Abstract
Background
Germany has more intensive care unit (ICU) beds per capita than the USA, but the utilization of these resources at the end of life is unknown.
Methods
Retrospective observational study using nationwide German hospital discharge data (DRG statistics; DRG, diagnosis-related groups) from 2007 to 2015. We investigated hospital deaths and use of intensive care services during terminal hospitalizations. Population-based incidences were standardized to the age and sex distribution of the German population.
Results
Standardized hospital admission rates increased by 0.8% annually (from 201.9 to 214.6 per 1000 population), while hospital admissions involving ICU care increased by 3.0% annually (from 6.5 to 8.2 per 1000 population). Among all deaths in the German population, the proportion of hospital deaths with ICU care increased by 2.3% annually (from 9.8% to 11.8%). Among all hospital deaths, the proportion involving ICU care increased by 2.8% annually from 20.6% (2007) to 25.6% (2015). In patients aged 65 and older, the use of intensive care services during terminal hospitalizations increased 3 times faster than hospital deaths.
Conclusion
Use of intensive care services during terminal hospitalizations increased across all age groups, particularly the elderly. The increased need for end-of-life care in the ICU calls for improvements in educational, policy, and reimbursement strategies. It is unclear whether ICU care was appropriate and compliant with patient preferences.
Healthcare systems in high-income countries are challenged by a growing population of elderly patients with increasing comorbidities and rising demand for technologically advanced care. These trends raise questions about the appropriate use of intensive care services at the end of life.
When faced with a serious illness, most people prefer to die at home (1). In contrast, intensive therapy signifies some of the most aggressive aspects of care, which can potentially worsen the experience of death for patients and their families and may increase burnout and distress among ICU personnel (2, 3). On the other hand, intensive care can stabilize an acute life-threatening condition and some intensive palliative treatments may be better performed in an ICU when patients are in crisis. Importantly, providing high-quality end-of-life care requires skills in decision-making and communication and the collaboration of a well-functioning interdisciplinary team (2).
In Germany, models predict that the total number of deaths will rise by 26.0% from 2009 to 2050 (4). Approximately 50% of Germans die in hospital (5). In 2004–2005, Germany had a higher rate of ICU admissions/100 000 population than the USA and 6–10 times more ICU admissions than Canada, the Netherlands, or the UK (6). USA data suggest increasing ICU care at the end of life: between 2000 and 2009, the proportion of deaths among patients = 66 years with ICU treatment in the last month of life grew from 24.3% to 29.2% (7). There are also indications that the use of intensive care at the end of life in this age group is directly linked to ICU capacity (8).
Little is known about the use of intensive care at the end of life in Germany. The goal of this study is to examine trends in hospital deaths and use of intensive care services during terminal hospitalizations. The results provide information on the scope and trends of intensive care use at the end of life for policy makers, clinicians, patients, and relatives.
Methods
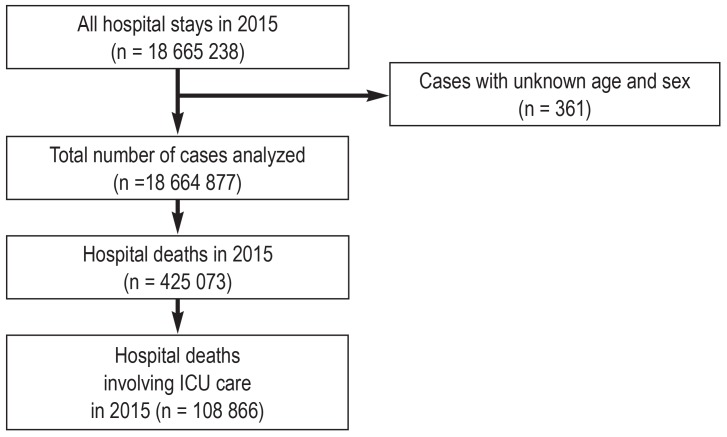
Details of study methodology can be found in the eMethods. In short, we used the German diagnosis-related groups (DRG) statistics for the analysis of hospitalizations with and without intensive care. We used the population and deaths statistics of the German Federal Statistical Office and data on hospital/ICU beds from the Federal Health Monitoring Service. We identified patients of all ages between 2007 and 2015 and excluded cases with unknown age and sex (figure 1). We opted for a conservative approach to identify ICU treatment by codes for operations and procedures (OPS codes 8–980, 8–98c, 8–98d, 8–98f, = intensive care complex treatment). Use of intensive care services during terminal hospitalizations was determined by the number of patients who died in hospital and received ICU care at any time during their hospital stay. We calculated annual population-based incidences and standardized these to the German population structure according to the age and sex distribution as of 31 December 2007 based on nationwide population data of the Federal Statistical Office for 2007–2015.
Figure 1.
Flow chart showing case identification and absolute numbers of cases in 2015
Results
Development of ICU bed numbers
Between 2007 and 2015, the number of ICU beds increased by a mean of 2.06% per annum (p.a.), from 23 357 to 27 489. In contrast, the number of hospitals and hospital beds declined by a mean of 0.81% and 1.1% p.a., respectively (etable 1).
eTable 1. Development of ICU beds.
| Total number of hospitals |
Hospitals with beds for intensive care |
Hospital beds |
Beds for intensive care |
Occupancy/billing days in intensive care |
|
| 2015 | 1956 | 1177 | 499 351 | 27 489 | 8 050 451 |
| 2014 | 1980 | 1191 | 500 680 | 27 018 | 7 919 139 |
| 2013 | 1996 | 1198 | 500 671 | 26 579 | 7 756 268 |
| 2012 | 2017 | 1213 | 501 475 | 26 162 | 7 657 365 |
| 2011 | 2045 | 1245 | 502 029 | 25 519 | 7 517 367 |
| 2010 | 2064 | 1260 | 502 749 | 24 974 | 7 413 503 |
| 2009 | 2084 | 1283 | 503 341 | 24 553 | 7 306 278 |
| 2008 | 2083 | 1281 | 503 360 | 23 890 | 7 042 898 |
| 2007 | 2087 | 1286 | 506 954 | 23 357 | 6 944 587 |
Data on the number of hospital beds, beds for intensive care and days of occupancy in intensive care were obtained from the Federal Health Monitoring Service (http://www.gbe-bund.de/)
Trends in hospitalization and intensive care use from 2007–2015
We analyzed a total of 16.6 million hospitalizations in 2007 and 18.7 million in 2015 (figure 1). Standardized rates of hospital admissions increased only slightly by a mean of 0.8% p.a. between 2007 and 2015. In contrast, the mean increase of hospital admissions involving intensive care p.a. was 3.0% and thus 3 times higher (table 1).
