ABSTRACT
BACKGROUND:
Patients with psychiatric illness are more prone to develop obesity and dental caries due to general self-negligence associated with psychiatric illness and side effect of various medications used in psychiatry.
OBJECTIVE:
Assess the association between dental caries status and obesity among resident patients.
DESIGN:
Descriptive, cross-sectional.
SETTING:
Mental health hospital.
PATIENTS AND METHODS:
A sample of psychiatric in-patients was recruited. Dental caries detection was performed according to the World Health Organization criteria and body mass index (BMI) was measured. Relationships were assessed using multivariable logistic regression.
MAIN OUTCOME MEASURES:
Relationships between decayed, missing and filled teeth (DMFT) and obesity.
SAMPLE SIZE:
223.
RESULTS:
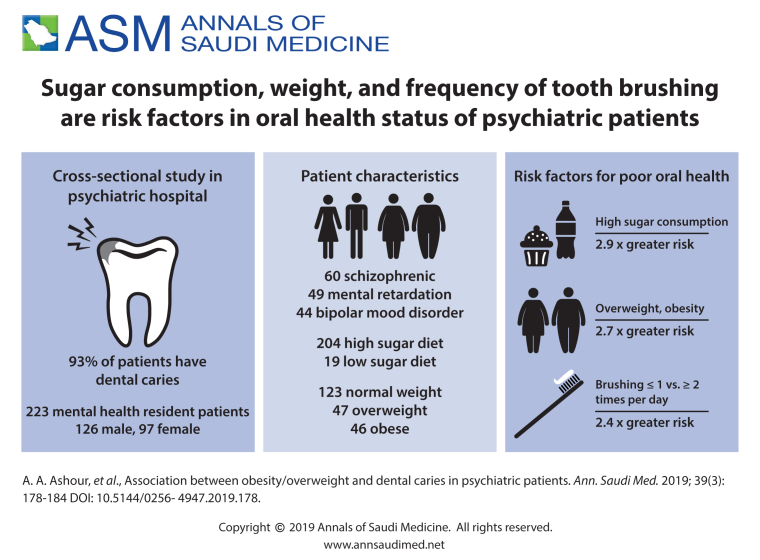
The sample included 126 males and 97 female with a mean (SD) age of 42.3 (2.2) years. The prevalence of dental caries was 92.6%. The mean (SD) DMFT score was 5.2 (4.2). Twenty-seven percent were schizophrenic, 21.9% had mental retardation and 19.7% had bipolar mood disorder. The mean (SD) BMI was 27.7 (6.3) kg/m2. One hundred twenty-three (55.2%) of in-patients were classified as normal weight, 47 (21.1%) as overweight, and 45 (20.2%) as obese. The logistic regression model showed a strong association between caries and obesity/overweight (adjusted odds ratios=2.7; 95% CI=1.4 – 4.3, P<.001).
CONCLUSION:
The present study demonstrated a significant association between the frequency of caries and obesity/overweight among resident patients at a psychiatric hospital.
LIMITATIONS:
Since the data were cross-sectional, causal relationships cannot be established and the observed association could be due to other unexplored factors.
CONFLICT OF INTEREST:
None.
