ABSTRACT
BACKGROUND:
Frailty status among Saudi adults is unknown due to the lack of a reliable and validated Arabic instrument that can be applied directly to the Saudi population.
OBJECTIVE:
Cross-culturally adapt and validate the Arabic version of the FRAIL scale in community-dwelling older adults.
DESIGN:
Cross-sectional.
SETTINGS:
The outpatient clinic of a tertiary care hospital.
SUBJECTS AND METHODS:
People aged ≥65 years who attended the outpatient clinic were recruited to participate. The original FRAIL scale was translated into Arabic and psychometric properties were examined for each item on the FRAIL scale and the total score, test-retest reliability over two visits with a one-week interval. We assessed criterion-related validity with the Fried Frailty Index as a reference measure and construct validity with other related measurements.
MAIN OUTCOME MEASURES:
Arabic version of the FRAIL Scale, grip strength, the Mini-Mental State Examination, a short physical performance battery, the Timed Up and Go test, the Fried Frailty Index, and the Duke Comorbidity Index.
SAMPLE SIZE AND CHARACTERISTICS:
47 community-dwelling older adults (66% male, mean [SD] age 70 [4] years).
RESULTS:
The Arabic version of the FRAIL scale showed acceptable internal consistency (Cronbach's alpha=0.786) and good test-retest reliability within a one-week interval (intraclass correlation coefficient=0.77). Statistically significant correlations were found between the Arabic FRAIL scale, the Fried Frailty Index, and other frailty related measurements such as the Mini-Mental State Examination, the Duke comorbidity index, the Short Physical Performance Battery, and the Timed Up And Go Test. Using the Fried Frailty Index as the criterion measure, the Arabic FRAIL scale demonstrated good diagnostic accuracy for frailty (AUC=0.71). The optimal cutoff point for frailty on the Arabic FRAIL scale was 3, which yielded a sensitivity of 72% and specificity of 67%. The prevalence of frailty varied according to the FRAIL-AR (37%) and the Fried Frailty Index (28%).
CONCLUSIONS:
The FRAIL scale was successfully translated and culturally-adapted to Saudi older adults. The adapted Arabic version demonstrated acceptable internal consistency, test-retest reliability, and validity. Further study is needed to establish the validity of FRAIL-AR scale in a larger cohort in Saudi Arabia
LIMITATIONS:
The small sample size and single geographic area may affect the generalizability of the results across the country.
CONFLICT OF INTEREST:
None.
INTRODUCTION
The size of the elderly population in Saudi Arabia will increase significantly over the next few decades. The United Nations projected that in 2017 about 5.6% of Saudi Arabia's population would be 60 or older. This percentage will increase to 22.9% by 2050.1 This significant growth in the number of elderly presents numerous challenges to the health-care system because of the high prevalence of comorbidities such as diabetes, arthritis, and heart diseases, which require close observation and continuous care.
Normal aging is associated with a decline in different body systems such as sensory, musculoskeletal, cardiovascular, and cognitive function.2–4 Frailty, which is associated with aging, can lead to functional limitations, an increased risk of falling, greater vulnerability to adverse outcomes, and institutionalization.5–7 Due to the current significant growth in the elderly population in Saudi Arabia, the frailty issue becomes more important now than ever.8
Frailty can be defined as a clinical geriatric syndrome that is associated with vulnerability to external stressors.9, 10 Research has suggested that frailty may become one of the most serious public health problems in the elderly population.11, 12 According to a recent systematic review of studies from different locations, the prevalence of frailty ranges from 4% in China to 51% in Cuba.13
Frailty is a dynamic condition and with proper intervention can be altered or improved, but without proper intervention, can worsen and increase susceptibility to disability.14 Therefore, recognizing frailty states through early assessment can decrease the burden in the elderly population.
