Abstract
Purpose
While LUTS and bladder behaviors are known to be associated with certain occupations, little is known about restroom access or environmental factors that may contribute to this relationship. This study aimed to characterize reasons women limit restroom use at work and to determine whether women who limit use at work report more unhealthy bladder habits and LUTS.
Materials and Methods
We conducted a cross-sectional study of full-time working U.S. women. Women completed validated questionnaires recording toileting behaviors, LUTS, and perceptions of their occupational toilet environment. Women who limited restroom use at work “most” or “all of the time” were compared to those who either did not limit or did so “occasionally” or “sometimes.”
Results
Of the 3,062 women in the final analytic sample, 11% reported limiting restroom use at work ‘most’ or ‘all of the time’. This group reported lower satisfaction with restroom cleanliness and privacy, in particular, and more frequently identified toilet factors of poor quality, limited accessibility, and restricted use by employer. The prevalence of unhealthy bladder habits was significantly higher among women who limited restroom use, as was the prevalence of urgency, monthly urinary incontinence, and infrequent voiding.
Conclusions
In this cross-sectional study of women working full time, those who limit restroom use at work reported higher prevalence of unhealthy bladder habits and certain urinary disorders. Future studies should determine if limited restroom use at work is a modifiable risk factor for unhealthy bladder habits and bladder health outcomes.
Mesh Terms/Keywords: lower urinary tract symptoms, urinary incontinence, risk factors, women, bladder health, workplace, toilet facilities
Introduction
A central tenet of current understanding of bladder dysfunction is that certain occupations have higher risks for developing LUTS.1,2 Conceptually this occurs through adoption of unhealthy bladder habits or toilet behaviors, such as infrequent voiding, urine holding, or suppression of normal sensory driven behaviors, in response to workplace environments or policies that limit restroom accessibility.2 These habits or behaviors then subsequently contribute to the development of LUTS. However, despite being widely-accepted, limited data actually support this conceptual model.1 Few studies have addressed underlying reasons why infrequent voiding may occur or why restroom use in the workplace may be limited.
We conducted a cross-sectional survey of non-institutionalized U.S. adults collecting information on self-reported LUTS, toileting behaviors, and perceptions of access to public toilets.3 Based on the concept that limiting restroom use at work might be associated with an increased risk for LUTS,1,4 we hypothesized that women who limited restroom use at work would report a greater frequency of unhealthy toileting behaviors and more frequent LUTS and LUT conditions. As such, the primary objectives were to 1) identify reasons why women working full time (i.e. 40 hours or more a week) limited restroom use at work; 2) characterize bladder habits, measured with a toileting behavior questionnaire, of women who limit restroom use at work; and 3) determine whether women who limit restroom use report more LUTS or LUT conditions than those who do not limit restroom use.
Methods
Eligibility and Recruitment
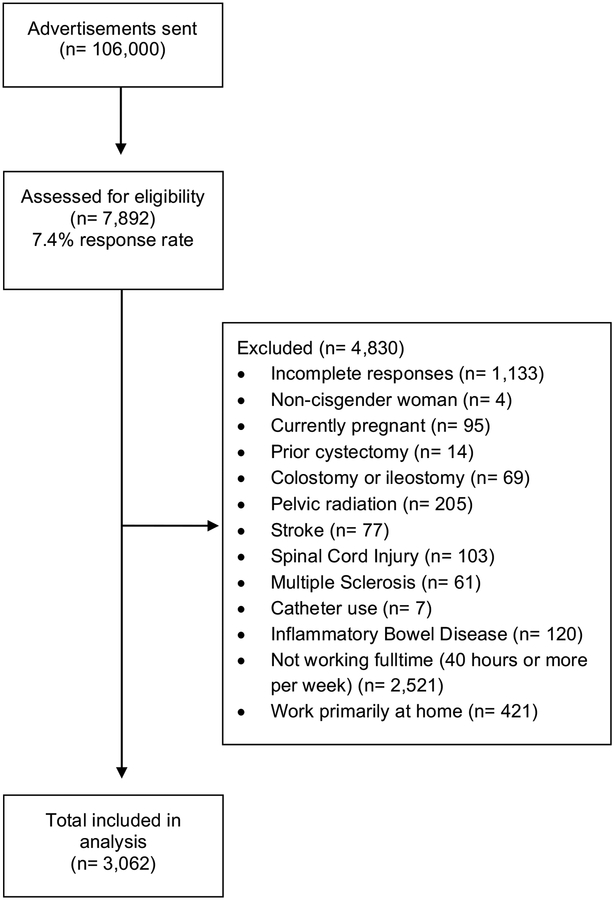
This was a secondary, planned analysis from a cross-sectional, survey-based study of research participants identified through two recruitment referral databases available at our institution.3,5–7 Between October and December 2017, approximately 106,000 potential subjects from Researchmatch and the Research Notifications Distribution received a single email advertisement that incentivized women to complete an anonymous, English-only, electronic survey with the chance to win two randomly drawn Apple iPads. Of those, 7,892 at least started the survey, for a response rate of 7.4%. No data were available for non-responders.
