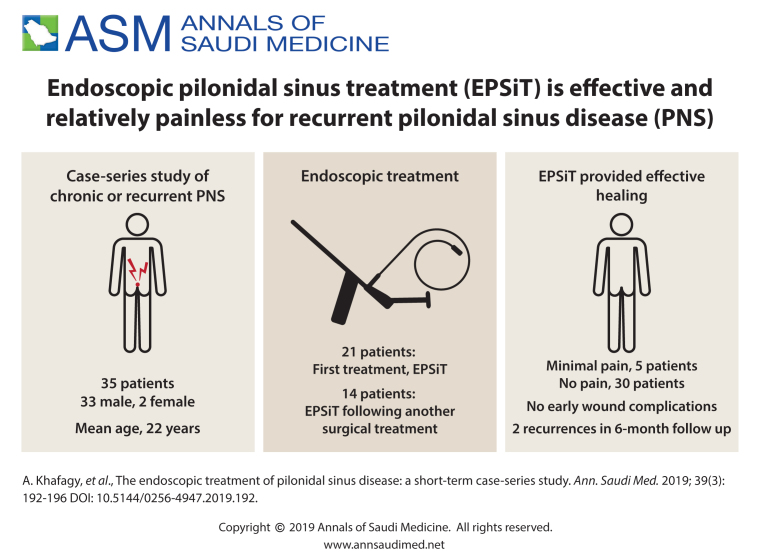
ABSTRACT
BACKGROUND:
Pilonidal disease (PNS) is a common inflammatory disease that can significantly impact the quality of life of the patient. Previous open techniques for the management of this condition have been unsatisfactory, with high recurrence rates reported.
OBJECTIVE:
Investigate a new endoscopic procedure for the management of PNS disease.
DESIGN:
Case series.
SETTING:
Single hospital in Kuwait.
PATIENTS:
From April 2014 to October 2017, patients with symptomatic chronic or recurrent PNS were consecutively enrolled to undergo the endoscopic pilonidal sinus treatment (EPSiT) procedure.
MAIN OUTCOME MEASURES:
Control of pain, wound complications, recurrence rate over a 6-month follow up.
SAMPLE SIZE:
35 patients.
RESULTS:
The mean age of the patients was 22 years, with 33 (94%) males. Fourteen (40%) presented with recurrent disease and were recommended to undergo an EPSiT procedure. A single tract was used in 32 (91%) of the cases, with an average operative time of 51 mins. On follow-up 5 patients reported minimal pain judging by the need of only mild analgesics for the control of pain. No patient experienced early wound complications necessitating hospitalization. There were 2 (6%) recurrences encountered by the time of the 6-month follow-up period.
CONCLUSION:
In these early results, the EPSiT procedure provided effective healing with acceptable recurrence rates and aesthetics. In addition, the procedure allows the surgeon to see the PNS, fistula tracts or any abscess cavities.
LIMITATIONS:
Short follow-up period with a small number of patients
CONFLICTS OF INTEREST:
None.
INTRODUCTION
Pilonidal sinus (PNS) disease is an inflammatory condition that affects the gluteal folds of the body. It is known to occur mainly in young men and is associated with obesity, sedentary lifestyle, local irritation and hirsutism.1–3 It causes subcutaneous abscesses and recurrent acute or chronic infections of the natal cleft area.4 The etiology of this disease is categorized by a follicular and perifollicular inflammatory response caused by follicular hair or keratin retention in those clefts, as well as hair from the head.5–7 The disease consequently arises due to the chronic retention of debris due to the long-lasting pressure that occurs in that region from the forces on the sacrococcygeal terminal hair follicles. The symptoms seen can range from asymptomatic pits to acute abscess to chronic cysts, and can significantly impact the quality of life of patients.1–10
Currently, management can involve non-excisional options such as the use of phenol, glue, Floseal (human gelatine-thrombin matrix sealant), radiofrequency and laser ablation. The ideal surgical technique should theoretically eradicate the cyst and remove and clean the sinus tract or tracts, leading to complete and durable healing with good aesthetic results. Excisional approaches include lay-open, modified rhombic flaps (MRF) and Bascom's cleft lift (BCL). However, healing after some surgical excisional repairs for the treatment of PNS results in poor postoperative quality of life, with frequent clinical observation, as well as significant postoperative discomfort with recurrence rates reaching 40%.8–10
In the year 2011, Mienero was able to develop the endoscopic pilonidal sinus treatment (EPSiT),11 which drew on experiences using the video-assisted anal fistula treatment technique. Here we report on early results after the use of the EPSiT procedure for the first time in Kuwait.
