 18.1 (15.8-20.4) | 19.1 (16.7-21.6) | 19.2 (17.1-21.3) | 19.2 (18.0-20.3) |
| ≥75 000 | 35.2 (33.3-37.0) | 31.8 (29.4-34.2) | 36.2 (33.6-38.8) | 39.6 (36.9-42.3) | 35.7 (34.6-36.9) |
| Metropolitan statusd | |||||
| Metropolitan | 83.4 (81.8-85.0) | 84.4 (82.4-86.4) | 83.8 (81.8-85.9) | 85.9 (83.8-87.9) | 84.4 (83.4-85.4) |
| Non-metropolitan | 16.6 (15.0-18.2) | 15.6 (13.6-17.6) | 16.2 (14.1-18.2) | 14.1 (12.1-16.2) | 15.6 (14.6-16.6) |
| Used internet first in most recent health information search | |||||
| Yes | 61.2 (59.7-62.7) | 69.6 (67.6-71.7) | 69.4 (66.2-72.5) | 74.9 (72.1-77.7) | 68.9 (67.8-70.1) |
a Includes all adults who searched for health information regardless of information source (online or other). All values are percentage (95% confidence interval).
b Data sources: HINTS 3, HINTS 4 (Cycles 1 and 3), and HINTS 5 (Cycle 1). National Institutes of Health, National Cancer Institute.20
c Includes all race categories and subcategories for American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander among respondents indicating they were non-Hispanic.
d Geographic location (metropolitan vs nonmetropolitan) was defined using the US Department of Agriculture’s 2013 Rural–Urban Continuum Codes, which distinguish metropolitan counties and nonmetropolitan counties.28
Health Information-Seeking Experience
The percentage of the population who accessed health information without frustration was similar across survey years (range, 36.1%-38.5%) (Table 3). Of the population who used the internet first for their most recent search, the percentage who accessed health information without frustration was 40.9% in 2008 and 38.4% in 2017. Of health information seekers who used a source other than the internet during their most recent search, the percentage of the population who accessed health information without frustration ranged from 31.3% in 2008 to 42.7% in 2017 (Table 3). During each survey year, the internet was the most frequently used source of health information; the percentage of the population who used the internet first for their most recent search ranged from 61.2% in 2008 to 74.4% in 2017 (Table 2). The second most frequently named source of health information in each survey administration was physician or health care provider (range, 13.9% in 2008 to 13.3% in 2017).
Table 3.
Weighted, unadjusted estimates of adults aged ≥18 who searched for health or medical information and reported accessing health information without frustration,a by sociodemographic characteristics, overall and by survey year, Health Information National Trends Survey (HINTS), 2008-2017, United Statesb
| Characteristics | HINTS 3, January 7–April 27, 2008 (n = 5625) | HINTS 4 | HINTS 5, Cycle 1: January 25–May 5, 2017 (n = 2593) | Total (N = 13 907) | |
|---|---|---|---|---|---|
| Cycle 1: October 25, 2011–February 21, 2012 (n = 3181) | Cycle 3: September 6–December 30, 2013 (n = 2508) | ||||
| Accessed health information without frustration, % | 37.2 (35.3-39.2) | 36.1 (33.0-39.1) | 37.8 (34.3-41.3) | 38.5 (35.0-41.9) | 37.4 (35.9-38.9) |
| Used internet first in most recent health information search | |||||
| Yes | 40.9 (38.4-43.3) | 38.4 (34.2-42.6) | 40.3 (35.4-45.1) | 38.4 (33.9-42.9) | 39.4 (37.3-41.5) |
| No | 31.3 (28.6-34.1) | 35.8 (31.0-40.6) | 36.5 (30.4-42.6) | 42.7 (35.5-49.9) | 36.1 (33.6-38.6) |
| P valuec | <.001 | .40 | .33 | .32 | .047 |