One of the earliest attempts to characterize this concept was put forth by Fried.15 She proposed a phenotype of frailty that involved five domains including loss of weight, exhaustion, grip strength weakness, gait speed, and physical activity level. Using this index, she characterized adults as robust, pre-frail and frail. Investigators have demonstrated that the index was associated with falls, hospitalizations, disability and death.11 Ensrud and colleagues simplified the index into three measures including weight loss, difficulty getting up from a chair and low energy. Her index, the Study of Osteoporotic Fractures index (SOF index), predicted disability, fractures, risk of falling and mortality in both males and females in the Cardiovascular Health Study (CHS).16, 17 Although frequently used for assessing frailty, in some instances obtaining gait speed and grip strength using a dynamometer are not easy. An alternative is using the FRAIL scale, which was originally proposed by the Geriatric Advisory Panel of the International Academy of Nutrition, Health and Aging Task Force, uses a five-point scale that involves fatigue, resistance, ambulation, number of chronic conditions, and loss of weight.18 The three main domains come from the SF-36 questions.19 It can be easily used by geriatricians and healthcare professionals in the primary care or geriatric clinics as an assessment measure in clinical practice. It can also be used as self-administered instrument, or by telephone.10, 20, 21 A relationship has existed between the FRAIL scale, and mortality, disability, and functional limitations in older adults.22 The scale was translated from English and validated in different languages, including Spanish,23 Chinese,24 and German,25 but there is no validated comprehensive assessment of frailty in Arabic.
Given the dramatic growth in the elderly population in Saudi Arabia, the issue of frailty in Saudi population is now more crucial than before. Although numerous studies have been done on frailty in different countries, frailty status among Saudi adults is unknown due to the lack of validated Arabic instruments that can be applied directly to the Saudi population. The FRAIL scale needs to be culturally adapted and fully validated to use it with older Saudi adults. Thus, the aims of our study include cross-culturally adaptation and translation of the FRAIL scale into the Arabic language, and measurement of internal consistency, criterion-related validity (concurrent), test-retest reliability, and construct validity among Arab-speaking (Saudi) community-dwelling older adults.
SUBJECTS AND METHODS
The research design was a cross-sectional. People aged 65 years and older who came to the out-patient clinic in 9 months from January 2018 to September 2018 were recruited to participate in the current study. All participants provided written informed consent. The research was approved by the ethical committee of the Prince Sattam Bin Abdulaziz University. Enrollment criteria included the ability to walk independently within the household with or without assistive devices. Participants were excluded if they had cognitive impairment, which was determined by an inability to follow two-step commands or understand the informed consent process, a score below 24 on the Mini-Mental State Examination (MMSE), or a medical condition that was not stable and could affect participation, or were unable to read or understand Arabic.
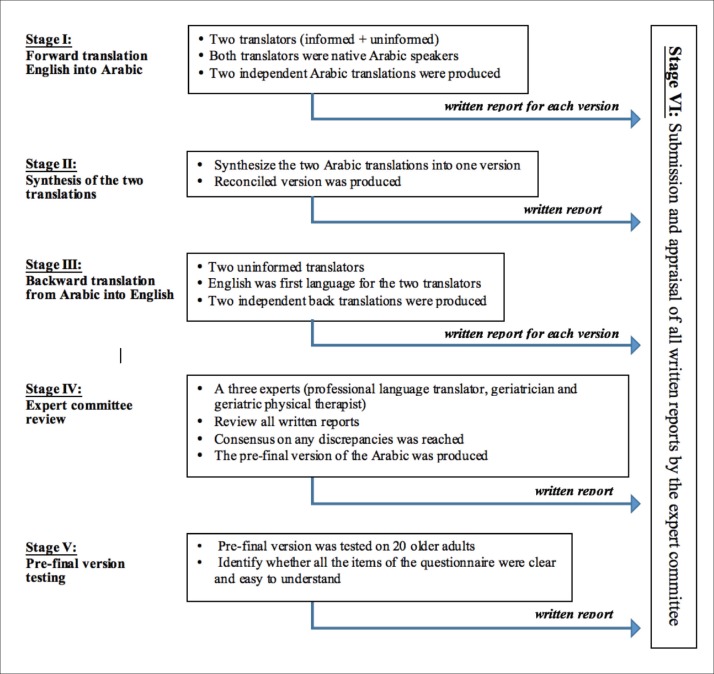
Translation and cross-cultural adaptation
Translation and cross-cultural adaptation was done according to the Beaton guidelines (Figure 1).26 The process included the following phases: forward translation, synthesis of the translation, backward translation, expert committee and pre-final version testing. First, the FRAIL scale was forward translated from English into Arabic by two independent Arabic native speakers, both of whom were bilingual. The first translator was informed about the concepts being examined in the FRAIL scale, and the second translator was a professional English translator without a medical background. Two independent Arabic translations were obtained. Second, an expert committee reviewed the two translated versions and a reconciled version was obtained. Next, the reconciled Arabic version was backward translated into the original language by two bilingual independent translators with English as their first language. Both translators had no knowledge of the original instrument. Two independent English translations were produced. Then, the backward translated English version was evaluated by an expert committee (include professional language translator, geriatrician and geriatric physical therapist). The expert committee ensured that the semantic, idiomatic, conceptual and experiential equivalences were obtained, via consensus among the committee. Then, the pre-final version the FRAIL scale was applied and tested on a group of older adults (n=20) to identify whether all the items of the questionnaire were clear and easy to understand. The pre-final version was approved and ready to use. The approved version of the Arabic FRAIL scale (FRAIL-AR) is shown in Supplementary Table 1.