INTRODUCTION
Psychiatric illness is a serious medical condition that affects people of all economic levels and all nations and influences the affected individual's feeling, moods, thoughts and behavior.1 There are a wide range of psychiatric illness such as anxiety, depression, schizophrenia, bipolar disorder, panic disorder, eating disorder, and addictive behaviors.1 Worldwide, the prevalence of psychiatric illness ranges from 17% to 30%, affecting one in four people both in developed and developing nations.2–4 In Saudi Arabia, few point prevalence studies conducted have reported 48% prevalence of mental illness among High school students, 18.2% among adult primary care patients, 59.4% of adolescents suffering from at least one of the Depression Anxiety and Stress Scale (DASS) disorders and increase in relative frequency of drug combinations for substance abuse form 25 to 43% between 1986 to 2006.5–8 These psychiatric illnesses are of great concern because these disorders affect the general behavior of a person, alter the level of perception and impair the level of functioning.4 This group is often neglected because of social stigma, ignorance, negative attitudes, misconception and fear.4 They are more prone to metabolic disorders like obesity because of psychotropic medications, unhealthy lifestyles, cigarette smoking and healthcare inequalities.9–13 Ringen et al10 showed a 44% obesity prevalence among psychiatric inpatients. Individuals with chronic mental illness have nearly a four-fold greater risk of developing obesity than individuals without psychiatric illness, and all antipsychotics are associated with weight gain.13 Along with obesity, patients with psychiatric illness are more prone to develop oral diseases,14–19 in particular dental caries. A systematic review by Kisely et al20, 21 showed significantly higher mean caries scores among patients with mental illness compared to those without psychiatric illness. The odds of getting dental caries was 1.2 (95% CI 1.14–1.30) among individuals with psychiatric illness compared with a nonpsychiatric population. This may be attributed to the adverse effects of various medications used in mental illness, self-negligence associated with psychiatric illness, fear of dental treatment and lack of access to oral health care.14–25 Antipsychotics tend to cause obesity9–13 and an increased prevalence of oral disease,14–21 in particular dental caries due to reduced salivary flow associated with these drugs. Both obesity and tooth decay are multifactorial diseases, with diet being a common factor.26 The few authors who have studied the relationship between tooth decay and obesity have found a positive association.27–35 Considering the high prevalence of dental caries14–21 and obesity9–13 in patients with psychiatric disorders, and the common risk factor associated with both the disease—consumption of simple sugars26 and the use of antipsychotic medication,13 the present study was conducted with an aim to assess the association between dental caries and obesity among psychiatric patients at a mental health hospital in Taif, Saudi Arabia.
PATIENTS AND METHODS
This descriptive cross-sectional study included psychiatric in-patients at the Mental Hospital, Taif, Saudi Arabia during December 2017 to April 2018. Based on the results of a pilot study of 25 psychiatric in-patients, we estimated that 65% of our study population had indicators of caries. Assuming a proportion of 0.65, at type I error of 0.5% and a power of 80%, a sample of 210 was needed for this study. The final sample was size increased to 220 to cover nonresponse. Ethical approval was obtained from the Ministry of Health, Directorate of Health Affairs, Research and Studies Department, Taif (Ethical clearance number – HAP–02–T–067). Written informed consent was obtained from the guardians of selected participants prior to the start of the study. Subjects with aggressive behavior and lack of cooperation, edentulous patients and subjects unable to provide written informed consent were excluded from the study.
All guardians of the selected participants received a semi-structured questionnaire. The information was collected from the guardians through face-to-face interview. Questionnaires were used to get sociodemographic details, duration of stay in hospital, medications, oral hygiene practices and dietary habits. The following information was collected on each study participant: age of the participants (years and months), oral hygiene practices (frequency of tooth brushing categorized as ≤1 time/day versus ≥2 times / day and use of fluoridated toothpaste), dietary information (72-hour recall dietary history, which spanned 2 weekdays and a weekend day with information on meals frequency, sugar consumption in terms of frequency, form, time of consumption and consistency. Sugar consumption was recorded as present if the participants consumed snacks like candies, cakes, cookies, chocolate, biscuits and ice-creams, fruit juice, non-diet or other sugar-containing drinks. The reliability of the questionnaire was assessed by asking 20 guardians to complete it through face to face interview. Questionnaire showed high reliability with a Cronbach's Alpha=0.85.
