ABSTRACT
BACKGROUND:
Laryngeal masks are increasingly used in place of endotracheal intubation or face masks for maintaining the airway during surgery.
OBJECTIVES:
Compare the insertion time and other features of the Baska and I-gel masks in patients undergoing general anesthesia for urological surgery.
DESIGN:
Randomized-controlled, single-blind study.
SETTINGS:
Urology surgical operating rooms of a tertiary care hospital.
SUBJECTS AND METHODS:
We enrolled concomitant patients whose surgery was expected to last less than two hours. Following premedication and adequate relaxation, subjects were randomly allocated to the I-gel mask or the Baska mask. Computer-generated random numbers were used for randomization with sealed opaque envelopes for allocation concealment.
MAIN OUTCOME MEASURES:
The primary outcome measure of the study was the time required for laryngeal mask airway (LMA) insertion. Also, the number of device placement attempts, the number of postoperative signs and symptoms (cough, breath holding, laryngeal spasm, lip trauma, blood on the mask), and laryngopharyngeal morbidity scores at 1 and 24 hours postoperatively.
SAMPLE SIZE:
211 met inclusion criteria, 200 participants completed the study.
RESULTS:
Compared to I-gel, the Baska mask required a longer time for insertion, and its airway pressure was higher. The median (minimum-maximum) duration of LMA insertion in the Baska and I-gel groups was 14 (6-25) and 7 (5-12) seconds, respectively (z=-10.934; P<.001). The mean (SD) airway pressures were significantly different between the two groups (15.8 [1.9] and 14.9 [1.7] cm/H2O for Baska and I-gel, respectively; t=3.668; P<.001). Seal pressure was not significantly different between the groups (0.08 [0.2] vs. 0.07 [0.2] cm/H2O in the Baska and I-gel groups, respectively, (t=1.35; P=.194).
CONCLUSIONS:
The Baska and I-gel masks are similar in most respects. Both have reasonably acceptable insertion times and can be used for selected surgical procedures.
LIMITATIONS:
The requirement for more vigorous training is a limitation of the Baska mask. Results could differ with patients younger than 18 years of age or obese patients.
CONFLICT OF INTEREST:
None.
CLINICAL TRIAL REGISTRY:
Not registered.
INTRODUCTION
The most vital parameter in establishing functional respiration during surgery is having a proper airway, which is a fundamental anesthetic skill during general anesthesia.1 Tracheal intubation, the long-used gold-standard method for this purpose, requires training and practice and may also cause laryngopharyngeal problems. Laryngeal masks have emerged during recent years as an alternative to endotracheal intubation. These new airway devices are claimed to produce no cardiopulmonary response during intubation, nor stimulate laryngeal reflexes, require fewer anesthetic medications, and to have fewer complications and side effects such as coughing during awakening or sore throat.2 Despite some disadvantages, such as being not suitable for controlled ventilation and gas leakage leading to potential stomach distention and regurgitation, laryngeal masks are used increasingly more often than endotracheal intubation or face masks. Laryngeal masks ease ventilation and passage of the tube in patients with difficult airways and allow for the insertion of the fiberoptic bronchoscope. As the pressure increases with positive pressure ventilation, the cuff itself is inflated, which may improve the seal, reducing leakage and making ventilation more efficient.
Among the commonly used supraglottic airway devices (SADs) are Baska, I-gel, and the Proseal laryngeal mask airway (LMA). Seal pressure is better with the supraglottic airways compared to the classic LMA, but first-time insertion success rates are fewer.3 The Baska mask (Logikal Health Products PTY Ltd., Morisset, NSW, Australia) is a relatively new SAD with a non-inflatable cuff, an esophageal drainage inlet, lateral channels to assist aspiration of gastric contents, and an integral bite-block.4
The I-gel is a disposable SAD containing a pliable, gel-like cuff requiring no inflation (Intersurgical Ltd, Berkshire United Kingdom). The device is produced from a thermoplastic elastomer.5 The stem is broad and flat and has an inelastic bite-block serving intended to stabilize the jaw and minimize axial rotation and malpositioning, as well as serving as a port to assist gastric tube insertion. The I-gel device contains no latex, and digital insertion into the oral cavity is not required. It also has an epiglottic rest and a broad, short stem, permitting excellent visualization of the glottis using a fiberoptic scope. The shorter tube is especially designed for ease of endotracheal tube insertion. Research has shown that I-gel takes no longer to insert than a classic LMA. The I-gel also permits adequate ventilation and entails no major airway complications.6 We hypothesized that the Baska and I-gel masks are comparable in advantages and disadvantages. We studied their strengths and weaknesses in patients undergoing general anesthesia for elective urological surgical procedures.