Table 1. Hospitalizations and intensive care use from 2007 to 2015.
| Hospitalizations*1 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| Total population, n | 82 217 837 | 82 002 356 | 81 802 257 | 81 751 602 | 80 327 900*3 | 80 523 746 | 80 767 463 | 81 197 537 | 82 175 684 |
| Total hospitalizations, n | 16 599 512 | 16 923 506 | 17 190 595 | 17 433 846 | 17 708.555 | 17 974.993 | 18 133.338 | 18 531.489 | 18 664.877 |
| Crude rate per 1000 population | 201.9 | 206.4 | 210.1 | 213.3 | 220.5 | 223.2 | 224.5 | 228.2 | 227.1 |
| Standardized rate per 1000 population*2 | 201.9 | 204.7 | 206.8 | 208.3 | 213.8 | 214.7 | 214.6 | 216.3 | 214.6 |
| Hospitalizations involving intensive care use n | 538 309 | 579 959 | 616 453 | 646 048 | 667 448 | 687 271 | 706 076 | 727 062 | 736 444 |
| Percentage of all hospitalizations | 3.2 | 3.4 | 3.6 | 3.7 | 3.8 | 3.8 | 3.9 | 3.9 | 3.9 |
| Crude rate per 1000 population | 6.5 | 7.1 | 7.5 | 7.9 | 8.3 | 8.5 | 8.7 | 9.0 | 9.0 |
| Standardized rate per 1000 population*2 | 6.5 | 7.0 | 7.3 | 7.6 | 7.9 | 8.0 | 8.1 | 8.2 | 8.2 |
| Deaths | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| All deaths in the German population, n | 827 155 | 844 439 | 854 544 | 858 768 | 852 328 | 869 582 | 893 825 | 868 356 | 925 200 |
| Hospital deaths, n | 393 388 | 398 942 | 406 470 | 405 490 | 400 002 | 404 073 | 415 190 | 401 156 | 425 073 |
| Percentage of all decedents | 47.6 | 47.2 | 47.6 | 47.2 | 46.9 | 46.6 | 46.5 | 46.2 | 45.9 |
| Crude rate per 1000 population | 4.8 | 4.9 | 5.0 | 5.0 | 5.0 | 5.0 | 5.1 | 4.9 | 5.2 |
| Standardized rate per 1000 population*2 | 4.8 | 4.8 | 4.7 | 4.6 | 4.6 | 4.5 | 4.5 | 4.3 | 4.4 |
| Hospital mortality rate (%) | 2.4 | 2.4 | 2.4 | 2.3 | 2.3 | 2.2 | 2.3 | 2.2 | 2.3 |
| Hospital deaths involving intensive care use, n | 80 978 | 85 765 | 90 818 | 93 940 | 96 146 | 97 924 | 103 322 | 103 030 | 108 866 |
| Percentage of all decedents | 9.8 | 10.2 | 10.6 | 10.9 | 11.3 | 11.3 | 11.6 | 11.9 | 11.8 |
| Percentage of all hospital deaths | 20.6 | 21.5 | 22.3 | 23.2 | 24.0 | 24.2 | 24.9 | 25.7 | 25.6 |
| Crude rate per 1000 population | 1.0 | 1.0 | 1.1 | 1.1 | 1.2 | 1.2 | 1.3 | 1.3 | 1.3 |
| Standardized rate per 1000 population*2 | 1.0 | 1.0 | 1.1 | 1.1 | 1.1 | 1.1 | 1.1 | 1.1 | 1.2 |
| ICU mortality rate (%) | 15.0 | 14.8 | 14.7 | 14.5 | 14.4 | 14.2 | 14.6 | 14.2 | 14.8 |
* Includes multiple admissions for some patients
** Directly standardized to the German age- and sex-based population structure as of 31 December 2007 on the basis of nationwide population data of the Federal Statistical Office for 2007–2015
*** Population estimates were adjusted after a nationwide census in 2011, leading to a decrease in the total population in Germany compared to 2010 and prior.
Mean annual changes of standardized rates: total hospitalizations +0.8%, hospitalizations involving intensive care use +3.0%, total hospital deaths –1.1%, hospital deaths involving intensive care use +2.3%
Mean annual changes of proportions: hospital deaths among all decedents –0.4%, hospital deaths involving intensive care use among all decedents +2.3%, hospital deaths involving ICU care among all hospital deaths +2.8%
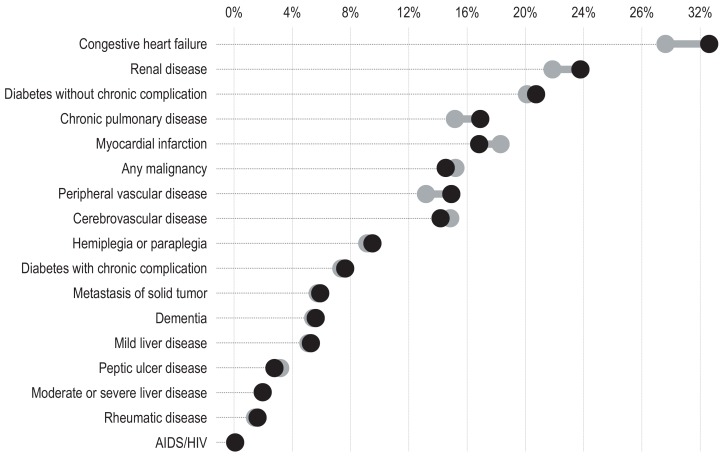
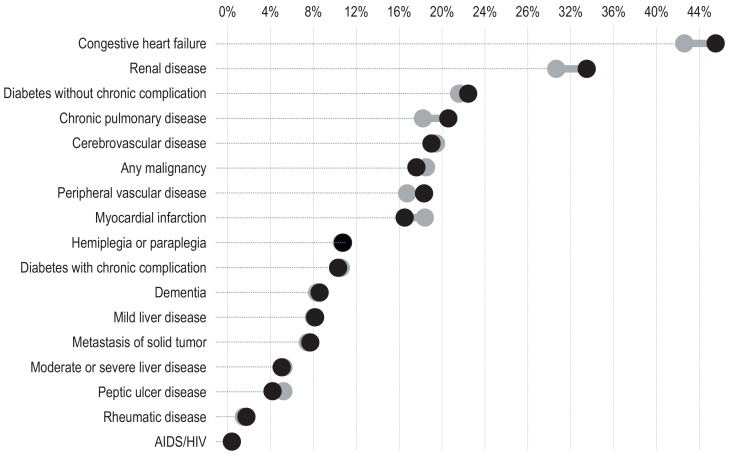
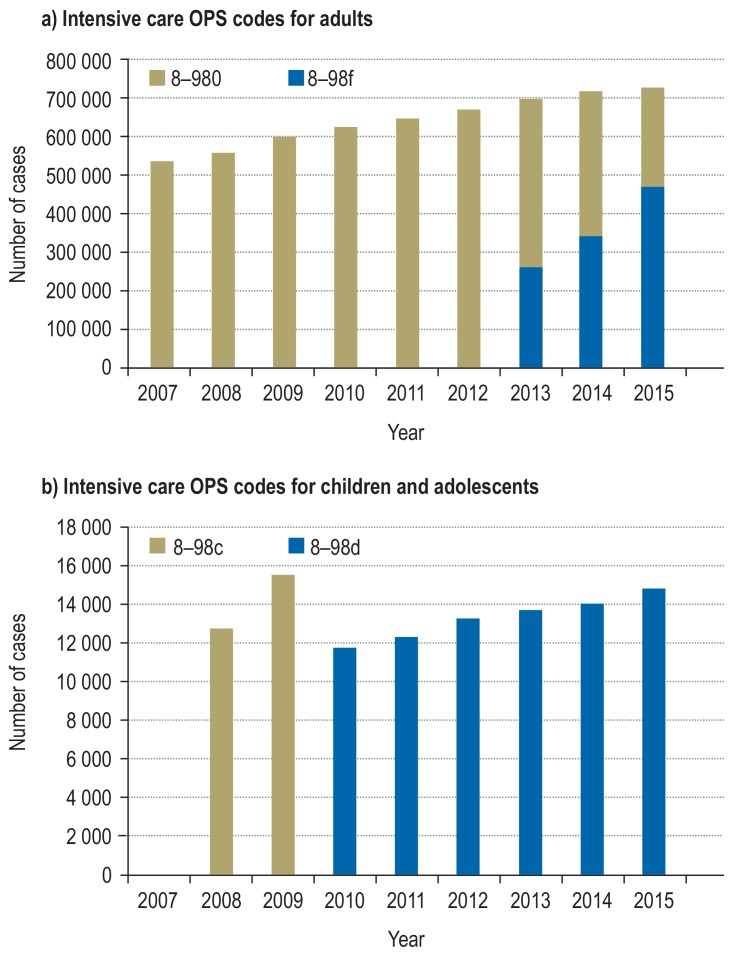