The participants were weighed to the nearest 100 g using a platform scale that was calibrated prior to each weight measurement. The participants were dressed in a minimum amount of clothing, which permitted them to stand erect and relaxed. A stadiometer was used to measure the height of the participants. The participants were barefoot, maintaining the head in a neutral position, with spinal column, neck and knees in physiological extension, and the soles of feet totally supported on a horizontal surface. Body mass index (BMI; weight/height in kg/m2) was calculated and participants were classified into four categories: obese: >30 kg/m2, overweight: 25–30 kg/m2, normal weight: 18.5-25 kg/m2 and underweight <18.5 kg/m2.36
Dental examination of study participants was done under natural light using Community Periodontal Index (CPI) probes and plane mouth mirrors. The instruments were sterilized by autoclave. No radiographs/transillumination were used. The single examiner examined all participants. Dental caries as decayed missing filled teeth/surface (DMFT/DMFS) were diagnosed according to World Health Organization guidelines.37 Frank cavities and visible caries in interproximal surfaces were recorded. The intra-examiner calibration was performed with respect to dental caries diagnosis criteria. The analysis showed significant correlation with a kappa value of 0.95, P<.05.
Frequency distribution tables were obtained for all independent and outcome variables. Differences in proportion was tested using chi-square tests and Kruskal-Wallis H analysis of variance followed by intergroup comparisons using the Mann-Whitney U test. Difference in means were tested using independent sample t tests and one way analysis of variance (ANOVA) followed by intergroup comparison using Tukey's post hoc. Relationships between DMFT, BMI, age, gender, sugar consumption, and oral hygiene practice were assessed using multivariable logistic regression analysis. Adjusted odds ratios (ORs) and their 95 percent confidence intervals (CI) were calculated. We adjusted for the following confounders: age, gender, sugar consumption and oral hygiene habits. Multivariate regression included age, gender, BMI, oral hygiene practices and sugar consumption as predictors and caries as outcome. Analysis was performed using the SPSS version 17 (SPSS Inc, Chicago IL USA). All statistical tests were two-sided, and the significance level was set at P<.05.
RESULTS
The study included 223 (126 male, 97 female) psychiatric in-patients with a mean (SD) age of 42.3 (2.2) years. Sixty (27%) patients were schizophrenic, 49 (21.9%) had mental retardation and 44 (19.7%) presented with bipolar mood disorder. The overall sample mean BMI was 27.7 (6.3). One hundred twenty-three (37.2%) inpatients were normal weight, 47 (31.2%) were overweight and 45 (27.3%) were obese. The mean (SD) duration of stay in the hospital was 7.2 (4.7) years. One hundred and thirty-seven (61.4%) patients were receiving antidepressants (amitriptyline, mirtazapine, agomelatine). Fifty-two (23.3%) psychiatric patients were taking antipsychotics (haloperidol, trifluoperazine, aripiprazole, invega, benztropine) and anticonvulsant drugs (valproic acid, carbamazepine). Thirty-four (15.2%) were taking anxiolytics (diazepam, clonazepam), and mood stabilizers (sodium valproate).
Older subjects had a higher prevalence of obesity compared to younger subjects (Table 1). Mean DMFT scores were higher (6.7 [5.2]) among 31 to 60 year-old psychiatric inpatients compared to 19 to 30 year-olds (5.1 [4.1], P=.04). Female psychiatric inpatients had higher (7.4 [6.4]) mean DMFT scores compared to males (6.4 [5.3], P=.02). Table 2 presents mean caries scores (DMFT) by BMI, sugar consumption and oral hygiene habits. Statistically significant differences were seen between mean caries scores and all the variables studied. Overweight and obese patients presented with higher mean DMFT scores compared to normal weight patients (P<.05).
Table 1.
Demographic and clinical characteristics by body mass index categories.
| Variable | BMI categories | |||
|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | |
| Age (years) | ||||
| 19–30 (n=136) | 5 (3.7) | 83 (61.03) | 29 (21.3) | 19 (13.9) |
| 31–63 (n=87) | 3 (3.4) | 40 (45.9) | 18 (20.7) | 26 (29.9) |
| Total (n=223) | 8 (3.6) | 123 (55.2) | 47 (21.1) | 45 (20.2) |
| Chi-square, P value | .2 | .08 | .21 | .03 |
| Gender | ||||
| Male (n=126) | 2 (1.6) | 71 (56.3) | 28 (22.2) | 25 (19.8) |
| Female (n=97) | 6 (6.2) | 52 (53.6) | 19 (19.6) | 20 (20.6) |
| Chi-square, P value | 0.21 | 0.17 | 0.32 | 0.23 |
| Duration of stay in hospital | ||||
| Acute (<5 years) (n=168) | 5 (3) | 95 (56.5) | 37 (22.02) | 31 (18.5) |
| Chronic (≥5 years) (n=55) | 3 (5.5) | 28 (50.9) | 10 (18.2) | 14 (25.5) |
| Chi-square, P value | .12 | 0.9 | 0.7 | 0.07 |
Data are number (percentage)
Table 2.
