Abstract
Objective:
Emergency departments (EDs) are critical settings for hepatitis C care in the United States. We assessed trends and characteristics of hepatitis C–associated ED visits during 2006-2014.
Methods:
We used data from the 2006-2014 Nationwide Emergency Department Sample to estimate numbers, rates, and costs of hepatitis C–associated ED visits, defined by either first-listed diagnosis of hepatitis C or all-listed diagnosis of hepatitis C. We assessed trends by demographic characteristics, liver disease severity, and patients’ disposition by using joinpoint analysis, and we calculated the average annual percentage change (AAPC) from 2006 to 2014.
Results:
During 2006-2014, the rate per 100 000 visits of first-listed and all-listed hepatitis C–associated ED visits increased significantly from 10.1 to 25.4 (AAPC = 13.0%; P < .001) and from 484.4 to 631.6 (AAPC = 3.4%; P < .001), respectively. Approximately 70% of these visits were made by persons born during 1945-1965 (baby boomers); 30% of visits were made by Medicare beneficiaries and 40% by Medicaid beneficiaries. Significant rate increases were among visits by baby boomers (first-listed: AAPC = 13.8%; all-listed: AAPC = 2.6%), persons born after 1965 (first-listed: AAPC = 14.3%; all-listed: AAPC = 9.2%), Medicare beneficiaries (first-listed: AAPC = 18.0%; all-listed: AAPC = 3.9%), and persons hospitalized after ED visits (first-listed: AAPC = 20.0%; all-listed: AAPC = 2.3%; all P < .001). Increasing proportions of compensated cirrhosis were among visits by baby boomers (first-listed: AAPC = 11.5%; all-listed: AAPC = 6.3%). Annual hepatitis C–associated total ED costs increased by 400.0% (first-listed) and 192.0% (all-listed) during 2006-2014.
Conclusion:
Public health efforts are needed to address the growing burden of hepatitis C care in the ED.
Keywords: hepatitis C virus, emergency department visits, trends, baby boomers, Medicare beneficiaries, Medicaid beneficiaries
Hepatitis C virus (HCV) infection is a major public health problem in the United States that affects approximately 2.4 million persons.1-4 HCV infection is the major cause of liver cirrhosis, hepatocellular carcinoma, and liver transplantation, all of which are associated with increased mortality and health care burden in the United States.5-7
The emergency department (ED) is an important setting for hepatitis C care in the United States. EDs not only serve severely ill patients from a broad spectrum of society but also provide health care access to vulnerable and difficult-to-reach populations. For example, Medicaid beneficiaries, racial/ethnic minority groups, and uninsured/underinsured persons are known to be disproportionately affected by HCV infection.8 Baby boomers (those born during 1945-1965) and persons who inject drugs, the 2 major at-risk subgroups for HCV infection, also tend to use EDs more than the general population.9-16 Several studies of local ED-based HCV screenings showed HCV antibody prevalence ranging from 6% to 18%,9-13,16 which is higher than national estimates for baby boomers (3%-4%)17 and the general population (1%).1,4 Among study participants with RNA test results after a reactive antibody test, estimates of current HCV infection were as high as 70%.9,10,13
Compared with studies of local ED use, studies of national ED use for hepatitis C care are limited. One study estimated the rate of hepatitis C–associated ED visits at 80.0 per 100 000 visits annually during 2001-2010.7 The study found no changes in the percentage of ED visits for hepatitis C in the overall US population or among baby boomers.7 HCV epidemiology has evolved quickly in recent years.18 Since 2012, both the Centers for Disease Control and Prevention (CDC) and the US Preventive Services Task Force have recommended one-time hepatitis C testing for all baby boomers.17,19 The availability of highly effective direct-acting antiviral agents since 2013 has substantially transformed hepatitis C care,20 which may have prompted more patients to seek treatment in EDs and other settings. Understanding more recent hepatitis C–associated ED use is essential for developing effective guidelines and programs for ED-based hepatitis C care, including screening and linkage-to-care services. The objective of this study was to assess trends in numbers, rates, and costs of hepatitis C–associated ED visits overall and in subgroups defined by demographic characteristics, liver disease severity, and patients’ dispositions (ie, the discharge destination of patients after ED care) in the United States during 2006-2014.
Methods
Data Sources
We used data from the 2006-2014 releases of the Nationwide Emergency Department Sample (NEDS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.21 NEDS is the largest publicly available all-payer ED database in the United States. It contains approximately 31 million records each year from more than 950 hospitals with data on diagnoses and procedures, discharge status from the ED, patient demographic characteristics, payment source, and total ED charges. It is a nationally representative, 20% stratified sample of visits to EDs of noninstitutional, general, short-stay, nonfederal hospitals, selected according to geographic region, location, teaching status, ownership, and trauma-level designation. Because this secondary analysis used de-identified NEDS data, institutional review board approval was not required.
Study Variables
NEDS contains up to 30 diagnosis codes per ED visit. In general, the first-listed diagnosis is the primary reason for a visit; however, all-listed diagnoses may need to be considered when the first-listed diagnosis is symptom-based.22 In this study, we estimated hepatitis C–associated ED visits with both a first-listed diagnosis of hepatitis C (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes23 070.41 [acute hepatitis C with hepatic coma], 070.44 [chronic hepatitis C with hepatic coma], 070.51 [acute hepatitis C without hepatic coma], 070.54 [chronic hepatitis C without hepatic coma], 070.70 [unspecified hepatitis C with hepatic coma], 070.71 [unspecified hepatitis C without hepatic coma], or V02.62 [hepatitis C carrier]) (narrow definition) and all-listed diagnoses of hepatitis C, using the same codes, listed anywhere in the record (broad definition).