Among hospital patients receiving intensive care, median age increased from 69 [interquartile range, IQR 57–77] to 71 [58–79] years (etable 2). Hospital length of stay declined from median 14 [8–24] to 13 [7–22] days. The proportion of patients receiving mechanical ventilation increased from 25.0% to 30.5%, and for mechanical ventilation > 4 days from 15.6% to 16.2%. The proportion of patients with multimorbidity (= 2 comorbidities) increased from 55.2% to 57.5%. There were increases in congestive heart failure, renal disease, chronic pulmonary disease, and peripheral vascular disease, while myocardial infarction and malignancy decreased (eFigures 1 and 2). The use of palliative care services was very low but increased from 0.1% to 0.7% (etable 2). Documentation of intensive care cases with increased complexity rose rapidly after the more rigorous OPS code 8–93f was introduced in 2013 to describe cases with increased complexity and higher costs (eFigure 3a).
eTable 2. Demographics, comorbidities, and resource use for hospital patients with intensive care treatment.
|
2007 n = 538 309 |
2011 n = 667 448 |
2015 n = 736 444 |
|
| Age in years, median (IQR) | 69 (57–77) | 70 (57–78) | 71 (58–79) |
| Female sex, % | 42.0 | 42.1 | 41.7 |
| Charlson Comorbidity Index, median (IQR) | 2 (1–4)* | 2 (1–4) | 2 (1–4) |
| Comorbidities according to Charlson, % | |||
| None | 18.4* | 18.6 | 17.1 |
| 1 | 26.3* | 26.2 | 25.3 |
| 2–4 | 50.5* | 50.5 | 52.3 |
| >4 | 4.7* | 4.8 | 5.2 |
| Hospital length of stay, days, median (IQR) | 14 (8–24) | 13 (8–23) | 13 (7–22) |
| Surgical treatment, n (%) | 325 767 (60.5) | 382 391 (57.3) | 414 058 (56.2) |
| Renal replacement treatment, n (%) | 40 976 (7.6) | 54 252 (8.1) | 58 502 (7.9) |
| Mechanical ventilation, n (%) | 135 688 (25.0) | 181 705 (27.2) | 224 852 (30.5) |
| more than 4 days, n (%) | 83 833 (15.6) | 104 620 (15.7) | 119 655 (16.2) |
| Tracheostomy | 35 673 (6.6) | 42 331 (6.3) | 42 650 (5.8) |
| temporary, n (%) | 28 111 (5.2) | 32 898 (4.9) | 32 048 (4.4) |
| permanent, n (%) | 8 620 (1.6) | 10 539 (1.6) | 11 723 (1.6) |
| Palliative care, n (%) | 541 (0.1) | 2 133 (0.3) | 5 084 (0.7) |
* Descriptive statistics refer to earliest available data from the year 2010, n = 646 048. IQR, interquartile range
eFigure 1.
Changes in comorbidities for all hospital discharges involving intensive care from 2010 (gray bullets) to 2015 (black bullets)
eFigure 2.
Changes in comorbidities for all hospital deaths involving intensive care from 2010 (gray bullets) to 2015 (black bullets)
eFigure 3.
Number of intensive care hospitalizations from 2007 to 2015 according to different codes for the classification of operations and procedures (OPS codes)
a) OPS codes for complex intensive care treatment (8–980) and costly complex intensive care treatment (8–98f)
b) OPS codes for complex intensive care treatment for children and adolescents (8–98c and 8–98d)
Trends in discharge dispositions of survivors
Table 2 shows the discharge dispositions of survivors of hospitalization who had received intensive care. The majority of patients were discharged home or to other hospitals. Discharges to nursing homes increased by a mean 8.0% p.a., while discharges to rehabilitation facilities decreased by a mean of 3.5% p.a. Only few patients were discharged to a hospice. eTable 3 explains the discharge categories.
Table 2. Discharge dispositions of survivors of hospitalization involving intensive care.