SUBJECTS AND METHODS
In this randomized-controlled, single-blind study, we enrolled concomitant patients admitted to the urology department of the hospital for surgical intervention with general anesthesia, when the operation was expected to last less than two hours. Other inclusion criteria were: American Society of Anesthesiologists (ASA) physical status classification I-III, no history of allergy, body mass index (BMI) less than 35 kg/m2, and age 18-85 years. Emergency cases, patients with neck, airway, or gastrointestinal problems, pregnant women, patients with mouth openings less than 3 cm, and patients with a risk of gastric aspiration were excluded from the study.
The study was conducted during July 2016-July 2017 at the Erzurum Regional Training and Research Hospital, Turkey. The hospital serves a population of 750 000 inhabitants with a 1200 bed-capacity. A monthly average of 700 operations are performed in the 19 surgical intervention theaters. The department of urology performs around ten surgical interventions per day (ureteroneocystostomy, transurethral prostatectomy, cystoscopy). The patients were recruited from urology clinics while waiting for their scheduled surgical interventions. Each day inpatients were invited to join the study. Patients who accepted and signed the informed consent form were added to the randomization pool. Ethical approval for the study was obtained from the local ethics board (number 2016/12-111, date 21/06/2016). We followed the CONSORT guidelines in reporting the study.7,8
All patients were uniformly premedicated with oral 0.1 mg/kg midazolam about an hour before induction of anesthesia. Anesthesia was induced with the patient lying supine with the head in a neutral position, using propofol 2-3 mg/kg, fentanyl 1-2 mcg/kg, 2% sevoflurane in 50% O2/air, remifentanil 0.10-0.20 mcg/kg/min. Positive pressure ventilation with sevoflurane 0.6-1 minimum alveolar concentration in 50% O2/air, was used for maintenance. Once loss of reflexes indicated that adequate relaxation had been achieved, a suitably lubricated Baska9 or I-gel6 # 3, 4 or 5 device was inserted digitally, in line with the manufacturer's instructions, by an anesthesiologist with previous experience in at least 20 such insertions. The jaw thrust maneuver was performed once the operator was satisfied that satisfactory insertion had been achieved, based on a poor capnographic curve and/or provision of satisfactory tidal volumes (partial loss exceeding 20% of set tidal volume). The device was then manually moved upward and downward. If the device was considered not to be functioning properly, despite this precaution, the operator attempted to reinsert it two more times. Repeated unsatisfactory results were interpreted as failure, and airway management was instead achieved using endotracheal intubation. At the conclusion of surgery, the mask was removed after establishing adequate respiration and patient's eye-opening response on verbal command. Intraoperatively, all patients received one gram of paracetamol as an intravenous infusion. Post-operative pain was treated as per protocol. The Baska insertion was done by well-trained staff members, who had inserted the device in at least 20 previous operations.
Outcomes
The main study outcome was defined as the duration of LMA insertion (seconds). Secondary outcome measures were the number of device placement attempts, the number of postoperative signs and symptoms (cough, breath holding, laryngeal spasm, lip trauma, blood on mask), and laryngopharyngeal morbidity (LPM) scores at 1 and 24 hours postoperatively. The LPM score (sum of sore throat, dysphagia and hoarseness scores) was calculated as follows: sore throat, 0= none, 1=minimal, 2=moderate, 3=severe; dysphagia, 0=none, 1=minimal, 2=moderate, 3=severe and cannot eat; hoarseness, 0=none, 1=minimal, 2=moderate, 3=severe and cannot speak. Other variables recorded were age (years), height (cm), weight (kg), BMI (kg/m2), tobacco use, ASA risk score, Mallampati score, LMA size, mouth opening (cm), thyromental distance, airway pressure, seal pressure (cm H2O), and total anesthesia duration (min).