We grouped patient ages at ED admission as ≤34, 35-44, 45-54, 55-64, and ≥65 years. We classified birth cohort as baby boomers (born during 1945-1965), younger cohort (born after 1965), and older cohort (born before 1945). We classified place of residence as an urban area or a rural area; primary payer as Medicare, Medicaid, private insurance, uninsured, and other payers (including workers’ compensation, Civilian Health and Medical Program of the Uniformed Services [CHAMPUS], Civilian Health and Medical Program of the Department of Veterans Affairs [CHAMPVA], Title V, and other government programs). We grouped the median annual household income of the patient’s ZIP code as 4 national quartiles (0-25, 26-50, 51-75, 76-100 percentile), indicating the poorest to wealthiest populations. In 2014, the lowest income quartile ranged from $1 to $39 999 and the highest income quartile was ≥$66 000.24 We divided disposition of the patient from ED visits into the following categories: routine discharge, admitted to hospital (transferred to short-term hospital or admitted as inpatient to the same hospital), transferred to other facilities (nursing facility, intermediate care, home health care, and other types of facilities), discharged against medical advice, and other discharges (including died in ED, discharged/transferred to court/law enforcement, not admitted, or destination unknown). We summarized total charges for each ED visit service annually and reported in 2014 dollars using the Consumer Price Index adjustment for Medical Care.25
We classified liver disease severity (end-stage liver disease, compensated cirrhosis, and non-cirrhotic liver disease) by ICD-9-CM diagnosis codes, procedure codes, or Current Procedural Terminology codes.26-28 End-stage liver disease includes liver failure with hepatic encephalopathy (572.2), portal hypertension/portal decompression procedures (572.3, 37140, 37160, 37180, 37181, 37182, 37183), hepatorenal syndrome (572.4), esophageal varices complication with or without bleeding (456.0, 456.20, 456.21, 42.91, 44.91, 96.06, 43204, 43205, 43243, 43244, 43400, 43401), ascites/paracentesis procedures (789.5, 789.59, 54.91, 49080, 49081), splenomegaly (789.2), hypersplenism (289.4), jaundice (782.4), encephalopathy (348.3x), hepatocellular carcinoma (155.0, 155.1, 155.2, 070.0, 070.2x, 070.4x, 070.6, 070.71), and liver transplantation (996.82, V42.7, 50.5, 50.51, 50.59, 47135, 47136). Compensated cirrhosis includes alcoholic cirrhosis of liver without ascites (571.2) and cirrhosis of liver without mention of alcohol (571.5). All other conditions were listed as non-cirrhotic liver disease.
Statistical Analysis
We tabulated descriptive statistics using the NEDS survey sampling design and weight variables to calculate nationally representative estimates and corresponding 95% confidence intervals (CIs). We calculated and analyzed the 9-year trends in numbers, rates per 100 000 visits, and average costs of hepatitis C–associated ED visits for each year from 2006 through 2014. We assessed hepatitis C–associated ED visits by demographic characteristics (age, sex, birth cohort, place of residence, payer, and median household income quartiles), liver disease severity (non-cirrhotic liver disease, compensated cirrhosis, and end-stage liver disease), disposition from ED, and costs. We assessed differences in proportions from 2006 to 2014 using the z score test. We analyzed trends in numbers, rates, and costs of hepatitis C–associated ED visits by using the joinpoint regression program (National Cancer Institute). Because baby boomers account for most hepatitis C–associated ED visits, we also investigated trends in liver disease severity among visits by these patients. We described the resulting trends by annual average percentage change (AAPC) by applying the least-squares linear regression methods. We considered P < .05 to be significant. We conducted all analyses for both first-listed hepatitis C–associated ED visits and all-listed hepatitis C–associated ED visits using SAS version 9.4.29
Results
In the United States, the annual number of first-listed hepatitis C–associated ED visits nearly tripled, from 12 090 visits in 2006 to 34 975 visits in 2014, and the number of all-listed hepatitis C–associated ED visits increased 50.0%, from 581 350 visits in 2006 to 870 385 visits in 2014 (Table 1). The distribution of hepatitis C–associated ED visits changed significantly from 2006 to 2014 for most characteristics examined. Most persons with a first-listed diagnosis of hepatitis C or all-listed diagnosis of hepatitis C were aged 45-54 in 2006 but aged 55-64 in 2014. The percentage of persons with Medicare as the primary payer increased for first-listed (23.5% in 2006 to 35.6% in 2014; P < .001) and all-listed (27.3% in 2006 to 31.6% in 2014; P < .001) hepatitis C–associated ED visits. Similarly, the percentage of persons with Medicaid as the primary payer increased for first-listed (32.6% in 2006 to 37.1% in 2014; P = .01) and all-listed (33.0% in 2006 to 41.4% in 2014; P < .001) hepatitis C–associated ED visits.
Table 1.
Hepatitis C–associated emergency department (ED) visits, by characteristics, United States, 2006 and 2014a
| Characteristic | ED Visits With First-Listed Diagnosis of Hepatitis C, No. (%)b | ED Visits With All-Listed Diagnosis of Hepatitis C, No. (%)b | ||||
|---|---|---|---|---|---|---|
| 2006 | 2014 | P Valuec | 2006 | 2014 | P Valuec | |
| Overall | 12 096 (100.0) | 34 975 (100.0) | 581 350 (100.0) | 870 385 (100.0) | ||
| Age at ED visit, mean (median), y | 48.7 (48.8) | 54.2 (55.4) | 48.8 (48.4) | 52.4 (53.5) | ||
| Age, y | ||||||
| ≤34 | 1410 (11.7) | 2974 (8.5) | <.001 | 52 082 (9.0) | 94 066 (10.8) | <.001 |
| 35-44 | 2262 (18.7) | 2599 (7.4) | <.001 | 129 997 (22.4) | 100 095 (11.5) | <.001 |
| 45-54 | 5141 (42.5) | 9707 (27.8) | <.001 | 254 737 (43.8) | 258 788 (29.7) | <.001 |
| 55-64 | 2382 (19.7) | 14 806 (42.3) | <.001 | 103 450 (17.8) | 311 538 (35.8) | <.001 |
| ≥65 | 901 (7.4) | 4889 (14.0) | <.001 | 41 124 (7.1) | 105 885 (12.2) | <.001 |
| Sex | ||||||
| Male | 7443 (61.5) | 22 326 (63.8) | .19 | 351 202 (60.4) | 532 356 (61.2) | .20 |
| Female | 4653 (38.5) | 12 649 (36.2) | .19 | 230 148 (39.6) | 338 006 (38.8) | .20 |
| Birth cohort | ||||||