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| All survivors, n | 457 331 | 494 194 | 525 635 | 552 108 | 571 302 | 589 347 | 602 754 | 624 032 | 627 578 |
| Discharge disposition, n (%) | |||||||||
| Regular | 310 216 (67.8) |
338 868 (68.6) |
359 343 (68.4) |
375 840 (68.1) |
386 163 (67.6) |
401 129 (68.1) |
412 519 (68.4) |
429 968 (68.9) |
431 608 (68.8) |
| Other hospital | 73 334 (16.0) |
77 324 (15.6) |
81 081 (15.4) |
84 770 (15.4) |
87 073 (15.2) |
91 498 (15.5) |
93 131 (15.5) |
98 426 (15.8) |
101 726 (16.2) |
| Hospice | 446 (0.1) | 520 (0.1) | 574 (0.1) | 622 (0.1) | 637 (0.1) | 691 (0.1) | 777 (0.1) | 934 (0.1) | 922 (0.1) |
| Rehabilitation facility | 55 290 (12.1) |
56 473 (11.4) |
60 311 (11.5) |
63 659 (11.5) |
66 713 (11.7) |
64 447 (10.9) |
63 109 (10.5) |
59 076 (9.5) |
56 913 (9.1) |
| Nursing home | 9052 (2.0) |
11 306 (2.3) |
13 917 (2.6) |
15 708 (2.8) |
17 517 (3.1) |
19 000 (3.2) |
20 352 (3.4) |
22 032 (3.5) |
22 894 (3.6) |
| Other | 8993 (2.0) |
9703 (2.0) |
10 409 (2.0) |
11 509 (2.1) |
13 199 (2.3) |
12 582 (2.1) |
12 866 (2.1) |
13 596 (2.2) |
13 515 (2.2) |
eTable 3. Discharge disposition according to the DRG statistics.
| Discharge disposition | Definition |
| Regular | Regular termination of treatment Regular termination of treatment, post-discharge treatment intended |
| Other hospital | Transfer to another hospital Transfer to another hospital as part of a cooperation External transfer for psychiatric treatment |
| Hospice | Discharge to a hospice |
| Rehabilitation facility | Discharge to a rehabilitation facility |
| Nursing home | Discharge to a care facility |
| Other | Treatment terminated for other reasons Treatment terminated for other reasons, post-discharge treatment intended Treatment terminated against medical advice Treatment terminated against medical advice, post-discharge treatment intended Change of cost unit responsible Internal transfer with change in DRG remuneration category, according to the Federal Ordinance on Hospital Care Rates or for special facilities according to section 17b (1) first sentence of the Hospital Funding Act Case end (internal transfer) when changing between full and part-time inpatient treatment Discharge at the end of the year while admitted the year before (for accounting purposes, § 4 PEPPV 2013) |
Trends in overall hospital deaths and deaths involving ICU care from 2007 to 2015
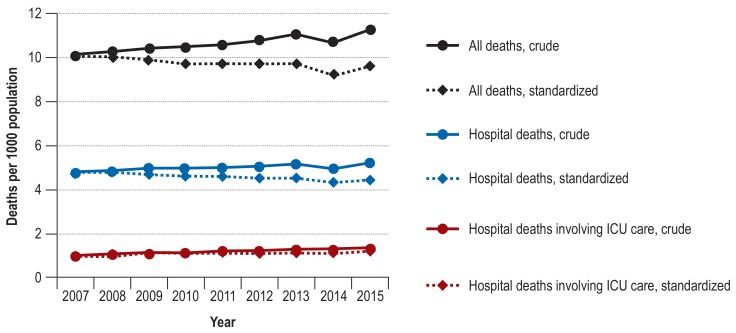
Standardized rates of hospital deaths declined from 4.8/1000 to 4.4/1000 population (mean -1.1% p.a.) and the proportion of all Germans who died in hospital decreased from 47.6% to 45.9% (mean -0.4% p.a). In contrast, hospital deaths involving ICU care increased from 1.0/1000 to 1.2/1000 population (mean +2.3% p.a.) (Table 1, Figure 2). In 2007, every fifth patient who died in hospital had received intensive care; in 2015, it was every fourth (mean +2.8% p.a.). Hospital and ICU mortality rates were essentially stable (from 2.4% to 2.3% and from 15.0% to 14.8%, respectively). Over time, more of the patients who died in hospital and received intensive care had congestive heart failure, renal disease, chronic pulmonary disease, or cerebrovascular disease than did patients with ICU care overall (eFigures 1 and 2).
Figure 2.
Crude and standardized rates of death
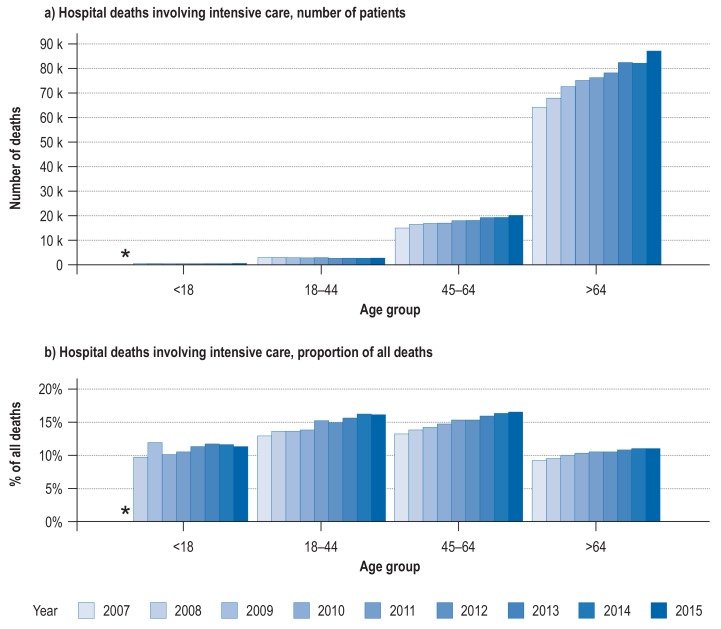
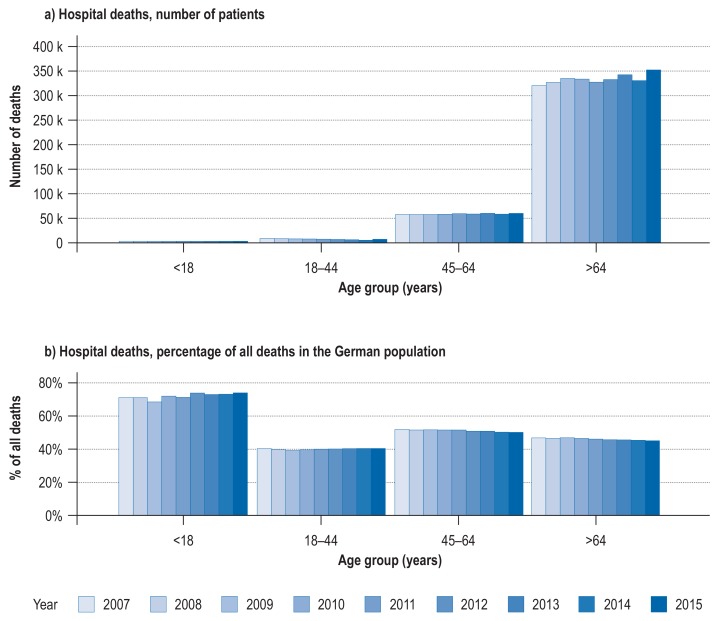
Trends in overall hospital deaths and deaths involving ICU care stratified by age from 2007 to 2015
Figure 3, and eFigure 4 depict hospital deaths and deaths involving ICU care for different age groups. The increasing trend of deaths involving ICU care was most marked in the age group 65 years and older. In this age group, the number of hospital deaths involving ICU care increased approximately 3 times faster than the number of overall hospital deaths. In patients = 85 years, hospital deaths involving ICU care increased by a mean of 7.0% p.a. and thus 2 times faster than hospital deaths (etable 4). The introduction in 2010 of new OPS codes for intensive care use in children and adolescents resulted in a temporary reduction of ICU use codes for this age group (Figure 3, eFigure 3b).