| Sex | |||||
| Female | 37.4 (35.1-39.6) | 36.7 (33.0-40.4) | 38.4 (33.7-43.2) | 41.0 (36.8-45.1) | 38.4 (36.5-40.3) |
| Male | 37.3 (33.8-40.7) | 35.6 (30.3-40.9) | 37.5 (32.7-42.2) | 36.0 (30.3-41.7) | 36.5 (34.1-39.0) |
| P valuec | .97 | .74 | .76 | .16 | .23 |
| Age, y | |||||
| 18-34 | 40.4 (35.4-45.4) | 33.7 (27.2-40.3) | 35.6 (26.0-45.2) | 32.8 (23.3-42.3) | 35.5 (31.7-39.4) |
| 35-49 | 38.1 (34.9-41.2) | 40.1 (34.7-45.5) | 38.7 (31.2-46.1) | 44.6 (37.8-51.3) | 40.4 (37.4-43.4) |
| 50-64 | 34.6 (31.8-37.3) | 36.4 (33.1-39.6) | 37.6 (33.6-41.6) | 40.0 (35.5-44.5) | 37.4 (35.5-39.3) |
| 65-74 | 34.4 (30.6-38.1) | 35.9 (29.7-42.0) | 41.0 (34.4-47.5) | 32.8 (26.5-39.1) | 35.8 (32.8-38.9) |
| ≥75 | 34.2 (28.9-39.6) | 30.3 (23.4-37.1) | 41.3 (30.3-52.3) | 36.4 (28.0-44.8) | 35.7 (31.5-39.9) |
| P valuec | .06 | .28 | .90 | .12 | .19 |
| Race/ethnicity | |||||
| Hispanic | 32.3 (25.5-39.1) | 32.4 (22.2-42.6) | 36.8 (27.6-46.1) | 41.0 (31.7-50.2) | 36.2 (31.5-40.9) |
| Non-Hispanic white | 37.8 (35.4-40.2) | 35.8 (32.3-39.2) | 38.5 (34.1-42.9) | 37.1 (32.7-41.5) | 37.2 (35.4-39.1) |
| Non-Hispanic black | 42.1 (35.1-49.2) | 51.3 (40.4-62.3) | 41.1 (31.1-51.0) | 51.3 (41.0-61.5) | 46.6 (41.7-51.4) |
| Non-Hispanic otherd | 34.9 (25.3-44.6) | 29.1 (20.6-37.7) | 37.3 (25.4-49.2) | 30.2 (20.2-40.2) | 32.6 (27.6-37.6) |
| P valuec | .20 | .04 | .90 | .048 | .001 |
| Education | |||||
| <High school graduate | 27.5 (17.5-37.5) | 26.4 (14.3-38.5) | 38.2 (25.8-50.6) | 38.2 (21.1-55.3) | 31.9 (25.5-38.3) |
| High school graduate | 37.1 (32.3-41.9) | 31.0 (25.0-36.9) | 34.5 (25.9-43.1) | 40.3 (32.4-48.2) | 35.7 (32.2-39.2) |
| Some college | 37.2 (34.0-40.4) | 37.8 (32.1-43.4) | 37.9 (30.4-45.5) | 40.4 (33.0-47.7) | 38.4 (35.3-41.4) |
| College graduate | 40.3 (38.0-42.6) | 39.1 (34.6-43.5) | 39.5 (35.0-44.1) | 36.4 (31.8-41.0) | 38.6 (36.5-40.8) |
| P valuec | .03 | .11 | .81 | .74 | .18 |
| Annual household income, $ | |||||
| <20 000 | 31.0 (24.6-37.4) | 26.5 (20.6-32.3) | 37.8 (28.3-47.4) | 35.5 (25.4-45.6) | 32.2 (28.2-36.2) |
| 20 000-34 999 | 31.6 (25.6-37.6) | 38.3 (29.6-46.9) | 31.8 (24.9-38.6) | 36.7 (26.9-46.4) | 35.0 (30.9-39.0) |
| 35 000-49 999 | 36.6 (31.2-42.1) | 37.6 (31.5-43.7) | 39.4 (28.6-50.2) | 43.9 (29.9-57.9) | 39.7 (34.5-44.9) |
| 50 000-74 999 | 37.0 (32.1-41.8) | 36.2 (27.4-45.1) | 36.5 (28.3-44.7) | 37.0 (30.6-43.4) | 36.7 (33.1-40.3) |
| ≥75 000 | 42.7 (39.7-45.8) | 39.7 (34.6-44.8) | 41.3 (35.9-46.7) | 40.3 (36.0-44.6) | 40.9 (38.6-43.2) |
| P valuec | .001 | .02 | .40 | .76 | .001 |
| Metropolitan statuse | |||||
| Metropolitan | 37.6 (35.4-39.8) | 36.7 (33.4-40.1) | 38.5 (34.8-42.2) | 39.0 (35.5-42.5) | 38.0 (36.3-39.6) |
| Non-metropolitan | 35.6 (31.4-39.8) | 32.8 (25.7-39.9) | 34.6 (25.7-43.4) | 35.2 (27.1-43.3) | 34.5 (30.9-38.1) |
| P valuec | .43 | .31 | .41 | .35 | .08 |
a Accessing health information without frustration is defined as responding “strongly disagree” to the question: “Based on the results of your most recent search for information about health or medical topics, how much do you agree or disagree with the following statement? You felt frustrated during your search for the information.” Response options were measured on a 4-point scale, ranging from 1 = strongly disagree to 4 = strongly agree. All values are percentage (95% confidence interval), unless otherwise indicated.