For this analysis, we excluded non-cisgender women who were younger than 18 years, did not complete the questionnaires, were currently pregnant, or had medical comorbidities thought to affect their bladder function and potential use of the restroom (see Figure 1 for specific exclusion reasons). In addition, we limited the analyses to those who were working full-time, defined as working 40 hours or more per week and working primarily outside of the home. The final analytic sample included 3,062 women or 38.7% of women that responded to the invitation to participate.
Figure 1.
Participant Flow Diagram.
Data Collection
In addition to demographic and clinical information, we assessed perceptions of the toileting environment and toileting practices. Our primary exposure was whether women limited restroom use at work, which was assessed by asking “Do you purposefully limit your use of the restroom at work?” (Not at all, Occasionally, Sometimes, Most of the time, All of the time). Participants indicating that they limit restroom use at least occasionally were also asked, “Please select reasons you limit use of the bathroom at work. Check all that apply” with response options of “Quality of the restroom is poor”, “Limited availability of restroom”, “Too busy with work”, “Restricted access by supervisor/company”, and “Other reason”. We also asked: “Thinking about the restroom at your place of employment, please rate how satisfied you are with the following” with questions specific to restroom accessibility, cleanliness, availability of toiletries, safety, and privacy. Responses were scored individually on a 10-point VAS (1 extremely dissatisfied, 5 neutral, 10 extremely satisfied) for each domain (e. g, accessibility, cleanliness, etc.).
Toileting behaviors were assessed using the TB-WEB scale, which collects behavior responses across five domains: place preference, premature voiding, delayed voiding, straining voiding, and position preference.8 Responses were summed for each domain to create subscale scores and dichotomized to whether a woman performs the behavior at least often (i.e. often or always vs. never, occasionally, or sometimes), representing habitual behavior.9 In addition, women responded to a single item about limiting fluid intake: “Do you cut down on the amount of fluid you drink so that your urinary symptoms improve?” (Never, Occasionally, Sometimes, Most of the time, All of the time).10
The primary bladder health outcomes targeted were LUTS and LUT conditions assessed with the ICIQ-FLUTS with a 4-week recall.10 This allowed us to calculate total score and subscales for filling, voiding, and OAB symptoms and to define LUT conditions with dichotomized items for infrequent voiding (<7 times per day), and for urgency, UUI, and SUI defined as at least sometimes. We defined OAB as urgency and/or UUI at least sometimes.11 Participants completed the ICIQ-Urinary Incontinence Short Form.12 Monthly UI was defined as any frequency of urine leakage in the past month and any amount of urine leaked more than “none”.13 Subjects reported whether they had 3 or more urinary tract infections in the past year (i.e. recurrent UTI).
Statistical Analysis
The primary exposure for study analyses was whether women limit using the restroom at work. We arbitrarily defined women as limiting restroom use if they selected either “most of the time” or “always”, as we considered this to potentially reflect habitual behavior, in a manner analogous to dichotomous definitions reported for toileting behaviors.9 Women selecting “not at all”, “occasionally”, or “sometimes” were considered to not limit restroom use. For descriptive analyses, we used t-tests to compare continuous variables and Chi square statistics for categorical variables. We also calculated 95% confidence intervals around point estimates.