Sample size and randomization
Sample size was based on the duration of LMA insertion. Considering a mean (SD) LMA insertion time of 10 (4) seconds, 100 participants in each group would be needed to detect a difference of 1.6 seconds between the groups with a power of 80% and an alpha error of 5%.10 Randomization was done one day before the operation using computer-generated random numbers. Sealed opaque envelopes were used for allocation concealment. Randomization was stopped after reaching 100 patients in each group, excluding failed insertions. The patients did not know which type of mask would be used and were not told until the end of data collection (24 hours). Data were collected by an individual who was not part of the study. Postoperative scoring of the masks was done by a nursing staff member who was unaware of the grouping.
Statistical analysis
Data are presented as mean and standard deviation (SD) or median (minimum-maximum) for numerical variables and number (percentage) for categorical variables. For analysis of continuous variables an independent samples t test or Mann-Whitney U test was applied depending on the data distribution, whereas for categorical variables the chi-square test was used. Multiple linear regression analysis was used to determine factors involved in LMA insertion time. P<.05 was considered statistically significant. ISM SPSS version 25 (IBM Armonk, NY) was used for the statistical analysis.
RESULTS
Of 211 patients who met inclusion criteria, 5 were excluded due to either emergency intervention (n=2), an airway problem (n=1), or a mouth opening less than 3 cm (n=2) (Figure 1). Two patients in each group were excluded from the analysis due to failed insertion of the mask. The mean age of the participants was 39.4 (11.9) years with a sex distribution of 136 (68.0%) men and 64 (32.0%) women. There were no differences in the baseline characteristics of the Baska and I-gel groups (Table 1).
Figure 1.

Participant flow diagram.
Table 1.
Baseline characteristics of the participants.
| Baska | I-gel | |
|---|---|---|
| Sex | ||
| Female | 38 (59.4) | 26 (40.6) |
| Male | 62 (45.6) | 74 (54.4) |
| Tobacco use | ||
| No | 72 (46.8) | 82 (53.2) |
| Yes | 28 (69.9) | 18 (39.1) |
| ASA Risk Score | ||
| 0 | 2 (50.0) | 2 (50.0) |
| 1 | 58 (51.8) | 54 (48.2) |
| 2 | 37 (48.1) | 40 (51.9) |
| 3 | 3 (42.9) | 4 (57.1) |
| Age (years) | 38.1 (13.3) | 40.8 (10.3) |
| Height (m) | 1.68 (0.09) | 1.69 (0.08) |
| Weight (kg) | 71.8 (10.9) | 74.27 (9.61) |
| BMI (kg/m2) | 25.4 (3.01) | 25.84 (2.56) |
| Mouth opening | 4.37 (0.51) | 4.40 (0.63) |
| Thyromental distance (cm) | 6.61 (0.83) | 6.44 (0.82) |
| Mallampati score | 2.14 (0.77) | 2.16 (0.81) |
| Anesthesia duration (min.) | 54.3 (12.6) | 51.43 (12.7) |
Values are n (%) or mean (SD).
Both masks could be successfully inserted at the first attempt in 95% of the cases. In each group, 5 cases required two attempts, and only two cases were considered a failure. Compared to I-gel, the Baska mask required a longer time for insertion, and airway pressure was higher. The median (minimum-maximum) duration of LMA insertion in the Baska and I-gel groups was 14 (6-25) and 7 (5-12) seconds respectively (z=- 10.934; P<.001) (Figure 2). The mean airway pressures were significantly different between the two groups (15.8 [1.9] and 14.9 [1.7] cm/H2O for Baska and I-gel respectively; t=3.668; P<.001) (Table 2). Seal pressures were not significantly different between the groups 0.08 (0.2) vs. 0.07 (0.2) cm/H2O in the Baska and I-gel groups respectively, t=1.35; P=.194).
Figure 2.