PATIENTS AND METHODS
From April 2014 to October 2017, patients with symptomatic chronic or recurrent PNS were consecutively enrolled in the study and underwent the EPSiT procedure. Patients presenting with an acute abscess received antibiotic therapy for 2 weeks before enrollment. Ethical approval to conduct the study was obtained from the Ministry of Health and Kuwait Institute for Medical Specialization Ethical Approval Board.
All patients underwent the procedure under local anesthesia and sedation while prone, while the buttocks were parted by two large plasters. A single dose of cefodizime 1g was administered as prophylaxis, 30 minutes before surgery. Informed consent was obtained from all patients before surgery. Data is expressed as means and/or ranges. A weekly examination of each patient was performed in the outpatient clinic by the operating surgeon beginning 2 weeks post-operatively. Follow-up was continued until the wound fully healed, or until further intervention was required. Long-term follow-up and the recurrence of the disease was assessed during these outpatient consultations.
Complete wound healing was the primary end-point; if wound discharge or swelling persisted after postoperative day 60, healing was considered incomplete. A recurrence was defined by symptoms of local pain, discharge or intermittent swelling 4 months or more after the time of complete healing.
Endoscopic pilonidal sinus treatment (EPSiT) surgical technique
EPSiT is performed with a fistuloscope manufactured by Karl Storz (Southbridge, Massachusetts, USA). In the kit (Figure 1), there is an electrode connected to the electrosurgical knife power unit, an endobrush, tongs, and a Volkmann spoon. The fistuloscope has an 8° angle eyepiece and is equipped with an optical channel 14-cm long with a handle, an operative channel, and an irrigation channel. The latter channel is connected to a 5000-mL bag containing a solution of glycine with 1% mannitol. If the external orifice is too small, it is enlarged with a scalpel or diathermy, to allow introduction of the fistuloscope.
Figure 1.

Equipment used for the endoscopic pilonidal sinus treatment (EPSiT) procedure.
The first step of the EPSiT procedure is diagnostic, used to characterize the anatomy of the tracts, during which a fistuloscope is introduced through the external opening. The sinus cavity and fistula tract are identified. This is followed by the operative step, which attempts to achieve intraluminal destruction and removal of waste material via the fistula tract.. During this phase, an electrode is introduced through the operative channel, and the cavity and fistula tract are ablated and the granulation tissue is destroyed. A brush or Volkmann spoon are then inserted into the operative channel, which are used to remove the granulation tissue. If hairs are identified during the procedure, they are removed with tongs designed for that purpose that are inserted through the operative channel. The continuous lavage of the washing solution allows full elimination of debris and blood (Figure 2). At the end of the procedure, a light dressing with no packing was applied. Daily bath and weight reduction were advised to all patients post operatively.
Figure 2.
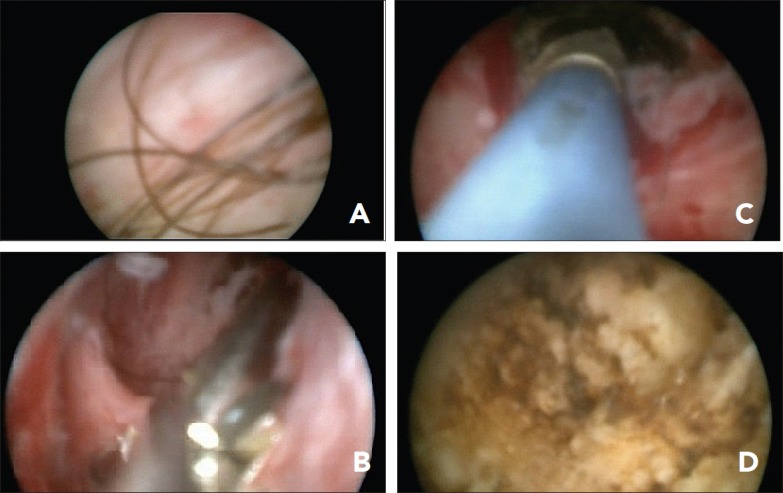
Endoscopic visualization while performing the procedure: (A) diagnostic phase hair inside sinus tract; (B) hair extraction by endoscopic forceps; (C) ablation of the tract using endoscopic diathermy; (D) final appearance after tract ablation.