b Data sources: HINTS 3, HINTS 4 (Cycles 1 and 3), and HINTS 5 (Cycle 1). National Institutes of Health, National Cancer Institute.20
c Using the Wald χ2 test of significance for categorical variables, with P < .05 considered significant.
d Includes all race categories and subcategories for American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander among respondents indicating they were non-Hispanic.
e Geographic location (metropolitan vs nonmetropolitan) was defined using the US Department of Agriculture’s 2013 Rural–Urban Continuum Codes, which distinguish metropolitan counties and nonmetropolitan counties.28
In bivariate analyses, we found no significant differences in population estimates by sex, age, education, or geographic location in a metropolitan or non-metropolitan area. However, we found significant differences by race/ethnicity, income, and use of internet during the most recent search, where a higher percentage of non-Hispanic black persons (vs other racial/ethnic groups), adults with annual household incomes ≥$75 000 (compared with persons with lower incomes), and persons who used the internet (vs other sources) for their most recent health information search reported accessing health information online without frustration.
Health Information-Seeking Experience by Source
In Model 1, among the population who used the internet first during their most recent search for health information (n = 6794), age, race/ethnicity, and income were significantly and independently associated with accessing health information without frustration (Table 4). The population aged 35-49 was significantly more likely than the population aged 18-34 to access health information without frustration (OR = 1.34; 95% CI, 1.03 -1.73). The non-Hispanic black population was more likely than the non-Hispanic white population to access health information without frustration (OR = 2.15; 95% CI, 1.55-2.97). The population with an annual household income <$75 000 was less likely than the population with an annual household income ≥$75 000 to access health information without frustration.
Table 4.
Weighted, fully adjusted estimates of adults aged ≥18 who searched for health or medical information who reported accessing health information without frustration,a by sociodemographic characteristics and survey year, stratified by source of recent search for health information, Health Information National Trends Survey (HINTS), 2008-2017, United Statesb
| Variable | Model 1: Used the Internet First for Most Recent Search (n = 6794) | Model 2: Used a Source Other Than Internet for Most Recent Search (n = 4808) | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | P Valuec | Odds Ratio (95% CI) | P Valuec | |
| Overall | 0.53 (0.42-0.67) | 0.82 (0.54-1.24) | ||
| Survey data collection period | ||||
| 2008 | 1.00 [Reference] | 1.00 [Reference] | ||
| 2011-2012 | 0.93 (0.74-1.16) | .50 | 1.35 (1.04-1.74) | .02 |
| 2013 | 1.03 (0.79-1.33) | .83 | 1.20 (0.85-1.67) | .31 |
| 2017 | 0.91 (0.75-1.11) | .36 | 1.61 (1.09-2.35) | .02 |
| Sex | ||||
| Female | 1.15 (0.96-1.38) | .13 | 1.03 (0.78-1.35) | .86 |
| Male | 1.00 [Reference] | 1.00 [Reference] | ||
| Age, y | ||||
| 18-34 | 1.00 [Reference] | 1.00 [Reference] | ||
| 35-49 | 1.34 (1.03-1.73) | .03 | 0.74 (0.48-1.14) | .17 |
