Abstract
Objectives:
Racial differences in mortality in the United States have narrowed and vary by time and place. The objectives of our study were to (1) examine the gap in life expectancy between white and black persons (hereinafter, racial gap in life expectancy) in 4 states (California, Georgia, Illinois, and New York) and (2) estimate trends in the contribution of major causes of death (CODs) to the racial gap in life expectancy by age group.
Methods:
We extracted data on the number of deaths and population sizes for 1969-2013 by state, sex, race, age group, and 6 major CODs. We used a Bayesian time-series model to smooth and impute mortality rates and decomposition methods to estimate trends in sex- and age-specific contributions of CODs to the racial gap in life expectancy.
Results:
The racial gap in life expectancy at birth decreased in all 4 states, especially among men in New York (from 8.8 to 1.1 years) and women in Georgia (from 8.0 to 1.7 years). Although few deaths occurred among persons aged 1-39, racial differences in mortality at these ages (mostly from injuries and infant mortality) contributed to the racial gap in life expectancy, especially among men in California (1.0 year of the 4.3-year difference in 2013) and Illinois (1.9 years of the 6.7-year difference in 2013). Cardiovascular deaths contributed most to the racial gap in life expectancy for adults aged 40-64, but contributions decreased among women aged 40-64, especially in Georgia (from 2.8 to 0.5 years). The contribution of cancer deaths to inequality increased in California and Illinois, whereas New York had the greatest reductions in inequality attributable to cancer deaths (from 0.6 to 0.2 years among men and from 0.2 to 0 years among women).
Conclusions:
Future research should identify policy innovations and economic changes at the state level to better understand New York’s success, which may help other states emulate its performance.
Keywords: mortality, race, inequality
Racial differences in mortality in the United States have long been a bellwether of progress in equity and justice, with a narrowing gap in mortality over time reflecting improvements in access to healthy environments, nutrition, and medical care.1 Moreover, differences among states in these inequalities reflect changing demographic, social, and economic circumstances, as well as changes in diverse policies such as housing, incarceration, and medical insurance programs.2 Few studies have considered state-specific differences, in part because of the challenge of reporting results for the large number of states that have sizable black populations.
One study that used mortality data from 1997-2004 found large gaps in life expectancy between black and white Americans (hereinafter, racial gap in life expectancy) for a handful of states, mostly in the Rust Belt and the Midwest.3 Washington, DC, although not a state, also ranked among the most unequal states in racial gaps in life expectancy. Another study that examined racial gaps in life expectancy during 1990-2009 found that New York and Florida made the biggest contributions to overall national improvement and California hindered progress, because gains in life expectancy among black persons occurred more slowly there than in other states.2 Several studies focused on racial differences in life expectancy at the county level4 or city level.5 Focusing on states instead of smaller units provides more stable mortality estimates from year to year. Many health, economic, and social policies are set at the state level6; as such, patterns of racial inequality in life expectancy at the state level over time can reveal the effects of policy innovation more directly than can patterns at a finer level of aggregation.7
The objective of our study was to expand on this previous description of state-specific trends by analyzing state-level differences in the contributions of various age groups and causes of death (CODs) to changes in racial gaps in life expectancy during 1969-2013. To avoid the multiplicity of results that would result from including all states, and the uncertainty due to smaller black populations in many states, we examined 4 large, geographically diverse states: California, Georgia, Illinois, and New York. Each state has a major city: New York, New York; Los Angeles, California; Chicago, Illinois; and Atlanta, Georgia, are the first, second, third, and ninth largest urban centers in the United States, respectively. In addition, more than one-quarter of the black population in the United States lives in these 4 states. They also cover historically distinct regions: Midwest, Northeast, South, and West, and all 4 states have large urban and rural populations.