Figure 1.
Flowchart of the cross-cultural adaptation process.
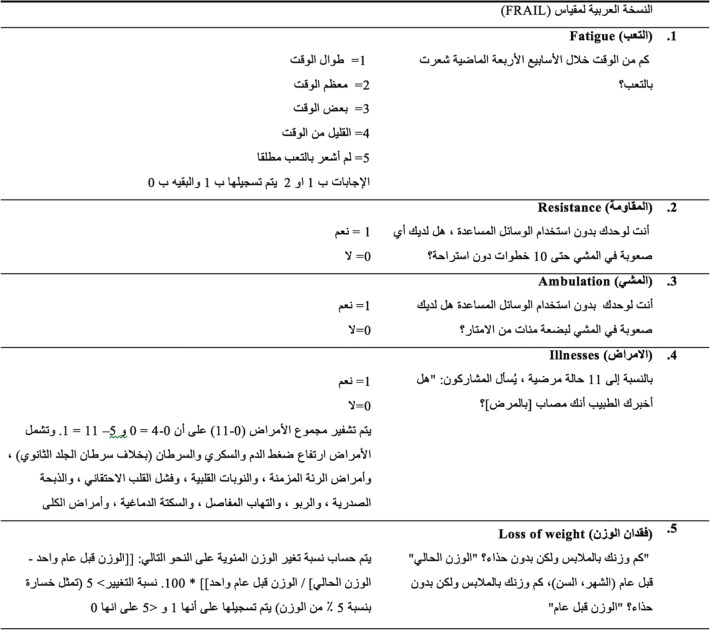
Supplementary Table 1.
The Arabic version of the fatigue, resistance, ambulation, illnesses, and loss of weight (FRAIL-AR) scale. A score of 0 indicates nonfrail, 1–2 prefrail, and 3 or more indicates frail.
Frailty Assessment (FRAIL scale)
Five different domains were included in the FRAIL scale: fatigue, resistance, illness, ambulation, and weight loss.18 The FRAIL scale scores ranged from 0 (best) to 5 (worst). Scores from 3-5 are perceived as frail, 1 to 2 as pre-frail, and 0 represents no frailty. Fatigue was assessed by asking subjects if they felt exhaustion in the last 4 weeks with a response of ‘all of the time’ or ‘most of the time’ scored as 1 point. For resistance, subjects were asked if they had difficulty ascending 10 steps independently without resting and without assistive devices; A “yes” response was scored as 1 point. Ambulation was assessed by asking about the difficulty of walking several hundred meters by themselves and without assistive devices; A “yes” response was scored as 1 point. For Illness, subjects who had 5 or more chronic conditions out of 11 total illnesses, were scored 1 point; these conditions included hypertension, diabetes, cancer, chronic lung disease, heart attack, congestive heart failure, angina, asthma, arthritis, stroke, or kidney disease. Finally, for weight loss, subjects were given 1 point if they had a weight loss of 5 percent or more in the previous year by asking subjects about current weight without shoes on, and their weight one year ago without shoes on. The percentage was calculated as the weight 1 year ago minus the current weight, and divided by weight 1 year ago.