| 50-64 | 1.12 (0.90-1.39) | .30 | 0.75 (0.47-1.14) | .17 |
| 65-74 | 1.22 (0.89-1.67) | .21 | 0.70 (0.45-1.08) | .10 |
| ≥75 | 1.48 (0.97-2.65) | .07 | 0.99 (0.62-1.57) | .95 |
| Race/ethnicity | ||||
| Hispanic | 1.16 (0.87-1.54) | .32 | 0.96 (0.63-1.44) | .83 |
| Non-Hispanic white | 1.00 [Reference] | 1.00 [Reference] | ||
| Non-Hispanic black | 2.15 (1.55-2.97) | .001 | 1.17 (0.78-1.73) | .45 |
| Non-Hispanic otherd | 0.92 (0.66-1.28) | .63 | 0.65 (0.39-1.11) | .11 |
| Education | ||||
| <High school graduate | 1.18 (0.65-2.15) | .58 | 0.82 (0.50-1.35) | .43 |
| High school graduate | 1.21 (0.91-1.58) | .18 | 0.69 (0.49-0.97) | .03 |
| Some college | 1.19 (0.96-1.46) | .11 | 0.81 (0.60-1.09) | .16 |
| College graduate | 1.00 [Reference] | 1.00 [Reference] | ||
| Annual household income, $ | ||||
| <20 000 | 0.66 (0.47-0.93) | .02 | 0.76 (0.50-1.14) | .18 |
| 20 000-34 999 | 0.70 (0.51-0.97) | .03 | 0.83 (0.54-1.27) | .38 |
| 35 000-49 999 | 0.87 (0.64-1.18) | .36 | 0.91 (0.62-1.33) | .61 |
| 50 000-74 999 | 0.78 (0.64-0.96) | .02 | 1.16 (0.80-1.68) | .44 |
| ≥75 000 | 1.00 [Reference] | 1.00 [Reference] | ||
| Metropolitan statuse | ||||
| Metropolitan | 1.00 [Reference] | 1.00 [Reference] | ||
| Non-metropolitan | 0.93 (0.70-1.24) | .63 | 0.75 (0.54-1.04) | .09 |
a Accessing health information without frustration is defined as responding “strongly disagree” to the question: “Based on the results of your most recent search for information about health or medical topics, how much do you agree or disagree with the following statement? You felt frustrated during your search for the information.” Response options were measured on a 4-point scale, ranging from 1 = strongly disagree to 4 = strongly agree. All values are percentage (95% confidence interval), unless otherwise indicated.
b Data sources: HINTS 3 (January 7–April 27, 2008), HINTS 4 (Cycle 1 [October 25, 2011–February 21, 2012] and Cycle 3 [September 6–December 30, 2013]), and HINTS 5, Cycle 1 (January 25–May 5, 2017). National Institutes of Health, National Cancer Institute.20
c Using the t test of significance, with P < .05 considered significant.
d Includes all race categories and subcategories for American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander among respondents indicating they were non-Hispanic.
e Geographic location (metropolitan vs nonmetropolitan) was defined using the US Department of Agriculture’s 2013 Rural–Urban Continuum Codes, which distinguish metropolitan counties and nonmetropolitan counties.28
In Model 2, among the population who used a source other than the internet during their most recent search for health information (n = 4808), survey year and education were significantly and independently associated with accessing health information without frustration (Table 4). Compared with survey year 2008, the odds of reporting accessing health information without frustration using sources other than the internet were significantly higher in 2011-2012 (OR = 1.35; 95% CI, 1.04 -1.74; P = .02) and 2017 (OR = 1.61; 95% CI, 1.09-2.35; P = .02). High school graduates were significantly less likely than college graduates to report accessing health information without frustration from sources other than the internet (OR = 0.69; 95% CI, 0.49-0.97; P = .03).