To test our hypothesis that women who limit using the rest room are more likely to report LUT conditions, we created multivariable linear and logistic regression models to calculate beta co-efficients and OR for each LUT symptom scale and condition, respectively, as the dependent variable and whether women limited restroom use as the primary exposure variable. A beta coefficient greater than 0 or OR greater than 1 suggests a positive association between limited restroom use and a LUTS or condition. Covariates in the model included demographic and clinical factors described in Table 1. All analyses used STATA 15.1 (StataCorp, College Station, TX).
Table 1:
Demographic and clinical information for women working fulltime, (n = 3,062) by whether they limit rest room use at work.
| Total | Do not, occasionally, or sometimes | Most or all of the time | P value | |
|---|---|---|---|---|
| n | 3,062 | 2,717 (89%) | 345 (11%) | |
| Age, years, mean (SD) | 38.7 (12.2) | 39.0 (12.4) | 36.7 (10.8) | .001 |
| Age range, years | 18 – 73 | 18 – 73 | 20 – 65 | |
| N (%) | N (%) | N (%) | ||
| Race/ethnicity | ||||
| NH White | 2,433 (79.5) | 2,200 (81.0) | 233 (67.5) | <.001 |
| NH Black | 269 (8.8) | 208 (7.7) | 61 (17.7) | |
| Asian | 138 (4.5) | 124 (4.6) | 14 (4.1) | |
| Other or multiple | 99 (3.2) | 80 (2.9) | 19 (5.5) | |
| Hispanic | 123 (4.0) | 105 (3.9) | 18 (5.2) | |
| General Health | ||||
| Excellent | 553 (18.1) | 502 (18.5) | 51 (14.8) | .021 |
| Very good | 1,486 (48.5) | 1,332 (49.0) | 154 (44.6) | |
| Good | 829 (27.1) | 721 (26.5) | 108 (31.3) | |
| Fair | 184 (6.0) | 154 (5.7) | 30 (8.7) | |
| Poor | 10 (.3) | 8 (.3) | 2 (.6) | |
| Pregnancies | ||||
| 0 | 1,586 (51.8) | 1,422 (52.3) | 164 (47.5) | .31 |
| 1 | 465 (15.2) | 406 (14.9) | 59 (17.1) | |
| 2 | 473 (15.5) | 420 (15.5) | 53 (15.4) | |
| 3 or more | 538 (17.6) | 469 (17.3) | 69 (20.0) | |
| Relationship Status | ||||
| Single | 1,259 (41.1) | 1,114 (41.0) | 145 (42.0) | .94 |
| Married | 1,390 (45.4) | 1,236 (45.5) | 154 (44.6) | |
| Divorced/separated/widow | 413 (13.5) | 367 (13.5) | 46 (13.3) | |
| Education | ||||
| Less than college graduate | 613 (20.0) | 517 (19.0) | 96 (27.8) | <.001 |
| College, graduate or professional | 2,449 (80.0) | 2,200 (81.0) | 249 (72.2) |
Results.
Overall, the participants were relatively young, non-Hispanic white, educated, and nulliparous (see Table 1). Of the 3,062 women, 46% reported they did not limit restroom use at work, while 24%, 19%, 8%, and 3% reported limiting restroom use occasionally, sometimes, most of the time, and all of the time, respectively. Therefore, 11% met our primary exposure definition (i.e. most or all of the time). Age, race, general health, and education were all statistically different across the two groups; however, mean age only differed by 2.3 years. Of those that limited restroom use, larger proportions described themselves as black, other, multiple race, or Hispanic and fewer had college or higher degrees.