| Born after 1965 | 2322 (19.2) | 7863 (22.5) | .01 | 108 780 (18.7) | 265 823 (30.5) | <.001 |
| Baby boomersd | 8549 (70.7) | 25 068 (71.7) | .43 | 416 120 (71.6) | 556 452 (63.9) | <.001 |
| Born before 1965 | 1224 (10.1) | 2043 (5.8) | <.001 | 56 490 (9.7) | 48 098 (5.5) | <.001 |
| Place of residence | ||||||
| Urban | 9973 (83.1) | 30 171 (87.5) | .01 | 503 348 (87.7) | 754 331 (88.9) | .26 |
| Rural | 2035 (16.9) | 4319 (12.5) | .01 | 70 848 (12.3) | 94 398 (11.1) | .26 |
| Payer | ||||||
| Medicare | 2830 (23.5) | 12 452 (35.6) | <.001 | 158 483 (27.3) | 275 162 (31.6) | <.001 |
| Medicaid | 3933 (32.6) | 12 954 (37.1) | .01 | 191 665 (33.0) | 360 149 (41.4) | <.001 |
| Private insurance | 2363 (19.6) | 4764 (13.6) | <.001 | 96 981 (16.7) | 108 647 (12.5) | <.001 |
| Uninsurede | 2170 (18.0) | 2919 (8.4) | <.001 | 97 347 (16.8) | 89 309 (10.3) | <.001 |
| Otherf | 765 (6.3) | 1870 (5.3) | .44 | 35 748 (6.2) | 36 217 (4.2) | .004 |
| National quartile for median household income of patient’s ZIP codeg | ||||||
| 0-25 | 4511 (38.9) | 13 302 (39.6) | .78 | 222 668 (39.8) | 360 617 (43.7) | .08 |
| 26-50 | 3090 (26.6) | 9661 (28.7) | .23 | 144 363 (25.8) | 223 820 (27.1) | .32 |
| 51-75 | 2434 (21.0) | 6250 (18.6) | .13 | 116 549 (20.8) | 142 861 (17.3) | .002 |
| 76-100 | 1574 (13.6) | 4395 (13.1) | .75 | 76 375 (13.6) | 98 265 (11.9) | .14 |
| Liver disease severity | ||||||
| Non-cirrhotic liver disease | 5577 (46.1) | 6245 (17.9) | <.001 | 434 643 (74.8) | 615 373 (70.7) | <.001 |
| Compensated cirrhosis | 2078 (17.2) | 14 226 (40.7) | <.001 | 57 919 (10.0) | 128 534 (14.8) | <.001 |
| End-stage liver diseaseh | 4441 (36.7) | 14 504 (41.5) | .02 | 88 851 (15.3) | 126 478 (14.5) | .11 |
| Disposition of patient from the ED | ||||||
| Routine discharge | 4467 (36.9) | 6158 (17.6) | <.001 | 184 865 (31.8) | 336 967 (38.7) | <.001 |
| Admitted to hospital | 7152 (59.1) | 28 354 (81.1) | <.001 | 369 629 (63.6) | 503 555 (57.9) | .002 |
| Transferred to other facilitiesi | 100 (0.8) | 220 (0.6) | .43 | 8752 (1.5) | 14 783 (1.7) | .30 |
| Discharged against medical advice | 112 (0.9) | 210 (0.6) | .14 | 5001 (0.9) | 13 324 (1.5) | <.001 |
| Other dischargesj | 264 (2.2) | NC | NC | 13 167 (2.3) | 1757 (0.2) | <.001 |
Abbreviation: NC, not calculated because of limited sample size.
a Data source: Nationwide Emergency Department Sample database.21
b The number of ED visits are weighted to be nationally representative. Some rows by characteristics may not sum to the column total because of missing data.
cP values were from z score tests comparing category-specific proportions from 2006 to 2014. P < .05 was considered significant.
d Born during 1945-1965.
e Uninsured payments include self-pay and no charge.
f Other payers include Workers’ Compensation, Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), Title V, and other government programs.
g The median household incomes of residents in the patients’ ZIP code were classified as 4 quartiles by 0-25th, 26th-50th, 51st-75th, and 76th-100th percentiles, indicating the poorest to wealthiest populations.24
hEnd-stage liver disease includes decompensated cirrhosis, hepatocellular carcinoma, and liver transplantation.
i Other facilities include nursing facility, intermediate care, home health care, and other type of facilities.
j Other discharges include died in ED, discharged/transferred to court/law enforcement, not admitted, or destination unknown.
Baby boomers accounted for most first-listed hepatitis C–associated ED visits in both years: approximately 70.7% in 2006 and 71.6% in 2014. For all-listed hepatitis C–associated ED visits, the percentage of baby boomers decreased from 71.6% in 2006 to 63.9% in 2014 (P < .001), and the percentage of the younger cohort increased from 18.7% in 2006 to 30.5% in 2014 (P < .001). The percentage of persons who had liver disease with compensated cirrhosis increased significantly for first-listed (17.2% in 2006 to 40.7% in 2014; P < .001) and all-listed (10.0% in 2006 to 14.8% in 2014; P < .001) hepatitis C–associated ED visits. The percentage of hospital admissions after ED visits increased from 59.1% in 2006 to 81.1% in 2014 (P < .001) for first-listed hepatitis C–associated ED visits. In 2006 and 2014, most hepatitis C–associated ED visits were made by male patients, by patients who resided in urban area, and by patients who lived in ZIP codes with median annual household incomes in the 2 lowest quartiles in the nation. Changes in demographic distribution, such as by age and birth cohort, of all-cause ED visits were smaller than demographic changes of hepatitis C–associated ED visits (Supplementary Table available at https://figshare.com/articles/Supplemental_Table_Distributions_of_all-cause_emergency_department_ED_visits_by_characteristics_in_the_United_States_2006_and_2014/9 585 839).
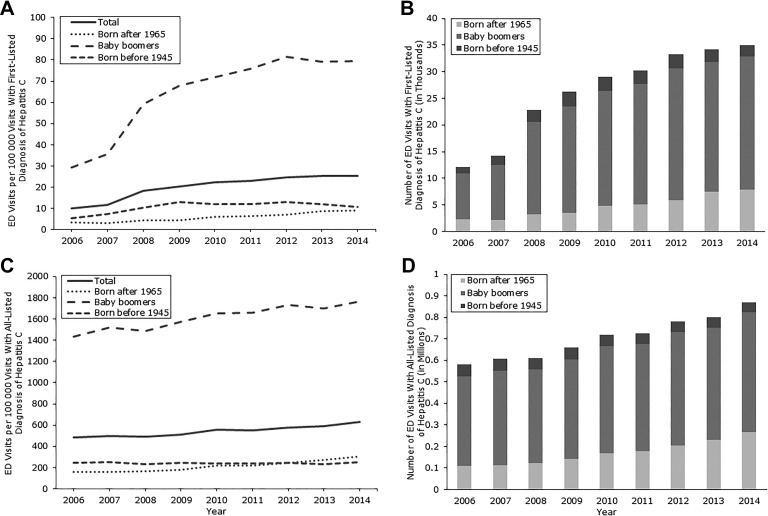
Trends in rates and numbers of first-listed and all-listed hepatitis C–associated ED visits were assessed overall and by birth cohort (Figure 1). Overall, the rate per 100 000 visits of first-listed hepatitis C–associated ED visits more than doubled, from 10.1 (95% CI, 9.1-11.1) in 2006 to 25.4 (95% CI, 23.2-27.5) in 2014 (AAPC = 13.0%; P < .001) (Figure 1). By birth cohort, increases in the rate of first-listed hepatitis C–associated ED visits were 170.0% among baby boomers (AAPC = 13.8; P < .001), 164.7% among the younger cohort (AAPC = 14.3; P < .001), and 98.1% among the older cohort (AAPC = 9.1; P < .001) (Table 2). The rate per 100 000 visits of all-listed hepatitis C–associated ED visits increased 30.4%, from 484.4 (95% CI, 449.9-518.8) in 2016 to 631.6 (95% CI, 584.6-678.6) in 2014 (AAPC = 3.4%; P < .001). By birth cohort, increases in the rate of first-listed hepatitis C–associated ED visits were 23.3% among baby boomers (AAPC = 2.6; P < .001) and 90.9% among the younger cohort (AAPC = 9.2; P < .001) (Table 3). The number of ED visits for both first-listed hepatitis C–associated ED visits and all-listed hepatitis C–associated ED visits also increased significantly from 2006 to 2014. During these years, baby boomers remained as the majority (approximately 70%) of both first-listed hepatitis C–associated ED visits and all-listed hepatitis C–associated ED visits.