Methods
Data
We extracted data on the number of deaths, CODs, and demographic characteristics from the National Cancer Institute’s SEER*Stat software program, the data for which are provided by the US National Vital Statistics System.8 We used annual data on the number of deaths for non-Hispanic and Hispanic black and white persons by year (1969-2013), by sex (male, female), and by 5-year age groups (except for the groups <1, 1-4, and ≥85). We used bridged-race intercensal population denominators. We grouped the number of deaths for each state-year-race-sex-age stratum according to 6 broad CODs: cardiovascular disease (CVD), cancer, noncommunicable disease, injury, communicable disease, and all other causes (exact causes contributing to each category are provided in Supplementary Table 1, which is available at https://github.com/corinne-riddell/BlackWhiteMortalityGap/blob/master/Manuscript2/Supplementary-appendix.pdf). If the cause-specific number of deaths was 1 through 9, the National Center for Health Statistics suppressed these values. Death counts of 0 or >9 were known exactly but may be unstable over time for small strata.9
Statistical Analysis
To account for unstable estimates and data suppression, we used a Bayesian time-series analysis, described elsewhere.10 Briefly, we used a Bayesian generalized linear model based on a Poisson likelihood for nonmissing death rates and a truncated Poisson likelihood for cells with counts of 1 to 9 deaths, which were suppressed. This analysis yielded mean log-mortality rates that we used to estimate smoothed and imputed death counts for each state-year-race-sex stratum over time. Using data on these deaths, we calculated life expectancy at birth separately for the 4 groups defined by race and sex. We also calculated the absolute difference in life expectancy, and we used Arriaga’s decomposition method to partition the difference between races by age and COD.11,12 Arriaga’s decomposition method divides the total gap in life expectancy into components attributable to each age and COD group. For example, for a life expectancy gap of 4 years, 1.5 years of the gap may be attributed to black-white differences in cardiovascular mortality among adults aged 40-45. To visualize these results, we collapsed smaller age groups that were used for computation into 6 broader groups (<1, 1-19, 20-39, 40-64, 65-84, and ≥85 years) and summed the decomposition results within these groups.
To aid in the interpretation of our primary findings, we also conducted sensitivity analyses of the imputation strategy. For the sensitivity analyses, we calculated cause- and age-specific mortality rates for the 4 race-by-sex groups by using the raw data, which contain suppressed deaths when cell counts were small. We then applied 3 simple imputations as extreme scenarios to assess the potential effect of the imputation used in the primary analysis. This assessment involved setting all suppressed counts to 1 (minimum), 5 (midpoint), or 9 (maximum). Because the 4 selected states all had large black populations and large white populations, these imputations resulted in overlapping mortality trends for nearly all age–COD groupings that contribute importantly to mortality. We used R statistical software for all analyses. The data sets analyzed for the current study and all of the analysis codes used are available at https://github.com/corinneriddell/BlackWhiteMortalityGap. This study used publicly accessible data; as such, institutional review board review was not required.
Results
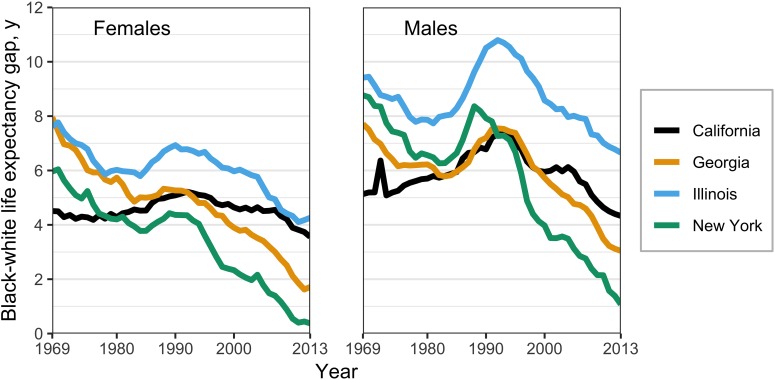
The racial gap in life expectancy declined substantially for both sexes from 1969 to 2013, with notable differences by state (Figure 1). Although California had the smallest difference in the racial gap in life expectancy in 1969 (4.5 years for women and 5.1 years for men), it showed the slowest progress among these 4 states: the gap declined by only about 1 year of life expectancy for women and men. Conversely, the racial gap in life expectancy in New York decreased substantially during the study period, by about 5 years for women (from 6.0 years to 0.4 years) and 8 years for men (from 8.8 years to 1.1 years). Inequalities were exacerbated, particularly for men, in all 4 states in the mid-1980s through the early-1990s, followed by a steady decline through 2013. Illinois had the largest racial gap in life expectancy throughout the study period. For example, black men had a life expectancy deficit of >6 years relative to white men (70.5 years vs 77.6 years) in 2013.