Psychometric measurements
The number of subjects enrolled in the study was higher than the suggested minimum sample size.27, 28 To determine the validity of the FRAIL-AR scale: First, the internal consistency was examined by looking at correlations between the FRAIL scale items and total score. Second, the Fried Frailty Index (FFI)15 was used to establish the criterion-related validity with the FRAIL-AR scale. Scoring was based on the presence of five frailty criteria: weight loss (defined by asking subjects if they had weight loss of five kilogram or more in the last year), exhaustion (subjects were asked two questions from the Center for Epidemiological Studies depression scale: “I felt that everything I did was an effort” and “I could not get going”), slow walk speed (5-meter walking test, normalized by gender and height), grip strength (reference values, stratified by gender and body mass index were used), and physical activity level (assessed by asking subject about leisure time activities, adopted from the Minnesota Leisure Time Activities Questionnaire).15 For each criteria score of 0 or 1 was assigned. Participants were categorized into three groups based on total score: 0 indicated nonfrail, 1 to 2 prefrail, 3 or more frail.15 Third, test–retest reliability for the FRAIL scale was determined over two testing sessions one-week apart. A time interval of one week was short enough to make sure that no real change had occurred, and long enough that learning or practice effects could be minimized.29 Fourth, the FRAIL scale was validated against different measurements related to frailty in the elderly population such as grip strength assessed using a digital handheld dynamometer (JAMAR PLUS+, Sammons, Bolingbrook, IL) to quantify grip strength. Participants performed a practice session and two testing trials. The average of both trials was included in the main analysis. The handheld dynamometer has strong concurrent validity and excellent reliability with intraclass correlation coefficients ranging from 0.90 to 0.97.30 The MMSE was used to examine the cognitive function in the current sample.31 The Arabic version of the MMSE has high validity and reliability, and high sensitivity and specificity.32 The Duke comorbidity index is a simple 18-item self-reported questionnaire that was used to count the number of chronic conditions. This index is well validated and has been used in different cohorts including community-dwelling adults and people with stroke.33, 34 In addition, the Short Physical Performance Battery (SPPB),35 and the timed Up and Go Test (TUG)36 were included to evaluate lower extremity function. Finally, the body mass index was estimated as weight (kg)/height (m2). These measures were obtained by a trained physical therapist.
Statistical analysis
Data were analyzed using Stata statistical software (version 15.1, Stata Corp, College Station, TX). Descriptive data for subject demographics and clinical characteristics were reported. Mean and standard deviations were used for continuous variables, and numbers and percentages were used for categorical variables. Intraclass correlation coefficients (ICC, model 3.1, two-way mixed-effects model), and 95% confidence intervals (95% CI) were used for test-retest reliability. The ICC is known as the ratio of between subject variability to the total variability.37 The ICC index ranges from zero to one; values indicate high reliability if they are closer to one.37 The internal consistency of the FRAIL-AR scale was evaluated by looking at the item-total correlation and the Cronbach's alpha coefficients. Criterion-related validity (concurrent) between the FRAIL-AR and FFI was examined by kappa coefficients. In addition, construct validity was examined by using Spearman's rho correlation coefficients between the FRAIL-AR scale, MMSE, grip strength, comorbidity index, SPPB test, and the TUG test. The frequency of frailty on the FRAIL-AR scale and FFI was compared using the chi-square test. The receiver operating curve (ROC) analysis was done to assess the criterion-related validity of the FRAIL-AR scale plus area under the curve (AUC) was computed. The alpha level was set at .05 for all analyses to determine significance.
RESULTS
Forty-seven community-dwelling older adults were enrolled in the current research. The mean (SD) age was 70 (4) years. Sixty-seven percent (31/46) of the participants were male (Table 1). Table 2 presents the results of the internal consistency of the FRAIL-AR scale. The internal consistency with the overall Cronbach's alpha was 0.79. The corrected item-total correlations ranged from 0.44 to 0.69. For the test-retest reliability, ICC was 0.77 (95% CI, 0.58–0.87).
Table 1.