Figure 3.
Development of hospital deaths involving ICU care in Germany from 2007 to 2015. The numbers of deaths are expressed in thousands (k)
eFigure 4.
Hospital deaths per year stratified by age group. The bars represent the years from 2007 to 2015. The numbers of deaths are presented in thousands (k)
eTable 4. Overall hospital deaths and hospital deaths involving ICU care in different age groups during the period 2007 to 2015.
| All age groups | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | ||
| Younger than 18 years | All deaths, n | 4543 | 4272 | 4142 | 3982 | 4026 | 3723 | 3756 | 3681 | 3926 |
| Hospital deaths, n (%) | 3238 (71.3) |
3046 (71.3) |
2845 (68.7) |
2875 (72.2) |
2878 (71.5) |
2757 (74.1) |
2749 (73.2) |
2701 (73.4) |
2914 (74.2) |
|
| Hospital deaths involving ICU care, n (%) | 104 (2.3) |
415 (9.7) |
494 (11.9) |
404 (10.1) |
421 (10.5) |
422 (11.3) |
439 (11.7) |
426 (11.6) |
444 (11.3) |
|
| 18–44 years | All deaths, n | 22 430 | 21 422 | 20 628 | 19 907 | 18 661 | 17 381 | 16 877 | 16 079 | 16 589 |
| Hospital deaths, n (%) | 9062 (40.4) |
8519 (39.8) |
8106 (39.3) |
7904 (39.7) |
7489 (40.1) |
6992 (40.2) |
6819 (40.4) |
6510 (40.5) |
6725 (40.5) |
|
| Hospital deaths involving ICU care, n (%) | 2894 (12.9) |
2913 (13.6) |
2805 (13.6) |
2748 (13.8) |
2843 (15.2) |
2585 (14.9) |
2638 (15.6) |
2603 (16.2) |
2666 (16.1) |
|
| 45–64 years | All deaths, n | 111 854 | 112 402 | 112 273 | 113 542 | 115 732 | 115 970 | 118 883 | 116 800 | 120 320 |
| Hospital deaths, n (%) | 58 177 (52.0) |
58 127 (51.7) |
58 119 (51.8) |
58 657 (51.7) |
59 840 (51.7) |
59 172 (51.0) |
60 622 (51.0) |
58 924 (50.4) |
60 524 (50.3) |
|
| Hospital deaths involving ICU care, n (%) | 14 745 (13.2) |
15 485 (13.8) |
15 935 (14.2) |
16 727 (14.7) |
17 692 (15.3) |
17 798 (15.3) |
18 958 (15.9) |
19 010 (16.3) |
19 852 (16.5) |
|
| 65 years and older | All deaths, n | 688 328 | 706 342 | 717 501 | 721 337 | 713 909 | 732 508 | 754 309 | 731 796 | 784 365 |
| Hospital deaths, n (%) | 322 911 (46.9) |
329 250 (46.6) |
337 400 (47.0) |
336 054 (46.6) |
329 795 (46.2) |
335 152 (45.8) |
345 000 (45.7) |
333 021 (45.5) |
354 910 (45.2) |
|
| Hospital deaths involving ICU care, n (%) | 63 235 (9.2) |
66 952 (9.5) |
71 584 (10.0) |
74 061 (10.3) |
75 190 (10.5) |
77 119 (10.5) |
81 287 (10.8) |
80 991 (11.1) |
85 904 (11.0) |
|
| Subgroup | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | ||
| 85 years and older | All deaths, n | 258 291 | 272 476 | 279 990 | 285 965 | 289 344 | 304 338 | 319 369 | 313 421 | 343 908 |
| Hospital deaths, n (%) | 94 880 (36.7) |
100 209 (36.8) |
103 973 (37.1) |
105 317 (36.8) |
105 416 (36.4) |
110 906 (36.4) |
116 948 (36.6) |
115 071 (36.7) |
125 628 (36.5) |
|
| Hospital deaths involving ICU care, n (%) | 11 182 (4.3) |
12 544 (4.6) |
13 757 (4.9) |
14 616 (5.1) |
15 245 (5.3) |
16 367 (5.4) |
17 461 (5.5) |
17 931 (5.7) |
19 205 (5.6) |
|
Presented are absolute numbers (n) and proportions of all deaths accounted for by the respective age group (%)
Discussion
Our study investigated trends in hospital deaths and intensive care treatment during terminal hospitalizations between 2007 and 2015. In 2015, approximately 50% of Germans died in hospital and 25% of hospital deaths occurred during or after intensive care treatment. Compared with 2007, hospital deaths decreased, but terminal hospitalizations involving ICU care increased. In 2007, one in five hospital deaths occurred after ICU care; by 2015, this proportion had increased to one in four. In patients = 65 years, deaths involving ICU care increased 3 times faster than hospital deaths. Hospital deaths involving intensive care in patients = 85 years increased 2 times faster than hospital deaths.
These findings raise questions about the potential reasons for the growth in use of intensive care treatment. Population demographics is unlikely to be the major contributor, because age- and sex-standardized incidence rates also increased. Another possible explanation is increasing morbidity and disease severity: ICU patients are getting sicker and older (9), which may account for an increasing demand for intensive care in hospitals (10). Moreover, economic incentives may play a role. In the DRG system, hospitals’ profits increase exponentially with the numbers of days when mechanical ventilation is used and staffing ratios are low (11). This economic incentive may explain why ICU capacity and occupancy rates are increasing steadily in hospitals of all sizes (12), although the total number of hospital beds is going down (13), and may have accelerated the increase in “complex” intensive care cases we observed after introduction of the more rigorous yet better financed OPS codes 8–98f.