Figure 1.
Trends in the number and rate of emergency department (ED) visits with first-listed and all-listed diagnosis of hepatitis C, overall and by birth cohort, United States, 2006-2014. (A) Rate of ED visits with first-listed diagnosis of hepatitis C; (B) number of ED visits with first-listed diagnosis of hepatitis C; (C) rate of ED visits with all-listed diagnosis of hepatitis C; (D) number of ED visits with all-listed diagnosis of hepatitis C. Data are from the 2006-2014 Nationwide Emergency Department Sample (NEDS) survey.21 Visits are nationally representative by using the NEDS weights and sampling design. Birth cohort is stratified as younger cohort (born after 1965), baby boomers (born 1945-1965), and older cohort (born before 1945). Trends were assessed by joinpoint analysis.
Table 2.
Trends in emergency department (ED) visits with first-listed diagnosis of hepatitis C, by subgroups, United States, 2006-2014a
| Characteristic | First-Listed Hepatitis C–Associated ED Visits per 100 000 Visits, Rate (95% CI)b | % Increase From 2006 to 2014c | AAPC From 2006 to 2014d | ||||
|---|---|---|---|---|---|---|---|
| 2006 | 2008 | 2010 | 2012 | 2014 | |||
| Overall | 10.1 (9.1-11.1) | 18.3 (16.8-19.8) | 22.5 (20.6-24.4) | 24.8 (22.3-27.2) | 25.4 (23.2-27.5) | 151.5e | 13.0e |
| Sex | |||||||
| Male | 13.6 (12.0-15.2) | 26.1 (23.6-28.6) | 33.3 (30.3-36.3) | 35.9 (31.9-39.9) | 36.4 (33.0-39.8) | 167.6e | 13.8e |
| Female | 7.1 (6.3-8.0) | 12 (10.9-13.0) | 13.8 (12.5-15.0) | 15.8 (14.4-17.3) | 16.5 (15.1-18.0) | 132.4e | 11.8e |
| Birth cohort | |||||||
| Born after 1965 | 3.4 (3.0-3.8) | 4.4 (3.9-4.9) | 6.2 (5.5-6.8) | 7.0 (6.3-7.7) | 9.0 (8.1-9.9) | 164.7e | 14.3e |
| Baby boomersf | 29.5 (26.2-32.7) | 59.2 (54.2-64.1) | 72 (65.7-78.3) | 81.6 (73.0-90.2) | 79.6 (72.5-86.7) | 170.0e | 13.8e |
| Born before 1945 | 5.4 (4.4-6.3) | 10.4 (9.1-11.8) | 12.2 (10.6-13.8) | 13 (10.9-15.2) | 10.7 (9.1-12.4) | 98.1e | 9.1e |
| Place of residence | |||||||
| Urban | 10.4 (9.2-11.6) | 19.7 (17.9-21.4) | 23.9 (21.7-26.1) | 26.3 (23.5-29.1) | 26.6 (24.2-29.0) | 155.8e | 14.5e |
| Rural | 8.6 (7.4-9.9) | 11.8 (10.2-13.3) | 15.8 (13.9-17.6) | 17.0 (14.8-19.2) | 18.2 (15.9-20.6) | 111.6e | 11.4e |
| Payers | |||||||
| Medicare | 11.7 (10.2-13.1) | 27 (24.5-29.6) | 33.8 (30.7-37.0) | 38.2 (33.8-42.7) | 40.0 (36.1-43.8) | 241.9e | 18.0e |
| Medicaid | 14.8 (12.6-17.1) | 25.2 (22.2-28.2) | 28.2 (25.1-31.3) | 29.5 (26.0-33.1) | 29.4 (26.6-32.1) | 98.6e | 10.6e |
| Private insurance | 5.7 (4.9-6.5) | 11.2 (9.3-13.1) | 12.7 (11.1-14.3) | 12.8 (11.1-14.6) | 12.7 (11.2-14.3) | 122.8e | 12.1e |
| Uninsuredg | 10.5 (9.2-11.8) | 12.2 (10.8-13.6) | 14.6 (12.6-16.6) | 16.5 (14.7-18.3) | 15.5 (13.4-17.5) | 47.6e | 7.5e |
| Otherh | 11.6 (8.3-15.0) | 22.1 (17.9-26.3) | 34.3 (26.0-42.7) | 31.7 (24.7-38.7) | 30.9 (20.0-41.9) | 166.4e | 12.3e |
| National quartile for median annual household income of patient’s ZIP codei | |||||||
| 0-25 | 12.3 (10.5-14.1) | 18.4 (16.5-20.3) | 23 (20.4-25.6) | 26.1 (23.2-29.1) | 28.0 (25.1-30.9) | 127.6e | 11.5e |
| 26-50 | 9.8 (8.6-11.0) | 18.5 (16.3-20.6) | 22.2 (19.9-24.6) | 25.0 (21.6-28.3) | 24.7 (22.1-27.4) | 152.0e | 14.4e |
| 51-75 | 8.9 (7.8-10.1) | 17.7 (15.6-19.9) | 21.6 (18.9-24.4) | 23.0 (19.5-26.6) | 22.6 (20.2-25.0) | 153.9e | 13.5e |
| 76-100 | 7.2 (6.1-8.3) | 15.4 (13.1-17.6) | 19.9 (16.9-22.9) | 21.5 (18.3-24.6) | 21.1 (17.9-24.4) | 193.1e | 13.6e |
| Disposition of patient from the ED | |||||||
| Routine discharge | 4.9 (4.3-5.4) | 4.9 (4.3-5.6) | 4.9 (4.2-5.5) | 5.3 (4.8-5.8) | 5.5 (4.9-6.1) | 12.2 | 2.2e |
| Admitted to hospital | 36.3 (31.5-41.0) | 84.2 (76.8-91.6) | 109.2 (99.9-119.0) | 127.9 (114.0-142.0) | 132 (120.0-144.0) | 263.6e | 20.0e |
| Transferred to other facilitiesj | 5.8 (3.1-8.5) | 7.8 (4.6-11.0) | 6.7 (3.8-9.6) | 10.8 (7.3-14.3) | 11.2 (7.7-14.7) | 93.1e | 5.7 |
| Discharged against medical advice | 7.1 (4.2-10.0) | 6.6 (3.7-9.6) | 8.4 (4.9-11.9) | 7.7 (5.0-10.5) | 10.2 (7.1-13.3) | 103.2e | 6.7e |
| Other dischargesk | 5.2 (2.9-7.4) | 4.2 (1.7-6.6) | 9.7 (4.1-15.3) | NC | NC | NC | NC |
| Total ED costs, mean (95% CI), 2014 $ | 2008 (1832-2183) | 2011 (1874-2148) | 2395 (2236-2554) | 2650 (2426-2875) | 2979 (2758-3200) | 48.4e | 5.2e |
Abbreviations: AAPC, average annual percentage change; NC, not calculated because of small sample size.