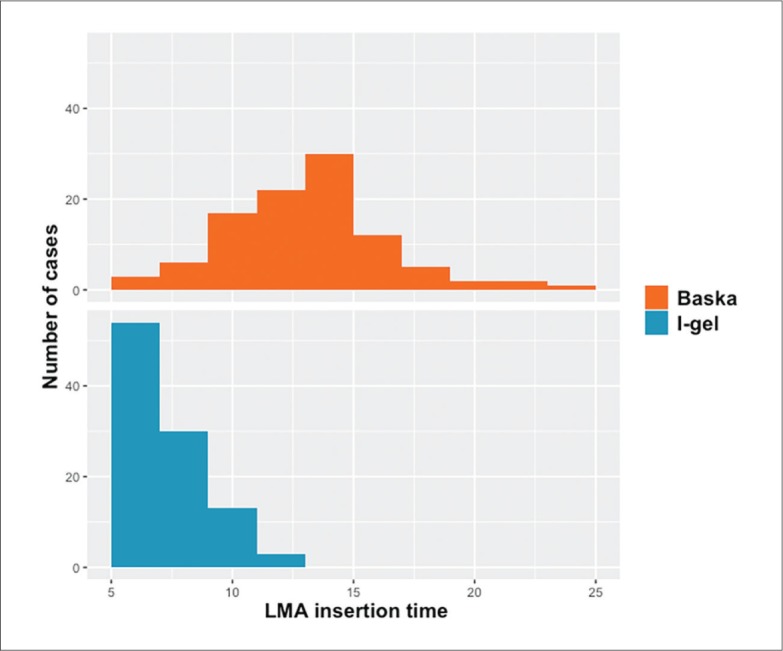
Distribution of LMA insertion times in the Baska and I-gel groups.
Table 2.
Duration of laryngeal mask airway insertion and airway pressures.
| Baska | I-gel | P value | |
|---|---|---|---|
| Median (min-max) insertion time (s) | 14 (6-25) | 7 (5-12) | <.001 |
| Mean (SD) airway pressure (cm/H2O) | 15.9 (1.9) | 14.9 (1.7) | <.001 |
| Mean (SD), median seal pressure (cm/H2O) | 0.75 (0.41), 0.6 | 0.56 (0.29), 0.5 | .194 |
Seal pressure excludes 176 0 observations.
Most of the postoperative complications were minimal or absent in both groups. Postoperative one-hour hoarseness and dysphagia and thus the LPM scores were significantly more common among the I-gel group. At 24 hours, the difference between the groups in hoarseness persisted, but the difference in dysphagia was not statistically significant (Table 3).
Table 3.
Distributions of the outcome variables between the Baska and I-gel groups.
| Baska n (%) | I-gel n (%) | Chi-square | P | |
|---|---|---|---|---|
| LMA insertionattempts | ||||
| 1 | 95 (95.0) | 94 (94.0) | 0.096 | .756 |
| 2 | 5 (5.0) | 6 (6.0) | ||
| Postextubation | ||||
| Cough | ||||
| No | 99 (99.0) | 95 (95.0) | 2.749 | .097 |
| Yes | 1 (1.0) | 5 (5.0) | ||
| Breath holding | ||||
| No | 100 (100.0) | 100 (100.0) | ||
| Yes | 0 (0.0) | 0 (0.0) | ||
| Laryngeal spasm | ||||
| No | 100 (100.0) | 98 (100.0) | 2.020 | .155 |
| Yes | 0 (0.0) | 0 (0.0) | ||
| Trauma to the lips or teeth | ||||
| No | 100 (100.0) | 99 (99.0) | 1.005 | .316 |
| Yes | 0 (0.0) | 1 (1.0) | ||
| Blood on mask | ||||
| No | 95 (95.0) | 95 (95.0) | 0.000 | .99 |
| Yes | 5 (5.0) | 5 (5.0) | ||
| One hour post operation | ||||
| Hoarseness | ||||
| No | 96 (96.0) | 77 (77.0) | 15.457 | <.001 |
| Yes | 4 (4) | 23 (23.0) | ||
| Dysphagia | ||||
| No | 100 (100.0) | 93 (93.0) | 7.254 | .007 |
| Yes | 0 (0.0) | 7 (7.0) | ||
| Hoarseness | ||||
| No | 99 (99.0) | 98 (98.0) | 0.338 | .561 |
| Yes | 1 (1.0) | 2 (2.0) | ||
| Laryngopharyngeal morbidity score | ||||
| 0 | 95 (95.0) | 75 (75.0) | 16.701 | <.001 |
| 1 | 5 (5.0) | 18 (18.0) | ||
| 2 | 0 (0.0) | 7 (7.0) | ||
| Hoarseness | ||||
| No | 100 (100.0) | 93 (93.0) | 7.254 | .007 |
| Yes | 0 (0.0) | 7 (7.0) | ||
| Dysphagia | ||||
| No | 100 (100.0) | 98 (98.0 | 2.020 | .155 |
| Yes | 0 (0.0) | 2 (2.0) | ||
| Hoarseness | ||||
| No | 100 (100.0) | 100 (100.0) | - | - |
| Yes | 0 (0.0) | 0 (0.0) | - | - |
| Laryngopharyngeal morbidity score | ||||
| 0 | 100 (100.0) | 92 (92.0) | 8.333 | .016 |
| 1 | 0 (0.0) | 7 (7.0) | ||
| 2 | 0 (0.0) | 1 (1.0) | ||
A linear regression model was built with LMA insertion time as the dependent variable. Variables entered into the model were tobacco use (dummy), mouth opening (cm), BMI (kg/m2), Mallampati score, LMA type (dummy), age (years), sex (dummy), and thyromental distance (cm). LMA type proved to be the only significant factor affecting LMA insertion time independent of other variables (t=14.884; P<.001; Beta=5.916 95% CI: 5.132-6.700 R2=0.55).