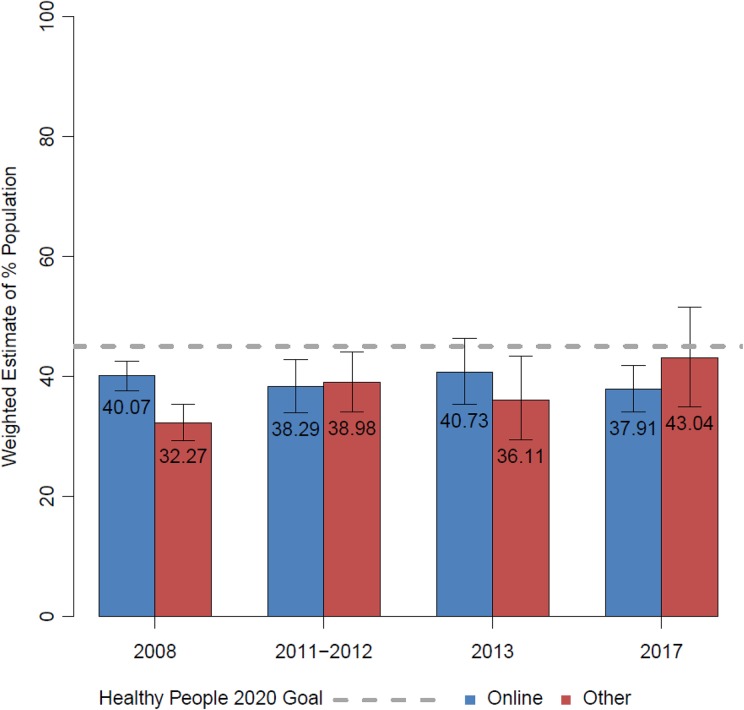
Consistent with findings from the logistic regression analyses, we found no significant changes over time in the percentage of online information seekers who reported accessing health information without frustration. However, we found a significant positive linear trend in accessing health information without frustration from other sources over time (Wald F1, 11,602 = 4.37, P = .04) (Figure).
Figure.
A comparison of the percentage of adults aged ≥18 (with 95% confidence intervals) who sought health information and accessed health information without frustration during their most recent search, by source of health information, Health Information National Trends Survey (HINTS), 2008-2017, United States.20 Accessing health information without frustration is defined as responding “strongly disagree” to the question: “Based on the results of your most recent search for information about health or medical topics, how much do you agree or disagree with the following statement? You felt frustrated during your search for the information.” Response options were measured on a 4-point scale, ranging from 1 = strongly disagree to 4 = strongly agree. All HINTS respondents were asked, “Have you ever looked for information about health or medical topics from any source?” Those who responded yes were asked, “The most recent time you looked for information about health or medical topics, where did you go first?” Response options for this item included various information sources (eg, books, brochures, cancer organizations, family, friend, coworker, physician or health care provider, internet, library, magazines, newspapers, telephone information line, or unconventional practitioner); responses were dichotomized as internet vs other.
Discussion
Our study found that the percentage of the population who accessed health information online without frustration was stable during the study period and was below the HP2020 goal of 45%. The odds of accessing health information without frustration did not change significantly over time among the population who used the internet for their last search, controlling for sociodemographic characteristics. From 2008 to 2017, the internet was the most frequently used source of health information, with physician or health care provider consistently emerging as the second most frequent source.
In bivariate analyses, 46.6% of the non-Hispanic black population reported accessing health information without frustration. A report published in 2013 on data collected in late 2012 by the Pew Research Center showed that non-Hispanic black adults were more likely than adults from other racial/ethnic groups to use mobile devices to look up health information and more likely to use social media for such information.29 Greater use of mobile devices to search for health information may, in part, explain why non-Hispanic black adults in our study reported accessing health information without frustration more frequently than other racial/ethnic groups. The differences in accessing information without frustration by education observed in 2008 were not present in the 2011, 2013, and 2017 HINTS data. Similarly, differences by income observed in 2008 and 2011 were not present in the 2013 and 2017 HINTS data. These findings may indicate a closing of the gap in access to health information by education and income, which coincides with an increase in the use of mobile devices.30
Results from our multivariable analysis among adults who used the internet first for their most recent search for health information indicated higher odds of accessing health information without frustration among adults aged 35-49 than among younger adults. This finding is inconsistent with previous research that generally found younger age to predict the use of online information sources.31,32 Although research shows that men may have an easier time than women finding information and a better experience in doing so,33 we found no significant differences by sex in accessing health information online without frustration. In the current study, non-Hispanic black adults who used the internet first during their most recent search for health information were more likely than non-Hispanic white adults to report accessing health information without frustration. Non-Hispanic black adults are more likely than adults from other racial/ethnic groups to access the internet with mobile devices and are less likely to interact with the health care system.29,34 Consistent with previous research, income emerged as an independent predictor of easily accessing health information online, with lower