a Data source: Nationwide Emergency Department Sample database.21
b The number of ED visits are weighted to be nationally representative.
c Percentage increase was analyzed by using the z score test, with P < .05 considered significant.
d AAPC were analyzed by joinpoint analysis, with P < .05 considered significant.
e Significant at P < .001.
f Born during 1945-1965.
g Uninsured payments include self-pay and no charge.
h Other payers include Workers’ Compensation, Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), Title V, and other government programs.
i The median household incomes of residents in the patients’ ZIP code were classified as 4 quartiles by 0-25th, 26th-50th, 51st-75th, and 76th-100th percentiles, indicating the poorest to wealthiest populations.24
j Other facilities include nursing facility, intermediate care, home health care, and other type of facilities.
k Other discharges include died in ED, discharged/transferred to court/law enforcement, not admitted, or destination unknown.
Table 3.
Trends in emergency department (ED) visits with all-listed diagnosis of hepatitis C, by subgroups, United States, 2006-2014a
| Characteristics | All-Listed Hepatitis C–Associated ED Visits per 100 000 Visits, Rate (95% CI)b | % Increase (2014 vs 2006)c | AAPC (2006- 2014)d | ||||
|---|---|---|---|---|---|---|---|
| 2006 | 2008 | 2010 | 2012 | 2014 | |||
| Overall | 484.4 (449.9-518.8) | 489.5 (454.9-524.0) | 556.6 (520.4-592.7) | 580.2 (533.3-627.2) | 631.6 (584.6-678.6) | 30.4e | 3.4e |
| Sex | |||||||
| Male | 641.7 (596.1-687.3) | 664.0 (615.1-712.8) | 760.9 (709.8-811.9) | 791.5 (727.3-855.8) | 868.2 (801.7-934.7) | 35.3e | 3.7e |
| Female | 352.5 (325.7-379.4) | 346.3 (321.8-370.8) | 392.0 (366.2-417.8) | 410.5 (376.5-444.4) | 441.9 (409.4-474.5) | 25.4e | 3.2e |
| Birth cohort | |||||||
| Born after 1965 | 159.6 (143.7-175.5) | 166.9 (151.4-182.4) | 217.5 (196.9-238.2) | 243.0 (215.8-270.2) | 304.6 (275.8-333.3) | 90.9e | 9.2e |
| Baby boomersf | 1433.6 (1343.0-1524.3) | 1488.8 (1395.3-1582.2) | 1655.4 (1560.7-1750.1) | 1733.4 (1609.9-1856.9) | 1767.2 (1648.0-1886.5) | 23.3e | 2.6e |
| Born before 1945 | 247.3 (232.1-262.5) | 234.3 (215.0-253.5) | 242.0 (222.4-261.7) | 244.9 (222.7-267.0) | 252.6 (227.3-277.9) | 2.1 | –0.4 |
| Place of residence | |||||||
| Urban | 526.0 (484.3-567.7) | 520.3 (480.7-559.9) | 595.1 (553.2-636.9) | 621.2 (566.1-676.3) | 665.8 (612.8-718.9) | 26.6e | 3.1e |
| Rural | 299.8 (271.2-328.4) | 283.3 (256.0-310.6) | 327.4 (285.9-368.8) | 345.3 (311.2-379.4) | 398.3 (358.2-438.4) | 32.9e | 3.8e |
| Payer | |||||||
| Medicare | 653.4 (614.6-692.2) | 656.5 (616.1-697.0) | 754.9 (711.5-798.2) | 808.8 (752.1-865.5) | 883.1 (822.1-944.1) | 35.2e | 3.9e |
| Medicaid | 722.9 (649.1-796.7) | 751.0 (663.2-838.9) | 783.3 (711.3-855.2) | 734.6 (649.8-819.3) | 816.5 (737.6-895.4) | 12.9 | 0.6 |
| Private insurance | 233.2 (216.7-249.8) | 234.5 (216.8-252.3) | 251.5 (234.4-268.6) | 265.9 (245.5-286.3) | 290.7 (261.8-319.6) | 24.7e | 2.6e |
| Uninsuredg | 471.0 (428.5-513.5) | 435.8 (401.6-469.9) | 462.1 (423.6-500.6) | 508.2 (454.2-562.3) | 473.1 (413.4-532.9) | 0.4 | 1.6 |
| Otherh | 543.8 (455.3-632.3) | 602.3 (516.8-687.8) | 806.4 (679.4-933.4) | 683.1 (584.7-781.5) | 599.1 (471.2-726.9) | 10.2 | 2.0 |
| National quartile for median household income of patient’s ZIP codei | |||||||
| 0-25 | 609.1 (545.3-672.9) | 549.8 (490.2-609.4) | 642.9 (578.3-707.5) | 678.3 (608.2-748.3) | 759.9 (686.2-833.5) | 24.8e | 2.3 |
| 26-50 | 456.9 (424.3-489.5) | 439.0 (406.5-471.6) | 504.3 (466.9-541.6) | 549.1 (481.3-616.9) | 573.2 (525.8-620.6) | 25.5e | 3.6e |
| 51-75 | 428.0 (391.9-464.0) | 437.3 (402.5-472.2) | 488.5 (444.7-532.3) | 509.0 (463.1-554.9) | 516.3 (474.9-557.6) | 20.6e | 3.1e |
| 76-100 | 348.0 (317.2-378.8) | 366.3 (334.4-398.3) | 416.9 (377.3-456.6) | 435.0 (395.2-474.8) | 472.8 (422.9-522.7) | 35.9e | 3.6e |
| Disposition of patient from the ED | |||||||
| Routine discharge | 201.2 (178.2-224.2) | 217.6 (197.2-238.1) | 263.4 (235.7-291.1) | 282.0 (252.2-311.7) | 301.2 (270.7-331.6) | 49.7e | 5.5e |
| Admitted to hospital | 1873.5 (1735.2-2011.8) | 1806.4 (1668.3-1944.5) | 1958.0 (1838.5-2077.6) | 2109.4 (1934.4-2284.4) | 2343.6 (2180.5-2506.8) | 25.1e | 2.3e |
| Transferred to other facilitiesj | 504.6 (397.2-611.9) | 431.5 (325.9-537.1) | 676.2 (564.7-787.7) | 682.0 (599.0-764.9) | 751.0 (656.9-845.0) | 48.8e | 6.6e |
| Discharged against medical advice | 316.6 (266.4-366.7) | 380.3 (334.5-426.1) | 520.6 (455.7-585.5) | 558.3 (480.6-636.1) | 643.3 (551.4-735.1) | 103.2e | 9.6e |
| Other dischargesk | 257.4 (169.8-345.0) | 139.6 (40.3-238.8) | 389.7 (155.0-624.4) | 400.1 (311.1-489.2) | 440.7 (311.6-569.8) | 85.7 | 8.2e |
| Total ED costs, mean (95% CI), 2014 $ | 2090 (1942-2238) | 2412 (2243-2581) | 2868 (2665-3071) | 3098 (2832-3364) | 3720 (3463-3977) | 78.0e | 6.9e |
Abbreviations: AAPC, average annual percentage change; NC, not calculated because of small sample size.