Demographic and clinical characteristics of study participants (n=47).
| Age (y) | 70 (4.3) | 65–79 |
| Male | 31 (66) | - |
| Female | 16 (34) | - |
| No formal education | 5 (10.6) | - |
| Primary school | 22 (46.8) | - |
| Middle school or more | 20 (42.5) | - |
| Marital status | ||
| Single | 4 (8.5) | - |
| Married | 43 (91.5) | - |
| BMI (kg/m2) | 23.5 (3.5) | 17–37 |
| Grip strength | 18.5 (5.1) | 8–35 |
| MMSE | 25.6 (1.6) | 24–29 |
| Number of comorbidities | 6 (3) | 2–12 |
| SPPB total | 8.9 (2.6) | 6–12 |
| TUG | 13.9 (5.2) | 8–29 |
Data are mean (standard deviation) and range or number (percentage). BMI: Body Mass Index, MMSE: Mini-Mental State Examination, SPPB: Short Physical Performance Battery, TUG: Timed Up and Go.
Table 2.
Internal consistency of the Arabic version of the FRAIL scale.
| Item | Corrected item-total correlation | Cronbach's alpha if item deleted |
|---|---|---|
| Fatigue | 0.556 | 0.749 |
| Resistance | 0.694 | 0.702 |
| Ambulation | 0.604 | 0.734 |
| Illnesses | 0.437 | 0.787 |
| Loss of weight | 0.535 | 0.756 |
Overall Cronbach's alpha=0.786
The FRAIL-AR was significantly correlated with the FFI (kappa=0.320, P=.004). In the ROC analyses, the AUC for the FRAIL-AR was 0.77 (95% CI, 0.544–0.878), using the FFI as a reference measure (Figure 2). A cut-point of 3 was used as an optimal point for the FRAIL-AR, which yielded a sensitivity of 72% and specificity of 67%. In addition, a prevalence of frailty between the FRAIL scale and FFI is shown in Table 3. According to the FRAIL-AR 17 (37%) subjects were classified as frail, while 13 persons (28%) were classified as frail by the FFI (Table 3).
Figure 2.
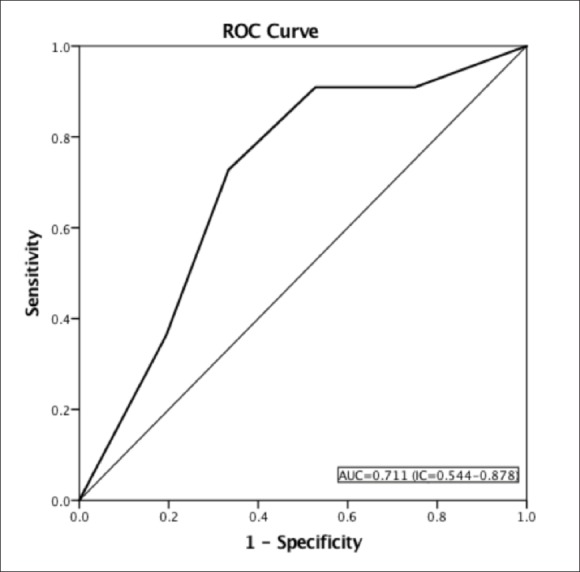
ROC curve for the Arabic version of the FRAIL scale using the Fried Frailty Index (FFI) as the reference criteria.
Table 3.
Frequency of frailty by the FFI and the FRAIL-AR Scale (n=47).
| FRAIL scale | Fried frailty index n (%) | P | ||
|---|---|---|---|---|
| Nonfrail | Prefrail | Frail | ||
| Nonfrail | 3 (6.4) | 3 (6.4) | 0 (0) | .001 |
| Prefrail | 1 (2.1) | 18 (38.3) | 5 (10.6) | |
| Frail | 0 (0) | 9 (19.1) | 8 (17) | |
P=.001 (chi-square test)
The FRAIL-AR was significantly positively associated with age and number of comorbidities, indicating that a high level of frailty was associated with increased age and an increased number of chronic illnesses. The FRAIL scale was also associated with the total time to finish the TUG test. Moreover, a significant negative association was shown between the FRAIL-AR and the MMSE, grip strength, and SPPB (Spearman's rho ranged from −.13 to −.39) (Table 4).
Table 4.