odds of accessing health information without frustration observed among adults with annual household incomes <$75 000 than among adults with annual household incomes ≥$75 000.35,36 To facilitate our interpretation of these results, we conducted post hoc analyses to examine differences in the use of information sources (online vs other) by sociodemographic characteristics. Although we found no significant differences in information source by sex, the use of online sources was more frequent among populations who were younger (vs older), were non-Hispanic white (vs all other racial/ethnic groups), had higher incomes and education levels (vs lower income and education levels), and resided in metropolitan (vs nonmetropolitan) areas. Our analysis was restricted to adults who reported using the internet first for their most recent health information search, which differs from adults who use other information sources. Further research is needed to inform the development of tailored health information sources for these populations.36,37
Healthy People 2020 objectives acknowledge the importance of easy access to health information.17 In the past several decades, the availability of health information through various sources, notably the internet, has increased dramatically.38,39 However, the emergence of communication technologies and greater availability of health information do not ensure access to health information nor do they ensure that said resources are valid. A 2014 review of research evaluating the quality of online information resources revealed variability in the quality of information available, citing concerns about inaccuracy, incompleteness, and commercial bias.40
Limitations
Our study had several limitations. First, data from HINTS included in our analyses were cross-sectional. As such, the observed trends over time do not represent within-respondent changes. Ascertainment of easily accessing online health information is challenging in a national survey that is constrained by concerns for respondent burden and survey length. Thus, a second limitation was the use of one survey item that only partially captured the complex phenomenon of easily accessing health information online. Although the HP2020 objective to improve ease of accessing information is measured by the HINTS item about experiencing frustration during information seeking, the construct of frustration does not necessarily fully capture notions of ease of information access. That is, an information seeker may have challenges in accessing information without experiencing frustration. Third, details about the online sources of information used were not available. Therefore, these data do not address the quality of the online information sources encountered and do not capture the range of online platforms available to access health information, including patient portals. Fourth, measures of general literacy, health care literacy, and English proficiency, which may be related to the information-seeking experience, were not available in the 4 HINTS data sets that we analyzed. Finally, although the survey response rates were generally low, they were consistent with response rates reported in other national surveys.41,42 Furthermore, we made a considerable effort to reduce bias in the data collection and weighting approach.43
Conclusions
Despite a proliferation of health communication technologies and availability of health information online, the proportion of health information seekers in the United States who easily access health information online has not met the HP2020 objective of 45%. Future studies should continue tracking national progress toward improving ease of access to health information to inform efforts that make quality health information available to diverse populations.
Acknowledgments
The authors acknowledge Allison Ottenbacher, PhD, MPH; Anna Gaysynsky, MPH; Faren Grant, MA; Sana Vieux, MPH; and Wen-Ying Sylvia Chou, PhD, MPH, for their input on an early analysis that informed the development of this article; and Carina Tornow for her analysis of the data.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Cancer Institute via HHSN261201800002B.
ORCID iD: Lila J. Finney Rutten, PhD, MPH  https://orcid.org/0000-0001-7487-9407
https://orcid.org/0000-0001-7487-9407
References
- 1. Percheski C, Hargittai E. Health information-seeking in the digital age. J Am Coll Health. 2011;59(5):379–386. doi:10.1080/07448481.2010.513406 [DOI] [PubMed] [Google Scholar]
- 2. Fox S. Health topics: 80% of internet users look for health information online. 2011. http://www.pewresearch.org/science. Accessed September 1, 2018.