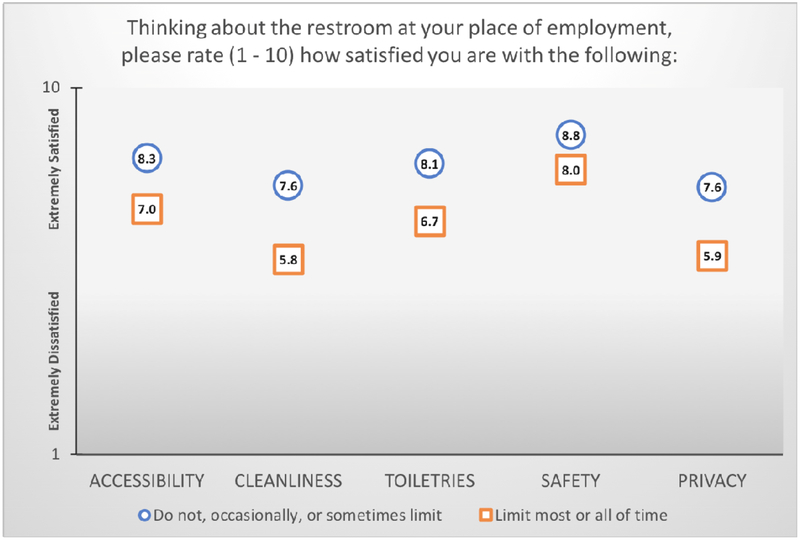
Perceived Toilet Environment
When asked to rate their satisfaction with work restrooms, most respondents indicated that they were highly satisfied with the factors presented, with VAS means anchored towards “extremely satisfied.” (Figure 2) Those who limited rest room use consistently graded satisfaction lower than those who did not limit. For both groups, Cleanliness and Privacy received the lowest scores on VAS, especially for those who limited restroom use.
Figure 2.
Women’s mean satisfaction scores from the visual analog scale (VAS) for factors associated with work restrooms, according to whether women limit the restroom while at work.
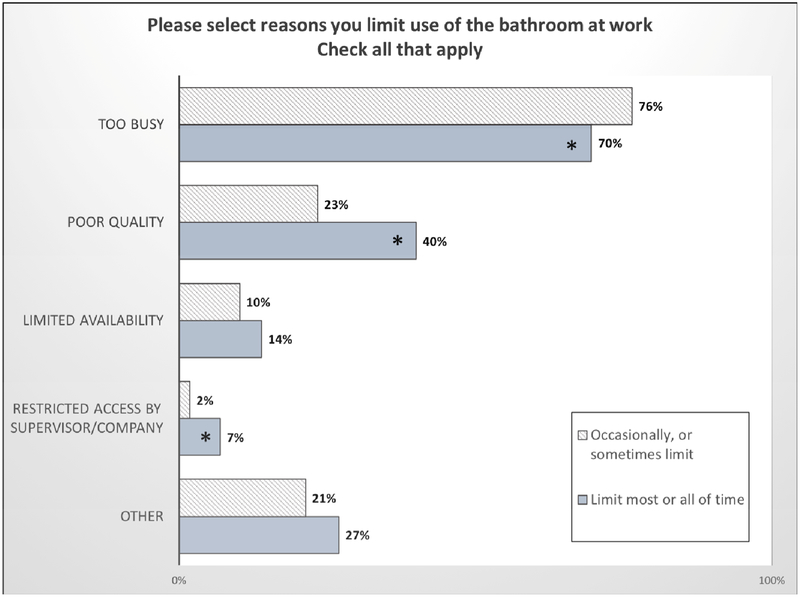
Figure 3 depicts reasons why women limit restroom use at work, for those who indicated they limited restroom use at least occasionally (n=1,668, 54%). Overall, the most common reason was that they were too busy. However, participants who limited restroom use reported being busy at work less frequently than participants who did not limit restroom use (70% vs. 76%, p<0.001). Instead, participants limiting rest room at work indicated more often that poor quality (40% vs. 23%, p<0.001), limited availability (14% vs. 10%, p=0.05), and employer restrictions (2% vs. 7%, p<.001) were reasons they limited the rest room at work.
Figure 3.
Reasons women working fulltime limited the restroom at work, if they limited use at all (i.e. items only assessed if the subjects did not answer “not at all”, n=1,668). * denotes significant differences with P<.001.