In 2012, the number of ICU beds in Germany was 31.8/100 000 (14), more than in the USA and double the European average (15). Importantly, this development goes along with one of the lowest nurse-to-patient ratios in Europe (16). In England, where financial incentives and societal perspectives are different, analysis of hospital discharge data showed that only 5.1% of deaths involved intensive care and there was almost no use of intensive care services in patients aged = 85 years (17).
Although the absolute number of palliative care treatments increased tenfold from 541 to 5084, overall the utilization of palliative care services was low compared with other countries. The lack of palliative care may also play a role in rising ICU utilization at the end of life. Less aggressive and expensive alternatives such as hospices or home-based palliative care have helped to reverse the trend of terminal hospitalizations in the UK (18). In-hospital palliative care services can potentially reduce the need for terminal ICU care (19). Our study showed that only 0.1% of hospitalized patients with ICU care were discharged to a hospice versus 5.9% of patients with sepsis in the USA (20). In Canada, nearly half of the patients who died in hospital received inpatient palliative care (21). The Netherlands have double the rate of inpatient palliative care services (1.27/100,000 population) compared with Germany (0.73) (22).
The question to what extent intensive therapy would be desired by informed patients or contributes to overtreatment—which in turn worsens the burden on the treatment team and increases healthcare costs—cannot be answered based on the administrative data we analyzed. However, our data describe important trends with implications for patients, relatives, health care professionals, and policy makers. Further prospective studies are needed to evaluate the benefits and harm of ICU utilization at the end of life.
Broadening the view to other countries, one sees that in the USA, for example, the use of mechanical ventilation among hospitalized nursing home residents with advanced dementia doubled from 2000 to 2013 without improving survival (8). At the hospital level, an increase in the number of ICU beds over time was associated with increasing use of mechanical ventilation for these patients (8).
In a German single-center survey among relatives of patients with sepsis, 23% stated that the intensity of treatment had not been consistent with the patients’ wishes (23). However, the prevalence of advance directives is only 9–13% in patients who die in the ICU in Germany (24, 25). Although advance directives are rarely specific enough to enable definitive decisions regarding treatment intensity at the end of life (26) and may have little or no impact on the intensity of the therapy provided (25, 27), the low prevalence of advance directives indicates that awareness of the importance of such directives is low in the general population. This may contribute to increasing use of intensive care services during terminal hospitalizations. In the USA, it is assumed that the increasing demand for ICU treatment with stable staffing levels and resources will have negative implications for all ICU patients and will increase demands on ICU treatment providers still further (28).
Taken together, our data show the growing demand for end-of-life care in the ICU and suggest an opportunity to implement and strengthen palliative care in the hospital and particularly in the ICU (2). Given that most critically ill patients have lost decision-making capacity, decisions to change the goal of treatment or not to admit patients with a poor prognosis lie in the hands of physicians and family members. For some patients, palliative treatments may be better performed in an ICU and by trained and experienced ICU clinicians. However, end-of-life care demands interdisciplinary collaboration, decision making, and communication with the family. Acquisition and implementation of the corresponding skills will require additional educational programs, better reimbursement, and increased staffing levels (11).
Strengths and limitations
The strength of this study is its representativeness, based as it is on nationwide administrative data. In addition, we selected a conservative approach to identify use of ICU care. The coding is strictly supervised by government agencies and routinely cross-checked by trained physicians of the medical service of the health insurance companies in Germany (MDK).
This study also has important limitations:
We cannot provide information on severity of critical illness, clinical decision making, or patients’ presumed or actual preferences. Therefore, we cannot assess whether use of intensive care at the end of life was appropriate and compliant with patient preferences. Nevertheless, the fact that end-of-life care in the ICU increases in older patients is important.
We cannot differentiate whether a hospitalized patient died during or after the ICU treatment. Although our approach allows understanding of ICU utilization during terminal hospitalizations, it does not permit identification of the proportion of patients who die in the ICU. We can neither retrace transfers between ICU and ward nor know the underlying medical and ethical decisions.
We cannot identify patients who were discharged from the ICU for palliative care elsewhere. However, low coding for palliative care services or hospice transfer make it unlikely that this applied to many patients.
There may be selection bias in that patients who died within 24 h of admission to the ICU were not included as per OPS coding prerequisites. This may lead to underestimation of hospital deaths after use of intensive care.
Since the patients are anonymized, multiple hospital admissions for individual patients and transfers between hospitals cannot be identified. This is not a limitation for exploring terminal hospitalizations but restricts our ability to examine repeat admissions and transfers.
Finally, coding of healthcare services and comorbidities may contain inaccuracies, be influenced by coding incentives, and change over time. These incentives may have led to increased coding of intensive care services in general with high relevance for monetary reimbursement. Therefore, the interpretation of trends based on the DRG statistics data remains tentative. Further prospective data are needed to better understand the underlying mechanisms of the observed increase in use of ICU services during terminal hospitalizations.
Conclusion
In the context of growing availability of ICU beds in Germany, we found an increase in hospital deaths among patients who received intensive care across all adult age groups, particularly the elderly, from 2007 to 2015. This increase in end-of-life care in the ICU calls for increased efforts to identify and implement patient preferences and develop policy and reimbursement strategies to improve the quality of care for these patients as their life draws to an end.
Supplementary Material
eMethods
Material and methods
Data sources
We used the German diagnosis-related groups (DRG) statistics for the analysis of hospitalizations with and without intensive care. The DRG statistics is a nationwide database comprising complete inpatient data from all acute-care hospitals in Germany except military and prison hospitals. These data are accessible via remote data processing from the German Federal Statistical Office. Each hospitalization is treated as an individual entry and contains one principal ICD-10 German Modification (ICD-10-GM) diagnosis, up to 89 secondary ICD-10-GM diagnoses, and up to 100 OPS codes (OPS, German classification of operations and procedures), as well as data on length of hospital stay, type of admission and discharge, and patient demographics. In addition, we used the population and deaths statistics of the German Federal Statistical Office, accessible online (https://www-genesis.destatis.de/genesis/online). Data on the number of hospital beds, beds for intensive care, and days of occupancy in intensive care were obtained from the Federal Health Monitoring Service (http://www.gbe-bund.de/).