Correlations between the Arabic version of the FRAIL scale and other related measurements (n=47).
| Variables | FRAIL scale total score | |
|---|---|---|
| Correlation coefficient | P | |
| Age | 0.284 | .005 |
| Number of comorbidities | 0.255 | .008 |
| MMSE | −0.182 | .003 |
| Grip strength | −0.285 | .001 |
| SPPB | −0.395 | .006 |
| TUG | 0.411 | .004 |
MMSE: Mini-Mental State Examination, SPPB: Short Physical Performance Battery, TUG: Timed Up and Go
DISCUSSION
The current research aimed to translate, cross-culturally adapt and validate the FRAIL-AR scale in Saudi older adults. The FRAIL-AR scale demonstrated a good internal consistency plus adequate test-retest reliability. Moreover, it was correlated with other related measurements, indicating concurrent validity. The FRAIL-AR scale provides an easy and quickly administered tool to assess frailty. The FRAIL-AR is the first frailty measure validated in Arabic. For reliability, the ICC and Cronbach's alpha values indicated that the FRAIL-AR scale shows high reliability and is internally consistent (ICC 0.77 and Cronbach's alpha 0.79). Our results were relatively close to the ICCs previously reported for the Chinese version within a 7-15 day interval (ICC=0.71),24 and in the Mexican Spanish version of the FRAIL scale with a 1-week interval (ICC=0.82),23 suggesting the stability of the FRAIL-AR over time.
A significant concurrent validity (i.e. criterion-related validity) was found between FRAIL-AR and the FFI, a commonly used frailty tool.15 Our results were consistent with previous findings such as the Spanish FRAIL scale15 and the Korean FRAIL,21 but only a fair correlation can be justified by the objective nature of some measurements in the FFI, whereas the FRAIL scale is solely a self-reported instrument that depends on the subject's report. The FRAIL-AR total score was correlated with other frailty related measurements (Spearman correlation ranged from −0.13 to −0.39). All correlations were significant and the direction and strength of the correlation coefficient was consistent with previous findings.23 Moreover, the scale correlated with age, number of comorbidities, grip strength, TUG, and SPPB, which further validates the FRAIL-AR. A similar association was found in previous studies.20, 23 These measurements were included in the main analysis to assess construct validity as they have been strongly related to frailty. The MSSE is associated with frailty; frail older adults have worse MMSE scores.39 In addition, physical performance measures such as SPPB are a good predictor in identification of frail people.40 The TUG test, number of comorbidities and grip strength were strongly associated with frailty status in older adults.41–43
The discrimination ability of the FRAIL-AR scale (AUC=0.711) was slightly higher than previous published results (AUC=0.681),24 but lower than the Chinese FRAIL scale (AUC=0.91).44 A good frailty screening instrument should have the ability to discriminate frail form nonfrail people (have high sensitivity and specificity).20 The FRAIL-AR scale was able to detect most frail participants (73%), but the Brazilian FRAIL scale had higher sensitivity.24 This discrepancy may be due to different cut off values and different reference measures.
Although the sample size was above the suggested minimum of 30 subjects for psychometric testing, caution should be taken when interpreting results as the sample may not be representative of the population. If the small sample size underestimated the frequency of frail elderly, the sensitivity and specificity may have been influenced. In addition, the current sample was recruited from the outpatient clinic and from a single geographic area, so this may limit the generalizability of the results. The nature of the study design (cross-sectional descriptive) limits the predictive validity of the FRAIL-AR scale.
In the present study, the Arabic version of the FRAIL scale was cross-culturally adapted so it can be used to assess frailty in an Saudi elderly population. The criterion-related validity and construct validity, and test-retest reliability were established. This measure was correlated with other validated physical and functional-performance measures in older adults. However, a future longitudinal study of Saudi older adults is needed to further establish the validity of FRAIL-AR scale in a larger cohort in Saudi Arabia.
Funding Statement
None.