Mean caries score, decayed teeth, decayed surface and decayed missing filled teeth (DMFT) score by clinical variables.
| Variables | n | Decayed teeth (DT) | DMFT | Decayed surface (DS) |
|---|---|---|---|---|
| Body mass index | ||||
| Underweight | 8 | 2.1 (1.0) | 2.7 (1.6) | 3.1 (2.2) |
| Normal weight | 123 | 3.7 (3.2) | 4.3 (4.1) | 6.1 (6.1) |
| Overweight (OW) | 47 | 4.7 (3.1) | 5.2 (4.7) | 7.2 (5.3) |
| Obese (O) | 45 | 4.3 (2.9) | 4.1 (3.6) | 7.1 (4.6) |
| ANOVA, P value | .007 | .04 | .04 | |
| Tukey Post Hoc | NA | OW > NW | OW and O > NW | |
| Sugar consumption | ||||
| Yes | 204 | 3.9 (3.2) | 5.9 (4.2) | 7.2 (6.5) |
| No | 19 | 1.5 (1.1) | 2.3 (1.8) | 2.8 (1.6) |
| t test, P value | 0.02 | 0.001 | 0.001 | |
| Oral hygiene habits | ||||
| Tooth brushing frequency | ||||
| ≤1 time/day | 198 | 4.1 (3.3) | 6.4 (5.1) | 8.7 (7.2) |
| ≥2 times/day | 25 | 1.9 (1.1) | 2.8 (2.1) | 3.2 (2.7) |
| t test, P value | .02 | .03 | .001 | |
ANOVA: Analysis of variance; DMFT: Decayed missing filled teeth.
The multiple logistic regression analysis showed that patients who brushed their teeth ≤1 times/day had a 2.4 times higher risk of having dental caries compared to those who brushed ≥2 times/day (Table 3). Overweight and obese patients has 2.7 times greater risk of having dental caries compared to underweight and normal weight patients. Subjects who consumed sugar were 2.9 times (adjusted ORs=2.9; 95% CI=1.1–4.5, P<.001) higher risk of having dental caries than subjects with no sugar consumption.
Table 3.
Multiple logistic regression of factors associated with presence of dental caries.
| Variable | Dental caries (yes/no) | Dental caries % yes | Un-adjusted odds ratio (95% CI) | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|
| Age in years | ||||
| 19–30a | 124/12 | 91.2 | ||
| 31–63 | 80/7 | 92 | 0.6 (0.12–1.2) | 0.6 (0.13–1.3) |
| Gender | ||||
| Male | 118/8 | 93.7 | 0.7 (0.01-2.1) | 0.7 (0.02-2.2) |
| Femalea | 86/11 | 88.7 | ||
| BMI | ||||
| Underweight and normal weighta | 117/14 | 89.3 | ||
| Overweight and obese | 87/5 | 94.7 | 2.6 (1.3–4.1)b | 2.7 (1.4–4.3)b |
| Sugar consumption | ||||
| Yes | 194/10 | 95.1 | 2.9 (1.1–4.5)b | 2.9 (1.1–4.5)b |
| Noa | 10/9 | 52.6 | ||
| Tooth brushing frequency (times per day) | ||||
| 1≤ | 194/4 | 97.9 | 2.3 (0.9–3.2)0b | 2.4 (0.7–3.6)b |
| ≥2 | 10/15 | 52.6 | ||
Reference value,
P<.001,
P< .05.