Description of patients
We identified hospitalized patients of all ages between 2007 and 2015 and excluded cases with unknown age and sex. In order to identify patients receiving intensive care, we chose a conservative approach, using corresponding codes for the classification of operations and procedures (OPS codes 8–980, 8–98c, 8–98d, 8–98f). These codes were introduced to specify so-called complex intensive care treatment. To prevent overcoding, the use of these codes was bound to prerequisites, including the continuous attendance of a physician, a team of specialized nurses and physicians, and a stay of at least 24 h. Monitoring without treatment of organ failure and short-term stabilization after surgical treatment cannot be classified using these codes. Use of intensive care services during terminal hospitalizations was determined by the number of patients who died in hospital and received ICU care at any time during their hospital stay.
We also evaluated the following patient demographics:
Statistical analyses
The data were analyzed using SAS® (Version 9.4; SAS Institute, Cary, NC, USA) and R (Version 3.4.0; R Core Team, Vienna, Austria) and are presented as percentages, absolute numbers, and either medians and interquartile ranges (IQR) or means and standard deviations (SD).
We calculated annual population-based incidences and standardized these to the German population structure according to the age and sex distribution as of 31 December 2007, based on nationwide population data of the Federal Statistical Office for the period 2007 to 2015. Given the large size of the data set, we did not perform inferential statistics, as all comparisons were likely to be statistically different.
Age
Sex
Underlying comorbidity, using the Charlson Comorbidity Index (CCI), which is determined on the basis of primary and secondary ICD discharge diagnoses (9)
Resource use, including hospital length of stay (LOS)
Surgical treatment (any OPS code for surgical conditions, OPS 5–01–5–99)
Renal replacement therapy (OPS codes 8–853, 8–854, 8–855)
Mechanical ventilation (OPS codes 8–70, 8–71)
Tracheostomy (OPS codes 5–311 for temporary, 5–312 for permanent tracheostomy)
Palliative care that can be delivered in specialized palliative care wards (8–98e) or by palliative care specialists and multidisciplinary teams on any hospital ward including intensive care units (8–982)
Discharge disposition
Hospital mortality
Key Messages.
Analysis of nationwide hospital discharge data (DRG statistics; DRG, diagnosis-related groups) shows that hospital deaths in Germany are decreasing, but the use of intensive care services during terminal hospitalizations is increasing.
In 2015, approximately 25% of patients who died in the hospital received ICU care during their terminal hospitalization.
In patients aged 65 years and older, the number of deaths during hospital stays involving ICU care increased from 63 235 in 2007 to 85 904 in 2015. The rate of increase was thus 3 times greater than that for overall hospital deaths, which increased from 322 911 to 354 910.
These findings call for increased efforts to implement and strengthen palliative care in the intensive care setting.
Acknowledgments
The authors acknowledge Dr. Hannah Wunsch, who provided helpful comments during the writing of the draft.
Data source
The research data center of the Federal Statistical Office and the statistical offices of the German federal states (DRG statistics 2007–2015)
Funding
This study was supported by the Federal Ministry of Education and Research (BMBF) through the Center for Sepsis Control and Care (CSCC; FKZ: 01EO1002 and 01EO1502) via InfectControl2020 (FKZ: 03ZZ0819B).
Footnotes
Conflict of interest statement
Prof.Reinhart is a partner in InflaRx Jena and a consultant for Adrenomed Henningsdorf Berlin.
Dr. Dennler has received reimbursement of congress attendance fees and travel costs from Aesculap Akademie.
The remaining authors declare that no conflict of interest exists.
References
- 1.Gomes B, Calanzani N, Gysels M, Hall S, Higginson IJ. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care. 2013;12 doi: 10.1186/1472-684X-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376:1347–1353. doi: 10.1016/S0140-6736(10)60143-2. [DOI] [PubMed] [Google Scholar]
- 3.Hartog CS, Hoffmann F, Mikolajetz A, et al. Nicht-nutzbringende Therapie und emotionale Erschöpfung in der Lebenszeitpflege: Ergebnisse einer Umfrage unter Intensivstation Personal. Anästhesist. 2018;67:850–858. doi: 10.1007/s00101-018-0485-7. [DOI] [PubMed] [Google Scholar]
- 4.Simon ST, Gomes B, Koeskeroglu P, et al. Bevölkerung, Sterblichkeit und Sterbeort in Deutschland (1950-2050) - Auswirkungen auf die Pflege am Lebensende in der Zukunft. Öffentliche Gesundheit. 2012;126:937–946. [Google Scholar]
- 5.Dasch B, Blum K, Gude P, Bausewein C. Place of death: trends over the course of a decade—a population-based study of death certificates from the years 2001 and 2011. Dtsch Arztebl Int. 2015;112:496–504. doi: 10.3238/arztebl.2015.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36:2787–2793. doi: 10.1097/CCM.0b013e318186aec8. e2781-9. [DOI] [PubMed] [Google Scholar]
- 7.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teno JM, Gozalo P, Khandelwal N, et al. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care unit beds. JAMA Intern Med. 2016;176:1809–1816. doi: 10.1001/jamainternmed.2016.5964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sjoding MW, Prescott HC, Wunsch H, et al. Longitudinal changes in ICU admissions among elderly patients in the United States. Crit Care Med. 2016;44:1353–1360. doi: 10.1097/CCM.0000000000001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kastrup M, Seeling M, Barthel S, et al. Effects of intensivist coverage in a post-anaesthesia care unit on surgical patients‘ case mix and characteristics of the intensive care unit. Crit Care. 2012;16 doi: 10.1186/cc11428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riessen R, Hermes C, Bodmann KF, et al. Erstattung von Intensivpflegeleistungen im deutschen DRG-System Aktuelle Probleme und mögliche Lösungen. Med Klin Intensivmed Notfmed. 2018;113:13–23. doi: 10.1007/s00063-017-0390-x. [DOI] [PubMed] [Google Scholar]
- 12.Thattil R, Klepzig D, Schuster M. Intensive Pflegekapazitäten in Deutschland: Versorgung und Nutzung zwischen 1991 und 2009. Anästhesist. 2012;61:56–62. doi: 10.1007/s00101-011-1969-x. [DOI] [PubMed] [Google Scholar]
- 13.Janssens U. Wirtschaft in der Intensivmedizin - ein Widerspruch? Med Klin Intensivmed Notfmed. 2015;110:264–271. doi: 10.1007/s00063-015-0028-9. [DOI] [PubMed] [Google Scholar]
- 14.Bittner MI, Donnelly M, van Zanten AR, et al. Wie wird die Intensivpflege erstattet? Ein Überblick über acht europäische Länder. Ann Intensivmedizin. 2013;3 [Google Scholar]
- 15.Rhodes A, Ferdinande P, Flaatten H, et al. Die Variabilität der Bettenzahlen in der kritischen Pflege in Europa. Intensivmedizin Med. 2012;38:1647–1653. [Google Scholar]