Figure 1.
Gaps in life expectancy from birth between black and white persons in 4 US states, by sex, 1969-2013. The peak in California’s trend line in 1972 for men resulted from a low number of deaths due to cardiovascular disease among white men, which resulted from a coding error in the cause-of-death information in the vital statistics system; thus, caution should be taken in interpreting the gap in life expectancy between black and white men in California in 1972. Data source: Riddell et al.10
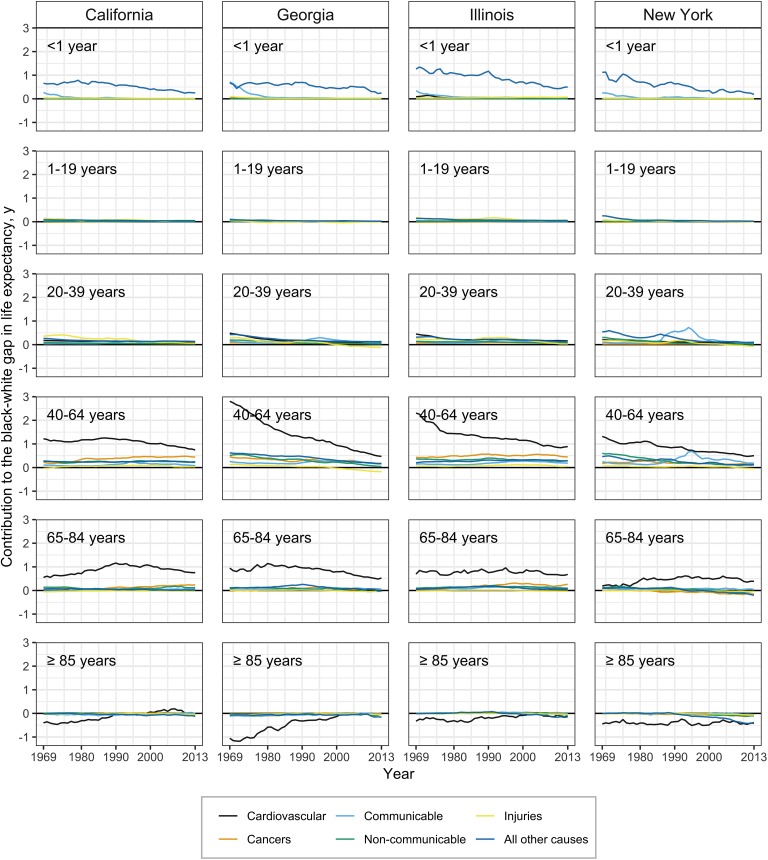
The contribution of infant mortality to the racial gap in life expectancy among women decreased to less than one-third of a year in all states except Illinois, where it was 0.6 years in 2013 (Figure 2). In all 4 states, the infant mortality rate decreased more quickly among black infants than among white infants; the largest decreases in black infant mortality were in New York and Illinois, the states that had the largest initial inequalities in life expectancy (supplemental Figures 1 and 2 are available at https://github.com/corinne-riddell/BlackWhiteMortalityGap/blob/master/Manuscript2/Supplementary-appendix.pdf).
Figure 2.
Contribution of age and cause of death to gaps in life expectancy between black and white females in California, Georgia, Illinois, and New York, 1969-2013. Negative contributions indicate lower age-specific mortality rates among black women compared with white women for the specified cause. Data source: Riddell et al.10
Cardiovascular CODs, primarily among adults aged 40-64, were the leading contributor to the racial gap in life expectancy among women for all years. However, their contribution to the racial gap in life expectancy declined in all 4 states, most notably in Georgia, where the contribution of CVD declined from 4.3 years to 1.4 years for women. CVD deaths among women aged 65-84, compared with CVD deaths among younger women, contributed less to the racial gap in life expectancy in the earlier years of the study data but changed less rapidly over time. By 2013, the contribution of CVD to the racial gap in life expectancy was similar in absolute terms among women aged 40-64 and 65-84: <1 year in each state. Thus, the contribution to the gap was similar for the 2 age groups even though absolute CVD death rates were substantially higher among older women than among younger women. For ages ≥85, white women generally had higher CVD mortality rates than black women. Consequently, CVD deaths in this age group generally narrowed the racial gap in life expectancy. However, CVD mortality rates for black and white women aged ≥85 trended more closely during the mid-2000s, with the contribution of women aged ≥85 being close to 0 by 2013 in all states except New York, where black women aged ≥85 maintained an advantage in CVD mortality over white women aged ≥85.