Pain scoring
Pain scoring was assessed by the need for analgesics. If patients required less than 500 mg of acetaminophen every 8 hours (less than 1500 mg per day), it was considered as mild pain; if the patients require between 500 mg–1000 mg of acetaminophen every 8 hours (1500 mg–3000 mg per day), it was considered as moderate pain; and if the patients required more than 1000 mg of acetaminophen every 8 hours (more than 3000 mg per day), they were considered to have severe pain.
Statistical analysis
Statistical analysis of the data was carried out using SPSS software version 22. The difference between the two values was analyzed using a two-tailed unpaired t test. Significance levels were assessed at P value <.05. The work has been reported in line with the STROCSS criteria (Strengthening the Reporting of Cohort Studies in Surgery).12
RESULTS
Thirty-five patients were consecutively enrolled to undergo PNS treatment using the EPSiT method. The EPSiT procedure was performed as a first time treatment for PNS in 21 cases (60%) patients, and after another surgical procedure in 14 patients (40%) (Table 1). A single tract was used in 32 (91%) of patients, while the rest had bilateral tracts. Twelve (34%) patients underwent the procedure as a day case (Table 2). On follow-up, 5 (14%) patients reported minimal pain while 30 (86%) reported no pain. None of our patients experienced early wound complications such as haematoma, seroma or necrosis, necessitating hospitalization. Patients were followed up for 6 months after the surgery. There were 2 (6%) recurrences encountered at the 6-month follow-up period (Table 3). Of the 2 recurrences, both were in male patients, while 1 was in a patient that received the EPSiT after recurrence. The 2 patients that experienced recurrence did not have any pain after surgery. Both women did not report any pain post-op after surgery.
Table 1.
Clinical and demographic characteristics of patients (n=35).
| Age (years) | 22 (15–51) |
| Male | 33 (94) |
| Recurrent disease | 14 (40) |
| Incision and drainage | 6 (17) |
| Rhomboid flaps | 4 (11) |
| Lay-0pen | 3 (9) |
| Multiple procedures | 1 (3) |
Data are mean (range) or number (percentage)
Table 2.
Intra-operative features.
| Tract length (cm) | 5.0 (1.5–12) |
| Tract Numbers | |
| Single | 32 (91) |
| Multiple | 3 (8.6) |
| Operative time (min) | 47.5 (30–115)* |
(%),
Range.
Table 3.
Post-operative features.