Behavioral habits
Overall one third of all women limited fluids to control LUTS at least occasionally (i.e. 67.2% never, 19.8% occasionally, 9.6% sometimes, 2.4% most of the time, and 1.1% all of the time), but this did not differ whether they did or did not limit restroom use. Those who did limit their restroom use reported significantly higher rates of habitual, unhealthy toileting behaviors, particularly for place preference, delayed voiding, straining voiding, and position preferences (see Table 2). While most women reported some degree of place preferences for voiding, greater proportions of those who limited were worried about the cleanliness of public toilets (84.4% vs. 54.5%) or avoided public toilets (72.5% vs. 26.3%), and many hold until they get home (63.8% vs. 17.3%). Other notable differences in habitual behaviors included: delay when busy (84.6% vs. 49.9%); wait until cannot hold any longer (49.3% vs. 16.2%); and, hover over the toilet when away from home (47.8% vs. 25.9%), respectively.
Table 2.
Individual toileting behaviors [% (95% CI)] and toileting behavior subscale scores [mean (95% CI)] reported by fulltime working women, according to how much they limit using the bathroom at work. Odds Ratios (individual behaviors) and beta coefficients (subscale scores) for simple regression models [measure (95%CI)].
| Do not limit restroom | Limit restroom | OR or Beta coefficient | |
|---|---|---|---|
| Place preference for voiding | |||
| Worry about cleanliness of public toilets | 54.5 (52.6, 56.4) | 84.4 (80.1, 87.8) | 4.5 (3.3, 6.1) |
| Avoid public toilets | 26.3 (24.7, 28.0) | 72.5 (67.5, 76.9) | 7.4 (5.7, 9.5) |
| Empty bladder before leaving home | 78.8 (77.2, 80.3) | 89.0 (85.2, 91.9) | 2.2 (1.5, 3.1) |
| Try to hold until get home | 17.3 (16.0, 18.8) | 63.8 (58.6, 68.7) | 8.4 (6.6, 10.7) |
| Subscale score | 13.2 (13.0, 13.3) | 16.7 (16.4, 17.0) | 3.6 (3.2, 3.9) |
| Premature voiding (empty without feeling the need to) | |||
| At home | 7.0 (6.1, 8.0) | 16.5 (13.0, 20.8) | 2.6 (1.9, 3.6) |
| When away from home | 4.2 (3.5, 5.0) | 7.0 (4.7, 10.2) | 1.7 (1.1, 2.7) |
| At someone else’s house | 3.0 (2.4, 3.7) | 5.2 (3.3, 8.1) | 1.8 (1.0, 3.0) |
| In public places | 2.5 (2.0, 3.2) | 2.0 (1.0, 4.2) | .8 (.4, 1.7) |
| Empty “just in case” | 11.6 (10.5, 12.9) | 17.4 (13.7, 21.8) | 1.6 (1.2, 2.2) |
| Subscale score | 8.8 (8.7, 9.0) | 9.4 (9.0, 9.8) | .6 (.2, 1.0) |
| Delay voiding | |||
| Delay when busy | 49.9 (48.1, 51.8) | 84.6 (80.4, 88.1) | 5.5 (4.1, 7.5) |
| Wait until cannot hold any longer | 16.2 (14.9, 17.6) | 49.3 (44.0, 54.5) | 5.0 (4.0, 6.4) |
| Wait too long (until strong urge or leak) | 18.0 (16.6, 19.5) | 52.5 (47.2, 57.7) | 5.0 (4.0, 6.3) |
| Subscale score | 8.4 (8.3, 8.5) | 11.0 (10.8, 11.3) | 2.7 (2.4, 2.9) |
| Straining voiding | |||
| To start urinating | 5.4 (4.6, 6.3) | 11.6 (8.6, 15.4) | 2.3 (1.6, 3.3) |