- 3. Prestin A, Vieux SN, Chou WY. Is online health activity alive and well or flatlining? Findings from 10 years of the Health Information National Trends Survey. J Health Commun. 2015;20(7):790–798. doi:10.1080/10810730.2015.1018590 [DOI] [PubMed] [Google Scholar]
- 4. Bundorf MK, Wagner TH, Singer SJ, Baker LC. Who searches the internet for health information? Health Serv Res. 2006;41(3 pt 1):819–836. doi:10.1111/j.1475-6773.2006.00510.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rice RE. Influences, usage, and outcomes of internet health information searching: multivariate results from the Pew surveys. Int J Med Inform. 2006;75(1):8–28. doi:10.1016/j.ijmedinf.2005.07.032 [DOI] [PubMed] [Google Scholar]
- 6. Finney Rutten LJ, Agunwamba AA, Wilson P, et al. Cancer-related information seeking among cancer survivors: trends over a decade (2003-2013). J Cancer Educ. 2016;31(2):348–357. doi:10.1007/s13187-015-0802-7 [DOI] [PubMed] [Google Scholar]
- 7. Cutrona SL, Mazor KM, Vieux SN, Luger TM, Volkman JE, Finney Rutten LJ. Health information-seeking on behalf of others: characteristics of “surrogate seekers.” J Cancer Educ. 2015;30(1):12–19. doi:10.1007/s13187-014-0701-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arora NK, Hesse BW, Rimer BK, Viswanath K, Clayman ML, Croyle RT. Frustrated and confused: the American public rates its cancer-related information-seeking experiences. J Gen Intern Med. 2008;23(3):223–228. doi:10.1007/s11606-007-0406-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cohen RA, Adams PF. Use of the internet for health information: United States, 2009. NCHS Data Brief. 2011;66:1–8. [PubMed] [Google Scholar]
- 10. McCloud RF, Okechukwu CA, Sorensen G, Viswanath K. Beyond access: barriers to internet health information seeking among the urban poor. J Am Med Inform Assoc. 2016;23(6):1053–1059. doi:10.1093/jamia/ocv204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nguyen A, Mosadeghi S, Almario CV. Persistent digital divide in access to and use of the internet as a resource for health information: results from a California population-based study. Int J Med Inform. 2017;103:49–54. doi:10.1016/j.ijmedinf.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 12. Miller LM, Bell RA. Online health information seeking: the influence of age, information trustworthiness, and search challenges. J Aging Health. 2012;24(3):525–541. doi:10.1177/0898264311428167 [DOI] [PubMed] [Google Scholar]
- 13. Walsh MC, Trentham-Dietz A, Schroepfer TA, et al. Cancer information sources used by patients to inform and influence treatment decisions. J Health Commun. 2010;15(4):445–463. doi:10.1080/10810731003753109 [DOI] [PubMed] [Google Scholar]
- 14. Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980-2003). Patient Educ Couns. 2005;57(3):250–261. doi:10.1016/j.pec.2004.06.006 [DOI] [PubMed] [Google Scholar]
- 15. Arora NK, Johnson P, Gustafson DH, McTavish F, Hawkins RP, Pingree S. Barriers to information access, perceived health competence, and psychosocial health outcomes: test of a mediation model in a breast cancer sample. Patient Educ Couns. 2002;47(1):37–46. [DOI] [PubMed] [Google Scholar]
- 16. Hesse BW, Gaysynsky A, Ottenbacher A, et al. Meeting the Healthy People 2020 goals: using the Health Information National Trends Survey to monitor progress on health communication objectives. J Health Commun. 2014;19(12):1497–1509. doi:10.1080/10810730.2014.954084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020: health communication and health information technology. Updated August 2019 http://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology. Accessed August 26, 2019.
- 18. Koch-Weser S, Bradshaw YS, Gualtieri L, Gallagher SS. The internet as a health information source: findings from the 2007 Health Information National Trends Survey and implications for health communication. J Health Commun. 2010;15(suppl 3):279–293. doi:10.1080/10810730.2010.522700 [DOI] [PubMed] [Google Scholar]
- 19. Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;16(7):e172 doi:10.2196/jmir.3117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Institutes of Health, National Cancer Institute. Health Information National Trends Survey: data. 2019. https://hints.cancer.gov/data/Default.aspx. Accessed June 18, 2019.
- 21. American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed 2016. https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf. Accessed July 5, 2019.
- 22. Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–460. doi:10.1080/10810730490504233 [DOI] [PubMed] [Google Scholar]
- 23. Finney Rutten LJ, Davis T, Beckjord EB, Blake K, Moser RP, Hesse BW. Picking up the pace: changes in method and frame for the Health Information National Trends Survey (2011-2014). J Health Commun. 2012;17(8):979–989. doi:10.1080/10810730.2012.700998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Blake KD, Portnoy DB, Kaufman AR, et al. Rationale, procedures, and response rates for the 2015 administration of NCI’s Health Information National Trends Survey: HINTS-FDA 2015. J Health Commun. 2016;21(12):1269–1275. doi:10.1080/10810730.2016.1242672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moser RP, Beckjord EB, Finney Rutten LJ, Blake K, Hesse BW. Using collaborative web technology to construct the Health Information National Trends Survey. J Health Commun. 2012;17(8):990–1000. doi:1080/10810730.2012.700999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SUDAAN [computer program] Version 11.0.1 Durham, NC: Research Triangle Institute; 2012. [Google Scholar]
- 27. SAS/STAT [computer program] Version 9.4 Cary, NC: SAS Institute, Inc; 2014. [Google Scholar]
- 28. US Department of Agriculture, Economic Research Service. Rural–urban continuum codes. 2013. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes. Accessed June 18, 2019.