−2 likelihood ratio chi-square=54.972, df=13, P<.001; goodness-of-fit chi-square=102.592, P=.002, Cox and Snell r-square=.185, Nagelkerke r-square=.327, McFadden r-square=.245
DISCUSSION
Obesity and tooth decay are multifactorial diseases that have the diet in common.26 Previous authors have shown that subjects with mental illness present with high a frequency of untreated tooth decay, poor oral hygiene status14–25 and a high prevalence of metabolic disorder like obesity, hyperglycemia, elevated blood pressure and an increased risk of cardiovascular disease9–13 because of side effects of the medication, ignorance and negative attitudes. The present study of 223 psychiatric inpatients examined the relationship between tooth decay and obesity, controlling covariates like, age, gender, oral hygiene practice and sugar consumption. Results showed that 31.2% of psychiatric patients were overweight and 27.3% were obese, which is consistent with other studies that showed a high prevalence of overweight and obesity among psychiatric patients.9–13 Ninety percent of study participants presented with caries and the mean caries score (DMFT=5.2 [4.2]) for the entire study population was high, bringing our findings closer to studies conducted around the world.14–17, 19–22, 24, 25 The mean caries score was significantly higher among females psychiatric patients compared to males, which may be attributable to negligence of dental care in females compared to males. This is in line with the studies conducted previously that showed high prevalence of caries in females compared to males,14, 24 though the difference was not statistically significant.
Exploration of the link between oral disease and increased weight has been controversial. In the present study, there was a strong association between overweight and obesity and dental caries prevalence. The data showed that overweight and obese psychiatric inpatients were 2.9 times higher risk of developing dental caries compared to underweight and normal weight patients. This result is in line with previous studies which showed strong association between obesity and dental caries.28–35 Marshall et al35 suggested that common risk factors, especially sugar consumption, increased the likelihood of both obesity and dental caries. Our study indicates that psychiatric inpatients who consumed sugar were 2.9 times higher risk for developing dental caries than those who do not consume sugar. In contrast to the present study, Chu et al14 showed significant association (β=0.07, P=.041) between underweight and dental caries among resident schizophrenic patients.
In the present study, a high number of patients (88.7%) presented with irregular tooth brushing habits (≤1 time per day) and they were 2.4 times higher risk of developing dental caries compared to those who brushed their teeth regularly (≥2 times/day). Previous publications are consistent with this finding.29–31 These results vouch for the need to establish measures that promote habits for adequate oral hygiene among psychiatric inpatients.
Since the present study was cross-sectional, it is not possible to establish a causal relationships and the observed association could be due to other unexplored factors. Also, there is a high chance of recall bias in collecting dietary information. Detection of dental caries was carried out visually and no X-rays were taken.
To conclude, the results of the present study support an association between obesity and caries among psychiatric inpatients. It suggest a need for measures in prevention and management of both diseases using common risk factor approach. In the present study 91% of psychiatric inpatients consumed sugar and that was associated with high risk of dental caries (adjusted ORs 2.9). This suggest a need for a well-planned nutrition control program to avoid high weight as well as caries among these psychiatric inpatients, including meal frequency control and reduction in fermentable carbohydrates. A high prevalence of dental caries (90%) among the resident psychiatric inmates indicates an urgent need for comprehensive oral health care for this population. Attending psychiatrists, physicians, nurses, hospital administration and caregivers must be aware of the high prevalence of dental caries among these patients and should coordinate efforts to facilitate prevention and access to dental care. The Saudi Arabian government recognizes the equal rights in health care for psychiatric patients and the government has implemented several policies and guidelines to ensure that the healthcare needs of these groups are met. There is a need for an integrated effort from both public and private sector to implement practical solutions to prevent and manage obesity and caries among psychiatric patients. There is a need for future research on the topic particularly longitudinal studies to confirm the findings of the present results. This research should incorporate validated dietary assessments, oral hygiene compliance, and the role of microbes and other factors that may act as confounders or effect modifiers. Study of dental caries at an individual level must account for these variables.
Funding Statement
None.
REFERENCES
- 1.10th ed. Geneva: World Health Organization; 1993. World Health Organization International classification of Mental and Behaviour disorder, Diagnostic criteria for research, ICD.