| To keep urine flowing | 6.4 (5.5, 7.4) | 12.8 (9.6, 16.7) | 2.1 (1.5, 3.0) |
| To empty bladder completely | 9.1 (8.1, 10.3) | 17.4 (13.7, 21.8) | 2.1 (1.5, 2.9) |
| To empty bladder faster | 9.6 (8.6, 10.8) | 22.6 (18.5, 27.3) | 2.7 (2.1, 3.6) |
| Subscale score | 7.3 (7.2, 7.5) | 8.5 (8.0, 8.9) | 1.1 (.7, 1.5) |
| Position preference, away from home | |||
| Sit on the toilet seat | 63.3 (61.4, 65.1) | 36.8 (31.9, 42.0) | .3 (.3, .4) |
| Crouch (hover) over the seat | 25.9 (24.3, 27.6) | 47.8 (42.6, 53.1) | 2.6 (2.1, 3.3) |
| Squat on the seat | 2.6 (2.1, 3.3) | 8.1 (5.7, 11.5) | 3.3 (2.1, 5.2) |
| Subscale score | 7.4 (7.3, 7.5) | 9.0 (8.7, 9.3) | 1.6 (1.3, 1.9) |
Bladder Health Outcomes
Table 3 presents the mean scores of LUTS subscales and prevalence of individual LUT conditions, as well as results of multivariable regression models. In general, the group that limited restroom use reported a higher total urinary symptom score, voiding subscale score, and urinary incontinence score, even after adjusting for co-factors. Of individual urinary conditions, urgency, OAB, monthly UI, and infrequent voiding were more commonly reported by the group that limited restroom use. Only urgency, SUI, monthly UI, and infrequent voiding were significantly associated with limiting restroom after controlling for age, race, education, pregnancy history, relationship status, and general health.
Table 3.
Comparisons of lower urinary tract symptoms and conditions in fulltime working women between those who do and do not limit restroom use at work, including results of multiple linear (beta) and logistic regression models (odds ratio).
| Do not limit restroom | Limit restroom | Regression Coefficients* | |
|---|---|---|---|
| Beta (95% CI) | |||
| ICIQ FLUTS Total Score | 6.6 (6.4, 6.8) | 7.4 (6.9, 7.9) | .66 (.14, 1.18) |
| ICIQ FLUTS Filling subscale | 2.6 (2.5, 2.7) | 2.8 (2.6, 3.0) | .03 (-.19, .25) |
| ICIQ FLUTS Voiding subscale | 1.4 (1.3, 1.4) | 1.7 (1.5, 1.9) | .25 (.06, .44) |
| ICIQ FLUTS OAB subscale | 3.0 (2.9, 3.1) | 3.1 (2.9, 3.3) | .02 (-.22, .26) |
| ICIQ urinary incontinence, short form | 3.2 (3.1, 3.4) | 3.9 (3.5, 4.4) | .58 (.15, 1.02) |
| OR (95% CI) | |||
| Urgency | 16.2 (14.9, 17.6) | 22.3 (18.2, 27.0) | 1.39 (1.04– 1.86) |
| Urgency incontinence | 14.7 (13.4, 16.1) | 16.8 (13.2, 21.1) | 1.11 (.80 – 1.52) |
| Overactive Bladder | 22.7 (21.2, 24.3) | 29.3 (24.7, 34.3) | 1.30 (.99 – 1.70) |
| Stress incontinence | 20.4 (18.9, 21.9) | 24.9 (20.6, 29.8) | 1.33 (1.01 – 1.76) |
| Urinary incontinence, monthly | 48.7 (46.8, 50.6) | 57.4 (52.1, 62.5) | 1.52 (1.18 – 1.94) |
| Recurrent UTI (≥3 in past year) | 4.2 (3.5, 5.0) | 5.8 (3.8, 8.8) | 1.35 (.82 – 2.23) |
| Void < 7 times per day | 58.0 (56.1, 59.9) | 73.6 (68.7, 78.0) | 2.02 (1.57 – 2.62) |
Adjusted for age, race, education, general health, relationship status, and pregnancies
Discussion.