The contributions of the remaining CODs to the racial gap in life expectancy were small. Notably, all 6 CODs contributed to the racial gap in life expectancy for women aged 40-64 in California and Illinois, with cancer contributing a half-year to the gap among that age group. Although the contribution of cancer deaths to the racial gap in life expectancy was nearly eliminated or reversed for women in Georgia and New York by 2013, black-white differences in cancer mortality in 2013 still accounted for 0.7 years of the racial gap in life expectancy among women in California and 0.8 years in Illinois. Injury mortality among white women aged 40-64 increased from 2000 to 2013, which narrowed the racial gap in life expectancy in all 4 states.13
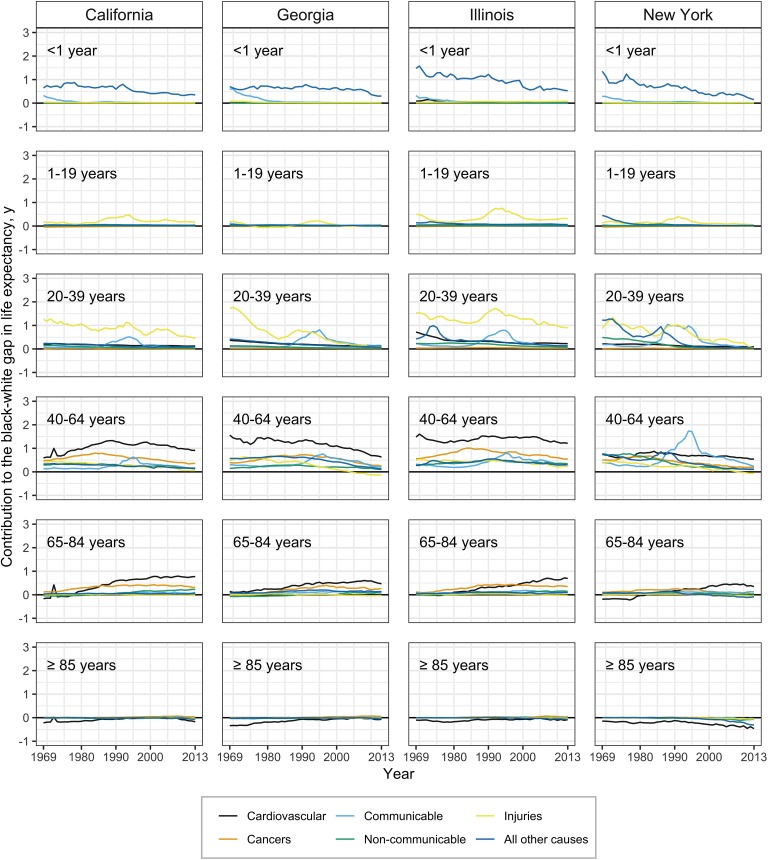
Comparable changes occurred during the study period by state in the contributions of CODs in each age group to the racial gap in life expectancy for men (Figure 3). The contribution of infant mortality differences in 1969 was largest in New York (1.7 years) and Illinois (1.9 years). During subsequent decades, New York largely eliminated infant mortality as a contributor to the racial gap in life expectancy (0.2 years in 2013), whereas Illinois maintained a contribution to the racial gap in life expectancy of 0.7 years in 2013.
Figure 3.