- 16.Aiken LH, Sloane DM, Bruyneel L, et al. Nurses‘ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Gestüt. 2013;50:143–153. doi: 10.1016/j.ijnurstu.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 17.Wunsch H, Linde-Zwirble WT, Harrison DA, et al. Use of intensive care services during terminal hospitalizations in England and the United States. Am J Respir Crit Care Med. 2009;180:875–880. doi: 10.1164/rccm.200902-0201OC. [DOI] [PubMed] [Google Scholar]
- 18.Gomes B, Calanzani N, Higginson IJ. Umkehrung der britischen Trends anstelle des Todes: Zeitreihenanalyse 2004-2010. Palliat Med. 2012;26:102–107. doi: 10.1177/0269216311432329. [DOI] [PubMed] [Google Scholar]
- 19.Khandelwal N, Kross EK, Engelberg RA, Coe NB, Long AC, Curtis JR. Estimating the effect of palliative care interventions and advance care planning on ICU utilization: a systematic review. Crit Care Med. 2015;43:1102–1111. doi: 10.1097/CCM.0000000000000852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009-2014. JAMA. 2017;318:1241–1249. doi: 10.1001/jama.2017.13836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qureshi D, Tanuseputro P, Perez R, et al. Place of care trajectories in the last two weeks of life: a population-based cohort study of ontario decedents. J Palliat Med. 2018;21:1588–1595. doi: 10.1089/jpm.2018.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centeno C, Lynch T, Garralda E, et al. Abdeckung und Entwicklung spezialisierter Palliativversorgungsdienste in der gesamten Europäischen Region der Weltgesundheitsorganisation (2005-2012): Ergebnisse einer Umfrage der European Association for Palliative Care Task Force in 53 Ländern. Palliat Med. 2016;30:351–362. doi: 10.1177/0269216315598671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matt B, Schwarzkopf D, Reinhart K, et al. Relatives‘ perception of stressors and psychological outcomes—Results from a survey study - Ergebnisse einer Umfragestudie. J Crit Care. 2017;39:172–177. doi: 10.1016/j.jcrc.2017.02.036. [DOI] [PubMed] [Google Scholar]
- 24.Graw JA, Spies CD, Wernecke KD, et al. Managing end-of-life decision making in intensive care medicine–a perspective from Charité Hospital, Germany. PLoS One. 2012;7 doi: 10.1371/journal.pone.0046446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartog CS, Peschel I, Schwarzkopf D, et al. Are written advance directives helpful to guide end-of-life therapy in the intensive care unit? A retrospective matched-cohort stud. J Crit Care. 2014;29:128–133. doi: 10.1016/j.jcrc.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 26.Leder N, Schwarzkopf D, Reinhart K, Witte OW, Pfeifer R, Hartog CS. The validity of advance directives in acute situations—a survey of doctors‘ and relatives‘ perceptions from an intensive care unit. Dtsch Arztebl Int. 2015;112:723–729. doi: 10.3238/arztebl.2015.0723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Halpern NA, Goldman DA, Tan KS, et al. Trends in critical care beds and use among population groups and medicare and medicaid beneficiaries in the United States: 2000-2010. Crit Care Med. 2016;44:1490–1499. doi: 10.1097/CCM.0000000000001722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bagshaw SM, Opgenorth D, Potestio M, et al. Healthcare provider perceptions of causes and consequences of ICU capacity strain in a large public funded integrated health region: a qualitative study. Crit Care Med. 2017;45:e347–e356. doi: 10.1097/CCM.0000000000002093. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Material and methods
Data sources
We used the German diagnosis-related groups (DRG) statistics for the analysis of hospitalizations with and without intensive care. The DRG statistics is a nationwide database comprising complete inpatient data from all acute-care hospitals in Germany except military and prison hospitals. These data are accessible via remote data processing from the German Federal Statistical Office. Each hospitalization is treated as an individual entry and contains one principal ICD-10 German Modification (ICD-10-GM) diagnosis, up to 89 secondary ICD-10-GM diagnoses, and up to 100 OPS codes (OPS, German classification of operations and procedures), as well as data on length of hospital stay, type of admission and discharge, and patient demographics. In addition, we used the population and deaths statistics of the German Federal Statistical Office, accessible online (https://www-genesis.destatis.de/genesis/online). Data on the number of hospital beds, beds for intensive care, and days of occupancy in intensive care were obtained from the Federal Health Monitoring Service (http://www.gbe-bund.de/).
Description of patients
We identified hospitalized patients of all ages between 2007 and 2015 and excluded cases with unknown age and sex. In order to identify patients receiving intensive care, we chose a conservative approach, using corresponding codes for the classification of operations and procedures (OPS codes 8–980, 8–98c, 8–98d, 8–98f). These codes were introduced to specify so-called complex intensive care treatment. To prevent overcoding, the use of these codes was bound to prerequisites, including the continuous attendance of a physician, a team of specialized nurses and physicians, and a stay of at least 24 h. Monitoring without treatment of organ failure and short-term stabilization after surgical treatment cannot be classified using these codes. Use of intensive care services during terminal hospitalizations was determined by the number of patients who died in hospital and received ICU care at any time during their hospital stay.
We also evaluated the following patient demographics:
Statistical analyses
The data were analyzed using SAS® (Version 9.4; SAS Institute, Cary, NC, USA) and R (Version 3.4.0; R Core Team, Vienna, Austria) and are presented as percentages, absolute numbers, and either medians and interquartile ranges (IQR) or means and standard deviations (SD).
We calculated annual population-based incidences and standardized these to the German population structure according to the age and sex distribution as of 31 December 2007, based on nationwide population data of the Federal Statistical Office for the period 2007 to 2015. Given the large size of the data set, we did not perform inferential statistics, as all comparisons were likely to be statistically different.
Age
Sex
Underlying comorbidity, using the Charlson Comorbidity Index (CCI), which is determined on the basis of primary and secondary ICD discharge diagnoses (9)
Resource use, including hospital length of stay (LOS)
Surgical treatment (any OPS code for surgical conditions, OPS 5–01–5–99)
Renal replacement therapy (OPS codes 8–853, 8–854, 8–855)
Mechanical ventilation (OPS codes 8–70, 8–71)
Tracheostomy (OPS codes 5–311 for temporary, 5–312 for permanent tracheostomy)
Palliative care that can be delivered in specialized palliative care wards (8–98e) or by palliative care specialists and multidisciplinary teams on any hospital ward including intensive care units (8–982)
Discharge disposition
Hospital mortality