a Data source: Nationwide Emergency Department Sample database.21
b The number of ED visits are weighted to be nationally representative.
c Percentage increase was analyzed by using the z score test, with P < .05 considered significant.
d AAPCs were analyzed by using joinpoint analysis, with P < .05 considered significant.
e Significant at P < .001.
f Born during 1945-1965.
g Uninsured payments include self-pay and no charge.
h Other payers include Workers’ Compensation, Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), V, and other government programs.
i The median household incomes of residents in the patients’ ZIP code were classified as 4 quartiles by 0-25th, 26th-50th, 51st-75th, and 76th-100th percentiles, indicating the poorest to wealthiest populations.24
j Other facilities include nursing facility, intermediate care, home health care, and other type of facilities.
k Other discharges include died in ED, discharged/transferred to court/law enforcement, not admitted, or destination unknown.
Trends in hepatitis C–associated ED visits were significant among other subgroups for both first-listed hepatitis C–associated ED visits and all-listed hepatitis C-associated ED visits. From 2006 to 2014, the rates of first-listed hepatitis C–associated ED visits increased by 241.9% among visits by Medicare beneficiaries (AAPC = 18.0; P < .001), 263.6% among visits that led to hospital admissions (AAPC = 20.0; P < .001), and 167.6% among visits by males (AAPC = 13.8; P < .001) (Table 2). The rates of all-listed hepatitis C–associated ED visits also increased from 2006 to 2014, overall and for most subgroups examined, although these increases were smaller than the increases in the rates of first-listed hepatitis C–associated ED visits. The rate of all-listed hepatitis C–associated ED visits increased significantly (103.2%) among those who left the ED against medical advice (AAPC = 9.6; P < .001) (Table 3).
The mean and annual total charges for hepatitis C–associated ED visits increased significantly from 2006 to 2014. The inflation-adjusted mean cost per first-listed hepatitis C-associated ED visit increased 48.4%, from $2008 in 2006 to $2979 in 2014 (AAPC = 5.2; P < .001) (Table 2). The annual total costs of first-listed hepatitis C–associated ED visits increased 400.0%, from $14.2 million in 2006 to $71.1 million in 2014. The mean cost per all-listed hepatitis C–associated ED visit increased 78.0%, from $2090 in 2006 to $3720 in 2014 (AAPC = 6.9; P < .001) (Table 3). The mean cost per all-listed hepatitis C–associated ED visit was significantly higher than that for all other ED visits without any diagnosis of hepatitis C during 2006-2014. The annual total costs of all-listed hepatitis C–associated ED visits increased 192.0%, from $773.9 million in 2006 to $2.3 billion in 2014.
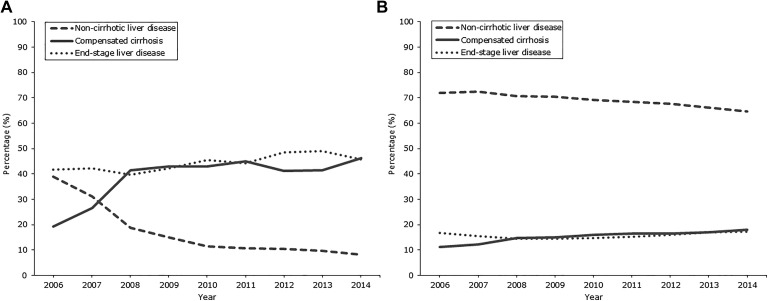
We also assessed changes in liver disease severity among visits by baby boomers (Figure 2). Among first-listed hepatitis C–associated ED visits by baby boomers, we found a significant increase in the proportion of persons with compensated cirrhosis, from 19.2% in 2006 to 46.2% in 2014 (AAPC = 11.5; P < .001), and the proportion of persons with end-stage liver disease, from 41.8% in 2006 to 45.7% in 2014 (AAPC = 2.2%; P < .001), as well as a significant decrease in the proportion of persons with non-cirrhotic liver disease, from 39.0% in 2006 to 8.1% in 2014 (AAPC = –17.3; P < .001) (Figure 2). Among all-listed hepatitis C–associated ED visits by baby boomers, the proportion with compensated cirrhosis increased significantly, from 11.2% in 2006 to 18.0% in 2014 (AAPC = 6.3; P < .001), and the proportion with non-cirrhotic liver disease decreased significantly, from 71.9% in 2006 to 64.7% in 2014 (AAPC = –1.3; P < .001). The difference in the proportion of persons with end-stage liver disease was not significant.
Figure 2.
Distributions of liver disease severity among emergency department visits by baby boomers (born during 1945-1965) with first-listed (A) and all-listed (B) diagnosis of hepatitis C, United States, 2006-2014. Data are from the 2006-2014 Nationwide Emergency Department Sample (NEDS) survey.21 Visits are nationally representative by using the NEDS weights and sampling design. Trends were assessed by joinpoint analysis.
Discussion
Using nationally representative data, we found significant increases in numbers, rates, and costs of hepatitis C–associated ED visits during 2006-2014, indicating a large and increasing burden of ED-based HCV care in the United States. These increases occurred overall and among most subgroups examined, especially baby boomers, Medicare beneficiaries, and Medicaid beneficiaries. To our knowledge, this study is the first to highlight the rising trends and substantial shifting of demographic and clinical characteristics of ED-based HCV care in the United States. A better understanding of these changes could improve public health efforts in hepatitis C care and treatment in the ED.