Contribution of age and cause of death to gaps in life expectancy among black and white males in California, Georgia, Illinois, and New York, 1969-2013. In New York, communicable diseases contributed approximately 2 years to the gap in life expectancy between black and white males in 1995 (during the HIV/AIDS epidemic) vs 0.75 years in Illinois at the same time. Negative contributions indicate lower age-specific mortality rates among black males compared with white males for the specified cause. The spike in the contribution of cardiovascular disease (CVD) to the gap in life expectancy between black and white males in 1972 resulted from a low number of CVD deaths to white men in that year, which was likely the result of a coding error in the cause-of-death information in the vital statistics system; thus, caution should be taken in interpreting California’s CVD estimate in 1972. Data source: Riddell et al.10
Injuries contributed most to the racial gap in life expectancy between young black and white men in all 4 states, particularly Illinois, where injuries accounted for 3 years of the racial gap in life expectancy in the early 1990s.14 Communicable causes also dominated during adulthood during the 1990s, particularly in New York. Mortality from communicable diseases at that time sharply increased for black and white men, but it was twofold to fivefold higher among black men aged 40-64 than among their white counterparts (see Supplemental Figure 11 in the supplementary appendix at https://github.com/corinne-riddell/BlackWhiteMortalityGap/blob/master/Manuscript2/Supplementary-appendix.pdf).
For men aged 40-64, cardiovascular CODs dominated throughout the time period, with the CVD contribution in California, Georgia, and Illinois being more than double the other CODs examined in 2013. For men aged 65-84, CVD contributed increasingly to racial gaps in life expectancy as other causes tended toward racial equality. Age-specific mortality rates showed that black men aged 65-84 had lower or equal CVD mortality in 1969 compared with white men, but white men had larger mortality reductions over time that resulted in an excess risk to black men near 500 per 100 000 population in all states except New York (see Supplementary Figure 8 in the supplementary appendix at https://github.com/corinne-riddell/BlackWhiteMortalityGap/blob/master/Manuscript2/Supplementary-appendix.pdf). Black men had lower CVD mortality than white men among the oldest age group and contributed to narrowing the racial gap in life expectancy, most notably in New York.
Cancer’s contribution to the racial gap in life expectancy peaked around 1985 among men aged 40-64, at which time cancer mortality decreased for black and white men. The racial mortality gap was eliminated by 2013 in New York but not in the other 3 states.
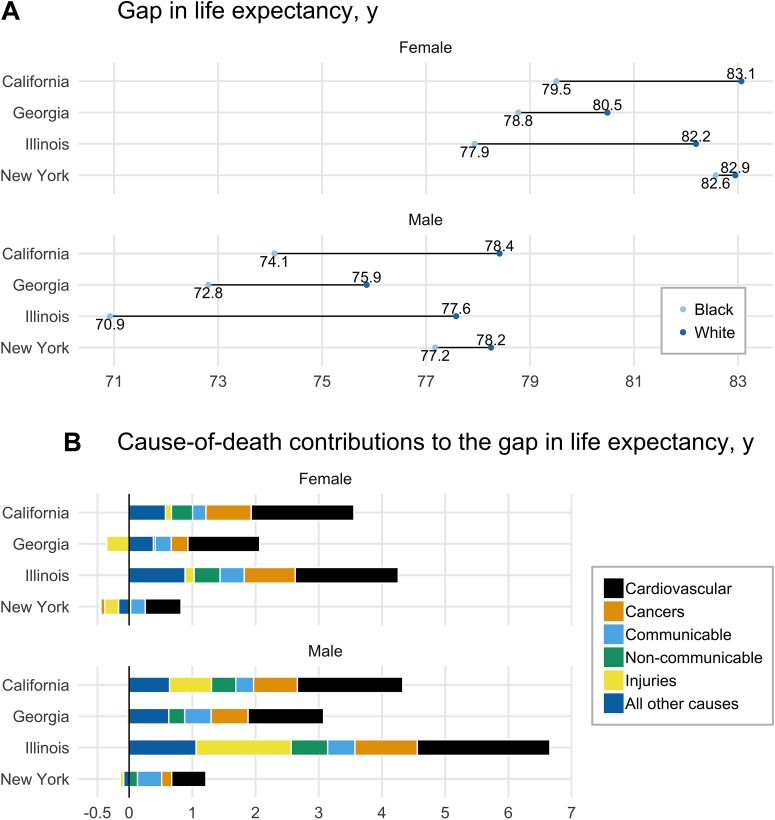
By 2013, gaps in absolute life expectancy declined for women and men in all 4 states overall, as well as by COD (Figure 4). The near equality of life expectancy in New York by 2013 differed from the black disadvantage in life expectancy in the other 3 states. Georgia had the lowest life expectancy overall but the second smallest racial gap in life expectancy (1.7 years for women and 3 years for men) after New York. Illinois had the most persistent racial gap in life expectancy of the 4 states; white life expectancy fared about as well as in other states, but black life expectancy lagged. Excess deaths caused by CVD made the largest contribution to the remaining racial gap in life expectancy in all 4 states, but cancer and infant mortality, which comprised most deaths in the “all other causes” group, contributed substantially to the racial gap in life expectancy in Illinois, Georgia, and California. For women in New York and Georgia, injury deaths contributed to a narrowing of the racial gap in life expectancy by 2013 but exacerbated the racial gap in life expectancy observed among men in Illinois and California.