DISCUSSION
Our results show that the Baska and I-gel supraglottic masks are comparable in many ways, but the Baska mask requires a longer insertion time and is associated with higher airway pressures. The postoperative complications were minimal or absent in both groups. Postoperative hoarseness and dysphagia were less common in the Baska group.
Most of the confounding factors that could influence the results were similar in both groups and we had an adequate sample size. This enabled us to make sound conclusions, taking into account the effects of the covariates. However, there are also some limitations of this study. The Baska insertion was done by well-trained staff members, who had done at least 20 previous insertions. The requirement of more vigorous training might be a limitation of the Baska mask. Furthermore, we worked with a low-risk patient group. Including patients younger than 18 years or obese patients could yield different results.
Alexiev et al11 have reported that the first-time success rate for the insertion of the Baska mask was lower than that seen with the classical LMA (73% vs. 98%). However, others12 have reported overall success rates as 100%. In our study comparing Baska with I-gel, the number of attempts needed to place the device correctly was similar in both groups. This demonstrates that a training program with a minimum 20 insertions is sufficient for the correct placement of the Baska mask. Besides, we observed that it took a median of 14 seconds to place the Baska mask, which is similar to previous studies.13,14 The median insertion time for I-gel is shorter in our study compared to Helmy et al's, who reported a median insertion time as 15.6 seconds.15 Although the Baska mask requires a relatively long time for insertion, it can probably be decreased by training and experience. Any difficulty in the negotiation of the oropharyngeal curve could be easily overcome by pulling the tab of the Baska mask, which increases its distal curvature. Additionally, the supralaryngeal masks are devoid of an inflatable cuff; thus, the time required to inflate the cuff and volume adjustment is saved. However, it may be argued that the small differences of a few seconds between the insertion times of the masks may not be of much clinical significance.
The sealing pressures of the two masks in our study were similar. Although the Baska mask does not have an inflatable cuff, one study reported that it had significantly higher sealing pressure compared to the Proseal laryngeal mask.14 However, there are also reports that with its second posterior cuff fitted to improve the seal,16 the Proseal mask achieves 50% better sealing.17 There is a gradual improvement in the Baska mask seal against the glottis over the first 2-3 minutes, which might be due to the thermolability of the membranous mask, making it more adaptable to the shape of the laryngeal outlet over time.13,14
An inflatable cuff in SADs may be responsible for LPM.18,19 Others have disagreed with this explanation.11 Also, due to the need for extra maneuvers, blood stains may be more common with the Baska mask.20 In our study, blood was present in 5% of both Baska and I-gel patients. Despite the similar seal pressures, patients in the Baska group had significantly less postoperative hoarseness or dysphagia, which can be attributed to the physical structure of the mask.
The multiple linear regression analysis showed that among the studied variables, the only independent variable affecting insertion time was the type of the mask. Thus, controlling for the effects of potential confounders, we can state that the Baska mask requires a longer time for insertion. The findings of this study support our hypothesis that the Baska and I-gel masks are similar in most respects: both have reasonably acceptable insertion times and can be used for selected elective surgical procedures. A systematic review that compares insertion time is warranted.
Funding Statement
None.