For this analysis, we used both a narrow definition (first-listed diagnosis of hepatitis C) and a broad definition (all-listed diagnosis of hepatitis C) to capture data for HCV-infected persons presenting to EDs. Although the numbers of hepatitis C–associated ED visits according to the narrow definition were lower than those according to the broad definition, they had much higher rates of increase and larger proportions of hospitalization and cirrhosis. The narrow definition may reflect a subgroup of patients with severe medical conditions directly caused by HCV infection. We used the broad definition to reflect the total level of hepatitis C–associated ED visits. Using the all-listed diagnosis approach and the National Hospital Ambulatory Medical Care Survey (NHAMCS) data, Galbraith et al7 estimated 73 000 hepatitis C–associated ED visits annually (80.0 per 100 000 ED visits), which was substantially lower than our estimate of 581 350 visits (484.4 per 100 000 visits) in 2006. However, the authors indicated that they may have underdetected the number of hepatitis C–associated visits, particularly in the ED setting, because of the small number of diagnoses collected by NHAMCS (up to 3 diagnoses per visit). NEDS contains up to 30 diagnoses per visit, which would capture more hepatitis C–associated ED visits under the broad definition.
Reasons for the increase in hepatitis C–associated ED visits and changes in demographic characteristics and liver disease severity are likely multifactorial. Baby boomers account for up to 75% of all HCV infections in the United States.17 Because of HCV testing efforts,17 aging, entry of new patients who were waiting for more efficacious treatment, and progression of HCV-related liver diseases and other comorbid conditions among baby boomers, increasing numbers of this population may present to the ED for emergent complications of chronic HCV infection. In our study, we found that baby boomers accounted for most hepatitis C–associated ED visits and were one of the driving forces for the increasing trends in ED-based HCV care. The proportion of visits by baby boomers with compensated cirrhosis substantially increased, especially during 2006-2008, among ED visits by baby boomers, which may be a contributing factor to the large increase in the percentage of persons admitted to hospitals from the ED. Second, we found that the rate of ED-based HCV screening among the total ED population increased significantly (AAPC = 11.9; P < .001) during 2006-2014 (Supplementary Figure available at https://figshare.com/articles/Supplemental_Figure_Number_and_Rate_of_Emergency_Department_ED_Visits_with_Any_Hepatitis_C_Virus_HCV_Testing_Procedures_in_the_United_States_2006-2014/9 587 018), which could lead to a higher rate of ED use for HCV care. Third, Medicare and Medicaid beneficiaries constituted most hepatitis C–associated ED visits in our study, and the number of visits by these beneficiaries increased significantly from 2006 to 2014. Finally, the percentage of hepatitis C–associated ED visits by the younger cohort increased significantly during 2006-2014, which may reflect the increase of new HCV infections among young persons who used opioids during 2004-2014.30
Our findings underscore the need to develop effective policies and programs for ED-based HCV care, including screening, linkage to care, treatment, and prevention services. With the availability of direct-acting antiviral agents for HCV treatment, hepatitis C–associated conditions have become more manageable and preventable at primary care sites. However, our study indicates that hepatitis C–associated ED visits increased significantly through 2014, and many visits led to hospital admission. Reasons for an increase in hepatitis C–associated ED visits may include limited access to primary care service, poor insurance coverage, or delayed HCV treatment, with persons not presenting for care until after developing severe liver disease and its sequelae. Many ED visits could be prevented with aggressive early diagnosis and referral to care and treatment of hepatitis C in primary care or other health care settings, avoiding the substantially higher costs of ED visits and later hospitalization.
We found a significant increase in all-listed hepatitis C–associated ED visits among persons who left the ED against medical advice. This finding is concerning because discharges against medical advice are associated with short-term mortality and hospital readmission.31-33 Predictors of discharges against medical advice include younger age, having Medicaid or no insurance, current substance or alcohol use or a history of substance or alcohol use, and longer waiting time at the ED.31,34,35 HCV-related education, counseling, and linkage-to-care services are needed to prevent such premature discharges.
Limitations
This study had several limitations. First, because NEDS does not specify the primary reason for an ED visit, we based our estimates on diagnosis codes, which may be subject to potential bias. Second, NEDS does not cover non-community hospitals (eg, Veterans Administration hospitals). Thus, our study likely underestimated the true burden of ED-based HCV care. Third, because NEDS does not have laboratory data, we may have underestimated the cirrhosis levels among patients at EDs. The code lists that we used to define end-stage liver disease may be subject to inaccuracy. For example, the presence of esophageal varices without bleeding in some patients may not necessarily indicate decompensated cirrhosis or end-stage liver disease. In addition, NEDS collects data only at the visit level, and individual identifiers were not available. Thus, we conducted all analyses of demographic characteristics and liver disease severity at the visit level. We could not track patients’ ED use longitudinally. Further studies using other data sources are needed to examine hepatitis C–associated morbidity and mortality at the individual level in the ED.
Conclusion
The number, rate, and cost of hepatitis C–associated ED visits increased significantly from 2006 to 2014, especially among baby boomers, Medicare beneficiaries, and Medicaid beneficiaries. Increasing numbers of these patients had liver disease complications and were hospitalized after ED visits. Efforts to improve primary prevention, early HCV detection, linkage to care, and curative treatment among these patients at primary care settings are warranted to reduce the burden of HCV on the ED system.
Acknowledgments
The authors thank Scott D. Holmberg, MD, for his suggestions.