In this large sample, most women did not limit their use of the restroom at work more than sometimes. However, those who did limit their use either most or all of the time reported less satisfaction with restrooms at work, more frequently identified facilities-based factors as reasons for why they limited restroom use, and described more habitual unhealthy bladder behaviors. The associations with LUTS and LUT conditions were less robust, although the ORs of urgency, stress incontinence, monthly UI, and voiding fewer than 7 times per day were significantly greater for the group that limited restroom use at work. These findings suggest that limiting restroom use at work may be associated with the development of LUTS in full time working women, especially in employment environments in which women perceive there to be restricted access to satisfactory facilities. In these circumstances women frequently report unhealthy bladder behavioral habits.
Markland et al recently reviewed several studies investigating associations between occupation groups and LUTS or LUT conditions.1 As the authors noted, almost all of these studies compared LUT conditions between occupation groups. In some cases, toilet access factors were assessed,14 but in none were toilet factors the primary level of comparison, as in the present study. Similarly, toileting behaviors have also been analyzed according to groups with or without LUTS,9,13,15,16 but not according to toilet access factors. Therefore, our approach extends beyond prior investigations by including individual restroom practices and access factors, such that comparison of the present results to previous studies is difficult.
The results of this study do provide important information on bladder behavior habits and perceptions of occupational toilet environments among adult working women that may inform future studies and policy positions. Conceptually, occupational environments may present several barriers to adequate toilet access, including factors related to time and to facilities. In this study sample, women commonly noted facility-restricted access factors such as cleanliness and privacy, which may be modifiable through design or maintenance of the restroom space. In contrast, a busy work schedule was the major reason women limited restroom use, and few attributed time limitations directly to supervisor or employer restrictions on toilet use. Addressing these time-restricted factors may require educational interventions or changes to policy and procedures in the workplace.
In this study, the insignificant or weak associations observed for bladder health outcomes could be related to several factors. Coping mechanisms that women adopt and were not assessed may mask the actual prevalence of LUTS.4,17,18 Certain LUT conditions, such as OAB, may preclude a woman from limiting her restroom use at work or it may preclude her from working full time at all.11 Similarly, working women may self-select employment opportunities without restroom limitations in order to fit their bladder conditions, thus reducing any link between restroom limitations and bladder outcomes. Our sample included relatively young adult women, and since bladder dysfunction may require long-term exposure or severely constrained toilet environments to develop LUTS, we may not have captured the most relevant workforce characteristics impacted by bladder health outcomes.
Several limitations with this study should be noted and considered in interpreting the results. As with all cross-sectional studies, we are unable to assess causality or temporal relationships. While there is an inherent selection bias to volunteer-based surveys, we tried to limit this by incentivizing participation. The large number of study subjects also helps to mitigate this bias. The response rate was low, but it is consistent with response rates for unsolicited email advertisement studies using Researchmatch.5,7 As we did not employ specific sampling strategies for recruitment to reflect certain population characteristics, our findings may not generalize or be applicable to the population at large. Certainly, our subjects do not reflect racial/ethnic and socio-economic diversity of the general population, which may be related to the mode of distribution and constituency of the data sources.5
We did not collect data on specific coping strategies that women with LUTS may employ nor did we collect data on duration of symptoms or toileting behaviors. Similarly, we did not collect data on specifics regarding the nature of work or occupation, time spent at work other than “full time”, duration of employment, or on specifics of toilet facilities. All of these opportunities would have allowed us to better characterize potential factors that may contribute to bladder behaviors and LUTS in certain employment environments and inclusion of these factors should be considered in future studies. Finally, as per the nature of a questionnaire-based study, we relied on self-report of LUTS and conditions, albeit with validated patient-reported outcome measures, when available. While developing this project, we found no examples of validated measures for assessing restroom use at work or in other situations, and therefore we explored these constructs with non-validated items. Future research is needed for developing such measures.
Despite these limitations, this study is significant in that it specifically examines restroom use at work directly. As noted above, most prior studies compare LUTS across occupational groups, for which restroom limiting is implied. This concept is not limited to a particular occupation but could be cross-cutting for any number of occupational groups, and further study is warranted on specifics related to the health impact of limiting work restroom use in diverse occupational settings.
Conclusion.