REFERENCES
- 1.Hillman DR, Platt PR, Eastwood PR.. The upper airway during anaesthesia. Br J Anaesth 2003; 91:31-9. [DOI] [PubMed] [Google Scholar]
- 2.Jannu A, Shekar A, Balakrishna R, Sudarshan H, Veena GC, Bhuvaneshwari S.. Advantages, Disadvantages, Indications, Contraindications and Surgical Technique of Laryngeal Airway Mask. Arch Craniofacial Surg 2017; 18:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramaiah R, Das D, Bhananker S, Joffe A.. Extraglottic airway devices: A review. Int J Crit Illn Inj Sci 2014; 4:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexiev V, Salim A, Kevin LG, Laffey JG.. An observational study of the Baska_mask: a novel supraglottic airway. Anaesthesia 2012; 640-5. [DOI] [PubMed] [Google Scholar]
- 5.Asai T, Liu EH.. The i-gel, a new supraglottic airway. Japanese J Anesthesiol 2010; 59:794-7. [PubMed] [Google Scholar]
- 6.Using the i-gel® supraglottic airway. Intersurgical n.d. https://www.intersurgical.com/content/files/61747/-1200643841 (accessed June 17, 2018).
- 7.Moher D, Schulz KF, Altman D.. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA 2001; 285:1987-91. [DOI] [PubMed] [Google Scholar]
- 8.Sunay D, engezer T, Oral M, Aktürk Z.. The CONSORT Statement: Revised Recommendations for Improving the Quality of Reports of Parallel Group Randomized Trials. Euras J Fam Med 2013; 2:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mask Baska. Single use instructions. Logikal Heal Prod Pty Ltd; n.d. http://www.baskamask.com.au/_literature_624/Baska_Mask_Single_Use (accessed June 17, 2018). [Google Scholar]
- 10.Lenth R. Java Applets for Power and Sample Size [Computer software] 2009. https://homepage.divms.uiowa.edu/~rlenth/Power/ (accessed May 24, 2018).
- 11.Figueredo E, Vivar-Diago M, Muñoz-Blanco F.. Laryngo-pharyngeal complaints after use of the laryngeal mask airway. Can J Anaesth 1999; 46:220-225. [DOI] [PubMed] [Google Scholar]
- 12.Zaballos JM, Salinas U.. Clinical Evaluation of BaskaMaskR. A New Generation Extraglottic Airway Device for Positive Pressure Ventilation During General Anesthesia. Am. Soc. Anesthesiol 2014. [Google Scholar]
- 13.van Zundert T, Gatt S.. The Baska Mask – A new concept in self-sealing membrane cuff extraglottic airway devices using a sump and two gastric drains: A critical evaluation. J Obstet Anaesth Crit Care 2012; 2. [Google Scholar]
- 14.Al-Rawahi SAS, Aziz H, Malik AM, Khan RM, Kaul N.. A comparative analysis of the Baska® Mask vs. Proseal® laryngeal mask for general anesthesia with IPPV. Anaesth Pain Intensive Care 2013; 17:233-6. [Google Scholar]
- 15.Helmy AM, Atef HM, El-Taher EM, Henidak AM.. Comparative study between I-gel and classical laryngeal mask airway in anesthetized spontaneously ventilated patients. Egypt J Anaesth 2010; 26:47-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brain AIJ, Verghese C, Strube PJ.. The LMA ‘ProSeal’- a laryngeal mask with an oesophageal vent. Br J Anaesth 2000; 650-4. [DOI] [PubMed] [Google Scholar]
- 17.Cook TM, Lee G, Nolan JP.. The ProSeal laryngeal mask airway: a review of the literature. Can J Anaesth 2005; 739-60. [DOI] [PubMed] [Google Scholar]
- 18.Wong JG, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS.. Impact of laryngeal mask cuff pressures on the incidence of sore throat. Paediatr Anaesth 2009; 464-9. [DOI] [PubMed] [Google Scholar]
- 19.Burgard G, Mollhoff T, Prien T.. The effect of laryngeal mask cuff pressure on postoperative sore throat incidence. J Clin Anesth 1996; 198-201. [DOI] [PubMed] [Google Scholar]
- 20.Bindal M, Sabuncu Ü, Demir A, Özgök A.. Comparison of Baska mask and classical laryngeal mask for seal pressures in ambulatory urological surgery. Turkiye Klin J Anest Reanim 2018; 16:1-7. [Google Scholar]