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shaoman Yin, PhD, MSPH  https://orcid.org/0000-0002-2633-6640
https://orcid.org/0000-0002-2633-6640
References
- 1. Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160(5):293–300. doi:10.7326/M13-1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62(5):1353–1363. doi:10.1002/hep.27978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Holmberg SD, Spradling PR, Moorman AC, Denniston MM. Hepatitis C in the United States. N Engl J Med. 2013;368(20):1859–1861. doi:10.1056/NEJMp1302973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating prevalence of hepatitis C virus infection in the United States, 2013-2016. Hepatology. 2019;69(3):1020–1031. doi:10.1002/hep.30297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ly KN, Hughes EM, Jiles RB, Holmberg SD. Rising mortality associated with hepatitis C virus in the United States, 2003-2013. Clin Infect Dis. 2016;62(10):1287–1288. doi:10.1093/cid/ciw111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grant WC, Jhaveri RR, McHutchison JG, Schulman KA, Kauf TL. Trends in health care resource use for hepatitis C virus infection in the United States. Hepatology. 2005;42(6):1406–1413. doi:10.1002/hep.20941 [DOI] [PubMed] [Google Scholar]
- 7. Galbraith JW, Donnelly JP, Franco RA, Overton ET, Rodgers JB, Wang HE. National estimates of healthcare utilization by individuals with hepatitis C virus infection in the United States. Clin Infect Dis. 2014;59(6):755–764. doi:10.1093/cid/ciu427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tsui JI, Maselli J, Gonzales R. Sociodemographic trends in national ambulatory care visits for hepatitis C virus infection. Dig Dis Sci. 2009;54(12):2694–2698. doi:10.1007/s10620-008-0659-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Galbraith JW, Franco RA, Donnelly JP, et al. Unrecognized chronic hepatitis C virus infection among baby boomers in the emergency department. Hepatology. 2015;61(3):776–782. doi:10.1002/hep.27410 [DOI] [PubMed] [Google Scholar]
- 10. Anderson ES, Galbraith JW, Deering LJ, et al. Continuum of care for hepatitis C virus among patients diagnosed in the emergency department setting [published erratum appears in Clin Infect Dis. 2017;65(8):1431-1433]. Clin Infect Dis. 2017;64(11):1540–1546. doi:10.1093/cid/cix163 [DOI] [PubMed] [Google Scholar]
- 11. White DA, Anderson ES, Pfeil SK, Trivedi TK, Alter HJ. Results of a rapid hepatitis C virus screening and diagnostic testing program in an urban emergency department. Ann Emerg Med. 2016;67(1):119–128. doi:10.1016/j.annemergmed.2015.06.023 [DOI] [PubMed] [Google Scholar]
- 12. Allison WE, Chiang W, Rubin A, et al. Hepatitis C virus infection in the 1945-1965 birth cohort (baby boomers) in a large urban ED. Am J Emerg Med. 2016;34(4):697–701. doi:10.1016/j.ajem.2015.12.072 [DOI] [PubMed] [Google Scholar]
- 13. Lyons MS, Kunnathur VA, Rouster SD, et al. Prevalence of diagnosed and undiagnosed hepatitis C in a Midwestern urban emergency department. Clin Infect Dis. 2016;62(9):1066–1071. doi:10.1093/cid/ciw073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anderson ES, Pfeil SK, Deering LJ, Todorovic T, Lippert S, White DA. High-impact hepatitis C virus testing for injection drug users in an urban ED. Am J Emerg Med. 2016;34(6):1108–1111. doi:10.1016/j.ajem.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 15. Fairbairn N, Milloy MJ, Zhang R, et al. Emergency department utilization among a cohort of HIV-positive injecting drug users in a Canadian setting. J Emerg Med. 2012;43(2):236–243. doi:10.1016/j.jemermed.2011.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kelen GD, Green GB, Purcell RH, et al. Hepatitis B and hepatitis C in emergency department patients. N Engl J Med. 1992;326(21):1399–1404. doi:10.1056/NEJM199205213262105 [DOI] [PubMed] [Google Scholar]
- 17. Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965 [published erratum appears in MMWR Recomm Rep. 2012;61(43):886]. MMWR Recomm Rep. 2012;61(RR-4):1–32. [PubMed] [Google Scholar]
- 18. Klevens RM, Hu DJ, Jiles R, Holmberg SD. Evolving epidemiology of hepatitis C virus in the United States. Clin Infect Dis. 2012;55(suppl 1):S3–S9. doi:10.1093/cid/cis393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moyer VA, US Preventive Services Task Force. Screening for hepatitis C virus infection in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(5):349–357. doi:10.7326/0003-4819-159-5-201309030-00672 [DOI] [PubMed] [Google Scholar]
- 20. Ghany MG, Liang TJ. Current and future therapies for hepatitis C virus infection. N Engl J Med. 2013;369(7):679–680. doi:10.1056/NEJMc1307589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project. Overview of the Nationwide Emergency Department Sample (NEDS). 2006-2014. Modified June 2019 http://www.hcup-us.ahrq.gov/nedsoverview.jsp . Accessed August 1, 2017.
- 22. Senathirajah M, Owens P, Mutter R, Nagamine M. Special Study on the Meaning of the First-Listed Diagnosis on Emergency Department and Ambulatory Surgery Records. HCUP Methods Series. Report # 2011-03 Rockville, MD: US Agency for Healthcare Research and Quality; 2011; https://www.hcup-us.ahrq.gov/reports/methods/2011_03.pdf. Accessed July 22, 2019. [Google Scholar]
- 23. Centers for Disease Control and Prevention, National Center for Health Statistics. International classification of diseases, ninth revision, clinical modification (ICD-9-CM). Updated 2015 https://www.cdc.gov/nchs/icd/icd9 cm.htm. Accessed May 12, 2017.
- 24. Agency for Healthcare Research and Quality. HCUP NEDS description of data elements. Healthcare Cost and Utilization Project (HCUP). 2015. https://hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nedsnote.jsp . Accessed August 15, 2017.
- 25. US Department of Labor, Bureau of Labor Statistics. Consumer Price Index: measuring price change in the CPI: medical care. Modified April 2019 https://www.bls.gov/cpi/factsheets/medical-care.htm. Accessed February 10, 2018.
- 26. Gordon SC, Pockros PJ, Terrault NA, et al. Impact of disease severity on healthcare costs in patients with chronic hepatitis C (CHC) virus infection [published erratum appears in Hepatology. 2013;58(3):1193]. Hepatology. 2012;56(5):1651–1660. doi:10.1002/hep.25842 [DOI] [PubMed] [Google Scholar]
- 27. Kanwal F, Hoang T, Kramer JR, et al. Increasing prevalence of HCC and cirrhosis in patients with chronic hepatitis C virus infection. Gastroenterology. 2011;140(4):1182–1188.e1. doi:10.1053/j.gastro.2010.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McAdam-Marx C, McGarry LJ, Hane CA, Biskupiak J, Deniz B, Brixner DI. All-cause and incremental per patient per year cost associated with chronic hepatitis C virus and associated liver complications in the United States: a managed care perspective. J Manag Care Pharm. 2011;17(7):531–546. doi:10.18553/jmcp.2011.17.7.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. SAS System for Windows [statistical software]. Release 9.4 Cary, NC: SAS Institute, Inc; 2013. [Google Scholar]
- 30. Zibbell JE, Asher AK, Patel RC, et al. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am J Public Health. 2018;108(2):175–181. doi:10.2105/AJPH.2017.304132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983 doi:10.1136/bmj.d2983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125(6):594–602. doi:10.1016/j.amjmed.2011.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43(7):798–802. doi:10.1111/imj.12109 [DOI] [PubMed] [Google Scholar]
- 34. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255–260. doi:10.1016/S0025-6196(11)61143-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. Discharge against medical advice in the United States, 2002-2011. Mayo Clin Proc. 2017;92(4):525–535. doi:10.1016/j.mayocp.2016.12.022 [DOI] [PubMed] [Google Scholar]