In this cross-sectional study of women working full time, those who limited restroom use at work also reported a higher prevalence of unhealthy bladder habits and certain LUT disorders, including monthly UI. In addition to being too busy, participants limited restroom use because of poor quality, limited availability, and employer restrictions. These findings suggest that limiting restroom use at work may be associated with unhealthy bladder habits and bladder health outcomes. Further studies are needed to determine if interventions to support restroom use at work would reduce LUTS.
Funding:
Research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number 1K23DK103910–01A1 and by CTSA award No. UL1 TR002243 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Markland A, Chu H, Epperson CN, et al. : Occupation and lower urinary tract symptoms in women: A rapid review and meta-analysis from the PLUS research consortium. Neurourol. Urodyn 2018; 37: 2881–2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brady SS, Bavendam TG, Berry A, et al. : The Prevention of Lower Urinary Tract Symptoms (PLUS) in girls and women: Developing a conceptual framework for a prevention research agenda. Neurourol. Urodyn 2018; 37: 2951–2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kowalik CG, Daily A, Delpe S, et al. : Toileting Behaviors of Women-What is Healthy? J. Urol 2019; 201: 129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nygaard I and Linder M: Thirst at work--an occupational hazard? Int. Urogynecol. J. Pelvic Floor Dysfunct 1997; 8: 340–343. [DOI] [PubMed] [Google Scholar]
- 5.Harris PA, Scott KW, Lebo L, et al. : ResearchMatch: a national registry to recruit volunteers for clinical research. Acad. Med 2012; 87: 66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris PA, Swafford JA, Edwards TL, et al. : StarBRITE: the Vanderbilt University Biomedical Research Integration, Translation and Education portal. J. Biomed. Inform 2011; 44: 655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heerman WJ, Jackson N, Roumie CL, et al. : Recruitment methods for survey research: Findings from the Mid-South Clinical Data Research Network. Contemp. Clin. Trials 2017; 62: 50–55. [DOI] [PubMed] [Google Scholar]
- 8.Wang K and Palmer MH: Development and validation of an instrument to assess women’s toileting behavior related to urinary elimination: preliminary results. Nurs. Res 2011; 60: 158–164. [DOI] [PubMed] [Google Scholar]
- 9.Zhou F, Newman DK and Palmer MH: Urinary Urgency in Working Women: What Factors Are Associated with Urinary Urgency Progression? J. Womens. Health 2018; 27: 575–583. [DOI] [PubMed] [Google Scholar]
- 10.Brookes ST, Donovan JL, Wright M, et al. : A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am. J. Obstet. Gynecol 2004; 191: 73–82. [DOI] [PubMed] [Google Scholar]
- 11.Coyne KS, Sexton CC, Thompson CL, et al. : Impact of overactive bladder on work productivity. Urology 2012; 80: 97–103. [DOI] [PubMed] [Google Scholar]
- 12.Avery K, Donovan J, Peters TJ, et al. : ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn 2004; 23: 322–330. [DOI] [PubMed] [Google Scholar]
- 13.Palmer MH and Newman DK: Women’s toileting behaviours: an online survey of female advanced practice providers. Int. J. Clin. Pract 2015; 69: 429–435. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y and Kwak Y: Urinary incontinence in women in relation to occupational status. Women Health 2017; 57: 1–18. [DOI] [PubMed] [Google Scholar]
- 15.Palmer MH, Willis-Gray MG, Zhou F, et al. : Self-reported toileting behaviors in employed women: Are they associated with lower urinary tract symptoms? Neurourol. Urodyn 2018; 37: 735–743. [DOI] [PubMed] [Google Scholar]
- 16.Sjögren J, Malmberg L and Stenzelius K: Toileting behavior and urinary tract symptoms among younger women. Int. Urogynecol. J 2017; 28: 1677–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fultz N, Girts T, Kinchen K, et al. : Prevalence, management and impact of urinary incontinence in the workplace. Occup. Med 2005; 55: 552–557. [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald ST, Palmer MH, Berry SJ, et al. : Urinary incontinence. Impact on working women. AAOHN J. 2000; 48: 112–118. [PubMed] [Google Scholar]