Figure 4.
Gaps in life expectancy between black and white males and black and white females and the contribution of major causes of death, California, Georgia, Illinois, and New York, 2013. In Panel B, causes to the right of the vertical black line contribute to widening the gaps in life expectancy between black and white persons and causes to the left contribute to narrowing the gap. The net effect of the cause-of-death contributions to the left and right of the vertical line equals the gap in life expectancy shown in Panel A.
Cardiovascular deaths made persistent contributions to the racial gap in life expectancy in all 4 states, and the contribution of infant mortality in Illinois was twice as high as that in the other 3 states. The negative contribution of all causes in the group aged ≥85 was most striking in New York.
Discussion
We found that state-specific trends were generally consistent with the overall progress in narrowing racial gaps in life expectancy from 1969 to 2013 in the United States. At the same time, disparate patterns of change were also evident in all 4 states. For men and women, life expectancy was more similar across states among white persons than among black persons. One study attributed this shorter life expectancy among black persons to lower age at death from each major cause rather than to a different distribution of causes.15 Two notable exceptions to this pattern were homicide and suicide. In 2016, rates of homicide were 10-fold higher among non-Hispanic black men than among non-Hispanic white men, and rates of suicide were 2.5 times higher among non-Hispanic white men than among non-Hispanic black men.16 The patterns may also reflect to some extent various historical patterns of migration between states in these cohorts. For example, the major migration of black persons from the South to the North in the first half of the 20th century lowered life expectancy in the South through selective departure of the healthiest segments of the population.17
Progress in reducing racial gaps in life expectancy has been especially pronounced in the new millennium, after a period in the 1990s in which homicide and AIDS exacerbated racial inequalities in urban centers such as Chicago and New York.18 Since the year 2000, reductions in racial inequalities in CVD played an important role in continuing to drive down the racial gap in life expectancy, particularly among women in California, Georgia, and Illinois. Nevertheless, CVD in late middle age continues to make the largest contribution to the racial gap in life expectancy, and much of this differential contribution to years of life lost is attributable to observed differences in known risk factors such as smoking, obesity, and elevated blood pressure and blood glucose.19 In addition to CVDs, differential trends in death rates from injuries since 2000 have helped to decrease the racial gap in life expectancy in all 4 states, although this decrease is largely due to adverse consequences of the opioid epidemic’s larger effect on white persons than on black persons. Given the recent uptick in opioid overdose deaths among black persons (particularly due to heroin and synthetic opioids),20 it is unclear whether this pattern will persist in the future.