| Pre-discharge | |
| Pain (minimal) | 5 (14%) |
| Fever | 0 (0%) |
| Hospital stay (days) | |
| Discharge same day | 12 (34%) |
| 1 day | 18 (51%) |
| 2 days | 1 (3%) |
| Follow-up at 6 months | |
| Recurrence | 2 (6%) |
DISCUSSION
Pilonidal sinus (PNS) disease is an insidious disease that significantly affects the quality of life. It arises as a foreign body response due to retention dermatopathy that occurs from the inclusion of keratin plugs, hair and debris at the level of follicular and head hair units in the natal cleft.11, 13–15 Surgical management for this disease is still a matter of great discussion, with no clear recommendations existing in the literature. Some surgeons opt for complete excision, while others debate whether primary closure or lay-open technique provides better outcomes with regards to hospital stay, healing time and recurrence. While healing by secondary intention is associated with significantly lower recurrence rates than closed healing, it involves a longer healing time than that seen with primary closure.3, 11, 16–21 However, there are downsides with primary healing, which include an increased risk of recurrence and wound complications and costs, especially when a reconstructive flap is used.22 Previous studies have had to demonstrate recurrence rates of 17% when the wound is left open, and 30% when primary closure is performed.23
In 2008, a minimally invasive technique for the treatment of PNS was proposed by Gips et al.24 It involved the eradication of the skin openings and removal of underlying hair and debris using trephines. This was done on 1358 patients having a follow up of 6.9 years. Non-healing operative wounds were seen in 4.4% of the patients in the early post-operative period, with a recurrence rate of 6.5% during the first year. However, follow-up was incomplete in 13.8% of the cases, which may have led to a higher overall recurrence rate than that reported. Based on these results, and the pathophysiology findings reported earlier, the need for direct endoscopic visualization was determined; this is how the EPSiT procedure came into play. The fistuloscope allows for the complete endoscopic exploration of the pilonidal cavity and secondary tracts without the need for a draining lateral suture, easily identifying and removing debris and hair and completely destroying the sinus cavity and tracts, while allowing the patient to be discharged quickly after surgery, resulting in negligible morbidity after the procedure. This was seen in our patients, with the majority either discharged on the same day of surgery (34%) or the day after (51%), and only 2 patients (6%) experiencing a recurrence at a 6-month follow-up period. EPSiT also offers the extra benefit of having no surgical scar due to the fact that the external orifice is used. Additionally, only 14% of our patients noted minimal pain directly after their procedure.
A previous multicenter study conducted by Meinero et al11 showed similar results using the EPSiT procedure, with a success rate close to 95%. This success rate of >90% is similar to the best seen results from reports on the open technique according to a recent meta-analysis,11 with the extra benefits of a shorter hospital stay, less pain encountered and decreased interruption of daily activities, as well as no surgical scar. Furthermore, a meta-analysis conducted by Emile et al25 was able to show a failure of the procedure in 8% of patients, with 4% presenting with a recurrent disease, and a weighted mean failure rate of 6% of this technique, with 27% presenting with a history of a previous surgery for PNS. These findings are strikingly similar to the ones from our study, further proving the low recurrence rate in patients undergoing this procedure.
Our study does have certain limitations. These include a short follow-up period with a small number of patients, as well as the learning curve required for this procedure. Nevertheless, the EPSiT technique appears to offer acceptable results with a low recurrence rate of 6% during the early follow-up period.
In conclusion, these early results show that the EPSiT procedure provides effective healing with low recurrence rates during a 6-month follow-up period. In addition, it allows the surgeon to visualize not only the PNS, but the fistula tracts or any abscess cavities present. It also guarantees the complete destruction of the granulation tissue, ensuring the complete removal of the debris that are often located in the surrounding tissue, as was previously illustrated, achieving effective hemostasis as well.
Funding Statement
None.
DISCLOSURE STATEMENT
No competing financial interests exist.
REFERENCES
- 1.De Parades V, Bouchard D, Janier M, Berger A.. Pilonidal sinus disease. J Visc Surg. 2013;150:237–247. [DOI] [PubMed] [Google Scholar]