- 2.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D.. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014. April;43(2):476–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA.. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015. March;56(3):345–65. [DOI] [PubMed] [Google Scholar]
- 4.Worldrightarrow Health Organization. WHO Mental Health Gap Action Programme (mhGAP) Geneva: World Health Organization; 2013. [Google Scholar]
- 5.Al-Sughayr AM, Ferwana MS.. Prevalence of mental disorders among high school students in National Guard Housing, Riyadh, Saudi Arabia. J Fam Community Med. 2012;19(1):47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Khathami AD, Ogbeide DO.. Prevalence of mental illness among Saudi adult primary-care patients in Central Saudi Arabia. Saudi Med J. 2002;23(6):721–724. [PubMed] [Google Scholar]
- 7.Al-Gelban KS. Depression, anxiety and stress among Saudi adolescent school boys. J R Soc Promot Health. 2007;127(1):33–37. [DOI] [PubMed] [Google Scholar]
- 8.AbuMadini MS, Rahim SI, Al-Zahrani MA, Al-Johi AO.. Two decades of treatment seeking for substance use disorders in Saudi Arabia: trends and patterns in a rehabilitation facility in Dammam. Drug Alcohol Depend. 2008;97:231–236. [DOI] [PubMed] [Google Scholar]
- 9.Hammoudeh S, Ghuloum S, Mahfoud Z, Yehya A, Abdulhakam A, Al-Mujalli et al.. The prevalence of metabolic syndrome in patients receiving antipsychotics in Qatar: a cross sectional comparative study. BMC Psychiatry 2018;27;18(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ringen PA, Faerden A, Antonsen B, Falk RS, Mamen A, Rognli EB et al.. Cardiometabolic risk factors, physical activity and psychiatric status in patients in long-term psychiatric inpatient departments. Nord J Psychiatry 2018;9:1–7. [DOI] [PubMed] [Google Scholar]
- 11.Ng B, Camacho A, Parra K, de la Espriella R, Rico V, Lozano S, Troncoso M et al.. Differences in BMI between Mexican and Colombian patients receiving antipsychotics: results from the International Study of Latinos on Antipsychotics (ISLA). Ethn Health 2018;7:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun L, Getz M, Daboul S, Jay M, Sherman S, Rogers E et al.. Independence of diabetes and obesity in adults with serious mental illness: Findings from a large urban public hospital. J Psychiatr Res 2018;99:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Correll CU, Detraux J, De Lepeleire J, De Hert M.. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015. June;14(2):119–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chu KY, Yang NP, Chou P, Chi LY, Chiu HJ.. The relationship between body mass index, the use of second-generation antipsychotics, and dental caries among hospitalized patients with schizophrenia. Int J Psychiatry Med. 2011;41(4):343–53. [DOI] [PubMed] [Google Scholar]
- 15.Denis F. The oral health of patients in psychiatric institutions and related comorbidities. Soins Psychiatr. [4][5]2014;(290):40–4. [PubMed]
- 16.Kebede Biruktawit, Kemal Temam, Abera Solomon.. Oral Health Status of Patients with Mental Disorders in Southwest Ethiopia. PLoS One. 2012; 7(6): e39142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gurbuz O, Alatas G, Kurt E, Issever H, Dogan F.. Oral health and treatment needs of institutionalized chronic psychiatric patients in Istanbul, Turkey. Community Dent Health. 2010;27(3):151–7. [PubMed] [Google Scholar]
- 18.Heaton Lisa J., Swigart Kimberly, McNelis Gavin, Milgrom Peter, Downing Donald F... Oral Health in Patients taking Psychotropic Medications: Results from a Pharmacy-Based Pilot Study. J Am Pharm Assoc (2003). 2016. Jul-Aug; 56(4): 412–417.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chu Kuan-Yu, Yang Nan-Ping, Chou Pesus, Chiu Hsien-Jane, Chi Lin-Yang.. Factors associated with dental caries among institutionalized residents with schizophrenia in Taiwan: a cross-sectional study. BMC Public Health. 2010; 10: 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson NW.. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med. 2015;77(1):83–92. [DOI] [PubMed] [Google Scholar]