Strengths
This study had several strengths. First, we engaged in population surveillance. As such, variability was not associated with sampling in the statistics reported, and we did not need to calculate P values or confidence intervals. Second, we focused on populous states to show stable estimates based on large numbers of deaths, and we showed in sensitivity analyses that the results were not affected by data suppression in sparse cells. Lastly, we showed results on the absolute scale, because differences can become misleading in relative terms when baseline rates are obscured. The absolute scale also provided ready decomposition of life expectancy by component causes in an additive fashion and avoided the false impression that inequality can widen when both groups are improving.21
Limitations
This study also had several limitations. First, to provide a detailed picture of the most recent 45 years of data, we focused on only 4 states. As such, the results do not necessarily reflect trends in all 50 states and Washington, DC. Second, we did not separate Hispanic persons from black and white persons because their contribution to America’s racial dichotomy is complex and evolving.22 Moreover, it was not possible to separate data on Hispanic persons from data on non-Hispanic black and non-Hispanic white persons during the study period because of inconsistent coding across states.23 Black Hispanic persons compose <5% of US black persons overall but up to 25% of black persons in New York State.24 Among persons classified in our study as white, the largest proportion who were Hispanic were likely to be in California, where more than one-third of residents are Hispanic, a percentage more than twice as high as in the other states we examined. As such, ignoring the dimensions of ethnicity could be viewed as obscuring an important source of within-group variability in risk factors and CODs. Third, we relied on COD coding that is known to be prone to errors, and these errors may potentially differ by race and state.25 For example, deaths in rural areas compared with urban areas may, in general, have more errors in age of decedent and COD, and Georgia has a substantial rural black population. When misclassification is differential, the direction of the bias cannot be predicted, which adds uncertainty to the estimates. As such, it is not possible to say that cause-specific rates are over- or underestimated in a given year, state, or group. Nevertheless, some evidence suggests more consistency in COD coding for black and white persons than for Hispanic persons.26 Although numerous studies have documented errors in age reporting among very old persons, and differentially more error in age reporting for black persons than for white persons, this differential error was unlikely to have affected our estimates substantially. Almost all misreporting errors were small until after age 85, and we used a single category for age ≥85 in the estimation and decomposition of life expectancy.27
Conclusions
We found important divergence in racial gaps in life expectancy across the 4 states, and even more so when we broke down the gaps further by broadly categorized dimensions of age and CODs. These patterns demonstrate that black-white differences in mortality can be eliminated or reversed, but progress toward equality has been differential across state environments. Future research should estimate the effects of policy innovations and economic changes on closing racial gaps in life expectancy. The arc of racial justice is long, but it bends toward equality. In some states, it bends more rapidly or substantially than in others, and these differences are important clues that need to be understood for the benefit of all persons in all states.
Footnotes
Availability of data and material: The data sets analyzed for the current study and the analysis code used are available at https://github.com/corinneriddell/BlackWhiteMortalityGap. An online appendix to this paper can be found at: https://github.com/corinne-riddell/BlackWhiteMortalityGap/blob/master/Manuscript2/Supplementary-appendix.pdf.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jay S. Kaufman, PhD  https://orcid.org/0000-0003-1606-401X
https://orcid.org/0000-0003-1606-401X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Hummer RA, Chinn JJ. Race/ethnicity and US adult mortality: progress, prospects, and new analyses. Du Bois Rev. 2011;8(1):5–24. doi:10.1017/S1742058X11000051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990-2009. Health Aff (Millwood). 2014;33(8):1375–1382. doi:10.1377/hlthaff.2013.1273 [DOI] [PubMed] [Google Scholar]
- 3. Bharmal N, Tseng CH, Kaplan R, Wong MD. State-level variations in racial disparities in life expectancy. Health Serv Res. 2012;47(1 pt 2):544–555. doi:10.1111/j.1475-6773.2011.01345.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Murray CJ, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States [published erratum appears in PLoS Med. 2006;3(12):e545]. PLoS Med. 2006;3(9):e260 doi:10.1371/journal.pmed.0030260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Benjamins MR, Hirschtick JL, Hunt BR, Hughes MM, Hunter B. Racial disparities in heart disease mortality in the 50 largest U.S. cities. J Racial Ethn Health Disparities. 2017;4(5):967–975. doi:10.1007/s40615-016-0300-6 [DOI] [PubMed] [Google Scholar]
- 6. Montez JK. Deregulation, devolution, and state preemption laws’ impact on US mortality trends. Am J Public Health. 2017;107(11):1749–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Volden C. States as policy laboratories: emulating success in the children’s health insurance program. Am J Polit Sci. 2006;50(2):294–312. [Google Scholar]
- 8. National Cancer Institute. SEER*Stat. [software]. Release 8.3.2. Bethesda, MD: National Cancer Institute; 2017. [Google Scholar]
- 9. National Cancer Institute. Surveillance, Epidemiology, and End Results Program: US mortality data, 1969-2016. https://seer.cancer.gov/mortality. Accessed May 16, 2017.