REFERENCES
- 1.United Nations, Department of Economic and Social Affairs PD. World Population Ageing 2017. United Nations. 2017;124. [Google Scholar]
- 2.Segev-Jacubovski O, Herman T, Yogev-Seligmann G, Mirelman A, Giladi N, Hausdorff JM.. The interplay between gait, falls and cognition: can cognitive therapy reduce fall risk? Expert Rev Neurother. 2011. July;11(7):1057–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P, et al.. Hypertension, Orthostatic Hypotension, and the Risk of Falls in a Community-Dwelling Elderly Population: The Maintenance of Balance, Independent Living, Intellect, and Zest in the Elderly of Boston Study. J Am Geriatr Soc. 2011. March 10;59(3):383–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lord SR. Visual risk factors for falls in older people. Age Ageing. 2006. September;35 Suppl 2:ii42–ii45. [DOI] [PubMed] [Google Scholar]
- 5.Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB, Walston JD.. Designing Randomized, Controlled Trials Aimed at Preventing or Delaying Functional Decline and Disability in Frail, Older Persons: A Consensus Report. J Am Geriatr Soc. 2004;52(4):625–34. [DOI] [PubMed] [Google Scholar]
- 6.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al.. Frailty and risk of falls, fracture, and mortality in older women: The study of osteoporotic fractures. Journals Gerontol - Ser A Biol Sci Med Sci. 2007;62(7):744–51. [DOI] [PubMed] [Google Scholar]
- 7.Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, et al.. Frailty in older men: Prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–23. [DOI] [PubMed] [Google Scholar]
- 8.Nations U. World Population Ageing [highlights]. 2017; [Google Scholar]
- 9.Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, et al.. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009. December;13(10):881–9. [DOI] [PubMed] [Google Scholar]
- 10.Abellan Van Kan G, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B.. The I.A.N.A. task force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12(1):29–37. [DOI] [PubMed] [Google Scholar]
- 11.Rockwood K, Howlett SE, MacKnight C, Beattie BL, Bergman H, Hébert R, et al.. Prevalence, attributes, and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci. 2004;59(12):1310–7. [DOI] [PubMed] [Google Scholar]
- 12.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K.. Frailty in elderly people. In: The Lancet. 2013. p. 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siriwardhana DD, Hardoon S, Rait G, Weerasinghe MC, Walters KR.. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018;8(3):e018195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu CK, Fielding RA.. Exercise as an intervention for frailty. Clin Geriatr Med. 2011. February 1;27(1):101–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al.. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. [DOI] [PubMed] [Google Scholar]
- 16.Ensrud KE. Comparison of 2 Frailty Indexes for Prediction of Falls, Disability, Fractures, and Death in Older Women. Arch Intern Med. 2008;168(4):382. [DOI] [PubMed] [Google Scholar]
- 17.Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al.. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009. March;57(3):492–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morley JE, Malmstrom TK, Miller DK.. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged african americans. J Nutr Health Aging. 2012;16(7):601–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabbah I, Drouby N, Sabbah S, Retel-Rude N, Mercier M.. Quality of life in rural and urban populations in Lebanon using SF-36 health survey. Health Qual Life Outcomes. 2003. August 6;1:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morley JE, Vellas B, Abellan van Kan G, Anker SD, Bauer JM, Bernabei R, et al.. Frailty Consensus: A Call to Action. J Am Med Dir Assoc. 2013. June;14(6):392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Kan GA, Rolland YM, Morley JE, Vellas B.. Frailty: Toward a Clinical Definition. J Am Med Dir Assoc. 2008;9(2):71–2. [DOI] [PubMed] [Google Scholar]
- 22.Rivera-Almaraz A, Manrique-Espinoza B, Ávila-Fune JA, Chatterji S, Naidoo N, Kowal P, et al.. Disability, quality of life and all-cause mortality in older Mexican adults: association with multimorbidity and frailty. BMC Geriatr. 2018. December 4;18(1):236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosas-Carrasco O, Cruz-Arenas E, Parra-Rodríguez L, García-González AI, Contreras-González LH, Szlejf C.. Cross-Cultural Adaptation and Validation of the FRAIL Scale to Assess Frailty in Mexican Adults. J Am Med Dir Assoc. 2016. December 1;17(12):1094–8. [DOI] [PubMed] [Google Scholar]