- 29. Fox S, Duggan M. Health online 2013. 2013. http://www.pewinternet.org/2013/01/15/health-online-2013. Accessed June 20, 2018.
- 30. Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries, but plateaus across developed ones. June 19, 2018 https://www.pewresearch.org/global/2018/06/19/social-media-use-continues-to-rise-in-developing-countries-but-plateaus-across-developed-ones/. Accessed July 20, 2018.
- 31. Bidmon S, Terlutter R. Gender differences in searching for health information on the internet and the virtual patient-physician relationship in Germany: exploratory results on how men and women differ and why. J Med Internet Res. 2015;17(6):e156 doi:10.2196/jmir.4127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Massey PM. Where do U.S. adults who do not use the internet get health information? Examining digital health information disparities from 2008 to 2013. J Health Commun. 2016;21(1):118–124. doi:10.1080/10810730.2015.1058444 [DOI] [PubMed] [Google Scholar]
- 33. Ybarra M, Suman M. Reasons, assessments and actions taken: sex and age differences in uses of internet health information. Health Educ Res. 2008;23(3):512–521. doi:10.1093/her/cy1062 [DOI] [PubMed] [Google Scholar]
- 34. Bratucu R, Gheorghe IR, Purcarea RM, Gheorghe CM, Popa Velea O, Purcarea VL. Cause and effect: the linkage between the health information seeking behavior and the online environment—a review. J Med Life. 2014;7(3):310–316. [PMC free article] [PubMed] [Google Scholar]
- 35. Koch-Weser S, Bradshaw YS, Gualtieri L, Gallagher SS. The internet as a health information source: findings from the 2007 Health Information National Trends Survey and implications for health communication. J Health Commun. 2010;15(suppl 3):279–293. doi:10.1080/10810730.2010.522700 [DOI] [PubMed] [Google Scholar]
- 36. Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2016;41(1):1–19. doi:10.3109/17538157.2014.948171 [DOI] [PubMed] [Google Scholar]
- 37. Smith M, Morita H, Mateo KF, Nye A, Hutchinson C, Cohall AT. Development of a culturally relevant consumer health information website for Harlem, New York. Health Promot Pract. 2014;15(5):664–674. doi:10.1177/1524839914530401 [DOI] [PubMed] [Google Scholar]
- 38. Viswanath K. Science and society: the communications revolution and cancer control. Nat Rev Cancer. 2005;5(10):828–835. doi:10.1038/nrc1718 [DOI] [PubMed] [Google Scholar]
- 39. Viswanath K, Nagler RH, Bigman-Galimore CA, McCauley MP, Jung M, Ramanadhan S. The communications revolution and health inequalities in the 21st century: implications for cancer control [published erratum appears in Cancer Epidemiol Biomarkers Prev. 2013;22(3):470]. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1701–1708. doi:10.1158/1055-9965.EPI-12-0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fahy E, Hardikar R, Fox A, Mackay S. Quality of patient health information on the internet: reviewing a complex and evolving landscape. Australas Med J. 2014;7(1):24–28. doi:10.4066/AMJ.2014.1900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking chronic disease and risk behavior prevalence as survey participation declines: statistics from the Behavioral Risk Factor Surveillance System and other national surveys. Prev Chronic Dis. 2008;5(3):A80. [PMC free article] [PubMed] [Google Scholar]
- 42. Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: evaluating the need for concern about wireless substitution. Am J Public Health. 2006;96(5):926–931. doi:10.2015/AJPH.2004.057885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cantor D, Coa K, Crystal-Mansour S, Davis T, Dipko S, Sigman R. Health Information National Trends Survey (HINTS) 2007 Final Report. Bethesda, MD: National Cancer Institute; 2009; https://hints.cancer.gov/docs/methodologyreports/HINTS_2007_Final_Report.pdf. Accessed December 15, 2014. [Google Scholar]