- 2.Ardelt M, Dennler U, Fahrner R, Hallof G, Tautenhahn HM, Dondorf F, et al. (2017). Puberty is a major factor in pilonidal sinus disease : Gender-specific investigations of case number development in Germany from 2007 until 2015. 88(11), 961–967. -7 [DOI] [PubMed] [Google Scholar]
- 3.Bascom J. Surgical treatment of pilonidal disease. BMJ Evid Based Med. 2008;336:842–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCallum I, King PM, Bruce J.. Healing by primary versus secondary intention after surgical treatment for pilonidal sinus. Cochrane Database Syst Rev. 2007; CD006213 Review. Update in: Cochrane Database Syst Rev. 2010; CD006213. [DOI] [PubMed] [Google Scholar]
- 5.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980; 87: 567–72. [PubMed] [Google Scholar]
- 6.Bascom J. Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum. 1983; 26: 800–7. [DOI] [PubMed] [Google Scholar]
- 7.Stelzner F. Causes of pilonidal sinus and pyoderma fistulans sinifica (abstract in English). Langenbecks Arch Chir Suppl Kongressbd. 1984; 362: 105–18 [DOI] [PubMed] [Google Scholar]
- 8.Tejirian T, Lee JJ, Abbas MA.. Is wide local excision for pilonidal disease still justified? Am Surg. 2007; 73: 1075–8. [PubMed] [Google Scholar]
- 9.Horwood J, Hanratty D, Chandran P, Billings P.. Primary closure of rhombic excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta-analysis of randomized controlled trials. Colorectal Dis. 2012; 14: 143–51. [DOI] [PubMed] [Google Scholar]
- 10.Enriquez-Navascues JM, Emparanza JI, Alkorta M, Placer C.. Meta-analysis of randomized controlled trials comparing different techniques with primary closure for chronic pilonidal sinus. Tech Coloproctol. 2014;18:863–872. [DOI] [PubMed] [Google Scholar]
- 11.Meinero P, Mori L, Gasloli G.. Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol. 2014; 18: 389–92. [DOI] [PubMed] [Google Scholar]
- 12.Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R and Orgill DP, for the STROCSS Group. The STROCSS Statement: Strengthening the Reporting of Cohort Studies in Surgery. Int J Surg. 2017. (article in press)[[AUTHOR: Replace if change guideline reference]] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Laffert M, Stadie V, Ulrich J et al.. Morphology of pilonidal sinus disease: some evidence of its being a unilocalized type of hidradenitis suppurativa. Dermatology. 2011; 223: 349–55. [DOI] [PubMed] [Google Scholar]
- 14.Page BH. The entry of hair into a pilonidal sinus. Br J Surg 1969; 56: 32. [DOI] [PubMed] [Google Scholar]
- 15.Da Silva JH.. Pilonidal cyst. Cause and treatment. Dis Colon Rectum 2000; 43: 1146–56. [DOI] [PubMed] [Google Scholar]
- 16.Kronberg O, Christensen KI, Zimmerman-Nielson O.. Chronic pilonidal disease: a randomised trial with complete three year follow up. Br J Surg 1986; 72: 303–4. [DOI] [PubMed] [Google Scholar]
- 17.Mercantini P, Di Somma S, Magrini L et al.. Preoperative brain natriuretic peptide (BNP) is a better predictor of adverse cardiac events compared to preoperative scoring system in patients who underwent abdominal surgery. World J Surg 2012; 36: 30. [DOI] [PubMed] [Google Scholar]
- 18.Rao M, Zawislak W, Gilliland R.. A prospective randomized trial comparing two treatment modalities for chronic pilonidal sinus. Int J Colorectal Dis 2001; 3(Suppl 1): 102. [DOI] [PubMed] [Google Scholar]
- 19.Fuzun M, Bakir H, Soylu M et al.. Which technique for treatment of pilonidal sinus—open or closed? Dis Colon Rectum 1994; 37: 1148–50. [DOI] [PubMed] [Google Scholar]
- 20.Fowler H, Javed MA, Jain Y, Singh S, Rajaganeshan R.. Comparison of conventional Incision and drainage for pilonidal abscess versus novel Endoscopic Pilonidal Abscess Treatment (EPAT) Tech Coloproctol. Conference: Association of coloproctology of great Britain and Ireland annual meeting, ACPGBI 2017. United Kingdom, 2017, 19(Supplement 4), 10. [DOI] [PubMed] [Google Scholar]
- 21.Mantoo S, Natarajan S.. Comparative analysis of Endoscopic Pilonidal Sinus Treatment (EPSiT) and non EPSiT therapies in an Asian population cohort Tech Coloproctol. Conference: 12th scientific and annual meeting of the European society of coloproctology. Germany, 2017, 19(Supplement 2), 64 [Google Scholar]
- 22.Fazeli MS, Adel MG, Abaschi AH.. Comparison of outcomes in Z plasty and delayed healing by secondary intention of the wound after excision of the sacral pilonidal sinus: results of a randomized, clinical trial. Dis Colon Rectum 2006; 49: 1831–6. [DOI] [PubMed] [Google Scholar]
- 23.Doll D, Krueger CM, Schrank S et al.. Timeline of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum 2007; 50: 1928–34. [DOI] [PubMed] [Google Scholar]
- 24.Gips M, Melki Y, Salem L et al.. Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum 2008; 51: 1656–62. [DOI] [PubMed] [Google Scholar]