- 24.Dong L, Qiao X, Tian X, Liu N, Jin Y, Si H, et al.. Cross-Cultural Adaptation and Validation of the FRAIL Scale in Chinese Community-Dwelling Older Adults. J Am Med Dir Assoc. 2018;19(1):12–7. [DOI] [PubMed] [Google Scholar]
- 25.Braun T, Gröneberg C, Thiel C.. German translation, cross-cultural adaptation and diagnostic test accuracy of three frailty screening tools. Prisma-7, Frail scale and Groningen Frailty Indicator. Z Gerontol Geriatr. 2017; [DOI] [PubMed] [Google Scholar]
- 26.Beaton DE, Bombardier C, Guillemin F, Ferraz MB.. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000. December 15;25(24):3186–91. [DOI] [PubMed] [Google Scholar]
- 27.Onwuegbuzie AJ, Collins KMT.. A typology of mixed methods sampling designs in social science research. Qual Rep. 2007;12(2):281–316. [Google Scholar]
- 28.Sousa VD, Rojjanasrirat W.. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. Vol. 17, Journal of Evaluation in Clinical Practice. 2011. p. 268–74. [DOI] [PubMed] [Google Scholar]
- 29.Leppink J, Pérez-Fuster P.. We need more replication research - A case for test-retest reliability. Perspect Med Educ. 2017. June;6(3):158–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mathiowetz V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup Ther Int. 2002;9(3):201–9. [DOI] [PubMed] [Google Scholar]
- 31.Folstein M, Folstein S.. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 32.Albanna M, Yehya A, Khairi A, Dafeeah E, Elhadi A, Rezgui L, et al.. Validation and cultural adaptation of the Arabic versions of the Mini-Mental Status Examination - 2 and Mini-Cog test. Neuropsychiatr Dis Treat. 2017;13:793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rigler SK, Studenski S, Wallace D, Reker DM, Duncan PW.. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clin Rehabil. 2002. June;16(4):420–8. [DOI] [PubMed] [Google Scholar]
- 34.Studenski SA, Lai SM, Duncan PW, Rigler SK.. The impact of self-reported cumulative comorbidity on stroke recovery. Age Ageing. 2004. March;33(2):195–8. [DOI] [PubMed] [Google Scholar]
- 35.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al.. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994. March;49(2):M85–94. [DOI] [PubMed] [Google Scholar]
- 36.Podsiadlo D, Richardson S.. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. [DOI] [PubMed] [Google Scholar]
- 37.Koo TK, Li MY.. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016. June;15(2):155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jung H-W, Jang I-Y, Lee YS, Lee CK, Cho E-I, Kang WY, et al.. Prevalence of Frailty and Aging-Related Health Conditions in Older Koreans in Rural Communities: a Cross-Sectional Analysis of the Aging Study of Pyeongchang Rural Area. J Korean Med Sci. 2016. March;31(3):345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brigola AG, Rossetti ES, Santos BR dos, Neri AL, Zazzetta MS, Inouye K, et al.. Relationship between cognition and frailty in elderly: A systematic review. Dement Neuropsychol. 2015;9(2):110–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pritchard JM, Kennedy CC, Karampatos S, Ioannidis G, Misiaszek B, Marr S, et al.. Measuring frailty in clinical practice: a comparison of physical frailty assessment methods in a geriatric out-patient clinic. BMC Geriatr. 2017;17(1):264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Curcio C-L, Henao G-M, Gomez F.. Frailty among rural elderly adults. BMC Geriatr. 2014. December 10;14(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Syddall H, Cooper C, Martin F, Briggs R, Aihie Sayer A.. Is grip strength a useful single marker of frailty? Age Ageing. 2003. November 1;32(6):650–6. [DOI] [PubMed] [Google Scholar]
- 43.Savva GM, Donoghue OA, Horgan F, O'Regan C, Cronin H, Kenny RA.. Using timed up-and-go to identify frail members of the older population. Journals Gerontol - Ser A Biol Sci Med Sci. 2013;68(4):441–6. [DOI] [PubMed] [Google Scholar]
- 44.Aprahamian I, Cezar NO de C, Izbicki R, Lin SM, Paulo DLV, Fattori A, et al.. Screening for Frailty With the FRAIL Scale: A Comparison With the Phenotype Criteria. J Am Med Dir Assoc. 2017;18(7):592–6. [DOI] [PubMed] [Google Scholar]