- 21.Kisely S, Sawyer E, Siskind D, Lalloo R.. The oral health of people with anxiety and depressive disorders - a systematic review and meta-analysis. J Affect Disord. 2016;200:119–32. [DOI] [PubMed] [Google Scholar]
- 22.Dordevic V, Jovanovic M, Milicic B, Stefanovic V, Dukic-Dejanovic S.. Prevalence of dental caries in hospitalized patients with schizophrenia. Vojnosanit Pregl. 2016;73(12):1102–8. [DOI] [PubMed] [Google Scholar]
- 23.Corridore D, Guerra F, La Marra C, Di Thiene D, Ottolenghi L.. Oral Health Status and Oral Health-Related Quality of Life in Italian Deinstitutionalized Psychiatric Patients. Clin Ter. 2017;168(2):e77–e83. [DOI] [PubMed] [Google Scholar]
- 24.Velasco-Ortega E, Monsalve-Guil L, Ortiz-Garcia I, Jimenez-Guerra A, Lopez-Lopez J, Segura-Egea JJ.. Dental caries status of patients with schizophrenia in Seville, Spain: a case-control study. BMC Res Notes. 2017;10(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Mobeeriek A. Oral health status among psychiatric patients in Riyadh, Saudi Arabia. West Indian Med J. 2012;61(5):549–54. [DOI] [PubMed] [Google Scholar]
- 26.Mathus-Vliegen EMH, Nikkel D, Brand HS.. Oral aspects of obesity. Int Dent J 2007;57:249–56. [DOI] [PubMed] [Google Scholar]
- 27.Tappuni AR, Al-Kaabi R, Joury E.. Effect of Free Sugars on Diabetes, Obesity, and Dental Caries. J Dent Res 2017;96:116. [DOI] [PubMed] [Google Scholar]
- 28.Basha S, Mohamed RN, Swamy HS, Ramamurthy PH, Sexena V.. Caries Incidence Among Obese Adolescents: A 3-year Prospective Study. Oral health & preventive dentistry 2017: 15 (1), 65. [DOI] [PubMed] [Google Scholar]
- 29.Idrees M, Hammad M, Faden A, Kujan O.. Influence of body mass index on severity of dental caries: cross-sectional study in healthy adults. Ann Saudi Med. 2017. Nov-Dec;37(6):444–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chala S, El Aidouni M, Abouqal R, Abdallaoui F.. U-shaped association between untreated caries and body mass index in adults at Rabat dental University hospital, Morocco: cross sectional study. BMC Res Notes. 2017. January 3;10(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alswat K, Mohamed WS, Wahab MA, Aboelil AA.. The Association Between Body Mass Index and Dental Caries: Cross-Sectional Study. J Clin Med Res. 2016. February;8(2):147–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prpic J, Kuis D, Pezelj-Ribaric S.. Obesity and oral health–is there an association? Coll Antropol. 2012. September;36(3):755–9. [PubMed] [Google Scholar]
- 33.Nisreen AS, Amal AS, Basha Sakeenabi.. Association between dental caries and obesity among special care female children from Makkah City, Saudi Arabia. Annals of Saudi Medicine 2018;38(1):28–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basha S, Mohamed RN, Swamy HS, Ramamurthy PH, Sexena V.. Caries Incidence Among Obese Adolescents: A 3-year Prospective Study. Oral health & preventive dentistry 2017: 15 (1), 65. [DOI] [PubMed] [Google Scholar]
- 35.Marshall TA, Eichenberger-Gilmore JM, Bronffitt BA, Warren JJ, Levy SM.. Dental caries and childhood obesity: roles of diet and socioeconomic status. Community Dent Oral Epidemiol. 2007;35:449–58. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Obesity and overweight, Fact sheet number 311. WHO; 2015. [accessed 30/12/2017]. Available from http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- 37.World Health Organization. Oral Health Surveys: basic Methods. 5th ed. Geneva: World Health Organization; 2013. [Google Scholar]