- 10. Riddell CA, Morrison KT, Kaufman JS, Harper S. Trends in the contribution of major causes of death to the black-white life expectancy gap by US state. Health Place. 2018;52:85–100. doi:10.1016/j.healthplace.2018.04.003 [DOI] [PubMed] [Google Scholar]
- 11. Arriaga EE. Measuring and explaining the change in life expectancies. Demography. 1984;21(1):83–96. [PubMed] [Google Scholar]
- 12. Arriaga EE. Changing trends in mortality declines during the last decades In: Ruzicka L, Wunsch G, Kane P, eds. Differential Mortality: Methodological Issues and Biosocial Factors. Oxford: Clarendon Press; 1989:105–129. [Google Scholar]
- 13. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010-2015 [published erratum appears in MMWR Morb Mortal Wkly Rep. 2017;66(1):35]. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445–1452. [DOI] [PubMed] [Google Scholar]
- 14. Fagan J, Richman D. Understanding recent spikes and longer trends in American murders. Columbia Law Rev. 2017;117(5):1235–1296. [Google Scholar]
- 15. Firebaugh G, Acciai F, Noah AJ, Prather C, Nau C. Why lifespans are more variable among blacks than among whites in the United States. Demography. 2014;51(6):2025–2045. doi:10.1007/s13524-014-0345-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Center for Health Statistics. Underlying cause of death, 1999-2017. https://wonder.cdc.gov/ucd-icd10.html. Accessed January 17, 2018.
- 17. Black DA, Sanders SG, Taylor EJ, Taylor LJ. The impact of the Great Migration on mortality of African Americans: evidence from the Deep South. Am Econ Rev. 2015;105(2):477–503. doi:10.1257/aer.20120642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Obiri GU, Fordyce EJ, Singh TP, Forlenza S. Effect of HIV/AIDS versus other causes of death on premature mortality in New York City, 1983-1994. Am J Epidemiol. 1998;147(9):840–845. doi:10.1093/oxfordjournals.aje.a009537 [DOI] [PubMed] [Google Scholar]
- 19. Danaei G, Rimm EB, Oza S, Kulkarni SC, Murray CJ, Ezzati M. The promise of prevention: the effects of four preventable risk factors on national life expectancy and life expectancy disparities by race and county in the United States. PLoS Med. 2010;7(3):e1000248 doi:10.1371/journal.pmed.1000248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alexander MJ, Kiang MV, Barbieri M. Trends in black and white opioid mortality in the United States, 1979-2015. Epidemiology. 2018;29(5):707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bond MJ, Herman AA. Lagging life expectancy for black men: a public health imperative. Am J Public Health. 2016;106(7):1167–1169. doi:10.2105/AJPH.2016.303251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Borrell LN, Lancet EA. Race/ethnicity and all-cause mortality in US adults: revisiting the Hispanic paradox. Am J Public Health. 2012;102(5):836–843. doi:10.2105/AJPH.2011.300345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat 2. 1999;128:1–13. [PubMed] [Google Scholar]
- 24. Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. March 2011 https://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed June 12, 2019.
- 25. Johns LE, Madsen AM, Maduro G, Zimmerman R, Konty K, Begier E. A. case study of the impact of inaccurate cause-of-death reporting on health disparity tracking: New York City premature cardiovascular mortality. Am J Public Health. 2013;103(4):733–739. doi:10.2015/AJPH.2012.300683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arias E, Eschbach K, Schauman WS, Backlund EL, Sorlie PD. The Hispanic mortality advantage and ethnic misclassification on US death certificates. Am J Public Health. 2010;100(suppl 1):S171–S177. doi:10.2105/AJPH.2008.135863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Black DA, Hsu YC, Sanders SG, Schofield LS, Taylor LJ. The Methuselah effect: the pernicious impact of unreported deaths on old-age mortality estimates. Demography. 2017;54(6):2001–2024. doi:10.1007/s13524-017-0623-x [DOI] [PMC free article] [PubMed] [Google Scholar]